Abstract
Background
This investigation aimed to examine and compare the predictive value of MADIT-II, FADES, PACE and SHOCKED scores in predicting one-year and long-term all-cause mortality in implantable cardioverter-defibrillator (ICD) implanted patients, 75 years old and older, since there has been an area of uncertainty about the utility and usefulness of these available risk scores in such cases.
Methods
In this observational, retrospective study, 189 ICD implanted geriatric patients were divided into two groups according to the presence of long-term mortality in follow-up. The baseline characteristics and laboratory variables were compared between the groups. MADIT-II, FADES, PACE and SHOCKED scores were calculated at the time of ICD implantation. One-year and long-term predictive values of these scores were compared by a receiver-operating curve (ROC) analysis.
Results
A ROC analysis showed that the best cutoff value of the MADIT-II score to predict one-year mortality was ≥ 3 with 87% sensitivity and 74% specificity (AUC 0.83; 95% CI 0.73–0.94; p < 0.001) and that for long-term mortality was ≥ 2 with 83% sensitivity and 43% specificity (AUC 0.68; 95% CI 0.60–0.76; p < 0.001). The predictive value of MADIT-II was superior to FADES, PACE and SHOCKED scores in ICD implanted patients who are 75 years and older.
Conclusion
MADIT-II score has a significant prognostic value as compared to FADES, PACE and SHOCKED scores for the prediction of one-year and long-term follow-up in geriatric patients with implanted ICDs for heart failure with reduced ejection fraction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the current practice, using an implantable cardioverter-defibrillator (ICD) is the recommended treatment strategy to prevent sudden cardiac death (SCD) in well-selected cases [1, 2]. However, a majority of cases receiving ICD implantation have experienced either inappropriate ICD shocks or pocket-sized complications during the long-term follow-up [3, 4]. Moreover, patients with significant comorbidities who have an ICD usually die from causes other than life-threating arrhythmias, such as progressive heart failure (HF), stroke and malignancy. According to the current guidelines, ICD implantation is not recommended for patients with less than one year of life expectancy [5].
Age, in particular, is not considered a contraindication for ICD implantation. However, comorbidities accumulated in elderly patients can reduce ICD benefits during the long-term follow-up period [6]. The MADIT-II, SHOCKED, PACE and FADES are well-known clinical risk scores for predicting mortality in patients receiving ICD implantation [7,8,9,10]. Nevertheless, the predictive value of these clinical risk scores has not been compared in patients, 75 years old and older, who receive ICD implantation. In this context, the present study aimed to examine and compare the predictive value of these clinical risk scores in predicting one-year and long-term all-cause mortality in ICD-implanted patients who were 75 years and older since there has been an area of uncertainty about the utility and usefulness of available risk scores in such cases.
Materials and methods
Data collection
The data of consecutive cases receiving an ICD implantation in our institution between January 2009 and December 2019 were retrospectively screened. We enrolled patients 75 years old and older at the time of implantation. Our institution was a tertiary heart centre, in which > 100 ICD implantations were performed each year. For each case, the decision to implant an ICD was performed according to the current guideline recommendations [11]. In this investigation, patients with severe functional and cognitive impairments (such as dementia or severe neuropsychological disorders) were not included in the analysis. Demographic properties, comorbidities, the aetiology of HF, the type of indication (primary or secondary) and the device type were retrieved either from electronic medical files, procedure notes or discharge summaries. The parameters related to echocardiographic findings, laboratory data and New York Heart Association (NYHA) functional class were collected at the time of device implantation. The MADIT-II, SHOCKED, PACE and FADES scores of each case were determined. The MADIT-II score includes atrial fibrillation, NYHA class, QRS > 120 msn, age and blood urea nitrogen; the SHOCKED score consists of age, NYHA class, atrial fibrillation, chronic obstructive lung disease, chronic renal disease, ejection fraction and diabetes mellitus; the FADES score includes age, NYHA class, diabetes mellitus, ejection fraction and smoking; and the PACE score includes age, creatinine, ejection fraction and peripheral arterial disease [7,8,9,10]. The outline of the study was approved by the Local Ethics Committee, after which our study was performed in accordance with the good clinical practice guidelines of the Declaration of Helsinki.
