Abstract
Purpose of Review
As interest in the mental health consequences of environmental disasters increases, this review aimed to summarize peer-reviewed studies published in 2018 on posttraumatic stress disorder (PTSD) and depression symptoms after such events.
Recent Findings
Notable trends in the past year of research included studies focusing on vulnerable populations (e.g., persons with preexisting physical health conditions), assessing the cumulative impact of exposure to multiple disasters, exploring pathway leading to PTSD and depression symptoms, and evaluating the effectiveness of post-disaster interventions.
Summary
Over 100 articles were identified, focused on 40 disasters that occurred between 1982 and 2017. Prevalence estimates ranged from 0 to 70.51% for PTSD and 1.9 to 59.5% for depression. Consistent predictors of adverse outcomes included female gender, socioeconomic disadvantage, high disaster exposure, and low psychosocial resources. Further research that expands upon recent advances in the literature is critical given the large proportion of the world’s population exposed to disasters and the increasing incidence of such events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Environmental disasters are catastrophic events that result from human activity and have a devastating impact on aspects of the environment, including ecosystems and biodiversity, wildlife and agriculture, and air and water quality. These include technological disasters, such as oil spills, chemical explosions, and nuclear radiation, in which the influence of human activity is clear and direct. Growing evidence suggests that human activity has also contributed to climate change and, as a result, the greater incidence of what have traditionally been defined as natural disasters, including floods, hurricanes, tornados, earthquakes, and tsunamis [1]. A definition of environmental disasters that includes these latter events is therefore warranted.
In addition to their effects on the environment, environmental disasters have evident effects on human health, including mental health. To date, there have been several reviews of the literature on post-disaster mental health, including the seminal review published in 2002 that summarized analyses of 160 independent samples in articles published between 1981 and 2001 [2], as well as more recent reviews [3, 4]. These syntheses have demonstrated that disasters have a clear impact on mental health, with the two most common adverse outcomes being depression and posttraumatic stress disorder (PTSD). In addition, they have highlighted a range of risk factors for psychiatric adversity, including demographic characteristics (e.g., female gender), indicators of socioeconomic disadvantage (e.g., low income and unemployment), exposure to more disaster-related stressors and traumatic events (e.g., bereavement, displacement), and fewer psychological and social resources (e.g., social support, adaptive coping skills).
In the past decade, there has been substantial growth in interest in the mental health consequences of environmental disasters and a corresponding surge of research on the topic. Therefore, recognizing that the field is rapidly evolving, we set out to review the research on this topic published in 2018 and ultimately narrowed our focus to two key mental health outcomes: PTSD and depression. In our review, we summarize several characteristics of the studies reviewed, including their geographic location, sample demographics, and timing relative to the disaster, as well as the prevalence estimates and predictors of adverse outcomes reported. In addition, we highlight studies that represent current trends and advances in the field that stand to improve our ability to identify survivors at risk of post-disaster PTSD and depression to mitigate adverse outcomes.
Method
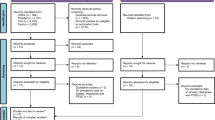
The initial intent of this review was to include any article on the mental health consequences of environmental disasters broadly defined—that is, including any psychiatric disorder, symptom, or phenomenon (e.g., stress or general psychological distress). To identify articles on this topic published in 2018, the MEDLINE and PSYCINFO databases were searched. Initial search terms included those related to environmental disasters (e.g., “oil spill,” “tornado”) and mental health (e.g., “posttraumatic stress,” “distress”). Over 700 (n=706) articles resulted from this search and an initial review of abstracts was conducted to determine eligibility. After review of abstracts, 178 articles were selected for a full-text review and we narrowed our focus to those including the two most commonly assessed psychiatric outcomes (i.e., PTSD and depression) and using quantitative analytic techniques. A total of 100 articles met these criteria and were included in the review. Three coders reviewed the articles, recording the instruments used to assess PTSD and depression, prevalence estimates reported, and significant predictors of outcomes in multivariable models. In addition, the coders reviewed articles with attention to overarching trends in the literature and efforts to understand post-disaster mental health beyond identification of prevalence estimates and predictors.
Results
Disaster Contexts
Table 1 provides an overview of the articles included in the review. The 100 articles identified drew on data from 83 studies (i.e., independent samples). These totals include six articles (five independent samples) with participants exposed to more than one disaster [5, 6•, 7,8,9,10], as well as two articles (two independent samples) with subsamples exposed to different disasters [11, 12], which are not included in Table 1.
The 31 disasters in Table 1 spanned from 1986 to 2017, with only two disasters (6.5%) occurring before the year 2000 and the majority (n = 24; 77.4%) since 2010. Of the 92 articles drawing on data from the aftermath of a single disaster, the majority (n = 87; 94.6%) were from studies conducted in the aftermath of what have been traditionally classified as natural disasters, including hurricanes (n = 12; 13.0%) and earthquakes (n = 51; 55.4%), whereas fewer (n = 9; 9.8%) were conducted in the aftermath of technological disasters, including oil spills (n = 3; 3.3%) and nuclear disasters (n = 5; 5.4%). Geographically, the majority of the 92 articles (n = 57, 62.0%) were conducted in Asia, including 18 articles from 13 independent samples after the 2008 earthquake in Wenchuan, China [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30]; 11 articles from five independent samples after the 2013 earthquake in Lushan, China [31,32,33,34,35,36,37,38,39,40,41]; and nine articles from nine independent samples after the 2015 earthquakes in Nepal [42,43,44,45,46,47,48,49, 50••]. Together, the disasters listed in Table 1 accounted for over 300,000 fatalities and nearly US$80 billion dollars in damages, according to data from the Centre for Research on the Epidemiology of Disasters [51].
Study Methods
Table 2 lists additional detail about each of the 100 articles reviewed, including descriptions of the sample and the timing of assessments. The majority of studies included adult samples (n = 49; 49.0%), nine (9.0%) focused on children and adolescent samples, and 42 (42.0%) included a mixture of adolescents and adults. The earliest post-disaster assessment was conducted 1 week post-disaster after the 2013 Ya’an earthquake in China [5], and the latest was 23 years post-disaster after the 1988 Spitak earthquake in Armenia [53]. Seven studies (7.0%) included pre-disaster data, and 24 (24.0%) were longitudinal studies (defined as having two or more waves of data). Forty-four articles (44.0%) used data from within the first post-disaster year, and 15 (15.0%) used data from five or more years post-disaster.
