Abstract
Background
Although chest pain and acute coronary syndrome (ACS) are among the most common complaints in the Emergency Departments (ED), little is known about this topic in the octogenarian population.
Objectives
This study aimed to describe the clinical presentation and to evaluate survival time according to the ACS type in a group of 80-year-old or over patients admitted for chest pain to an ED.
Methods
Patients were classified according to the discharge diagnosis. A multivariable Cox regression analysis was done to assess the association between ACS type and mortality with the non-ACS chest pain group as the reference category.
Results
ACS was diagnosed in 170 of the 391 patients analyzed and 51% of ACS patients were female. Within the ACS patients, 18.8% presented STEMI, 57% NSTEMI, and 24% unstable angina (UA). Most of the patients were treated conservatively. In the adjusted analysis, the incidence of death at 40 months of follow-up was higher in patients with STEMI (HR 3.24; CI 1.59–6.56) than NSTEMI (HR 2.53; CI 1.56–4.11). There was no difference between patients with UA and the non-ACS group (HR 0.64; CI 0.26–1.58), and myocardial revascularization was associated with reduced mortality risk (HR 0.45; CI 0.22–0.92).
Conclusions
A high prevalence of ACS was found among octogenarians admitted to the ED with chest pain, and the ACS type behaved as an independent predictor of mortality. Patients with UA diagnosis had a similar prognosis to patients with non-ACS chest pain, but this needs to be demonstrated by a prospective study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary arterial disease (CAD) incidence increases proportionally to age [1], and chest pain is a common presenting complaint in Emergency Departments (EDs). As such, an increase in the number of geriatric patients with acute coronary syndrome (ACS) in EDs is expected [2]. Diagnosing ACS in elderly patients with chest pain is a difficult task because they may not present with pathognomonic symptoms [3, 4], leading to a late diagnosis with a greater possibility of adverse outcomes [5].
Conversely, age is one of the most important predictors of mortality in patients with ACS [6]: elderly patients frequently have a greater number of comorbidities and a lower probability of receiving reperfusion therapy [7, 8]. Additionally, complications such as reinfarction, heart failure, cerebrovascular accident, kidney failure, and bleeding are more frequent in this population [9]. In geriatric patients, antithrombotic overdosing is a frequent event [10], and many of them are contraindicated for evidence-based treatments. In a study that included nonagenarians with non-ST segment elevation (NSTE)-ACS, 10–15% had contraindications for aspirin, beta-blockers, and statins, and up to 20% had contraindications for angiotensin-converting enzyme (ACE) inhibitors [9].
Despite the importance of this situation, octogenarians are poorly represented in clinical trials [11], and due to a selection bias, the included population may not represent this age group very well [12]. Likewise, the representation of this population in clinical trials such as the TRITON-TIMI 38 was only 13% [13], and 15% in the PLATO trial [14]. Although some studies have tried to address this problem [15], the frequency of ACS in octogenarian patients with chest pain from suspect cardiac etiology in EDs is unknown. There are also no studies that address the prognosis in terms of survival according to the ACS type in a geriatric population over 80 years old. Given all these reasons and the lack of available information, the goal of this study was to describe the clinical presentation and to evaluate survival time according to the ACS type in a group of octogenarians admitted for chest pain to an ED.
Materials and methods
Type of study
A retrospective cohort study was conducted at the Auna Clínica Las Américas, a high-complexity cardiovascular reference center in Medellín, Colombia. This center has recognized experience in the care of patients with cardiovascular diseases and has a well-structured emergency department and a 17-bed coronary care unit. The study protocol was classified as a risk-free investigation and approved by the institutional Research Ethics Committee.
