Abstract
Purpose of Review
I review literature on the impacts of climate change on air quality and human health, with a focus on articles published from 2013 on ozone and airborne particles. Selected previous literature is discussed where relevant in tracing the origins of our current knowledge.
Recent Findings
Climate and weather have strong influences on the spatial and temporal distribution of air pollution concentrations. Emissions of ozone and PM2.5 precursors increase at higher ambient temperatures. The reactions that form ozone occur faster with greater sunlight and higher temperatures. Weather systems influence the movement and dispersion of air pollutants in the atmosphere through the action of winds, vertical mixing, and precipitation, all of which are likely to alter in a changing climate. Recent studies indicate that, holding anthropogenic air pollution emissions constant, ozone concentrations in populated regions will tend to increase in future climate scenarios. For the USA, the climate impact on ozone is most consistently seen in north-central and north-eastern states, with the potential for many thousands of additional ozone-related deaths. The sensitivity of anthropogenic PM2.5 to climate is more variable across studies and regions, owing to the varied nature of PM constituents, as well as to less complete characterization of PM reaction chemistry in available atmospheric models. However, PM emitted by wildland fires is likely to become an increasing health risk in many parts of the world as climate continues to change.
Summary
The complex interactions between climate change and air quality imply that future policies to mitigate these twin challenges will benefit from greater coordination. Assessing the health implications of alternative policy approaches towards climate and pollution mitigation will be a critical area of future work.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Climate change and air pollution are two major global challenges, the causes and solutions of which are closely linked. Human-induced changes to the global climate system are driven largely by the burning of fossil fuels (emitting carbon dioxide, black carbon, and ozone precursors) and agricultural production (emitting methane). Adverse health effects from air pollution result from fossil fuel combustion and other atmospheric waste streams, including agricultural emissions of methane and ammonia. In addition, weather patterns have strong influences on the spatial and temporal distribution of air pollution concentrations through a variety of processes that affect the degree to which air pollutants remain concentrated near their sources, are dispersed and diluted, are chemically transformed, are transported long distances, and/or are ultimately removed through dry or wet deposition [1]. In addition to pollutants emitted by human activities, naturally occurring “air pollutants” that have adverse effects on human health, such as pollen, VOCs from trees, smoke from wildfires, and windblown dust, can be influenced by climate [2]. Because of the multiple interconnections via emissions and atmospheric processes, it is highly likely that climate change will have an influence on air pollution levels and resulting health impacts. At the same time, policy responses to mitigate climate change could bring enormous human health benefits [3].
Both ozone and PM2.5 are affected by climate, but in somewhat different ways. Ozone is created in the lower atmosphere through reactions of precursor pollutants in the presence of sunlight. Higher temperatures favor more rapid formation of ozone. Also, emissions of ozone precursors can increase at higher temperatures, promoting higher ozone concentrations. The two key precursor pollutants for ozone formation are nitrogen oxides (NOx) (emitted mainly by burning of fossil fuels) and volatile organic compounds (VOCs) (emitted both by burning of fuels and evaporation from vegetation and stored fuels). Emissions of both anthropogenic and biogenic VOCs increase with temperature. NOx emissions can also increase with temperature, due to increased fossil fuel combustion for electricity generation during heat waves. Because the reactions that form ozone happen faster with greater sunlight and higher temperatures, ozone concentrations reach their highest levels during warm weather, especially in summer. However, increasing global emissions of methane, the most common VOC, have led in recent decades to rising background levels of ozone throughout the year [1]. Major anthropogenic methane sources include fossil fuel production and use, and livestock productions. The health implications of background ozone levels remain uncertain but could be significant given the large numbers of people exposed.