Prevalence Estimates
Table 2 also provides the measures used to assess PTSD and depression, and the estimated prevalence of each outcome, if reported. The range in prevalence estimates was considerable. The lowest prevalence estimate reported for PTSD was 0.0% in a study conducted after the 1982–1983 flooding, tornadoes, dioxin contamination, and radioactive well water disaster and after the 1993 great floods, both of which occurred in Missouri, USA [10], and the highest was 70.5% in a subsample of New York City and Long Island residents who did not have access to medical care after Hurricane Sandy [85]. For depression, the lowest prevalence estimate reported was 1.9% in a sample of Missouri residents after the 1982 flooding, tornadoes, dioxin contamination, and radioactive well water disaster [10], and the highest was 59.5% in a study of shelter residents after a 2016 flood in China [93,94,95]. Among the 26 articles reporting prevalence estimates for both outcomes, the estimate for depression was higher in the majority of cases (n = 20, 76.9%). Several considerations must be kept in mind when comparing prevalence estimates, including the different measures used (22 identified for PTSD and 21 for depression), different criteria used to define cases, variability in study methodologies and sample characteristics, and potential cultural influences on the interpretation of assessment items and reporting of symptoms. The patterns of results nonetheless indicate substantial variability in the prevalence of PTSD and depression in the aftermath of environmental disasters and suggest the role of risk and protective factors—which are also likely to vary across the samples included—in shaping these outcomes.
An additional consideration is whether the prevalence estimates reported represent the impact of the disaster versus the persistence of preexisting mental health problems. This issue is somewhat less of a concern for PTSD, as symptoms are explicitly tied to the experience of the disaster. As mentioned previously, only seven studies in the review (7.0%) included pre-disaster data, which allow for documentation of whether prevalence estimates increased for pre- to post-disaster as well as exploration of the role of pre-disaster factors, including pre-disaster mental health, in shaping post-disaster PTSD and depression. Absent pre-disaster data, studies in the review relied on two alternative methods to assess the impact of disaster exposure on PTSD and depression. First, a handful of studies compared symptom levels of participants residing in regions with varying levels of exposure—for example, students from two districts that were differentially exposed to the 2015 Nepal earthquakes [48], and subsamples of participants residing in areas with varying distances from the epicenter of the 2008 earthquake in Iceland [64] and the 2013 earthquake in Lushan, China [37, 38]. Second, investigators examined associations between outcomes and participants’ self-reported exposure, including dichotomous indicators of whether the participant lived in the affected area at the time of disaster [52], and items assessing various disaster-related experiences (e.g., bereavement, household damage) e.g., [18, 22].
Predictors
The patterns of significant predictors of PTSD and depression were generally consistent with those documented in prior research. Several studies documented that female participants were at increased risk for PTSD and depression e.g., [44, 92,93,94,95], whereas male gender was associated with greater risk of PTSD in only one study [17]. Studies showing age differences in outcomes varied in the direction of effects, with older participants at increased risk in some cases e.g., [18, 74••, 92,93,94,95] and younger participants at increased risk in others e.g., [46, 72, 76], and with such variability evident across both adult and child/adolescent samples. Although less commonly explored, ethnic minority and low socioeconomic status were consistently associated with adverse outcomes e.g., [6•, 83, 87], with some exceptions e.g., [25, 46, 82].
Disaster exposure was a consistent and robust predictor of PTSD and depression across the studies reviewed. Indicators of exposure that were associated with adverse outcomes included living in an area that was affected by the disaster (vs. unaffected, as per self-report) [52]; living in a highly affected area (vs. a less affected area, as per geographically defined subsamples) [37, 38, 48, 64]; specific disaster-related experiences, including injury to oneself [69, 100], injury or death of a loved one [22, 46, 100], lack of vital resources (e.g., water, medical care) [85, 92], household damage [18, 29, 92], property loss [69], displacement [61, 78, 79], and financial impacts [6•, 64, 67, 71]; counts of disaster-related experiences [26, 46]; and exposure to aversive details about the disaster via the media [14, 25]. Additionally, participants who reported experience fear or distress during the disaster were shown to be at risk of adverse outcomes [29, 47, 63].
The reviewed studies also documented several psychosocial resources that were associated with lowered risk of PTSD and depression, including social support [61, 64, 91], social cohesion [50••, 68], gratitude [39], self-esteem [29], religiosity [42], and adaptive coping strategies (e.g., mindfulness, emotion regulation) [43, 69]. Conversely, psychosocial stressors associated with heightened risk were post-disaster negative life events [22, 32, 37], family members’ psychiatric symptoms [18], survivor guilt [39], rumination [98], and maladaptive coping styles (e.g., cognitive suppression, avoidant coping) [9, 43, 47]. Prior exposures to traumatic events were also associated with greater risk, including counts of lifetime trauma [48, 53, 70] and exposure to specific events (e.g., community violence [59], interpersonal violence [11]). PTSD and depression were also frequently comorbid with other psychiatric symptoms (e.g., anxiety [22], insomnia, and other sleep problems [33, 63, 93,94,95]) and physical health problems [60•] and were highly correlated with each other [16, 63, 81].
Trends in the Literature
In reviewing the past year of literature, we took note of studies that will push the field forward in terms of identifying disaster-affected individuals most vulnerable to PTSD and depression and mitigating these outcomes. These studies fell into four categories: (1) vulnerable populations, (2) cumulative disaster exposure, (3) pathways to post-disaster symptoms, and (4) interventions. A summary of key results from each category follows.
Vulnerable populations
As in the current review, prior research has identified several individual characteristics that increase risk for PTSD and depression [2,3,4]. Within any at-risk group, there is of course variability in adverse outcomes, and studies that seek to understand the drivers of such vulnerability provide useful information in identifying survivors that might be in particular need of mental health services. Research over the past year has examined such variability in two key at-risk populations: first responders and persons with preexisting physical health conditions.
First, research on first responders has replicated some of the risk factors documented in the more general population of disaster survivors, as well as others specific to their job responsibilities. For example, a longitudinal study of over 50,000 Japanese Ground Defense Force personnel dispatched after the Great East Japan Earthquake and subsequent tsunami and nuclear disaster found that women, older adults, and those who were personally affected by the disaster were at increased risk of high posttraumatic stress reactions (PTSR); additionally, those who were tasked with body recovery duties, who were deployed for a longer amount of time, who reported that they were overworked (e.g., worked during holiday or overtime hours), and who either did not take leave at all or within 2 weeks of the end of their response work had increased odds of high PTSR [74••]. Another study in the aftermath of the August 2007 wildfire disaster in Greece found that firefighters who experienced fear of dying during their response work and who were temporary (vs. permanent) employees had higher risk of probable PTSD [63].
Studies on persons with preexisting physical health conditions have similarly replicated previously documented predictors of PTSD and depression, while further demonstrating associations between PTSD and depression and outcomes related to participants’ conditions. For example, PTSD was associated with lower antiretroviral therapy adherence among a sample of persons with HIV who were exposed to the 2015 earthquake in Nepal [45]. In a sample of older adults with hypertension exposed to Hurricane Katrina, having high PTSD symptoms was also linked incident cardiovascular disease [60•]. As in prior research, female gender, ethnic minority status, lower education, and higher disaster exposure were among the significant predictors of PTSD in this sample [60•].
