Abstract
Background and aims
This study aimed to investigate the association between cumulative C-reactive protein (cumCPR) and arterial stiffness.
Methods
The cross-sectional study included 15,432 participants from the Kailuan Cohort. The participants were divided into four groups according to cumCRP quartiles. The average brachial–ankle pulse wave velocity (baPWV) and detective rate of increased arterial stiffness were compared between exposure groups. Statistical analysis was performed with multiple logistic regression analysis to estimate the association between cumCRP and arterial stiffness by calculating the odds ratios (ORs) and 95% confidence intervals (CIs). The several sensitivity analyses were performed to test the robustness of our findings.
Results
The average baPWV increased from 1425.70 cm/s of Q1 group to 1626.48 cm/s of Q4 group. And the detective rate of arterial stiffness increased from 44.7 to 70.1% (P < 0.001). Multiple logistic regression analysis showed that after adjusting the confounding factors, compared to the Q1 group, the Q4 group had 42% (adjusted OR 1.42; 95% CI 1.24–1.63) higher arterial stiffness risk. In addition, 10% (adjusted OR 1.10; 95% CI 1.02–1.18) arterial stiffness risk was increased per 1 standard deviation (SD) of cumCRP after a fully adjusted regression model.
Conclusion
Higher cumCRP exposure is associated with increased arterial stiffness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arteriosclerosis is associated with increased cardiovascular events [1], and also an independent predictor of these events [2, 3]. Arteriosclerosis decreases arterial elasticity and increases arterial stiffness, which shows that the pulse wave velocity (PWV) increases clinically. Carotid-femoral PWV is frequently considered as the standard measurement of arterial stiffness [4]. Inflammation plays an important role in the genesis and development of arteriosclerosis. And C-reactive protein (CRP) is one of the most sensitive markers of inflammation and tissue damage [5, 6]. Furthermore, numerous studies have shown that CRP is an independent risk factor of increased PWV among populations with metabolic syndrome, acute coronary syndrome, hypertension, and severe asthma [7,8,9,10,11,12].
The association between inflammation marker CRP and PWV has been confirmed; however, most of the related studies only using a single CRP concentration measurement to explore their association. Furthermore, serum CRP can be influenced by many factors, such as age, gender, race, lifestyle, and infections [13, 14]. Therefore, using a single CRP would not accurately reflect the association between CRP and PWV. Cumulative C-reactive protein (cumCPR) considers exposure dose and time sufficiently, and it is more precise than a single CRP. To the best of our knowledge, few studies concerning the association between cumCRP and brachial–ankle pulse wave velocity (baPWV). The Kailuan study (Trial identification: ChiCTR-TNC-11001489) was based on the risk factors of cardiovascular diseases in a functional community. The community received comprehensive cardiovascular risk factor assessments including CRP and baPWV, which can be used to analyze the association between cumCRP and baPWV.
Materials and methods
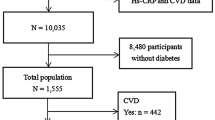
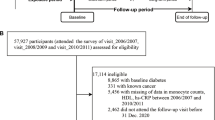
Population
We collected the data from the Kailuan community in Tangshan, a city in northern China. This community represented the Chinese population from a socioeconomic perspective. The Kailuan study is composed of independent data set from the staff of Kailuan community and also is an ongoing prospective cohort study which medical examination started in 2006–2007 in Tangshan. Detailed study design and procedures have been published previously [15]. Briefly, between 2006–2007 and 2007–2010 (visit 1), there were 101,510 participants (81,110 males and 20,400 females) were recruited from 11 hospitals of Kailuan community. All participants were then underwent repeated questionnaire assessment, clinical and laboratory tests every 2 years, i.e., in the years 2008 and 2009 (visit 2), in the years 2010 and 2011 (visit 3). Among them, 22,622 participants underwent baPWV assessment between 2010 and 2015. In our study, we excluded 7190 participants who lack of data for any two CRP values of the three medical examinations. Finally, 15,432 participants included in our analysis.
The protocol for this study was performed according to the guidelines of the Helsinki Declaration and approved by the Ethics Committee of the Kailuan Medical Group, Kailuan Company. All of the participants provided written informed consent.