In contrast to ozone, which is a simple gas, PM2.5 consists of a complex mixture of airborne particles, solid or liquid, that are less than 2.5 μm in aerodynamic diameter. Upon inhalation, particles of these small sizes are able to make it past the defenses of our nose and upper airways, potentially depositing deep in the lung, where tissues are more vulnerable, as well as penetrating and being transported by the bloodstream to other sensitive organs. PM2.5 is emitted from a great variety of sources and can also be formed through atmospheric reactions of precursor gases, including SO2, NO2, and VOCs. Key sources of PM2.5 include motor vehicles (especially diesel powered), power plants, heating systems for buildings, wildfires, and, in arid regions, wind-blown dust [4]. Because of their small size, PM2.5 particles can remain airborne for days after being emitted or formed in the atmosphere and may be carried long distances from their source regions [4, 5]. Power plant emissions of PM2.5 and its precursor gases can rise during heat waves. Also, atmospheric reactions that convert SO2 to sulfate particles occur more rapidly as temperatures rise. On the other hand, other PM2.5 components, such as nitrates and organics, can volatilize at higher temperatures, reducing PM2.5 concentrations (although those pollutants simply move to the gas phase, still with potential health impacts).
Both ozone and PM2.5 concentrations are influenced by weather systems that can be altered in a changing climate [1]. The movement and dispersion of air pollutants in the atmosphere are affected by the action of winds, vertical mixing, and rainfall. The mixing height of the lower atmosphere controls dilution of pollution near the Earth’s surface and thus affects the concentrations humans experience at the surface. Low mixing heights lead to higher surface concentrations. Stagnant winds, which occur with high pressure weather systems, limit the horizontal dispersion of pollutants and lead to higher concentrations. Climate change models have shown alterations in both mixing height and stagnating high pressure systems that could affect air pollution concentrations in either direction [1].
The remainder of this paper reviews literature addressing the interplay of climate change, air quality, and human health that has emerged mainly in the past 5 years, i.e., from 2013 to 2017. Initial papers were identified by searching the Web of Science database for papers published 2013 or later with titles that included either “air pollution” or “air quality” AND “climate change” AND also included the word “health” as a major topic. Eighty-nine papers were identified in July 2017. Other papers were added when citations pointed to relevant literature. Selected earlier literature was reviewed where relevant in tracing the origins of our current knowledge. We focus largely on the anthropogenic air pollutants fine particulate matter (“PM2.5”) and ozone, because together, they are thought to be responsible for most of the current burden of disease from ambient air pollution [6].
Climate, Air Pollution, and Health Impact Assessment Methodology and Inputs
Assessments of the potential future health effects of air pollution due to climate change are typically carried out using methods of risk assessment. Climate risk assessment requires four inputs: the number of people at risk (i.e. the population within a given region), the baseline rate of the health outcome in the population (e.g. the number of deaths per year per 100,000 persons), the concentration-response function (CRF) (i.e. the fractional change in the rate of the health outcome per unit change in air pollution), and the air pollution concentration that is projected to occur in the future climate (e.g. the annual mean PM2.5 concentration in 2050 assuming climate has changed). Baseline mortality and/or morbidity rates are taken from government sources (e.g. CDC Wonder) and are assumed to remain constant over time. CRFs are derived from the epidemiologic literature, ideally from the same country or region for which the future climate assessment is being carried out. Like baseline rates, CRFs are assumed to be constant in time. Population counts, e.g., obtained from the decadal census, usually are held constant at current levels but can be allowed to grow and/or age in the future based on demographic models.
To estimate air pollution in a future climate scenario, complex atmospheric models are run which simulate the dispersion and transformation of air pollution in response to future simulated climate as well as emissions of air pollution precursors. This is where things get complicated, as there are dozens of global climate models that could be used, as well as several different global and/or regional air pollution simulation models that can be run in conjunction with the climate model. Each set of models generates somewhat different results, even with the same inputs [7]. There are numerous analytical decisions that are made in the process of modeling that can affect the outcomes, including pollution and greenhouse gas emission trajectories, time periods, spatial scales, and model versions that differ in how climate or chemistry processes are parameterized.