Cumulative disaster exposure
A second trend in the literature was studies of PTSD and depression among persons who had endured exposure to multiple environmental disasters [6•, 7,8,9, 21]. Understanding the effects of multiple exposures will be crucial given the increasing frequency of climate change-related disasters, particularly in geographically vulnerable areas such as the US Gulf Coast [1]. In their study of multiply exposed women in Southeast Louisiana in the US Gulf Coast, Harville, Shankar, Schetter, and Lichtfeld [6•] summarized three competing models of how multiple exposures might influence mental health outcomes: a cumulative model, wherein disasters increase risk for adverse outcomes in a dose-response fashion; a sensitization model, wherein the effect of disaster exposure is enhanced among those with prior exposure, relative to those with no prior exposure; and a habituation model, wherein the effect of disaster exposure is lessened for those with prior exposure, relative to those with no prior exposure. The results of Haville and colleagues’ study [6•] mainly supported the cumulative model: participants who had a greater number of total exposures to Hurricanes Katrina, Rita, Gustav, and Ike, and the Deepwater Horizon oil spill had increased relative risk of both PTSD and depression. In one exception, the exposure to the oil spill was associated with higher PTSD symptoms for participants who had experienced illness or injury due to one of the hurricanes, consistent with the sensitization model [6•].
Another notable study took a slightly different approach to investigating multiple exposures in a sample of adolescents exposed to both the 2008 Wenchuan earthquake and the 2011 Ya’an earthquake in China [22]. The investigators of this study explored both the direct and indirect effects of Wenchuan exposure on post-Ya’an PTSD and depression symptoms, controlling for Ya’an exposure, using structural equation modeling. Greater Wenchuan exposure was directly associated with post-Ya’an PTSD only, indirectly associated with both post-Ya’an PTSD and depression via post-Wenchaun PTSD symptoms, and indirectly associated to post-Ya’an depression symptoms only via post-Wenchuan depression symptoms. Additionally, the authors found an interaction between Wenchuan and Ya’an exposure in predicting PTSD symptoms, such that the effect of greater Ya’an exposure was enhanced for adolescents who had endured greater Wenchuan exposure, thus supporting the sensitization model.
Pathways to post-disaster symptoms
A third trend in the past year of research focuses on the pathways leading to PTSD and depression. This research advances the field by showing how risk and protective factors work together to shape outcomes and offers the potential for identifying intervention targets. A few studies within this category investigated proximal consequences of trauma exposure that in turn increase risk for PTSD and depression. A study of survivors of the 2014 flood in Kashmir Valley, India, for example, found a significant indirect effect of disaster exposure on depression symptoms via declines on family support; the same indirect was non-significant for PTSD symptoms, however [91]. Similarly, greater exposure to the Ya’an earthquake was indirectly associated with higher depression symptoms via lower cognitive social capital, defined as survivors’ sense of community, trust, and social connectedness among a sample of affected adults [40].
Other research within this category has focused on pathways from the cognitive appraisal of environmental disasters to PTSD symptoms. Mordeno, Galela, Nalipay, and Cue [78] gathered data from child and adolescent survivors of the 2011 Tropical Storm Washi in the Philippines and assessed the centrality of the event—that is, whether the storm was perceived as a reference point around which other life events were interpreted, as a core aspect of one’s identity, or a turning point in one’s life. Higher levels of event centrality were linked with higher PTSD symptoms indirectly via stronger sensory-based memories of the storm [78]. Another study assessed posttraumatic cognitive change, defined as increased negative thoughts about one’s safety and stability due to the event, among adolescents after the 2016 Jiangsu tornado [98]. Adolescents who reported more posttraumatic cognitive change tended to have higher PTSD symptoms, an effect that was mediated by both intrusive and deliberate rumination—that is, repeatedly thinking about the disaster either unintentionally or purposefully [98].
Lastly, other work within this category has explored the pathways from social support to PTSD and depression via other risk and protective factors. For example, in a sample of residents living in shelters in Wuhu, China, after a major flood in 2016, higher social support was linked to lower depression symptoms via increases in self disclosure, greater feelings of safety, and fewer negative posttraumatic cognitions [93,94,95]. Social support also had negative indirect effects on depression symptoms through its associations with higher self-esteem and hope among middle school students affected by the 2013 Ya’an earthquake in China [29].
Interventions
Finally, we observed in the past year of research efforts to evaluate interventions to mitigate post-disaster PTSD and depression. Exemplary studies in this category over the past year included investigations of cognitive behavioral therapy for post-disaster stress (CBT-PD) and the Recent Traumatic Events protocol for eye movement desensitization and reprocessing therapy (EMDR R-TEP), which were associated with declines in PTSD symptoms in the aftermath of the 2010 Chile earthquake and the 2012 Northern Italy earthquake, respectively [65, 80]. A further study in this category explored whether interpersonal violence history and severe disaster exposure moderated the effectiveness of Bounce Back Now (BBN), a web-based intervention that provides psychoeducation and evidence-based symptom reduction skill-building for PTSD and depression, as well as cigarette and alcohol use [11]. The investigators found that the impact of BBN on PTSD symptoms was stronger for adolescent participants who had endured severe exposure (defined as having a parent or caregiver who was concerned about the safety or wellbeing of loved ones during the disaster) to the 2011 tornados in Joplin, Missouri, and areas throughout Alabama, relative to those who had not endured severe exposure [11].
An additional notable study in this category combined disaster preparedness training with efforts to address survivors’ mental health symptomology [50••]. This intervention was initially created for survivors of the 2010 Haiti earthquake, but culturally adapted for survivors of a major flood in Nepal in 2015, with consultation from local clinicians and staff from community organizations, and administered in a group format over the course of 3 days. Participation in the intervention was associated with declines in both PTSD and depression symptoms, as well as increased disaster preparedness and a sense of social cohesion. Additionally, path analytic models showed that the intervention had both direct effects on PTSD and depression symptoms and indirect effects via increases in social cohesion. Reports of a subsample of focus group participants further reinforced that the effects of the intervention were socially mediated, with common themes being that the intervention encouraged participants to both seek and provide mental health support to others, and to work collaboratively to solve problems.
Conclusions and Future Research Directions
The results of our review demonstrate the surge in research on the mental health consequences of environmental disaster in recent years. As mentioned previously, the seminal review on this topic by Norris and colleagues published in 2002 identified studies using data from 160 independent samples over the period between 1981 and 2001 [2]. In our review, we identified over 100 articles from 83 independent samples published in the past year alone. Our review was notably not as comprehensive in scope as the aforementioned review, which included studies in the aftermath of mass violence (e.g., terrorism) and a broader range of post-disaster outcomes, among them other specific psychiatric disorders (e.g., generalized anxiety disorder, panic disorder), non-specific psychological distress, sleep disruptions, substance use, and loss of psychosocial resources (e.g., social support, optimism). Further, our review was further limited in our use of only two databases (MEDLINE and PsycINFO), and keyword searches in the articles’ titles rather than their abstracts or full text. Had we broadened our search to replicate the 2002 review, we are certain that the articles identified in a single year would have outnumbered those published over the course of two decades.