Population and definitions
All patients aged 80 or over admitted to the ED for chest pain and suspected of ACS from January 1, 2016, to December 31, 2016, were included. Symptoms considered suggestive of SCA included chest pain described as discomfort, heaviness, tightness, pressure, burning, numbness, fullness, or tightness in the chest. Other symptoms considered suggestive of myocardial ischemia included pain or discomfort in the arms, neck, jaw or epigastrium. Patients who did not have an electrocardiogram (ECG) or a cardiac troponin (cTn) measured were excluded. The patients were classified according to the discharge diagnosis into four groups: ST segment elevation myocardial infarction (STEMI), non-ST segment elevation myocardial infarction (NSTEMI), unstable angina (UA), and non-ACS chest pain. The cases with doubts about the final diagnosis were reviewed by a second clinical cardiologist who was not part of the study. STEMI was definite by an ST elevation at the J point in two anatomically contiguous leads (1 mm in all leads other than V2–V3 where the diagnostic thresholds applied were ≥ 2 mm in men or 01.5 mm in women). NSTEMI was definite by non-ST elevation in ECG with at least one high-sensitivity troponin I (hs-cTnI) result > P99 (percentile 99th) in a patient with symptoms suggestive of cardiac ischemic. UA was considered in patients with symptoms suggestive of ACS and hs-cTnI result < P99. All hs-cTnI measurements were made with ARCHITEC® (Abbott Laboratories), which has a P99 threshold defined as 16 ng/L in females and 34 ng/L in males, and an LD (limit of detection) 2 ng/L. At the institution where the study was carried out, an algorithm is used at the diagnostic of acute myocardial infarction (AMI) in the ED. According to the algorithm, if the first hs-cTnI result is below the LD, the AMI diagnosis is ruled out, and when the first hs-cTnI result is between LD and P99, a second measurement is required.
Data recollection
Information about demographic characteristics, comorbidities, and clinical variables was obtained from medical records through a case report form (CRF), which was reviewed by the investigators and transferred to a database designed specifically for the study. The data on vital status and date of death were obtained directly from a national record (Registraduría Nacional del Estado Civil de Colombia).
Statistical analyses
Distributions of quantitative variables were described as means (± SD) or by the median and interquartile range (IQR) according to the assumption or not of the normality and compared by using the T test, Mann–Whitney U test or Kruskal–Wallis test as appropriate. Qualitative variables were summarized by count and percentage and compared with the use of the Chi-square test or Fisher’s exact test when necessary. For survival analysis differences in time-to-event, distributions were evaluated employing the log-rank test. A hazard estimator with a 95% confidence interval (CI) was calculated through a Cox regression. For Cox regression analyses, the exposure of interest was the ACS type, and the primary outcome was time to death. To provide adjusted measures of association between ACS type and mortality, the statistically significant variables in the univariable analysis, and other biological plausible confounders were included in the multivariable analysis. The proportional hazards assumption was tested through log–log curves and the Schoenfeld residual test. Data were managed with the Stata statistical package, version 14.2, and a two-sided p value of less than 0.05 was considered indicative of statistical significance.
Results
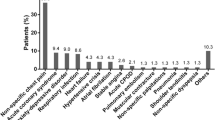
During the study period, 2968 adult subjects were admitted to the ED for chest pain and suspected cardiac ischemia; ACS was diagnosed in 820 of them (27.6%). In total, 391 (13.2%) subjects aged 80 years or older had a 12-lead ECG and at least one hs-cTnI measurement, and were included in this analysis. ACS was diagnosed in 170 (43.5%) of these patients and ruled out in 221 of them (non-ACS chest pain group). A second hs-cTnI measurement was taken in 90 (40.7%) of the non-ACS patients, transthoracic echocardiography in 136 (61.5%) and cardiac stress testing in 31 (14%) cases. Other tests for the study of chest pain in non-ACS patients included X-rays, tomography, ultrasound, and blood tests as was necessary. The most frequent discharge diagnoses among non-ACS patients were hypertensive crisis (25.8%), atrial fibrillation/flutter (13%), acid peptic disease (6.3%), and other multiple diseases such as heart failure, pneumonia, pulmonary embolism, sinus dysfunction, abdominal pain, muscle pain, chondritis, cholelithiasis, and sepsis; each one represented < 5% of cases.