An essential input to the climate models is the future trajectory of assumed greenhouse pollutant emissions that may cause changes in future temperature, precipitation, cloud cover, atmospheric circulation patterns, etc. In 2000, the Intergovernmental Panel on Climate Change (IPCC) published a set of consensus scenarios of future greenhouse gas emissions in their Special Report on Emission Scenarios [8] (these are called the SRES scenarios). More recently, IPCC adopted a different set of scenarios that are defined in terms of radiative forcing, which is the difference, in W/m2, between incoming and outgoing electromagnetic radiation at the Earth’s surface. These new scenarios are called representative concentration pathways or RCPs [9]. Most of the recent literature has used the RCP scenarios, which were developed in support of the fifth assessment report of the Intergovernmental Panel on Climate Change. The four RCPs are 2.0, 4.5, 6.0, and 8.5, with the numbers referring to progressively higher global average radiative forcing in W/m2 (that is, the solar energy that is being absorbed by the earth) and thus greater climate warming. Most recent climate-air pollution-health assessment studies include a low to medium RCP (2.0 or 4.5) and a high RCP (8.5) to illustrate the range of impacts across the span of potential future climate change.
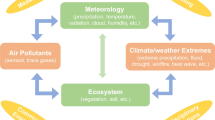
Another important consideration in the modeling of air pollution concentrations in a changing climate is that of spatial scale. Global models, which are needed to capture the climate change influence on future air pollution across the entire Earth, are necessarily coarse in their spatial resolution, with outputs averaged over grids that are 100 s of kilometers on a side. This is too coarse to assess concentration gradients over urban areas where population impacts would be greatest. Thus, most studies carry out a further step to “downscale” the future air pollution estimates to geographical units that are more relevant for understanding urban health impacts. This can be done using a regional-scale air pollution model, which takes the coarse scale outputs as inputs and produces outputs at a fine scale, or alternatively can be done using statistical methods derived from historical relationships between coarse and fine scale concentration patterns. In either case, additional uncertainties are introduced by the downscaling process. Figure 1, taken from [7], provides an overview of a typical climate-air quality-health assessment for ozone. In reviewing the recent literature, it is important to emphasize that the large range of potential modeling choices and input parameters introduces considerable variability across studies, presenting challenges in comparing results and deriving overall conclusions about the body of evidence. On the other hand, this variability captures some of the uncertainties inherent in future projections, which itself is valuable information for decision makers.
Framework for assessing health impacts of air pollution in a changing climate (from Post et al. [7])
To illustrate how this process can be applied in practice, it is instructive to review the study by Knowlton and colleagues [10], which was the first study to systematically assess air pollution-related health impacts due to climate change. The study’s objective was to estimate the future mortality impacts of ozone in the NYC metropolitan area in the 2020s, 2050s, and 2080s as a result of climate change. The Goddard Institute for Space Studies (GISS) global climate model was used to project climate in those future decades at a coarse spatial scale (approx. 400 × 500-km grid spacing), as well as a reference period in the 1990s [11]. This global climate model was run twice, driven by a low and a high greenhouse gas emission scenario. The climate projections were downscaled to a 36 × 36-km grid using the MM5 regional climate model [12]. Next, those climate data were used in conjunction with the US EPA ozone precursor emission inventory to model ozone concentration on the 36-km grid using the CMAQ model [13, 14]. Finally, the ozone data were used as the input to a risk assessment of ozone-related daily mortality, incorporating constant population and baseline mortality rate data, and a concentration response function for ozone, the latter estimated using 10 years of observed daily data from the 1990s [10]. The projected percent change in ozone-related mortality in 2050 is reproduced in Fig. 2, taken from that publication.
Estimated county-specific percent changes in annual ozone-related deaths in the 2050s compared with the 1990s for the A1 greenhouse gas emission scenario, holding anthropogenic ozone precursor emissions constant over time. Map covers the 31 county New York City metropolitan region (from Knowlton et al. [10])
More recently, Post and colleagues [7] projected 2050 ozone-related health effects derived from seven different modeling systems, analyzing the relative magnitude of uncertainties derived from model choices vs. population projections and concentration-response functions. While all of the risk assessment inputs contributed substantially to the overall range of results, the climate and air quality modeling systems appeared to contribute the most to uncertainties. The authors recommended that, where possible, an “ensemble” of multiple models be used to characterize the range of potential future health impacts.