The results of our review provide further evidence that exposure to environmental disasters is associated with increased prevalence of PTSD and depression. The studies published in 2018 replicate many of the risk factors for these outcomes that have been documented previously, including female gender, socioeconomic disadvantage, exposure to more disaster-related traumatic events and stressors, and having fewer psychosocial resources. The past year of work is not merely demonstrating again what we know already, however. Researchers are now identifying factors that augment the mental health vulnerability of populations known to be at risk and, in doing so, can help shed light on which survivors might be most in need of post-disaster services. It is also increasingly evident that among those most at risk are persons living in geographic areas that have faced exposure to multiple disasters, suggesting the need for ongoing support to these areas as well as efforts to strengthen their resilience to future hazards. Recent work has also elucidated some of the pathways from trauma exposure and related psychosocial losses to adverse mental health outcome, which could provide important insights for intervention targets. Finally, investigations have shown how adaptations of empirically supported treatments (e.g., CBT and EMDR) for the post-disaster contexts, as well as novel interventions—such as web-based therapies, and group therapies that target social support and disaster preparedness in addition to mental health—could mitigate post-disaster psychiatric adversity.
Future research can expand upon these areas to further our understanding of post-disaster mental health. For example, studies that include longitudinal data, and in particular pre-disaster data, can help elucidate the complex pathways leading to disaster exposure, and from exposure to key mental health outcomes. Post-disaster intervention research can further investigate which components of interventions drive optimal outcomes, and whether results vary by survivor characteristics. Despite not being common among the studies in our review, other recent trends in the disaster mental health literature, such as integration of community-level data on exposure and risk and protective factors, objective indicators of individual-level exposure (vs. self-report), and geospatial techniques [106,107,108,109], are recommended for a more thorough understanding of the range of factors that independently and through interaction drive post-disaster mental health. Similarly, recent work using agent-based modeling has shown the potential of simulating the reach, efficacy, and cost effectiveness of varied post-disaster interventions [110] and could inform how the range of empirically supported interventions are administered on a large scale to disaster-affected populations.
Finally, although the studies reviewed showed the geographic reach of research on mental health after environmental disasters, their geographic locations are far from representative of the areas affected by disasters across the world. For example, we did not identify any work on this topic being done in Africa, despite the occurrence of over 2500 environmental disasters on the continent since the year 2000 [51]. With over 10,000 environmental disasters on record since 2000 [51], it is likely that we are missing the full mental health impact of such events, and perhaps the factors shaping post-disaster symptoms as well. International collaborations could help foster research on disaster-affected areas across the globe. In forming such collaborations, disaster researchers could pool data from various disaster-affected samples for a more in-depth understanding of how various population characteristics, disaster-related exposures, and contextual factors influence post-disaster mental health. Such efforts to characterize, predict, and mitigate PTSD, depression, and other adverse mental health outcomes are of critical importance given the large proportion of the world’s population that are exposed to environmental disasters and the evidence that such events are becoming increasingly common [1].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pachauri RK, Mayer L, Intergovernmental Panel on Climate Change (eds) (2015) Climate change 2014: synthesis report. Intergovernmental Panel on Climate Change, Geneva, Switzerland doi:https://doi.org/10.1017/cbo9781107415416.
Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002;65:207–39. https://doi.org/10.1521/psyc.65.3.207.20173.
Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health. 2014;35:169–83. https://doi.org/10.1146/annurev-publhealth-032013-182435.
Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38:467–80. https://doi.org/10.1017/s0033291707001353.
Geng F, Zhou Y, Liang Y, Fan F. A longitudinal study of recurrent experience of earthquake and mental health problems among Chinese adolescents. Front Psychol. 2018;9. https://doi.org/10.3389/fpsyg.2018.01259.
• Harville EW, Shankar A, Dunkel Schetter C, Lichtveld M. Cumulative effects of the gulf oil spill and other disasters on mental health among reproductive-aged women: the gulf resilience on women’s health study. Psychol Trauma. 2018;10:533–41. https://doi.org/10.1037/tra0000345Article provides a comprehensive summary and rigorous analysis of three competing models of how multiple exposures to traumatic events could influence mental health.
Lee J, Blackmon BJ, Cochran DM, Kar B, Rehner TA, Gunnell MS. Community resilience, psychological resilience, and depressive symptoms: an examination of the Mississippi Gulf coast 10 years after hurricane Katrina and 5 years after the deepwater horizon oil spill. Disaster Med Public Health Prep. 2018;12:241–8. https://doi.org/10.1017/dmp.2017.61.
Lee J, Blackmon BJ, Lee JY, Cochran DM, Rehner TA. An exploration of posttraumatic growth, loneliness, depression, resilience, and social capital among survivors of hurricane Katrina and the deepwater horizon oil spill. J Community Psychol. 2019;47:356–70. https://doi.org/10.1002/jcop.22125.
Prost SG, Appel HB, Ai AL. Coping and post-traumatic stress after hurricanes Katrina and Rita: racial disparities in social work student-practitioners. J Soc Serv Res. 2018;44:459–69. https://doi.org/10.1080/01488376.2018.1476296.
Stough LM, North CS. The association of adverse mental health effects with repeated exposure to disasters. Ann Clin Psychiatry. 2018;30(1):17–24 Retrieved from https://oaktrust.library.tamu.edu/handle/1969.1/166177.
Gilmore AK, Price M, Bountress KE, Zuromski KL, Ruggiero K, Resnick H. A longitudinal examination of interpersonal violence exposure, concern for loved ones during a disaster, and web-based intervention effects on posttraumatic stress disorder among adolescent victims of the spring 2011 tornadoes, 2018. J Interpers Violence 0886260518791236. doi:https://doi.org/10.1177/0886260518791236.
Kannis-Dymand L, Carter JD, Lane BR, Innes P. The relationship of peritraumatic distress and dissociation with beliefs about memory following natural disasters. Aust Psychol. 2018;54:311–21. https://doi.org/10.1111/ap.12377.
Cao C, Wang L, Wu J, Li G, Fang R, Cao X, et al. Patterns of posttraumatic stress disorder symptoms and posttraumatic growth in an epidemiological sample of Chinese earthquake survivors. Front Psychol. 2018;9:1549. https://doi.org/10.3389/fpsyg.2018.01549.
Yeung NCY, Lau JTF, Yu NX, Zhang J, Xu Z, Choi KC, et al. Media exposure related to the 2008 Sichuan earthquake predicted probable PTSD among Chinese adolescents in Kunming, China: a longitudinal study. Psychol Trauma. 2018;10:253–62. https://doi.org/10.1037/tra0000121.
Cao X, Wang L, Cao C, Zhang J, Elhai JD. PTSD latent classes and class transitions predicted by distress and fear disorders in disaster-exposed adolescents. J Clin Child Adolesc Psychol. 2018;0:1–11. https://doi.org/10.1080/15374416.2017.1410825.
Cheng J, Liang Y, Fu L, Liu Z. Posttraumatic stress and depressive symptoms in children after the Wenchuan earthquake. Eur J Psychotraumatol. 2018;9:1472992. https://doi.org/10.1080/20008198.2018.1472992.
Du B, Ma X, Ou X, Jin Y, Ren P, Li J. The prevalence of posttraumatic stress in adolescents eight years after the Wenchuan earthquake. Psychiatry Res. 2018;262:262–9. https://doi.org/10.1016/j.psychres.2018.02.019.