ICD implantation
In our centre, ICD implantation was performed in the pectoral area by an experienced cardiologist. In all patients, a ventricular arrhythmia monitor zone was programmed between 150 and 188 bpm. Two bursts of anti-tachycardia pacing (ATP) were the choice of therapy for ventricular arrhythmias faster than 188 bpm. If ventricular arrhythmias were not terminated by ATP, the device delivered defibrillator shocks. On the other hand, defibrillator shocks were the first choice of therapy for ventricular arrhythmias faster than 210 bpm. The ICD programme settings for the detection zones were changed if clinically required.
Long-term follow-up
Following an ICD implantation, patients enrolled in our study were regularly followed up with six-month intervals or more frequently if clinically indicated. During the regular visit, an experienced physician used a programmer to interrogate the device to check for any arrhythmia episodes. The delivered therapy, including ATP and shocks, was categorised as an appropriate shock in case it occurred in response to VT or VF. The primary outcome of the research was the incidence of one-year and long-term all-cause mortality. We used the National Death Notification System to determine the vital status of each case.
Statistical analysis
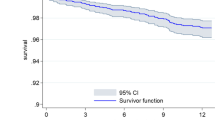
All statistical analyses were conducted using SPSS Windows software (ver. 21.0; IBM, USA). All continuous variables were not homogeneously distributed; hence, these variables were expressed as median and interquartile range (IQR) and compared with the Mann–Whitney U test. Categorical variables were presented as total numbers and percentages and compared using the chi-square test or Fisher exact test. To demonstrate the sensitivity and specificity of each score and their cutoff values for predicting one-year and long-term all-cause mortality, receiver-operating characteristics (ROC) curves were used. The area under the curve (AUC) comparison of each score was performed using the DeLong method. A Kaplan–Meir analysis was drawn to show the long-term mortality of patients according to the MADIT-II score. A two-tailed p value < 0.05 was considered as statistically significant and 95% confidence intervals (95% CI) were presented for all odds ratios (OR). A univariate Cox regression analysis was used to quantify the association of the variables and risk scores with long-term mortality. Variables found to be statistically significant (p < 0.05) in univariate analysis were used in a multivariate Cox regression analysis using the forward method to determine the independent prognostic factors for long-term mortality in ICD-implanted patients 75 years and older. Multivariable models were formed with each score one by one to prevent overfitting and if the variables were components of the risk score, they were not included in the multivariable model.
Results
In this retrospective study, we included 189 patients [median age = 79.0 years (IQR 76.0–82.0 years), 77.8% of them (n = 147 cases) were male] who were 75 years old and over and treated with ICD therapy. The median follow-up in our study was 57 months (IQR 22–90 months). During follow-up, one-year and long-term mortalities were 8.5% (n = 16 cases) and 38.0% (n = 72 cases), respectively. The study population was categorised into two groups; patients who survived and those who died during the long-term follow-up.
Table 1 summarises baseline features and clinical characteristics of all the cases enrolled in this study. Patients who died during the long-term period were older. There were no significant differences between the groups regarding baseline characteristics and comorbidities, excluding atrial fibrillation, which was significantly higher in the mortality group. The indications and types of implanted ICD device did not differ between the groups. As expected, patients who died during the long-term follow-up had a higher baseline NYHA functional class > 2. Notably, the frequency of appropriate shocks was more common in patients who died during the long-term follow-up.
