Abstract
Rubella, commonly known as ‘German Measles’ is a common childhood viral disease that may affect adults as well. More than half of the infections are either asymptomatic or present with mild flu like illness with a typical maculopapular rash. In contrast, primary rubella infection in pregnancy, especially in the first trimester, can have serious consequences, namely miscarriage, intrauterine fetal demise or congenital rubella syndrome (CRS). WHO recognizes CRS as the ‘leading vaccine preventable cause of birth defects’. Antenatal management primarily is based on testing for immunity in the first trimester and recognizing acute maternal infection. A correct interpretation of maternal serology using IgG avidity along with IgM and IgG is imperative to avoid false positive diagnoses. Diagnosis of fetal infection is by detection of Rubella virus specific RTPCR in amniotic fluid and is indicated if maternal seroconversion is seen in the periconceptional period and/or the first trimester or if there are ultrasound features suggestive of fetal infection. Since there is no treatment available to either prevent mother to child transmission or to treat fetal infection, the mainstay is prevention. India is amongst the 11 countries of WHO South East Asia Region who are committed to control of Rubella and CRS by 2020.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rubella is a common childhood viral disease characterized by a mild flu like illness with a typical post auricular maculopapular rash and is popularly known as ‘German measles’. Rubella infection in pregnancy especially in the first trimester can result in miscarriage, intrauterine fetal death, stillbirth or congenital rubella syndrome (CRS) [1]. The association between congenital defects and rubella in pregnancy was first described by the Australian ophthalmologist, Normal McAlister Gregg in 1941 [2]. More than seven decades later, CRS is still being recognized as the ‘leading vaccine preventable cause of birth defects’ (https://www.who.int/news-room/fact-sheets/detail/rubella).
CRS remains a huge burden in South east Asia. 46% of an estimated 103,000 infants diagnosed with CRS globally in 2010 were born in this region [3]. The risk is highest in countries where women of childbearing age are not immune to the disease. India introduced the MMR (measles, mumps and rubella) vaccine nationwide in 2017 and also launched a mass vaccination programme targeting children from 9 months to 14 years of age [4]. Government of India’s Ministry of Health and Family Welfare (MoHFW) along with Indian Council of Medical Research (ICMR) initiated surveillance for CRS only in December 2016. Currently, India is amongst the 11 countries of WHO South East Asia Region who are committed to control of Rubella and CRS by 2020 [5].
Virology
Rubella virus is a single stranded RNA virus that belongs to the Togaviridae family. Humans are the only known reservoirs and infection occurs from person to person through aerosols. The virus enters the human body via inhalation and then replicates in the respiratory mucosa and cervical lymph nodes. Its incubation period is 13–20 days. An affected person is infectious from 8 days before and 8 days after the rash appears.
Clinical Features
More than 50% of infections are asymptomatic. In the rest, it may present with a mild flu like illness with fever, malaise and lymphadenopathy involving mainly postauricular lymph nodes. A diffuse maculopapular rash may appear for 1–3 days. The most common complications in adults are polyarthritis and polyarthralgia for 3–4 days; though it may persist for one month. Rarely, the viral infection may cause encephalitis, thrombocytopenia, haemorrhagic manifestations and/or Guillen Barre syndrome [6]. Rubella reinfection can also occur but it is typically subclinical and is usually diagnosed only on serology showing a significant rise in antibody titres.
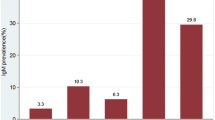
In contrast, when primary rubella infection occurs in pregnancy, especially in the first trimester, it can have serious consequences, namely miscarriage, intrauterine fetal demise or congenital rubella syndrome (CRS). The risk of fetal infection as well as fetal affectation following primary maternal infection depends on the gestation age at which infection is acquired (Table 1). The risk of fetal infection with secondary infection is estimated to be < 5% [6].
Routine Testing for Rubella in Pregnancy
All guidelines recommend testing for immunity to Rubella at the booking visit in the first trimester. Rubella IgG alone is sufficient for establishing immunity (or lack of it). IgM should be advised if there is any history suggestive of rubella infection or exposure to an infected individual. If at all, both IgM and IgG can be done: IgM alone should not be done. IgM testing is inconclusive and may be false positive in many cases due to chronic persistence of the IgM antibody [9]. History of past immunization must be taken. Other indications for repeat maternal testing would be ultrasound findings suggestive of fetal infection: early onset fetal growth restriction (FGR) especially when presenting before 24 weeks, ventriculomegaly, fetal cataract, microcephaly, placentomegaly, hepatic calcifications and/or echogenic bowel etc. Since these are nonspecific signs, it would warrant doing the entire TORCH panel (both IgM and IgG).