Fan M, Cao T, Feng Y, Su M, Lin J, Ran MS, et al. D allele of insertion/deletion polymorphism at angiotensin-converting enzyme gene is associated with reduced prevalence and severity of depression among Chinese adolescents at early stage after Wenchuan earthquake. Int J Psychiatry Clin Pract. 2018;22:136–42. https://doi.org/10.1080/13651501.2017.1383440.
Feng Y, Su M, Si YJ, Guo QW, Lin J, Cao T, et al. Longitudinal interplays of estrogen receptor alpha gene rs9340799 with social-environmental factors on post-traumatic stress disorder in Chinese Han adolescents after Wenchuan earthquake. Am J Med Genet B Neuropsychiatr Genet. 2018;177:337–45. https://doi.org/10.1002/ajmg.b.32615.
Memon NH, Fan M, Lin J, Si YJ, Su M, Guo QW, et al. Reduced recovery of depression in female T allele carriers of TNF-RII rs1061622 at earlier stage after Wenchuan earthquake. Int J Environ Res Public Health. 2018;15:1075. https://doi.org/10.3390/ijerph15061075.
Geng F, Liang Y, Shi X, Fan F. A prospective study of psychiatric symptoms among adolescents after the Wenchuan earthquake. J Trauma Stress. 2018;31:499–508. https://doi.org/10.1002/jts.22307.
Geng F, Zhou Y, Liang Y, Zheng X, Li Y, Chen X, et al. Posttraumatic stress disorder and psychiatric comorbidity among adolescent earthquake survivors: a longitudinal cohort study. J Abnorm Child Psychol. 2018;47:671–81. https://doi.org/10.1007/s10802-018-0462-2.
Shi X, Zhou Y, Geng F, Li Y, Zhou J, Lei B, et al. Posttraumatic stress disorder symptoms in parents and adolescents after the Wenchuan earthquake: a longitudinal actor-partner interdependence model. J Affect Disord. 2018;226:301–6. https://doi.org/10.1016/j.jad.2017.10.011.
Guo J, Liu C, Kong D, Solomon P, Fu M. The relationship between PTSD and suicidality among Wenchuan earthquake survivors: the role of PTG and social support. J Affect Disord. 2018;235:90–5. https://doi.org/10.1016/j.jad.2018.04.030.
He L, Lai K, Lin Z, Ma Z. Media exposure and general trust as predictors of post-traumatic stress disorder: ten years after the 5.12 Wenchuan earthquake in China. Int J Environ Res Public Health. 2018;15:2386. https://doi.org/10.3390/ijerph15112386.
Hu T, Xu S, Liu W. A senior high school-based survey on the long-term impact of the Wenchuan earthquake on survivors’ quality of life: PTSD as a mediator. Psychiatry Res. 2018;270:310–6. https://doi.org/10.1016/j.psychres.2018.09.043.
Liu L, Wang L, Cao C, Cao X, Zhu Y, Liu P, et al. Serotonin transporter 5-HTTLPR genotype is associated with intrusion and avoidance symptoms of DSM-5 posttraumatic stress disorder (PTSD) in Chinese earthquake survivors. Anxiety Stress Coping. 2018;31:318–27. https://doi.org/10.1080/10615806.2017.1420174.
Zhang X, Zhang J, Wang L, Zhang W. Altered gray matter volume and its correlation with ptsd severity in Chinese earthquake survivors. Front Psychiatry. 2018;9. https://doi.org/10.3389/fpsyt.2018.00629.
Zhou X, Wu X, Zhen R. Patterns of posttraumatic stress disorder and posttraumatic growth among adolescents after the Wenchuan earthquake in China: a latent profile analysis. J Trauma Stress. 2018;31:57–63. https://doi.org/10.1002/jts.22246.
Zhou X, Wu X, Zhen R, Wang W, Tian Y. Trajectories of posttraumatic stress disorders among adolescents in the area worst-hit by the Wenchuan earthquake. J Affect Disord. 2018;235:303–7. https://doi.org/10.1016/j.jad.2018.04.032.
Jin Y, Deng H, An J, Xu J. The prevalence of PTSD symptoms and depressive symptoms and related predictors in children and adolescents 3 years after the Ya’an earthquake. Child Psychiatry Hum Dev. 2018;50:300–7. https://doi.org/10.1007/s10578-018-0840-6.
Jin Y, Sun C, Wang F, An J, Xu J. The relationship between PTSD, depression and negative life events: Ya’an earthquake three years later. Psychiatry Res. 2018;259:358–63. https://doi.org/10.1016/j.psychres.2017.09.017.
Tang W, Lu Y, Xu J. Post-traumatic stress disorder, anxiety and depression symptoms among adolescent earthquake victims: comorbidity and associated sleep-disturbing factors. Soc Psychiatry Psychiatr Epidemiol. 2018;53:1241–51. https://doi.org/10.1007/s00127-018-1576-0.
Tang W, Xu D, Li B, Lu Y, Xu J. The relationship between the frequency of suicidal ideation and sleep disturbance factors among adolescent earthquake victims in China. Gen Hosp Psychiatry. 2018;55:90–7. https://doi.org/10.1016/j.genhosppsych.2018.09.013.
Tang W, Zhao J, Lu Y, Zha Y, Liu H, Sun Y, et al. Suicidality, posttraumatic stress, and depressive reactions after earthquake and maltreatment: a cross-sectional survey of a random sample of 6132 Chinese children and adolescents. J Affect Disord. 2018;232:363–9. https://doi.org/10.1016/j.jad.2018.02.081.
Tang W, Lu Y, Yang Y, Xu J. An epidemiologic study of self-reported sleep problems in a large sample of adolescent earthquake survivors: the effects of age, gender, exposure, and psychopathology. J Psychosom Res. 2018;113:22–9. https://doi.org/10.1016/j.jpsychores.2018.07.006.
Xu J, Wang Y, Tang W. Risk factors of post-traumatic stress and depressive disorders in Longmenshan adolescents after the 2013 Lushan earthquake. Community Ment Health J. 2018;55:497–506. https://doi.org/10.1007/s10597-018-0256-6.
Xu J, Wang Y, Tang W. Posttraumatic stress disorder in Longmenshan adolescents at three years after the 2013 Lushan earthquake. Gen Hosp Psychiatry. 2018;54:45–51. https://doi.org/10.1016/j.genhosppsych.2018.05.009.
Wang W, Wu X, Tian Y. Mediating roles of gratitude and social support in the relation between survivor guilt and posttraumatic stress disorder, posttraumatic growth among adolescents after the Ya’an earthquake. Front Psychol. 2018;9. https://doi.org/10.3389/fpsyg.2018.02131.
Wong H, Huang Y, Fu Y, Zhang Y. Impacts of structural social capital and cognitive social capital on the psychological status of survivors of the Yaan earthquake. Appl Res Qual Life. 2018. https://doi.org/10.1007/s11482-018-9661-9.