Table 2 presents the laboratory findings, echocardiographic data and the median values of each predictive score. The mortality group had a higher median white blood cell count and urea and lower serum albumin levels at the device implantation. The other laboratory results were similar between the groups. Regarding echocardiographic parameters, left ventricular (LV) ejection fraction was lower and LV end-diastolic diameter was higher in patients who died during the long-term follow-up. The median value of each clinical risk score, including MADIT-II, SHOCKED, PACE and FADES, was significantly higher in the mortality group.
The following factors were found to have prognostic significance in univariate Cox regression analysis: age; coronary artery bypass grafting; atrial fibrillation; NYHA > 2; appropriate shock; inappropriate shock; glucose; albumin, urea, ejection fraction; MADIT II, SHOCKED, FADES and PACE scores (Table 3). In multivariate Cox regression analysis using the enter method, appropriate shock (HR 2.196, 95% CI 1.393–3.464; p < 0.001), albumin (HR 0.674, 95% CI 0.456–0.996; p = 0.048), MADIT II score (HR 1.686, 95% CI 1.359–2.092; p < 0.001), SHOCKED score (HR 1.006, 95% CI 1.003–1.008; p = 0.001) and FADES score (HR 1.365, 95% CI 1.127–1.655; p < 0.001) were found to be independent factors to determine long-term mortality (Table 3).
Figure 1 shows the ROC curve analysis of each clinical risk score for one-year mortality in ICD implanted patients. To predict one-year mortality; the ideal value of the MADIT-II score was ≥ 3 with 87% sensitivity and 74% specificity (AUC 0.83; 95% CI 0.73–0.94; p < 0.001), the ideal value of SHOCKED score was ≥ 128 with 81% sensitivity and 63% specificity (AUC 0.78; 95% CI 0.65–0.92; p < 0.001), the ideal value of FADES score was ≥ 4 81% with sensitivity and 72% specificity (AUC 0.79; 95% CI 0.68–0.90; p < 0.001) and the ideal value of PACE score was ≥ 2 with 56% sensitivity and 76% specificity (AUC 0.66; 95% CI 0.51–0.81; p < 0.001). When the AUC values of each clinical risk score were compared to predict long-term mortality, we found that the MADIT-II score had the highest value (AUC 0.68; 95% CI 0.60–0.76; p < 0.001), followed by the SHOCKED score (AUC 0.59; 95% CI 0.50–0.67; p < 0.001), the FADES score (AUC 0.58; 95% CI 0.49–0.66; p < 0.001) and the PACE score (AUC 0.56; 95%CI 0.48–0.65; p < 0.001) (Fig. 2). To predict the long-term mortality; the ideal value of the MADIT-II score was ≥ 2 with 83% sensitivity and 43% specificity, the ideal value of the SHOCKED score was ≥ 128 with 50% sensitivity and 65% specificity, the ideal value of the FADES score was ≥ 3 72% with sensitivity and 39% specificity; and the ideal value of the PACE score was ≥ 2 with 36% sensitivity and 78% specificity. Pairwise comparison of the ROC curve analyses revealed that the MADIT-II score outperformed the other risk scores in predicting both one-year and long-term mortalities. When patients were categorised as high-risk (≥ 3 points) or intermediate risk (1 or 2 points) according to the MADIT-II score, the Kaplan–Meier analysis revealed that patients with a high-risk MADIT-II score had a lower chance of survival during the long-term follow-up (Fig. 3).
Discussion
In this study, we compared the well-known clinical risk scores to predict one-year and long-term mortalities in patients who were 75 years and older and received ICD implantation. The study results revealed that the MADIT-II score outperformed the other risk scores in predicting both one-year and long-term mortalities in these patients.
ICD implantation in geriatric patients appears to be a challenging circumstance in routine clinical practice due to the presence of numerous comorbidities along with age. Also, geriatric patients comprised approximately 10% of the study population in large-scale investigations [1, 12]. Thus, it is debatable to decide on ICD implantation in geriatric patients with several comorbidities, particularly primary prevention. Although SCD is prevalent in elderly patients, the ratio of SCD to all-cause mortality decreases in geriatric patients [13]. The need for a comparison of long-term mortality predictive scores in geriatric patients has been obvious. Thus, our study’s results could enlighten the prognostic power of the well-accepted ICD follow-up scores in elderly patients.