Epidemiological survey and anthropometric parameters
The epidemiological survey and anthropometric parameters were in accordance with the previous published articles by our research group [16]. CRP was measured by high-sensitivity nephelometry assay (Cias Latex CRP-H, Kanto Chemical, Tokyo, Japan). All blood samples were tested using an auto-analyzer (Hitachi 747; Hitachi, Tokyo, Japan) in the central laboratory of Kailuan General Hospital. The laboratory proficiency testing value was 100%, as assessed by the Ministry of Health in 2006–2009. The two other samples were tested twice a day with 2 h intervals and lasted for 20 days. The precision was evaluated using a Hitachi 7600 automatic biochemical analyzer. Smoking was defined as having at least one cigarette a day in the recent years; drinking was defined as having 100 ml/day (alcohol content > 50%) for more than 1 year; physical training was defined as having aerobic exercise (e.g., walking, jogging, balls, and swimming) for ≥ 3 times/week at ≥ 30 min/time.
Assessment of baPWV and ankle brachial index (ABI)
All the baPWV and ABI data were read from BP-203RPEIII Internet (Oumulong). The temperature of the examination room was stable at 22 °C to 25°. And smoking was not allowed and more than 5 min of rest was essential prior to the test. Age, gender, height, and weight of forehead were recorded. At the beginning of the measurement, the participant stayed calm and laid horizontally, and then keep the blood pressure cuffs which were attached to the upper arm and ankle, at the same time, with the balloon sign of the upper arm cuff aligned with the brachial artery, and guaranteed the balloon sign of the leg cuff placed preaxially. The cardiechema collecting device was placed at the precordial region, with the electrocardiography acquisition device clipped to left and right wrists. The specific measurement method in detail can be found in the published paper of our research group [17]. The test was repeated twice and the second readings were considered the final value. The larger values of the left-side and right-side baPWV and the smaller values of the left-side and right-side ABI were used for further analysis. BaPWV < 1400 cm/s was considered as normal and baPWV ≥ 1400 cm/s was considered as arterial stiffness [18]. And the reproducibility of PWV measurement was evaluated by professionals trained by Kailuan Research Kailuan General Hospital.
Assessment of cumCRP and mean arterial pressure (MAP)
CumCRP was calculated according to the method of cumulative exposure to heart rate [19] and blood pressure [20]. The formula was as follows: cumCRP = [(CRP1 + CRP2)/2 × time1–2] + [(CRP2 + CRP3)/2 × time2–3], where CRP1, CRP2 and CRP3 are the first, second, and third physical examinations for CRP, respectively; time1–2 and time2–3 are the time intervals of two adjacent measurements; and cumCRP is the cumulative C-reactive protein. Mean CRP (meanCRP) was calculated as follows: meanCRP = (CRP1 + CRP2 + CRP3)/3, where CRP1, CRP2, and CRP3 are the first, second and third physical examinations for CRP, respectively. MAP was calculated as follows [21]: MAP = (systolic pressure + 2×diastolic pressure)/3.
Statistical analysis
Participants were divided into four groups according to the quartile of cumCRP exposure levels. The physical examination data from 2006 to 2007, 2008 to 2009, and 2010 to 2011 were extracted by professional workers and used in creating an Oracle 10.2 database (Oracle, USA). BaPWV data were established into a database by Epidata 3.0 (EpiData Association, Denmark), and analyses were performed using SPSS 13.0 (IBM, USA). Data in normal distribution were presented as mean ± standard deviation (x ± s). Measurement data in multiple groups were compared with one-way ANOVA and LSD-t/Dunnett’s T test. When the participants lost any CRP measurement of the three examinations (n = 3499), we used the average value of the other two results. Mean CRP was in a skewed distribution and logarithmically transformed. Some CRP values presented 0 and could not be logarithmically transformed. Thus, we used 0.05 mg/L for calculation. These values showed normal distribution after logarithmic transformation and were analyzed by variance. Enumeration data were presented as N (%). Intergroup and rate comparisons were conducted using Chi-square test. Multivariable logistic regression analysis was applied to analyze the influence of different cumCRP groups and the increase in each standard deviation on baPWV. P < 0.05 was considered statistically significant. To avoid the influence of acute inflammation, infection, lipid-lowering agent, diabetes, hypertension, cardiovascular disease, and peripheral arterial diseases, we applied sensitivity analysis as follows: (i) exclusion of CRP > 10 mg/L, (ii) exclusion of those taking lipid-lowering agents, (iii) exclusion of those with hypertension, diabetes, and cardiovascular diseases when taking the first physical examination in 2006 and new onset during 2006–2010, (iv) exclusion of ABI < 0.9 and (v) CRP values were completed in three examinations.