Zhou X, Wu X, Zhen R. Self-esteem and hope mediate the relations between social support and post-traumatic stress disorder and growth in adolescents following the Ya’an earthquake. Anxiety Stress Coping. 2018;31:32–45. https://doi.org/10.1080/10615806.2017.1374376.
Acharya S, Bhatta DN, Assannangkornchai S. Post-traumatic stress disorder symptoms among children of Kathmandu 1 year after the 2015 earthquake in Nepal. Disaster Med Public Health Prep. 2018;12:486–92. https://doi.org/10.1017/dmp.2017.100.
Itzhaky H, Weiss-Dagan S, Taubman-Ben-Ari O. Internal and community recourses’ contribution to level of posttraumatic symptoms—the case of tourists after the earthquake in Nepal, 2015. Psychol Trauma. 2018;10:239–45. https://doi.org/10.1037/tra0000280.
Kane JC, Luitel NP, Jordans MJD, Kohrt BA, Weissbecker I, Tol WA. Mental health and psychosocial problems in the aftermath of the Nepal earthquakes: findings from a representative cluster sample survey. Epidemiol Psychiatr Sci. 2018;27:301–10. https://doi.org/10.1017/s2045796016001104.
Negi BS, Joshi SK, Nakazawa M, Kotaki T, Bastola A, Kameoka M. Impact of a massive earthquake on adherence to antiretroviral therapy, mental health, and treatment failure among people living with HIV in Nepal. PLoS One. 2018;13:e019807. https://doi.org/10.1371/journal.pone.0198071.
Schwind JS, Formby CB, Santangelo SL, Norman SA, Brown R, Hoffman Frances R, et al. Earthquake exposures and mental health outcomes in children and adolescents from Phulpingdanda village, Nepal: a cross-sectional study. Child Adolesc Psychiatry Ment Health. 2018;12:54. https://doi.org/10.1186/s13034-018-0257-9.
Sharma A, Kar N. Posttraumatic stress, depression, and coping following the 2015 Nepal earthquake: a study on adolescents. Disaster Med Public Health Prep, 2018; 1–7. doi:https://doi.org/10.1017/dmp.2018.37.
Silwal S, Dybdahl R, Chudal R, Sourander A, Lien L. Psychiatric symptoms experienced by adolescents in Nepal following the 2015 earthquakes. J Affect Disord. 2018;234:239–46. https://doi.org/10.1016/j.jad.2018.03.002.
Thapa P, Acharya L, Bhatta BD, Paneru SB, Khattri JB, Chakraborty PK, et al. Anxiety, depression and post-traumatic stress disorder after earthquake. J Nepal Health Res Counc. 2018;16:53–7. https://doi.org/10.3126/jnhrc.v16i1.19366.
•• Welton-Mitchell C, James LE, Khanal SN, James AS. An integrated approach to mental health and disaster preparedness: a cluster comparison with earthquake affected communities in Nepal. BMC Psychiatry. 2018;18:296. https://doi.org/10.1186/s12888-018-1863-zArticle represents a major effort to examine a post-disaster intervention, culturally adapted group treatment aimed at reducing symptoms and building psychosocial resources.
The international disasters database (EM-DAT) 2019. Retrieved from https://www.emdat.be.
Bolt MA, Helming LM, Tintle NL. The associations between Self-reported exposure to the Chernobyl nuclear disaster zone and mental health disorders in Ukraine. Front Psychiatry. 2018;9. https://doi.org/10.3389/fpsyt.2018.00032.
Goenjian AK, Khachadourian V, Armenian H, Demirchyan A, Steinberg AM. Posttraumatic stress disorder 23 years after the 1988 Spitak earthquake in Armenia. J Trauma Stress. 2018;31:47–56. https://doi.org/10.1002/jts.22260.
Adebäck P, Schulman A, Nilsson D. Children exposed to a natural disaster: psychological consequences eight years after 2004 tsunami. Nord J Psychiatry. 2018;72:75–8. https://doi.org/10.1080/08039488.2017.1382569.
Bondjers K, Willebrand M, Arnberg FK. Similarity in symptom patterns of posttraumatic stress among disaster-survivors: a three-step latent profile analysis. Eur J Psychotraumatol. 2018;9:1546083. https://doi.org/10.1080/20008198.2018.1546083.
Gudmundsdottir R, Hultman CM, Valdimarsdottir U. Evacuation of Swedish survivors after the 2004 southeast Asian tsunami: the survivors’ perspective and symptoms of post-traumatic stress. Scand J Public Health. 2018;1403494818771418:260–8. https://doi.org/10.1177/1403494818771418.
Sveen J, Johannesson KB, Cernvall M, Arnberg FK. Trajectories of prolonged grief one to six years after a natural disaster. PLoS One. 2018;13:e0209757. https://doi.org/10.1371/journal.pone.0209757.
Lai BS, Osborne MC, Piscitello J, Self-Brown S, Kelley ML. The relationship between social support and posttraumatic stress symptoms among youth exposed to a natural disaster. Eur J Psychotraumatol. 2018;9:1450042. https://doi.org/10.1080/20008198.2018.1450042.
Lai BS, Osborne MC, Lee N, Self-Brown S, Esnard A-M, Kelley ML. Trauma-informed schools: child disaster exposure, community violence and somatic symptoms. J Affect Disord. 2018;238:586–92. https://doi.org/10.1016/j.jad.2018.05.062.
• Lenane Z, Peacock E, Joyce C, Frohlich ED, Re RN, Muntner P, et al. Association of post-traumatic stress disorder symptoms following hurricane Katrina with incident cardiovascular disease events among older adults with hypertension. Am J Geriatr Psychiatry. 2018. https://doi.org/10.1016/j.jagp.2018.11.006Article representative of trend in research investigating post-disaster mental health among high-risk populations, and that links mental and physical health outcomes.
McGuire AP, Gauthier JM, Anderson LM, Hollingsworth DW, Tracy M, Galea S, et al. Social support moderates effects of natural disaster exposure on depression and posttraumatic stress disorder symptoms: effects for displaced and nondisplaced residents. J Trauma Stress. 2018;31:223–33. https://doi.org/10.1002/jts.22270.
Mikolajewski AJ, Scheeringa MS. Examining the prospective relationship between pre-disaster respiratory sinus arrhythmia and post-disaster posttraumatic stress disorder symptoms in children. J Abnorm Child Psychol. 2018;46:1535–45. https://doi.org/10.1007/s10802-017-0396-0.
Psarros C, Theleritis C, Kokras N, Lyrakos D, Koborozos A, Kakabakou O, et al. Personality characteristics and individual factors associated with PTSD in firefighters one month after extended wildfires. Nord J Psychiatry. 2018;72:17–23. https://doi.org/10.1080/08039488.2017.1368703.
Thordardottir EB, Gudmundsdottir H, Gudmundsdottir B, Hrólfsdóttir AM, Aspelund T, Hauksdottir A. Development and predictors of psychological outcomes following the 2008 earthquake in Iceland: a longitudinal cohort study. Scand J Public Health. 2018;47:269–79. https://doi.org/10.1177/1403494818771444.