The FADES score differs from the other scores regarding the contained number of parameters. Diabetes mellitus and smoking are the noticeable factors included only in FADES score. In our study population, the frequency of smoking and diabetes lacked an impact on long-term mortality, which might explain the lower predictive value of FADES compared to MADIT-II score. Similarly, atrial fibrillation, which has prognostic value for long-term mortality in our study population, was included in both the SHOCKED and MADIT-II scores. The SHOCKED score also had a lower predictive value than the MADIT-II score, which might be due to the inclusion of nonpredictive parameters in our population, such as diabetes mellitus, chronic renal failure and chronic obstructive pulmonary disease. Peripheral arterial disease is merely included in the PACE score. Since it is not an independent predictor of long-term mortality in this cohort, PACE score lacked additional prognostic acquisition in our study.
The MADIT-II score is the most powerful predictor of one-year and long-term mortalities, which is considered to be under favour of inclusion both NYHA and blood urea nitrogen variables in its model. Higher blood urea nitrogen levels have already been shown to induce higher mortality both in patients with and without heart failure [14,15,16]. The predictive significance of blood urea nitrogen has also been verified in our study with its contribution to the MADIT-II score in geriatric patients with ICDs for heart failure with reduced ejection fraction. NYHA > 2 has been repeatedly associated with an increased risk of mortality in early and late mortalities after ICD implantation [17, 18].The PACE score has the lowest predictive value for one-year and long-term mortalities, which might be secondary to not including NYHA as a variable in the model.
In our study, all the scores have acceptable predictive power to predict one-year mortality, which is considered to be secondary to a higher incidence of comorbidities in nonsurvivor patients through an one-year follow-up. Studies have shown that the MADIT-II score is significant for short-and long-term follow-ups [19, 20]. Also, it has a comparable prognostic value with the Seattle Heart Failure Model, which includes several clinical, laboratory and echocardiographic variables [20].
Limitations of the study
Our study has several limitations. First, there might be an increased risk of several confounding factors due to the retrospective design of the investigation. However, all consecutive elderly patients were included and a device follow-up was implemented following a standard protocol. Second, patients with a history of chanellopathies, left ventricular noncompaction, arrhythmogenic right ventricular dysplasia and hypertrophic cardiomyopathy were excluded from the investigation; thus, these results should be evaluated separately from these patients. Third, the scores were calculated at the time of ICD implantation; therefore, we ignored the variables that could have developed during the follow-up. Fourth, the exact cause of long-term mortality in our study population has not been noted; therefore, it is not possible to evaluate mortality outcomes regarding cardiac and noncardiac. Fifth, although patients with severe functional and cognitive impairment were excluded, we could not assess the remaining study population’s basic functional and cognitive functions. Sixth, as underlined before, elderly patients with heart failure do not appear to receive adequate treatment, therefore there might be a confounding factor about the medication usage in our study population [21]. Finally, we acknowledged that our study probably comprised a relatively small number of participants.
Conclusion
MADIT-II score has a significant prognostic value compared to FADES, PACE and SHOCKED scores for predicting one-year and long-term follow-ups in geriatric patients implanted ICD for heart failure with reduced ejection fraction.