Fifty-one percent of the ACS patients were female (n = 87), and the distribution of ACS patients was as follows: 32 presented as STEMI (18.8%), 97 NSTEMI (57%), and 41 corresponded to unstable angina (24%). Table 1 shows the characteristics of the patients classified according to ACS and non-ACS status. In general, a higher proportion of patients were female in STEMI (56%), NSTEMI (62.9%), and the non-ACS group (70.6%). No differences were observed in the median age between groups. Former or current cigarette smoking was more frequent in ACS patients compared with non-ACS patients. Similarly, previous dyslipidemia and chronic kidney disease (CKD) were more frequent in the ACS groups, while a history of MI and previous revascularization were more frequent in unstable angina (UA) patients (60.9% and 58%, respectively). The median time from symptom onset to admission was similar in patients with STEMI, UA, and non-ACS compared with the NSTEMI group which had double the time of the other groups (Table 2).
Invasive strategy
Only 60 of the 170 patients with ACS (35%) underwent coronary angiography. The most frequent reasons for not doing coronarography were older age, individual criteria of the cardiologist, and in some cases, a stress echocardiography result. The mean age of patients undergoing angiography was 82.7 ± 4.5 years compared to 85.9 ± 2.7 years in patients in conservative strategy (p value < 0.001). Within the invasive strategy group, there was a higher proportion of STEMI diagnosis and a lower proportion of kidney failure and heart failure (Fig. 1). Percutaneous coronary intervention (PCI) was performed on 39 (65%) patients undergoing to coronarography and coronary artery bypass graft (CABG) on 4 (7%) patients. Nonrevascularizable CAD was found in ten (16.7%) and coronary arteries without obstructive lesions in seven (11.7%) of the subjects.
Comparison of patients with ACS according to coronary angiographic realization. CABG coronary artery bypass graft surgery, GFR glomerular filtration rate, HF heart failure, NSTEMI non-ST elevation myocardial infarction, PCI percutaneous coronary intervention, STEMI ST elevation myocardial infarction, UA unstable angina
Survival analysis
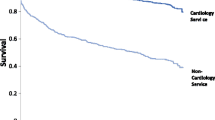
To assess the effect of ACS in octogenarians’ survival, mortality from any cause was evaluated after a median follow-up of 40 months (IQR 27.7 to 45), using the type of ACS (STEMI, NSTEMI, or UA) as the main exposure. Figure 2 shows the estimations of the incidence of death over time, according to the Kaplan–Meier method. The greatest incidence of death occurred in STEMI and NSTEMI groups and the lowest incidence in the UA group. The differences were statistically significant (log-rank test p value < 0.001). Table 3 shows the results of the univariate and multivariate analyses. For this analysis, the ACS type was defined like STEMI, NSTEMI, and UA using the non-ACS chest pain group as a reference category as was explained in “Materials and methods”. In the univariate analysis, a gradient association was found between the ACS type and the mortality risk. Taking the non-ACS as the reference category, no difference was observed with the UA group, while the NSTEMI and STEMI groups had a higher risk. A significant association was also found between risk of death and variable age (HR 1.07; 95% CI 1.03–1.11), glomerular filtration rate (GFR) (HR 0.98; 95% CI 0.97–0.99), and left ventricular ejection fraction (LVEF) (HR 0.97; 95% CI 0.95–0.98). Current myocardial revascularization showed no significant trend towards a decreased risk of death in the univariate analysis (HR 0.81; 95% CI 0.46–1.43), but this association became statistically significant in the multivariate analysis (HR 0.45; 95% CI 0.22–0.92).