Leiva-Bianchi M, Cornejo F, Fresno A, Rojas C, Serrano C. Effectiveness of cognitive-behavioural therapy for post-disaster distress in post-traumatic stress symptoms after Chilean earthquake and tsunami. Gac Sanit. 2018;32:291–6. https://doi.org/10.1016/j.gaceta.2017.07.018.
Rosellini AJ, Dussaillant F, Zubizarreta JR, Kessler RC, Rose S. Predicting posttraumatic stress disorder following a natural disaster. J Psychiatr Res. 2018;96:15–22. https://doi.org/10.1016/j.jpsychires.2017.09.010.
Gissurardóttir ÓS, Hlodversdóttir H, Thordardóttir EB, Pétursdóttir G, Hauksdóttir A. Mental health effects following the eruption in Eyjafjallajökull volcano in Iceland: a population-based study. Scand J Public Health. 2018;47:1403494817751327–259. https://doi.org/10.1177/1403494817751327.
Trip H, Tabakakis K, Maskill V, Richardson S, Dolan B, Josland H, et al. Psychological health and resilience: the impact of significant earthquake events on tertiary level professional students. A cross-sectional study. Contemp Nurse. 2018;54:319–32. https://doi.org/10.1080/10376178.2018.1503549.
Xiao Y, Liu D, Liu K, Jiang X. Post-traumatic stress disorder and its risk factors in bereaved Tibetan adolescents 3 years after the 2010 Yushu earthquake, a cross-sectional study in China. Arch Psychiatr Nurs. 2018;33:149–54. https://doi.org/10.1016/j.apnu.2018.11.010.
Ayer L, Engel C, Parker A, Seelam R, Ramchand R. Behavioral health of Gulf Coast residents 6 years after the deepwater horizon oil spill: the role of trauma history. Disaster Med Public Health Prep 1–7, 2018. doi:https://doi.org/10.1017/dmp.2018.84.
Buckingham-Howes S, Holmes K, Glenn Morris J, Grattan LM. Prolonged financial distress after the deepwater horizon oil spill predicts behavioral health. J Behav Health Serv Res. 2018;46:294–305. https://doi.org/10.1007/s11414-018-9602-2.
Rung AL, Oral E, Fontham E, Harrington DJ, Trapido EJ, Peters ES. The long-term effects of the Deepwater horizon oil spill on women’s depression and mental distress. Disaster Med Public Health Prep 1–8, 2018. doi:https://doi.org/10.1017/dmp.2018.14.
Kildea S, Simcock G, Liu A, Elgbeili G, Laplante DP, Kahler A, et al. Continuity of midwifery carer moderates the effects of prenatal maternal stress on postnatal maternal wellbeing: the Queensland flood study. Arch Womens Ment Health. 2018;21:203–14. https://doi.org/10.1007/s00737-017-0781-2.
•• Nagamine M, Yamamoto T, Shigemura J, et al. The psychological impact of the Great East Japan earthquake on Japan ground self-defense force personnel: a three-wave, one-year longitudinal study. Psychiatry. 2018;81:288–96. https://doi.org/10.1080/00332747.2017.1333340Exemplary study focused on a high-risk population of over 50,000 first responders after the 2011 Great East Japan earthquake, tsunami, and nuclear disaster.
Okuyama J, Funakoshi S, Tomita H, Yamaguchi T, Matsuoka H. Longitudinal characteristics of resilience among adolescents: a high school student cohort study to assess the psychological impact of the Great East Japan earthquake. Psychiatry Clin Neurosci. 2018;72:821–35. https://doi.org/10.1111/pcn.12772.
Shigemura J, Someda H, Tokuno S, Nagamine M, Tanichi M, Araki Y, et al. Disaster victim identification: psychological distress and posttraumatic stress in dentists after the 2011 Fukushima disaster. Psychiatry. 2018;81:85–92. https://doi.org/10.1080/00332747.2017.1297667.
Takaoka K, Niitsu T, Suzuki S, Kono A, Nakazato M, Shimizu E. The association of posttraumatic stress disorder risk with help-seeking behavior: a cross-sectional study of earthquake and tsunami survivors in Japan. Traumatology. 2018;24:123–30. https://doi.org/10.1037/trm0000138.
Mordeno IG, Galela DS, Nalipay MJN, Cue MP. Centrality of event and mental health outcomes in child and adolescent natural disaster survivors. Spanish J Psychol. 2018;21:E61. https://doi.org/10.1017/sjp.2018.58.
Salcioglu E, Ozden S, Ari F. The role of relocation patterns and psychosocial stressors in posttraumatic stress disorder and depression among earthquake survivors. J Nerv Ment Dis. 2018;206:19–26. https://doi.org/10.1097/nmd.0000000000000627.
Saltini A, Rebecchi D, Callerame C, Fernandez I, Bergonzini E, Starace F. Early eye movement desensitisation and reprocessing (EMDR) intervention in a disaster mental health care context. Psychol Health Med. 2018;23:285–94. https://doi.org/10.1080/13548506.2017.1344255.
Song JY, Jeong K-S, Choi K, Kim M, Ahn Y-S. Psychological risk factors for posttraumatic stress disorder in workers after toxic chemical spill in Gumi, South Korea. Workplace Health Saf. 2018;66:393–402. https://doi.org/10.1177/2165079917750168.
Vezzali L, Versari A, Cadamuro A, Trifiletti E, Bernardo GAD. Out-group threats and distress as antecedents of common in-group identity among majority and minority group members in the aftermath of a natural disaster. Int J Psychol. 2018;53:417–25. https://doi.org/10.1002/ijop.12406.
Li J, Alper HE, Gargano LM, Maslow CB, Brackbill RM. Re-experiencing 9/11-related ptsd symptoms following exposure to hurricane Sandy. Int J Emerg Ment Health. 2018;20. https://doi.org/10.4172/1522-4821.1000404.
Mandavia AD, Bonanno GA. When natural disaster follows economic downturn: the incremental impact of multiple stressor events on trajectories of depression and posttraumatic stress disorder. Disaster Med Public Health Prep, 2018 1–10. doi:https://doi.org/10.1017/dmp.2018.12.
Ruskin J, Rasul R, Schneider S, Bevilacqua K, Taioli E, Schwartz RM. Lack of access to medical care during hurricane Sandy and mental health symptoms. Prev Med Rep. 2018;10:363–9. https://doi.org/10.1016/j.pmedr.2018.04.014.
Schneider S, Rasul R, Liu B, Corry D, Lieberman-Cribbin W, Watson A, et al. Examining posttraumatic growth and mental health difficulties in the aftermath of hurricane Sandy. Psychol Trauma. 2019;11:127–36. https://doi.org/10.1037/tra0000400.
Schwartz RM, Rasul R, Kerath SM, Watson AR, Lieberman-Cribbin W, Liu B, et al. Displacement during hurricane Sandy: the impact on mental health. J Emerg Manag. 2018;16:17–27. https://doi.org/10.5055/jem.2018.0350.
Hetherington E, McDonald S, Wu M, Tough S. Risk and protective factors for mental health and community cohesion after the 2013 Calgary flood. Disaster Med Public Health Prep. 2018;12:470–7. https://doi.org/10.1017/dmp.2017.91.