Diagnosis of Maternal Infection
Rubella specific IgM appears within 3 days after the appearance of rash and usually disappears in 4 to 12 weeks. IgG antibodies appear within 5–8 days following the rash and persist throughout life [7]. However, since the clinical symptoms may not be reliable or even present, the diagnosis of maternal infection is primarily based on ‘seroconversion’ [8]. Low levels of IgM antibodies may be detected for months or even years following both primary infection as well as vaccination [9]. Thus as mentioned earlier, the diagnosis of maternal infection should not be based on IgM alone. The correct interpretation of serology results is extremely important (Table 2) [9]. The most important parameters are a fourfold increase in the IgG tire done from the same lab at least 2 weeks apart along with low IgG avidity [10].
Management of Infection in Pregnancy
Rubella in the pregnant mother is a self-limiting mild disease and may require symptomatic treatment of fever at most. However, if there is proven maternal primary infection prior to 12 weeks pregnancy, there is a high risk of fetal transmission as well as fetal defects and termination of pregnancy should be offered to the patient.
Infection suspected between 11 and 18 weeks warrants amniocentesis for detection of fetal infection. If the patient does not opt for amniocentesis, serial 4 weekly scans are recommended. The newborn should be checked for rubella specific IgM postnatally.
Infection after 18–20 weeks does not warrant invasive testing; however serial 4 weekly scans and postnatal evaluation of the newborn are recommended.
Diagnosis of Fetal Infection
The risk of fetal infection as well as affectation is as high as 90% when infection occurs in the first trimester. In contrast, the risk of fetal infection following secondary (re)infection is < 5%. The decision for performing prenatal diagnosis of fetal rubella infection would be either suspected maternal primary infection and/or ultrasound features suspicious of fetal infection.
Diagnosis of fetal infection is based on the detection of Rubella viral RTPCR in the amniotic fluid. The specificity of viral PCR on amniotic fluid is 100% and sensitivity is more than 90% presuming that the procedure is timed correctly [11]. Amniocentesis should be done after at least 6 weeks following suspected maternal infection or after 20 weeks whichever is later. It is also suggested that the sample be processed as soon as possible or if it needs to be transported, it should be transported frozen [11].
If Rubella viral PCR is found in the amniotic fluid, fetal infection is presumed.
Amniocentesis should also be offered if there are ultrasound features suggestive of fetal infection, e.g. early onset fetal growth restriction, microcephaly, ventriculomegaly, intracerebral calcifications, fetal cataract (Fig. 1a), echogenic bowel, hepatic calcifications (Fig. 1b), placentomegaly etc. [12,13,14]. Since all these features are nonspecific for any particular fetal infection, maternal serology can help in guiding which virus to test the amniotic fluid for. The specificity of ultrasound in diagnosing CRS is 100% though the sensitivity is only 11% considering the nonspecific nature of the findings [15].
Congenital Rubella Syndrome (CRS)
CRS is characterized by the classical triad of cataract, cardiovascular abnormalities and sensorineural deafness. Other features are summarised in Table 3. Sensorineural deafness is the most common abnormality and it may be the only abnormality especially when infection occurs between 12 and 20 weeks of gestation.
Postnatal Diagnosis of CRS
Prevention: Immunization
Currently there is no treatment to either prevent mother to child transmission or to treat an infected fetus. Thus prevention is the mainstay if we are to prevent the devastating CRS. The best way to eradicate CRS is to immunize all susceptible women.
All women of childbearing age and/or presenting for preconception counseling should be advised testing for rubella IgG. If she is nonimmune, vaccination (rubella alone or MMR) should be suggested. Pregnancy should be avoided for a month after vaccination. Women who are found to be non-immune during pregnancy should be vaccinated immediately postpartum. Breastfeeding is not a contraindication to the rubella vaccine [22,23,24]. India started a mass immunization programme with MMR targeting children aged 9 months to 14 years in 2017 [4].
Conclusions
Rubella in pregnancy is not uncommon and the sequelae of infection in the first trimester can be devastating. Since there is no treatment, prevention is the best strategy to avoid CRS. Thus all women presenting for pre-pregnancy counseling must be checked for their immune status and advised immunization if they are nonimmune. All pregnant women should be advised Rubella IgG in the first trimester to document immunity. Routine TORCH testing and/or only Rubella IgM testing must not be done.
References
Miller E, Cradock-Watson JE, Pollock TM. Consequences of confirmed maternal rubella at successive stages of pregnancy. Lancet. 1982;2(8302):781–4.
Gregg NM. Congenital cataract following German measles in mother. Trans Ophthalmol Soc Aust. 1944;3:35–46.