To evaluate the independent effect of ACS type on mortality, we carried out an analysis adjusted for variables that showed a significant association in the univariate analysis [age, GFR and LVEF]. Because of their plausible association with the outcome, the variable diabetes and myocardial revascularization were also included in the multivariate model (Table 3). In the adjusted estimation, the gradient between the ACS type and the risk of death was maintained even after adjusting for the covariate. Table 4 shows the incidence rate of death and adjusted hazard ratio estimation according to ACS type. No difference was observed between the UA and the non-ACS group (HR 0.64; 95% CI 0.26–1.58). Patients in the NSTEMI group had an increased risk of death (HR 2.53; 95% CI 1.56–4.11) and the STEMI group had a higher risk of mortality (HR 3.24; 95% CI 1.59–6.56). For multivariate analysis, the proportional hazard assumption was verified (Schoenfeld residual test with a p value of 0.670 for the complete model).
Discussion
In this cohort of octogenarians admitted to the ED for chest pain and suspected of cardiac ischemia, ACS was diagnosed in 43.5% of the patients. The type of ACS behaved as an independent predictor of mortality, with STEMI and NSTEMI diagnoses being independent predictors of mortality at 40 months of follow-up. Patients with UA had a similar prognosis to those with non-ACS chest pain and that behavior persisted even after the adjustment for age, sex, diabetes, GFR, LEVF, and myocardial revascularization.
Although other studies have evaluated geriatric chest pain patients in the ED [15], this is the first study to present the prevalence, ACS type, and survival prognosis in an octogenarians cohort with chest pain suspected of myocardial ischemia and admitted to the ED. We observed a high proportion of ACS diagnosis with a high number of women in the STEMI, NSTEMI and non-ACS chest pain groups. This contrasts with previous publications in which a low proportion of women with STEMI has been observed in the general population [11, 16,17,18,19,20,21,22,23]. Other studies that have exclusively included the elderly have also found a higher proportion of men [7, 8, 24,25,26,27]. However, in large cohorts of octogenarians, the female sex was predominant in those with AMI [9, 12, 28,29,30], a biologically plausible finding due to the tendency in women to present ACS at an older age [31]. Similar to other studies [9, 28,29,30], factors such as smoking, dyslipidemia, and CKD behaved as frequent risk markers in geriatric people with ACS compared to those with non-ACS chest pain. Strikingly, we observed a median time from the onset of pain to the first medical contact (FMC) of almost 22 h in patients with NSTEMI compared to a time of between 9 and 11 h in the other groups. Another publication has also reported a prolonged time to FMC in elderly patients [7].
The type of ACS behaved as an independent predictor of mortality in octogenarian patients, with STEMI and NSTEMI diagnoses being independent predictors of mortality in the medium term, just as has been found in previous studies [8, 9, 11, 12, 25, 27, 29, 32,33,34]. Although the myocardial revascularization seemed to decrease the risk of death in the multivariate analysis, these results are not interpretable because most of the patients received conservative treatment, and the patients in invasive strategy were carefully selected. It has been found in different studies that geriatric patients are less likely to undergo an invasive strategy [8, 9, 11, 12, 27, 29, 32,33,34,35], and it should be remembered that the benefits of routine revascularization in octogenarians are controversial. While some studies support a reduction in mortality [8, 24, 27, 32, 36, 37], others have found no benefits [38, 39] and the follow-up of studies that have tested the invasive strategy in the elderly population has varied between 6 months [27, 36] and 1 year [24], so the real impact of long-term revascularization in this age group remains unknown. Based on our results, we consider that the treatment strategy in octogenarians with ACS should be individualized. Due to the complexity of caring for this age group, it is necessary to consider, in addition to biological age, aspects such as cognitive and functional compromise, as well as the fragility of the patient [12, 40,41,42].