Labarda CE, Chan CS. Sleep disturbances, posttraumatic stress, and psychological distress among survivors of the 2013 super typhoon Haiyan. Psychiatry Res. 2018;266:284–90. https://doi.org/10.1016/j.psychres.2018.03.019.
Nagamine M, Shigemura J, Fujiwara T, Waki F, Tanichi M, Saito T, et al. The relationship between dispositional empathy, psychological distress, and posttraumatic stress responses among Japanese uniformed disaster workers: a cross-sectional study. BMC Psychiatry. 2018;18:328. https://doi.org/10.1186/s12888-018-1915-4.
Dar KA, Iqbal N, Prakash A, Paul MA. PTSD and depression in adult survivors of flood fury in Kashmir: the payoffs of social support. Psychiatry Res. 2018;261:449–55. https://doi.org/10.1016/j.psychres.2018.01.023.
Salgado Roa JA, Leria Dulčić FJ, Salgado Roa JA, Leria Dulčić FJ. Coping strategies for stress and pathological symptoms in university students in the face of a mudslide disaster. Acta Colombiana de Psicología. 2018;21:170–95. https://doi.org/10.14718/acp.2018.21.1.8.
Zhen R, Quan L, Zhou X. Fear, negative cognition, and depression mediate the relationship between traumatic exposure and sleep problems among flood victims in China. Psychol Trauma. 2018;10:602–9. https://doi.org/10.1037/tra0000331.
Zhen R, Quan L, Zhou X. How does social support relieve depression among flood victims? The contribution of feelings of safety, self-disclosure, and negative cognition. J Affect Disord. 2018;229:186–92. https://doi.org/10.1016/j.jad.2017.12.087.
Zhen R, Quan L, Zhou X. Co-occurring patterns of post-traumatic stress disorder and depression among flood victims: a latent profile analysis. J Health Psychol. 2018:135910531876350. https://doi.org/10.1177/1359105318763505.
An Y, Yuan G, Liu Z, Zhou Y, Xu W. Dispositional mindfulness mediates the relationships of parental attachment to posttraumatic stress disorder and academic burnout in adolescents following the Yancheng tornado. Eur J Psychotraumatol. 2018;9:1472989. https://doi.org/10.1080/20008198.2018.1472989.
An Y, Yuan G, Zhang N, Xu W, Liu Z, Zhou F. Longitudinal cross-lagged relationships between mindfulness, posttraumatic stress symptoms, and posttraumatic growth in adolescents following the Yancheng tornado in China. Psychiatry Res. 2018;266:334–40. https://doi.org/10.1016/j.psychres.2018.03.034.
Zhang Y, Xu W, Yuan G, An Y. The relationship between posttraumatic cognitive change, posttraumatic stress disorder, and posttraumatic growth among Chinese adolescents after the Yancheng tornado: the mediating effect of rumination. Front Psychol. 2018;9. https://doi.org/10.3389/fpsyg.2018.00474.
Xu W, Ding X, Goh PH, An Y. Dispositional mindfulness moderates the relationship between depression and posttraumatic growth in Chinese adolescents following a tornado. Pers Individ Dif. 2018;127:15–21. https://doi.org/10.1016/j.paid.2018.01.032.
Xu W, Yuan G, Liu Z, Zhou Y, An Y. Prevalence and predictors of PTSD and depression among adolescent victims of the summer 2016 tornado in Yancheng City. Arch Psychiatr Nurs. 2018;32:777–81. https://doi.org/10.1016/j.apnu.2018.04.010.
Yuan G, Xu W, Liu Z, An Y. Resilience, posttraumatic stress symptoms, and posttraumatic growth in Chinese adolescents after a tornado: the role of mediation through perceived social support. J Nerv Ment Dis. 2018;206:130–5. https://doi.org/10.1097/nmd.0000000000000778.
McElroy-Heltzel SE, Davis EB, Davis DE, Aten JD, Hook JN, Van Tongeren DR, et al. Benevolent theodicies protect against PTSD following a natural disaster. J Psychol Christ. 2018;37:6–16 Retrieved from http://eds.a.ebscohost.com/eds/.
Contreras C, Aguilar M, Eappen B, Guzmán C, Carrasco P, Millones AK, et al. Community strengthening and mental health system linking after flooding in two informal human settlements in Peru: a model for small-scale disaster response. Glob Ment Health. 2018;5. https://doi.org/10.1017/gmh.2017.33.
Ferré IM, Negrón S, Shultz JM, Schwartz SJ, Kossin JP, Pantin H. Hurricane Maria’s impact on Punta Santiago, Puerto Rico: community needs and mental health assessment six months postimpact, Disaster Med Public Health Prep, 2018; 1–6. doi:https://doi.org/10.1017/dmp.2018.103.
Schwartz RM, Tuminello S, Kerath SM, Rios J, Lieberman-Cribbin W, Taioli E. Preliminary assessment of hurricane Harvey exposures and mental health impact. Int J Environ Res Public Health. 2018;15:974. https://doi.org/10.3390/ijerph15050974.
Hikichi H, Aida J, Tsuboya T, Kondo K, Kawachi I. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 Tohoku earthquake and tsunami. Am J Epidemiol. 2016;183:902–10. https://doi.org/10.1093/aje/kwv335.
Matsuyama Y, Aida J, Hase A, Sato Y, Koyama S, Tsuboya T, et al. Do community- and individual-level social relationships contribute to the mental health of disaster survivors?: a multilevel prospective study after the Great East Japan earthquake. Soc Sci Med. 2016;151:187–95. https://doi.org/10.1016/j.socscimed.2016.01.008.
Gruebner O, Lowe SR, Sampson L, Galea S. The geography of post-disaster mental health: spatial patterning of psychological vulnerability and resilience factors in New York City after hurricane Sandy. Int J Health Geogr. 2015;14:16. https://doi.org/10.1186/s12942-015-0008-6.
Kwok RK, McGrath JA, Lowe SR, Engel LS, Jackson WB, Curry MD, et al. Mental health indicators associated with oil spill response and clean-up: cross-sectional analysis of the GuLF STUDY cohort. Lancet Public Health. 2017;2:e560–7. https://doi.org/10.1016/S2468-2667(17)30194-9.
Cohen GH, Tamrakar S, Lowe S, Sampson L, Ettman C, Linas B, et al. Comparison of simulated treatment and cost-effectiveness of a stepped care case-finding intervention vs usual care for posttraumatic stress disorder after a natural disaster. JAMA Psychiatry. 2017;74:1251–8. https://doi.org/10.1001/jamapsychiatry.2017.3037.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Environmental Disaster
Rights and permissions
About this article
Cite this article
Lowe, S.R., Bonumwezi, J.L., Valdespino-Hayden, Z. et al. Posttraumatic Stress and Depression in the Aftermath of Environmental Disasters: A Review of Quantitative Studies Published in 2018. Curr Envir Health Rpt 6, 344–360 (2019). https://doi.org/10.1007/s40572-019-00245-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-019-00245-5