Of the studies published since 2013, the study of Fann and colleagues provided the most comprehensive assessment of climate-related air quality impacts on health in the USA [15•]. This work was carried out in support of the US Global Change Research Program’s Climate and Health Assessment [16]. Health effects were assessed for the year 2030 under the assumption that all currently planned air pollution regulations will be implemented, which defines the air pollution emissions used as input to the modeling system. Given those emissions, ozone concentrations were modeled in response to several scenarios of climate change. Climate change was simulated using two different models and greenhouse gas emission scenarios (RCP6.0 and RCP8.5). Ozone was dynamically downscaled to a 36-km2 grid resolution using the state-of-the-art CMAQ model, with boundary conditions provided by the GEOS-Chem global air quality model. The study isolated the climate change effect on ozone around the year 2030, which is a more policy-relevant time point for most decision makers than later in the century. Health effects were assessed for a range of morbidity outcomes (emergency department visits, hospital admissions, acute respiratory symptoms, and lost school days) as well as mortality, and economic impacts were then computed based on standard methods.
The climate and air quality modeling system projected that daily maximum temperatures could increase by 1–4 °C and that daily 8-h maximum ozone concentrations could increase by 1–5 ppb, in 2030 due to climate change alone. However, there were large differences in impacts in different regions of the country, with impacts appearing greatest in the Midwest and Northeast regions (see Fig. 3 taken from [16]). The health risk assessment suggested that climate-induced changes in ozone concentrations could result in tens to thousands of additional ozone-related deaths and illnesses each year, with economic impacts reaching up to tens of billions of US dollars [15•].
Projected changes by 2030 in mean daily maximum temperature, seasonal average daily 8-h maximum ozone, and ozone-related premature deaths. The upper panels are from the NCAR/DOE Community Earth System Model (CESM) run with the RCP 8.5 radiative forcing scenario. The lower panels are from the NASA Goddard Institute for Space Studies (GISS) Model E2-R global climate model run with the RCP 6.0 radiative forcing scenario (from Fann et al. [15•])
The air quality model projections developed by Fann et al. were used as inputs to a 2030 mortality impact assessment for ozone in 94 US cities by Wilson and colleagues [17•]. The novelty here was the use of updated concentration-response functions that incorporated non-linear and synergistic effects of ozone and temperature, derived from an empirical analysis of daily data from the 1987–2000 NMMAPS database. The authors reported increases in ozone-related mortality of over 14% for ozone concentrations above 75 ppb by 2030. While this suggests that impacts can be much higher when non-linear, interactive risk functions are used, those new functions will require replication before they are more generally adopted. More generally, projections of interactive impacts of multiple climate-related health stressors is an important area for future research.
Garcia-Menendez and colleagues modeled US ozone and PM2.5-related health effects of climate change, with a focus on two future time points, 2050 and 2100 [18]. Three greenhouse gas scenarios were compared, a worst case “business as usual” scenario yielding a total radiative forcing of 10 W/m2 by 2100, and two climate stabilization scenarios that would reduce warming below 1.5 °C, one corresponding to a total radiative forcing of 4.5 W/m2, and the other 3.7 W/m2 by 2100. The modeling system they used produced outputs at a coarse scale over the globe, including the US (approx. 200 × 250-km grid boxes). Air pollution emissions were held constant in order to isolate the effect of climate change. Only mortality effects were assessed. The two climate stabilization scenarios were estimated to result in substantial reductions in mortality across the US due to reductions in both ozone and PM2.5 concentrations. Compared with the business as usual case, the two climate stabilization scenarios yielded mortality benefits ranging from 4000 to 22,000 avoided deaths in 2050 and 19,000 to 95,000 avoided deaths in 2100. The analysis quantified health benefits due to climate effects on air quality but did not assess the direct health benefits of reduced air pollution emissions under the climate stabilization scenarios; in this sense, the health benefits were likely underestimated.