The most remarkable finding of our research was that after 40 months of follow-up, patients aged 80 years or older with UA had a similar prognosis to those with non-ACS chest pain and that behavior persisted even after the adjustment for age, sex, diabetes, GFR, LEVF, and myocardial revascularization. This counterintuitive finding has a very likely explanation. Several decades ago, a group of patients with severe, prolonged anginal pain at rest that differed from stable angina, but sometimes preceded AMI, was described [43, 44]. The analytic sensitivities of the assays for cTn have improved progressively during the past years, and cTn has become detectable in an even larger fraction of patients, reducing the proportion of ACS patients with UA [45]. This reclassification of patients is of clinical importance because it increased the diagnosis of AMI among patients with acute chest pain: patients recently classified as having MI are treated more aggressively and their clinical outcomes have improved [46]. It is now evident that a large majority of patients with clinical manifestations of myocardial ischemia, with chest pain but without elevated circulating cTn measured by a conventional assay and, therefore, considered to have UA have an elevated cTn measured by a high-sensitivity cTn assay and are classified as NSTEMI nowadays. As a consequence, UA is likely to be a further marginalized diagnosis, and patients with a diagnosis of UA actually have a good prognosis [47]. For some experts, it is not clear that ACS events can occur without some increase in circulating high-sensitivity cTn assay [48]. This hypothesis could explain why we found similar survival rates between geriatrics patients with UA and those with non-ACS chest pain, but this needs to be demonstrated by a prospective study.
Limitations
This study has some important limitations. First, the patients were not prospectively enrolled in a specific manner for the clinical investigation, and the sample is not necessarily representative of the entire population of octogenarians admitted to the ED because this was a single-center study. Second, we were unable to determine the cause of death in most patients, so we were only able to measure the overall mortality rate. Finally, no indicators of functionality or fragility of patients were measured and few patients underwent coronarography; as in any nonexperimental study, it is not possible to eliminate the bias corresponding to residual confounding or time-dependent variables that were not measured.
Conclusions
A high prevalence of ACS was observed among octogenarian chest pain patients in an ED, with a high proportion of female patients. The ACS type behaved as an independent predictor of mortality at 40 months of follow-up and myocardial revascularization was associated with reduced mortality though this finding is subject to selection bias in this small subset. Patients with a diagnosis of UA had a similar prognosis to patients with non-ACS chest pain but it needs to be demonstrated by a prospective study.
References
Lerner DJ, Kannel WB (1986) Patterns of coronary heart disease morbidity and mortality in the sexes: A 26-year follow-up of the Framingham population. Am Heart J 111:383–390
Madhavan MV, Gersh BJ, Alexander KP et al (2018) Coronary artery disease in patients ≥ 80 Years of age. J Am Coll Cardiol 71:2015–2040
Wilson M, Welch J, Schuur J et al (2014) Hospital and emergency department factors associated with variations in missed diagnosis and costs for patients age 65 years and older with acute myocardial infarction who present to emergency departments. Acad Emerg Med 21:1101–1108
Solomon CG, Lee TH, Cook EF et al (1989) Comparison of clinical presentation of acute myocardial infarction in patients older than 65 years of age to younger patients: the multicenter chest pain study experience. Am J Cardiol 63:772–776
Brieger D, Eagle KA, Goodman SG, White et al (2006) Chest pain, an underdiagnosed and undertreated high-risk group *. CHEST J-Am Coll Chest Physicians 125:461–469