Results
Participant characteristics
The participants (n = 15,432) with 61.2% male (n = 9443) and 38.8% female (n = 5989) had a mean age of 51.52 ± 11.11 years at the baseline. The four groups of cumCRP were: Q1: cumCRP < 2.72 mg/L year; Q2: 2.72 < cumCRP < 5.08 mg/L year; Q3: 5.08 < cumCRP < 9.60 mg/L year; Q4: cumCRP3 > 9.60 mg/L year. When the cumCRP increased from Q1 to Q4, the age, heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), MAP, Visit1_lgCRP, Visit2_lgCRP, Visit3_lgCRP, lgmeanCRP, body mass index (BMI), fasting blood glucose (FBG), TC, low-density lipoprotein cholesterin (LDL-C), physical training, hypertension, diabetes, and use of hypotensive drugs and lipid-lowering drugs were significant increases (P < 0.001, respectively) (Table 1). And we also compared the characteristics of participants between inclusion and exclusion population at the baseline (Supplementary Table 1).
The mean baPWV and corresponding incidence of arterial stiffness of each group
The mean baPWV values of each group were 1425.70, 1499.54, 1557.62, and 1626.48 cm/s, respectively. From Q1 to Q4, the corresponding incidence of arterial stiffness was 44.7%, 55.5%, 61.5%, and 70.1% (P < 0.001). Results were the same in the male and female groups and showed statistical significance (P < 0.001) (Table 2).
Multivariable logistic regression analysis of the arterial stiffness
Using arterial stiffness as the dependent variable, cumCRP or cumCRP (+1SD) was the independent variable (Q1 was the control group) in the multivariable logistic regression analysis. In model 3, after adjusted for age, gender, BMI, LDL-C, FBG, baseline CRP, MAP, smoking, alcohol intake, physical exercise, the OR was 1.42 (95% CI 1.24–1.63) of Q4. Of note, in a fully adjusted regression model, when the cumCRP increased per SD, the OR was 1.10 (95% CI 1.02–1.18) (Table 3).
In addition, the baseline CRP quartiles also exhibited a predictive value for arterial stiffness (Supplementary Table 2).
Sensitivity analysis
We conducted the sensitivity analysis as follows: (i) exclusion of CRP > 10 mg/L, (ii) exclusion of those taking lipid-lowering agents, (iii) exclusion of hypertension, diabetes, and cardiovascular diseases when taking the first physical examination in 2006 and the new onset during 2006–2010, (iv) exclusion of ABI < 0.9, and (v) CRP values were completed in three examinations. Results were in agreement with those previously described (Table 4).
Discussion
Age, SBP, FBG, smoking, HDL-C, and other related factors were well established associated with arterial stiffness [22,23,24,25], and inflammation played a vital role in the development and progression of article stiffness. We discovered that with cumCRP increased, the incidence of article stiffness and mean value of baPWV also increased. The incidence of arterial stiffness of Q1 and Q4 was 44.7% and 70.1%, respectively. The mean value of Q1 was 1425.70 cm/s and that of Q4 was 1626.48 cm/s. The trend existed in different gender groups. These results were similar to an early cross-sectional study about the association between single CRP and baPWV. The cross-sectional study researched the middle-aged and elderly people in Japan, and found that the mean baPWV in males increased from 1358 cm/s (hs-CRP Q1) to 1381 cm/s (hs-CRP Q4) (P < 0.01) and that in females also increased from 1241 to 1266 cm/s [26].
After adjusting the confounding factors, the risk of arterial stiffness in the cumCRP exposure group increased by 1.42-fold more in Q4 than that in Q1. In addition, cumCRP increased per standard deviation, and the risk of arterial stiffness increased by 1.10-fold. Furthermore, the risk of arterial stiffness remained unchanged when cumCRP increased, except for those with CRP > 10 mg/L; taking lipid-lowering drugs; with hypertension, diabetes, and cardiovascular diseases; ABI < 0.9; and lacking any one of the CRP values. A prospective study concluded that in rheumatoid arthritis patients, the risk of arterial stiffness was high in the CRP ≥ 5.31 mg/L group, which is 4.84-fold higher than that in the CRP < 5.31 mg/L group [27].
In addition, we also found that there was association between the baseline CRP and arterial stiffness (Supplementary Table 2), but when baseline CRP was introduced into cumCRP quartiles (Table 3), no significance was observed in predicting arterial stiffness (OR= 1.0; 95% CI 0.99–1.02). Similarly, a study included 107 middle-aged males found that the baseline CRP has no relationship with baseline baPWV, and the results remained the same after 1 year of follow-up [28]. However, our results were contradictory to those of previous studies about the association between baseline CRP and arterial stiffness. McEniery et al. [29] studied 825 middle-aged males and pointed out that baseline CRP was both related to baseline aortic pulse wave velocity (aPWV) and aPWV of a 20-year follow-up. In another study that included 3769 Europeans which followed up 16 years, the baseline CRP was correlated with the aPWV of both genders [30]. Thus, single CRP measurement showed an unidentified relationship with PWV. This result might be because the single-time point measurement of CRP does not consider the long-lasting effects on the individual body. Our study applied the cumCRP measurement, which is made up of deficiencies, and might have precisely indicated the association between CRP exposure and arterial stiffness.