Lee and colleagues modeled US air quality and health in 2030 and 2055 using a coarse scale model with on-the-books US air pollution policies, or with a climate policy assuming 50% reduction in 2050 CO2 emissions largely by reducing coal use [19]. Both sets of scenarios yielded reduced future ozone- and PM2.5-related mortality but also warmed the US climate through 2055 as a result of SO2 and sulfate reductions (sulfate particles cool the atmosphere by scattering incoming light and by promoting cloud formation). The authors stressed the importance of climate policies that go after short-lived climate pollutants (SLCPs) such as ozone and black carbon to achieve win-win results for health AND climate. Trail and colleagues reported results of a US nationwide analysis of ozone and PM2.5 air quality in 2050, taking into account on-the-books air pollution regulations expected to be implemented by that time, with or without climate change [20]. While air pollution emission reductions would lead to substantial improvements in air quality, a climate penalty was noted for ozone, but not for PM2.5.
Several studies have analyzed future climate-air quality health impacts outside the US. Fang and colleagues reported global changes in both ozone and PM2.5-related premature mortality in 2090 vs. 2010 due to climate change [21]. Globally, both pollutants increased on average in populated regions due to climate change, with estimated increases in PM and ozone-related deaths of ca. 100,000 and 6000/year, respectively. Increased mortality was especially pronounced in North America and large parts of Asia. In Europe, projected future ozone-related mortality was found to vary substantially for different countries [22], with ozone increasing in some regions and decreasing in others. Results in Europe appeared to be quite sensitive to the modeling system used [23, 24] but in general observed a climate penalty for ozone (e.g. [25]). Other work has quantified the air pollution-related health effects of climate change that has already occurred, most finding that to date, the climate penalty has been relatively small compared to the burden due to pollution emission increases [26, 27].
The vast majority of modeling studies focus on anthropogenic air pollution. To date, only one study has assessed potential climate-driven changes in wildfire-related/health effects [28], and it suggested potential small increases in respiratory hospital admissions in the western USA by mid-century under moderate climate change scenarios. Outside the health literature, evidence suggests that climate change is leading to higher risks of wildfires, with potential implications for human health [29]. Similarly, only one study has so far examined future impacts of climate on pollen-related health impacts, which suggested that the oak tree pollen season could lengthen by mid-century across parts of the USA, potentially causing additional asthma emergency department visits [30]. Future work is needed to expand these findings for wildfires and pollen, as well as for windblown dust.
Future Perspectives
Given the importance of air pollution as a global risk factor for premature death and disease, along with the intimate connections between climate and air quality, the impacts of climate change on air quality-related health effects are likely to remain an important area of research for the foreseeable future. One important new direction for future research is to analyze potential interactive effects of climate on anthropogenic air pollution along with other climate-driven risk factors such as extreme temperatures [17•], flood-related damage to infrastructure, wildfires, etc. For example, wildfire risk can increase during extremely hot weather, such as occurred in Russia in the summer of 2010. Hot weather also drives elevated ozone concentrations. The potential for cascading, non-linear, interactive health impacts due to multiple, co-occurring climate-related stressors is an important topic for future studies. Tackling complex questions of this kind will require new models and methods, drawing on multidisciplinary expertise. We will need both empirical research to identify and quantify causal mechanisms, as well as projection studies that encompass multiple climate-related metrics and outcomes. Meanwhile, deriving results at spatial and temporal scales that are relevant to decision makers will remain an important challenge.
Conclusion
Several general points emerge from the recent literature. As a body, the studies confirm earlier work indicating that climate change will tend to increase ozone concentrations and related health effects, especially in populated regions, holding air pollution emissions constant [31]. For the USA, the climate impact on ozone is most consistently seen in north-central and north-east states. PM2.5 sensitivity to climate is more variable across studies and regions, owing to the varied nature of PM components, as well as to less complete characterization of PM reaction chemistry in available atmospheric models [1]. Regional differences and model to model variations make it difficult to offer quantitative conclusions. As Fiore states, “Opposing influences of changes in temperature, precipitation, relative humidity, and stagnation on the individual PM2.5 components and their chemistry confound a clean deciphering of PM2.5 changes.”