Fox KAA, Eagle KA, Gore JM et al (2010) The global registry of acute coronary events, 1999 to 2009-GRACE. Heart 96:1095–1101
Toleva O, Ibrahim Q, Brass N et al (2015) Treatment choices in elderly patients with ST: elevation myocardial infarction—insights from the vital heart response registry. Open Hear 2:e000235
Malkin CJ, Prakash R, Chew DP (2012) The impact of increased age on outcome from a strategy of early invasive management and revascularisation in patients with acute coronary syndromes: retrospective analysis study from the ACACIA registry. BMJ Open 2:1–7
Skolnick AH, Alexander KP, Chen AY et al (2007) Characteristics, management, and outcomes of 5557 Patients Age ≥ 90 years With Acute Coronary Syndromes. Results From the CRUSADE Initiative. J Am Coll Cardiol 49:1790–1797
Alexander KP, Chen AY, Roe MT et al (2005) Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. J Am Med Assoc 294:3108–3116
Hochman JS, Tamis JE, Thompson TD et al (1999) Sex, Clinical presentation, and outcome in patients with acute coronary syndromes. Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators. N Engl J Med 341:226–232
Alexander KP, Newby LK, Cannon CP et al (2007) Acute coronary care in the elderly, part I. Non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American heart association council on clinical cardiology. Circulation. 115:2549–2569
Wiviott SD, Braunwald E, McCabe CH et al (2007) Prasugrel versus Clopidogrel in Patients with Acute Coronary Syndromes. N Engl J Med 357:2001–2015
Wallentin L, Becker RC, Budaj A et al (2009) Ticagrelor versus Clopidogrel in Patients with Acute Coronary Syndromes. N Engl J Med 361:1045–1057
Madsen TE, Fuller M, Hartsell S et al (2016) Prospective evaluation of outcomes among geriatric chest pain patients in an ED observation unit. Am J Emerg Med 34:207–211
Jneid H, Fonarow GC, Cannon CP et al (2008) Sex differences in medical care and early death after acute myocardial infarction. Circulation 118:2803–2810
Maynard C, Litwin PE, Martin JS, Weaver WD (1992) Gender differences in the treatment and outcome of acute myocardial infarction: results from the myocardial infarction triage and intervention registry. Arch Intern Med 152:972–976
Chiriboga DE, Yarzebski J, Goldberg RJ et al (1993) A community-wide perspective of gender differences and temporal trends in the use of diagnostic and revascularization procedures for acute myocardial infarction. Am J Cardiol 71:268–273
Fiebach NH, Viscoli CM, Horwitz RI (1990) Differences between women and men in survival after myocardial infarction: biology or methodology? JAMA J Am Med Assoc 263:1092–1096
Robinson K, Conroy RM, Mulcahy R (1988) Risk factors and in-hospital course of first episode of myocardial infarction or acute coronary insufficiency in women. J Am Coll Cardiol 11:932–936
Kostis JB, Wilson AC, O’Dowd K et al. (1994) Sex differences in the management and long-term outcome of acute myocardial infarction: a statewide study. Circulation. 90:1715–30.
Clarke KW, Gray D, Keating NA et al (1994) Do women with acute myocardial infarction receive the same treatment as men? BMJ 309:563
Greenland; P, Reicher-Reiss H, Goldbourt et al. (1991) In-hospital and 1-year mortality in 1, 524 women after myocardial infarction. Circulation. 83:484–91.
Bauer T, Koeth O, Jünger C et al (2007) Effect of an invasive strategy on in-hospital outcome in elderly patients with non-ST-elevation myocardial infarction. Eur Heart J 28:2873–2878
Jaguszewski M, Ghadri JR, Diekmann J et al (2014) Acute coronary syndromes in octogenarians referred for invasive evaluation: treatment profile and outcomes. Clin Res Cardiol 104:51–58
Bueno H, Betriu A, Heras M et al. (2011) Primary angioplasty vs. fibrinolysis in very old patients with acute myocardial infarction: TRIANA (TRatamiento del Infarto Agudo de miocardio en Ancianos) randomized trial and pooled analysis with previous studies. Eur Heart J. 32:51–60.