References
Bardy GH, Lee KL, Mark DB et al (2005) Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 352:225–237
Moss AJ, Hall WJ, Cannom DS, et al (1996) Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N Engl J Med 335:1933–1940
Polewczyk A, Jachec W, Janion M et al (2015) Lead-dependent infective endocarditis: the role of factors predisposing to its development in an analysis of 414 clinical cases. Pacing Clin Electrophysiol 38:846–856
van Rees JB, Borleffs CJ, Bie MK et al (2011) Inappropriate implantable cardioverter–defibrillator shocks: incidence, predictors, and impact on mortality. J Am Coll Cardiol 57:556–562
Yancy CW, Jessup M, Bozkurt B et al (2017) 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of cardiology/American heart association task force on clinical practice guidelines and the heart failure society of America. J Am Coll Cardiol 70:776–803
Zakine C, Garcia R, Narayanan K et al (2019) Prophylactic implantable cardioverter-defibrillator in the very elderly. Europace 21:1063–1069
Goldenberg I, Vyas AK, Hall WJ et al (2008) Risk stratification for primary implantation of a cardioverter-defibrillator in patients with ischemic left ventricular dysfunction. J Am Coll Cardiol 51:288–296
Bilchick KC, Stukenborg GJ, Kamath S et al (2012) Prediction of mortality in clinical practice for medicare patients undergoing defibrillator implantation for primary prevention of sudden cardiac death. J Am Coll Cardiol 60:1647–1655
Kramer DB, Friedman PA, Kallinen LM et al (2012) Development and validation of a risk score to predict early mortality in recipients of implantable cardioverter-defibrillators. Heart Rhythm 9:42–46
van Rees JB, Borleffs CJ, Welsenes GH et al (2012) Clinical prediction model for death prior to appropriate therapy in primary prevention implantable cardioverter defibrillator patients with ischaemic heart disease: the FADES risk score. Heart 98:872–877
Brignole M, Auricchio A, Baron-Esquivias G et al (2013) ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J 34:2281–2329
Moss AJ, Zareba W, Hall WJ et al (2002) Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 346:877–883
Saba S, Adelstein E, Wold N et al (2017) Influence of patients’ age at implantation on mortality and defibrillator shocks. Europace 19:802–807
Sujino Y, Nakano S, Tanno J et al (2019) Clinical implications of the blood urea nitrogen/creatinine ratio in heart failure and their association with haemoconcentration. ESC Heart Fail 6:1274–1282
Rizas KD, McNitt S, Hamm W et al (2017) Prediction of sudden and non-sudden cardiac death in post-infarction patients with reduced left ventricular ejection fraction by periodic repolarization dynamics: MADIT-II substudy. Eur Heart J 38:2110–2118
Wybauw R (1910) Sur le point d’origine de la systole cardiaque dans l’oreillette droite. Arch internat d Physiol 10:78–90
Garcia R, Boveda S, Defaye P et al (2020) Early mortality after implantable cardioverter defibrillator: Incidence and associated factors. Int J Cardiol 301:114–118
Tandri H, Griffith LS, Tang T et al (2006) Clinical course and long-term follow-up of patients receiving implantable cardioverter-defibrillators. Heart Rhythm 3:762–768
Naksuk N, Akkaya M, Adabag S (2013) Application of the multicenter automatic defibrillator implantation trial II risk score in a nontrial setting. Am J Cardiol 112:530–532
Akoudad S, Dabiri Abkenari L, Schaer BA et al (2017) Comparison of multivariate risk estimation models to predict prognosis in patients with implantable cardioverter defibrillators with or without cardiac resynchronization therapy. Am J Cardiol 119:1414–1420
Abete P, Testa G, Della-Morte D et al (2013) Treatment for chronic heart failure in the elderly: current practice and problems. Heart Fail Rev 18:529–551
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest regarding to publishing this article.
Ethical approval
The study design was approved by the Health Sciences University Ethics Committee.
Informed consent
Fort his type of study, formal consent is not required.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Not applicable. The study has a retrospective design.
Consent to publication
All authors gave explicit consent to submit and publish the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hayıroğlu, M.İ., Çınar, T., Çinier, G. et al. Comparison of mortality prediction scores in elderly patients with ICD for heart failure with reduced ejection fraction. Aging Clin Exp Res 34, 653–660 (2022). https://doi.org/10.1007/s40520-021-01960-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-01960-6