The complex two-way interactions between climate change and air quality have important implications for policies to address each of these challenges. Reducing fossil fuel emissions, while always beneficial for health, does not always bring climate benefits in the short term. For example, decreased coal combustion reduces CO2 emissions, which helps the climate in the long run, but also reduces SO2 emissions and thus sulfate, which is a cooling pollutant, leading to short-term warming in regions near the source reductions [19]. Methane reductions on the other hand bring both climate and ozone air quality benefits. Reducing black carbon, an important component of PM2.5 and a warming pollutant, also results in win-win solutions for both health and climate. Given their complex interactions, there have been increasing calls for coordinated policies for addressing climate change and air pollution [32,33,34,35,36,37,38]. Reviews and global assessments demonstrate the potential health benefits that can be achieved through coordinated climate and air pollution planning [39, 40]. Innovative urban planning initiatives that integrate climate and health co-benefits are of increasing interest [41]. Achieving sustained impacts on coordinated pollution and climate mitigation will benefit from holistic, multi-stakeholder planning [42]. This is likely to be an area of expanded work in the next several years.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Fiore AM, Naik V, Leibensperger EM. Air quality and climate connections. J Air Waste Manage Assoc. 2015;65(6):645–85. https://doi.org/10.1080/10962247.2015.1040526.
Kinney PL. Climate change, air quality, and human health. Am J Prev Med. 2008;35(5):459–67.
Watts N, Adger WN, Agnolucci P, Blackstock A, Byass P, Cai WJ, et al. Health and climate change: policy responses to protect public health. Lancet. 2015;386(10006):1861–914. https://doi.org/10.1016/S0140-6736(15)60854-6.
Prospero JM, Lamb PJ. African droughts and dust transport to the Caribbean: climate change implications. Science. 2003;302(5647):1024–7. https://doi.org/10.1126/science.1089915.
Sapkota A, Symons JM, Kleissl J, Wang L, Parlange MB, Ondov J, et al. Impact of the 2002 Canadian forest fires on particulate matter air quality in Baltimore city. Environ Sci Technol. 2005;39(1):24–32. https://doi.org/10.1021/es035311z.
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. Lancet. 2017;389(10082):1907–18. https://doi.org/10.1016/S0140-6736(17)30505-6.
Post ES, Grambsch A, Weaver C, Morefield P, Huang J, Leung LY, et al. Variation in estimated ozone-related health impacts of climate change due to modeling choices and assumptions. Environ Health Perspect. 2012;120(11):1559–64. https://doi.org/10.1289/ehp.1104271.
Nakićenović N, Alcamo J, Davis G, de Vries B, Fenhann J, Gaffin S, et al. IPCC special report on emissions scenarios (SRES), working group III, intergovernmental panel on climate change (IPCC). Cambridge: Cambridge University Press; 2000. p. 595.
van Vuuren DP, Edmonds JA, Kainuma M, Riahi K, Weyant J. A special issue on the RCPs. Clim Chang. 2011;109(1–2):1–4. https://doi.org/10.1007/s10584-011-0157-y.
Knowlton K, Rosenthal J, Hogrefe C, Lynn B, Gaffin S, Goldberg R, et al. Assessing ozone-related health impacts under a changing climate. Environ Health Perspect. 2004;112(15):1557–63. https://doi.org/10.1289/ehp.7163.
Russell GL, Miller JR, Rind D. A coupled atmosphere-ocean model for transient climate change studies. Atmosphere-Ocean. 1995;33(4):683–730. https://doi.org/10.1080/07055900.1995.9649550.
Grell GA, Dudhia J, Stauffer DR. A description of the fifth-generation Penn State/NCAR mesoscale model (MM5). NCAR Technical Note, NCAR/TN-398+STR. Boulder: National Center for Atmospheric Research; 1994. p. 122.