World Health Organization India. India launches one of the world’s largest vaccination campaigns against measles and rubella syndrome with WHO support. New Delhi, India: World Health Organization Regional Office for South-East Asia; 2017. https://www.searo.who.int/india/mediacentre/events/2017/Measles_Rubella/en. Accessed 11 July 2017.
Murhekar M, Bavdekar A, Benakappa A, et al. Sentinel surveillance for congenital rubella syndrome—India, 2016–2017. MMWR Morb Mortal Wkly Rep. 2018;67(36):1012–6.
World Health Organization. Strategic plan for measles elimination and rubella and congenital rubella syndrome control in the South-East Asia Region. New Delhi, India: World Health Organization Regional Office for South-East Asia; 2015. https://www.searo.who.int/immunization/documents/sear_mr_strategic_plan_2014_2020.pdf
Bouthry E, Picone O, Hamdi G, et al. Rubella and pregnancy: diagnosis, management and outcomes. Prenat Diagn. 2014;34(13):1246–53.
Vauloup-Fellous C, Grangeot-Keros L. Humoral immune response after primary rubella virus infection and after vaccination. Clin Vaccine Immunol. 2007;14:644–7.
Deka D, Rustgi R, Singh S, et al. Diagnosis of acute rubella infection in pregnancy. J Obstet Gynecol India. 2006;56(1):44–6.
Best JM, O'Shea S, Tipples G, Davies N, Al-Khusaiby SM, Krause A, et al. Interpretation of rubella serology in pregnancy–pitfalls and problems. BMJ. 2002;325(7356):147–8.
Vauloup-Fellous C, Ursulet-Diser J, Grangeot-Keros L. Development of a rapid and convenient method for determination of rubella virus-specific immunoglobulin G avidity. Clin Vaccine Immunol. 2007;14:1416–9.
Macé M, Cointe D, Six C, et al. Diagnostic value of reverse transcription-PCR of amniotic fluid for prenatal diagnosis of congenital rubella infection in pregnant women with confirmed primary rubella infection. J Clin Microbiol. 2004;42:4818–20.
Yazigi A, De Pecoulas AE, Vauloup-Fellous C, et al. Fetal and neonatal abnormalities due to congenital rubella syndrome: a review of literature. J Matern Fetal Neonatal Med. 2017;30(3):274–8.
Lambert N, Strebel P, Orenstein W, et al. Rubella. Lancet. 2015;385(9984):2297–307.
Cordier AG, Vauloup-Fellous C, Grangeot-Keros L, et al. Pitfalls in the diagnosis of congenital rubella syndrome in the first trimester of pregnancy. Prenat Diagn. 2012;32:496–7.
Migliucci A, Di Fraja D, Sarno L, et al. Prenatal diagnosis of congenital rubella infection and ultrasonography: a preliminary study. Minerva Ginecol. 2011;63:485–9.
Oster ME, Riehle-Colarusso T, Correa A. An update on cardiovascular malformations in congenital rubella syndrome. Birth Defects Res A Clin Mol Teratol. 2010;88:1–8.
Givens KT, Lee DA, Jones T, et al. Congenital rubella syndrome: ophthalmic manifestations and associated systemic disorders. Br J Ophthalmol. 1993;77:358–63.
Ginsberg-Fellner F, Witt ME, Fedun B, et al. Diabetes mellitus and autoimmunity in patients with the congenital rubella syndrome. Rev Infect Dis. 1985;7(Suppl 1):S170–S176176.
Forrest JM, Turnbull FM, Sholler GF, et al. Gregg’s congenital rubella patients 60 years later. Med J Aust. 2002;177:664–7.
Thomas HIJ, Morgan-Capner P, Cradock-Watson JE, et al. Slow maturation of IgG1 avidity and persistence of specific IgM in congenital rubella: implications for diagnosis and immunopathology. J Med Virol. 1993;41:196–200.
Bosma TJ, Corbett KM, Eckstein MB, et al. Use of PCR for prenatal and postnatal diagnosis of congenital rubella. J Clin Microbiol. 1995;33:2881–7.
Gruslin A, Steben M, Halperin S, et al. Immunization in pregnancy. Infectious diseases committee of the society of obstetricians and gynaecologists of Canada. J Obstet Gynaecol Can. 2009;31(11):1085–101.
Swamy GK, Heine RP. Vaccinations for pregnant women. Obstet Gynecol. 2015;125(1):212–26.
Briggs G, Freeman R. Drugs in pregnancy and lactation. 9th ed. Williams and Willkins, Philadelphia: Lippincott; 2009.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, C. Rubella in Pregnancy. J. Fetal Med. 7, 37–41 (2020). https://doi.org/10.1007/s40556-019-00238-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40556-019-00238-2