Devlin G, Gore JM, Elliott J et al (2008) Management and 6-month outcomes in elderly and very elderly patients with high-risk non-ST-elevation acute coronary syndromes: the global registry of acute coronary events. Eur Heart J 29:1275–1282
Saunderson CED, Brogan RA, Simms AD et al (2014) Acute coronary syndrome management in older adults: Guidelines, temporal changes and challenges. Age Ageing 43:450–455
Mehta RH, Rathore SS, Radford MJ et al (2001) Acute myocardial infarction in the elderly: differences by age. J Am Coll Cardiol 38:736–741
Amsterdam EA, Kirk JD, Bluemke DA et al (2010) Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation 122:1756–1776
Regitz-Zagrosek V, Oertelt-Prigione S, Prescott E et al (2016) Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J 37:24–34
Vandecasteele EH, De Buyzere M, Gevaert S et al (2013) Reperfusion therapy and mortality in octogenarian STEMI patients: results from the Belgian STEMI registry. Clin Res Cardiol 102:837–845
Haase KK, Schiele R, Wagner S et al (2000) In-hospital mortality of elderly patients with acute myocardial infarction: data from the mitra (Maximal individual therapy in acute myocardial infarction) registry. Clin Cardiol 23:831–836
Alexander KP, Newby LK, Armstrong PW et al (2007) Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American heart association council on clinical cardiology. Circulation 115:2570–2589
Fox KAA, Clayton TC, Damman P et al (2010) Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome. A meta-analysis of individual patient data. J Am Coll Cardiol 55:2435–2445
Bach RG, Cannon CP, Weintraub WS (2004) The effect of routine, early invasive management on outcome for elderly patients with non-ST-segment elevation acute coronary syndromes. ACC Curr J Rev 13:53–54
Saraswat A, Rahman A, Singh K (2018) An invasive vs a conservative approach in elderly patients with non-ST-segment elevation myocardial infarction: systematic review and meta-analysis. Can J Cardiol 34:274–280
Savonitto S, Cavallini C, Petronio AS et al (2012) Early aggressive versus initially conservative treatment in elderly patients with non–ST-segment elevation acute coronary syndrome: a randomized controlled trial. JACC Cardiovasc Interv 5:906–916
Tegn N, Abdelnoor M, Aaberge L et al (2016) Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study): an open-label randomised controlled trial. Lancet 387:1057–1065
Pemberthy-López C, Jaramillo-Gómez N, Cardona-Vélez J et al (2016) Estratificación de riesgo para enfermedad coronaria en adultos mayores. Rev Colomb Cardiol 23:286–292
Afilalo J, Alexander KP, Mack MJ et al (2014) Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol 63:747–762
Ekerstad N, Swahn E, Janzon M et al (2011) Frailty is independently associated with short-term outcomes for elderly patients with non-ST-segment elevation myocardial infarction. Circulation 124:2397–2404
Sampson JJ, Eliaser M (1937) The diagnosis of impending acute coronary artery occlusion. Am Heart J 13:675–686
Feil H (1937) Preliminary pain in coronary thrombosis. Am J Med Sci 193:42–47
Bonaca M, Scirica B, Sabatine M et al (2010) Prospective evaluation of the prognostic implications of improved assay performance with a sensitive assay for cardiac troponin I. J Am Coll Cardiol 55:2118–2124
Mills NL, Churchhouse AMD, Lee KK et al (2011) Implementation of a sensitive troponin I assay and risk of recurrent myocardial infarction and death in patients with suspected acute coronary syndrome. JAMA 305:1210–1216
Mahmoud O, Mahmaljy H, Youniss M et al. (2020) Comparative outcome analysis of stable mildly elevated high sensitivity troponin T in patients presenting with chest pain. A single-center retrospective cohort study. IJC Hear Vasc 30:100586
Braunwald E, Morrow DA (2013) Unstable angina is it time for a requiem? Circulation 127:2452–2456
Acknowledgements
We are grateful to the non-invasive cardiology service, the hemodynamic laboratory, and the clinical laboratory of Auna Clínica las Américas.
Funding
Not applicable. This work was supported by the authors' own resources. We did not receive grants, contracts or other forms of financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Not applicable. On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Ethics approval
The study protocol was classified as a risk-free investigation and approved by the Institutional Research Ethics Committee.
Consent to participate
Not applicable. This was a retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Díaz-Betancur, J.S., Martínez, J., Zapata, J. et al. Chest pain and acute coronary syndrome in octogenarians admitted to the Emergency Department. Aging Clin Exp Res 33, 2213–2221 (2021). https://doi.org/10.1007/s40520-020-01737-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01737-3