Byun DW, Ching JKS, Novak J, Young J. In: Gryning SE, Chaumerliac N, editors. Development and implementation of the EPA’s models-3 initial operating version: Community multi-scale air quality (CMAQ) model. New York: Plenum Press Div Plenum Publishing Corp; 1998. p. 357–68.
Hogrefe C, Lynn B, Civerolo K, Ku J, Rosenthal J, Rosenzweig C, et al. Simulating changes in regional air pollution over the eastern United States due to changes in global and regional climate and emissions. J Geophys Res-Atmos. 2004;109(D22):D22301. https://doi.org/10.1029/2004JD004690.
• Fann N, Nolte CG, Dolwick P, Spero TL, Brown AC, Phillips S, et al. The geographic distribution and economic value of climate change-related ozone health impacts in the United States in 2030. J Air Waste Manage Assoc. 2015;65(5):570–80. This paper comprehensive quantifies health and economic impacts of climate change on future ozone in the US.
USGCRP. The impacts of climate change on human health in the United States: a scientific assessment. Washington: DC; 2016.
• Wilson A, Reich BJ, Nolte CG, Spero TL, Hubbell B, Rappold AG. Climate change impacts on projections of excess mortality at 2030 using spatially varying ozone-temperature risk surfaces. J Expo Sci Environ Epidemiol. 2017;27(1):118–24. This paper suggests that high temperatures may enhance the health effects of future climate-induced increases in ozone concentrations.
Garcia-Menendez F, Saari RK, Monier E, Selin NE. US air quality and health benefits from avoided climate change under greenhouse gas mitigation. Environ Sci Technol. 2015;49(13):7580–8. https://doi.org/10.1021/acs.est.5b01324.
Lee Y, Shindell DT, Faluvegi G, Pinder RW. Potential impact of a US climate policy and air quality regulations on future air quality and climate change. Atmos Chem Phys. 2016;16(8):5323–42. https://doi.org/10.5194/acp-16-5323-2016.
Trail M, Tsimpidi AP, Liu P, Tsigaridis K, Rudokas J, Miller P, et al. Sensitivity of air quality to potential future climate change and emissions in the United States and major cities. Atmos Environ. 2014;94:552–63. https://doi.org/10.1016/j.atmosenv.2014.05.079.
Fang YY, Mauzerall DL, Liu JF, Fiore AM, Horowitz LW. Impacts of 21st century climate change on global air pollution-related premature mortality. Clim Chang. 2013;121(2):239–53. https://doi.org/10.1007/s10584-013-0847-8.
Orru H, Andersson C, Ebi KL, Langner J, Astrom C, Forsberg B. Impact of climate change on ozone-related mortality and morbidity in Europe. Eur Respir J. 2013;41(2):285–94. https://doi.org/10.1183/09031936.00210411.
Lacressonniere G, Foret G, Beekmann M, Siour G, Engardt M, Gauss M, et al. Impacts of regional climate change on air quality projections and associated uncertainties. Clim Chang. 2016;136(2):309–24. https://doi.org/10.1007/s10584-016-1619-z.
Lacressonniere G, Peuch VH, Vautard R, Arteta J, Deque M, Joly M, et al. European air quality in the 2030s and 2050s: impacts of global and regional emission trends and of climate change. Atmos Environ. 2014;92:348–58. https://doi.org/10.1016/j.atmosenv.2014.04.033.
Jimenez-Guerrero P, Gomez-Navarro JJ, Baro R, Lorente R, Ratola N, Montavez JP. Is there a common pattern of future gas-phase air pollution in Europe under diverse climate change scenarios? Clim Chang. 2013;121(4):661–71. https://doi.org/10.1007/s10584-013-0944-8.
Silva RA, West JJ, Zhang YQ, Anenberg SC, Lamarque JF, Shindell DT, et al. Global premature mortality due to anthropogenic outdoor air pollution and the contribution of past climate change. Environ Res Lett. 2013;8(3):11.
Fang Y, Mauzerall DL, Liu J, Fiore AM, Horowitz LW. Impacts of 21st century climate change on global air pollution-related premature mortality. Clim Chang. 2013;121(2):239–53. https://doi.org/10.1007/s10584-013-0847-8.
Liu JC, Mickley LJ, Sulprizio MP, Yue X, Peng RD, Dominici F, et al. Future respiratory hospital admissions from wildfire smoke under climate change in the Western US. Environ Res Lett. 2016;11(12):6.
Jolly WM, Cochrane MA, Freeborn PH, Holden ZA, Brown TJ, Williamson GJ, et al. Climate-induced variations in global wildfire danger from 1979 to 2013. Nat Commun. 2015;6:11.
Anenberg S, Weinberger KR, Roman H, Neumann JE, Crimmins A, Fann N, et al. Impacts of oak pollen on allergic asthma in the USA and potential effect of future climate change: a modelling analysis. Lancet. 2017;389:2.
Bell ML, Goldberg R, Hogrefe C, Kinney PL, Knowlton K, Lynn B, et al. Climate change, ambient ozone, and health in 50 US cities. Clim Chang. 2007;82(1–2):61–76. https://doi.org/10.1007/s10584-006-9166-7.
Melamed ML, Schmale J, von Schneidemesser E. Sustainable policy-key considerations for air quality and climate change. Curr Opin Environ Sustain. 2016;23:85–91. https://doi.org/10.1016/j.cosust.2016.12.003.
Maione M, Fowler D, Monks PS, Reis S, Rudich Y, Williams ML, et al. Air quality and climate change: designing new win-win policies for Europe. Environ Sci Pol. 2016;65:48–57. https://doi.org/10.1016/j.envsci.2016.03.011.
Pettersen MV, Fleck F. Bringing air pollution into the climate change equation. Bull World Health Organ. 2014;92(8):553–4. https://doi.org/10.2471/BLT.14.030814.
Hassan NA, Hashim Z, Hashim JH. Impact of climate change on air quality and public health in urban areas. Asia Pac J Public Health. 2016;28(2_suppl):38S–48S. https://doi.org/10.1177/1010539515592951.
Klausbruckner C, Annegarn H, Henneman LRF, Rafaj P. A policy review of synergies and trade-offs in South African climate change mitigation and air pollution control strategies. Environ Sci Pol. 2016;57:70–8. https://doi.org/10.1016/j.envsci.2015.12.001.
Perera FP. Multiple threats to child health from fossil fuel combustion: impacts of air pollution and climate change. Environ Health Perspect. 2017;125(2):141–8.
Kelly FJ. Twin problems of climate change and air pollution. Br Med J. 2016;355:2.
De Sario M, Katsouyanni K, Michelozzi P. Climate change, extreme weather events, air pollution and respiratory health in Europe. Eur Respir J. 2013;42(3):826–43. https://doi.org/10.1183/09031936.00074712.
Rao S, Pachauri S, Dentener F, Kinney P, Klimont Z, Riahi K, et al. Better air for better health: forging synergies in policies for energy access, climate change and air pollution. Glob Environ Change Human Policy Dimens. 2013;23(5):1122–30. https://doi.org/10.1016/j.gloenvcha.2013.05.003.
Erickson LE, Jennings M. Energy, transportation, air quality, climate change, health nexus: sustainable energy is good for our health. AIMS Public Health. 2017;4(1):47–61. https://doi.org/10.3934/publichealth.2017.1.47.
Schmale J, von Schneidemesser E, Chabay I, Maas A, Lawrence MG. In: Drake JL, Kontar YY, Eichelberger JC, Rupp TS, Taylor KM, editors. Building interfaces that work: a multi-stakeholder approach to air pollution and climate change mitigation. Dordrecht: Springer; 2016. p. 65–76.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Patrick L. Kinney declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Climate Change and Health
Rights and permissions
About this article
Cite this article
Kinney, P.L. Interactions of Climate Change, Air Pollution, and Human Health. Curr Envir Health Rpt 5, 179–186 (2018). https://doi.org/10.1007/s40572-018-0188-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-018-0188-x