We discovered that higher cumCRP could promote the increase in baPWV and increase the incidence of arterial stiffness, and its possible pathogenesis is as follows: (1) as a biomarker of inflammation, CRP is related to the increased risk factors in cardiovascular diseases; in addition, baPWV is a sensitivity index of arteriosclerosis [31, 32] that could predict cardiovascular events [33,34,35]. Increased cumCRP expedited the baPWV, possibly by enhancing the risk factors of cardiovascular diseases. (2) CRP could suppress the mobilization and differentiation of endothelial progenitor cells (EPCs) and newly formed blood vessels by down-regulating the expression of endothelial nitric oxide synthesis. In addition, CRP could promote the apoptosis of endothelial cells. Endothelial cells receive no repairs for a prolonged period, which results in endothelial dysfunction and increases aortic stiffness [36, 37]. (3) CRP might be related with medial vascular calcification, which increases aortic stiffness and PWV [38,39,40,41]. CRP induces vascular endothelial injury in different ways. The damaged endothelial tissues affected with inflammatory factors exhibit hyaline degeneration and necrosis. Elastic fiber thickening and muscle fiber fracture may increase aortic stiffness. Such injury is a chronic pathological process, because it will take years for vascular sclerosis to occur.
Although we confirmed the association between cumCRP and baPWV among Chinese population, our analysis still has some limitations. First, the study population showed a weak balance in both genders, which might have influenced the representative effect of our cohort. The popularity remains to be confirmed. Second, although we adjusted the impact of various confounding factors in multivariable logistic regression analysis, several factors influencing the results were remain unadjusted, such as the white coat effect and the environmental changes. Third, the absence of CRP values (n = 3499) might have influenced the results accordingly, but we carried out a sensitivity analysis, and the results of which had no effect on our findings. Finally, our study only confirmed the association between cumCRP and arterial stiffness, but did not specifically determine their causal relationship.
In conclusion, our study provided that further evidence of high cumCRP exposure is associated with increased arterial stiffness.
References
Sawabe M (2010) Vascular aging: from molecular mechanism to clinical significance. Geriatr Gerontol Int 10:S213–S220
Karin Willeit, Stefan Kiechl (2014) Atherosclerosis and atrial fibrillation–two closely intertwined diseases. Atherosclerosis 233:679–681
Sutton-Tyrrell K, Najjar SS, Boudreau RM et al (2005) Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation 111:3384–3390
Pepys MB, Baltz ML (1983) Acute phase proteins with special reference to C-reactive protein and related proteins (pentaxins) and serum amyloid A protein. Adv Immunol 34:141–212
Laurent S, Cockcroft J, Van Bortel L et al (2006) Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 27:2588–2605
Libby P, Okamoto Y, Rocha VZ et al (2010) Inflammation in atherosclerosis: transition from theory to practice. Circ J 74:213–220
Yasmin, McEniery CM, Wallace S et al (2004) C-reactive protein is associated with arterial stiffness in apparently healthy individuals. Arterioscler Thromb Vasc Biol 24:969–974
Tsai SS, Lin YS, Lin CP et al (2015) Metabolic syndrome-associated risk factors and high-sensitivity C-reactive protein independently predict arterial stiffness in 9903 Subjects With and Without Chronic Kidney Disease. Medicine (Baltimore) 94:e1419
Oh EG, Kim SH, Bang SY et al (2012) High-sensitivity C-reactive protein is independently associated with arterial stiffness in women with metabolic syndrome. J Cardiovasc Nurs 27:61–67
Taverner D, Paredes S, Ferré R et al (2019) Assessment of arterial stiffness variables in patients with rheumatoid arthritis: a mediation analysis. Sci Rep 9:4543
Mahmud A, Feely J (2005) Arterial stiffness is related to systemic inflammation in essential hypertension. Hypertension 46:1118–1122
Sun WX, Jin D, Li Y et al (2014) Increased arterial stiffness in stable and severe asthma. Respir Med 108:57–62
Wu SL, Li JF, Li Y et al (2010) The distribution and influential factors of serum high sensitivity C-reactive protein in general population. Zhonghua Nei Ke Za Zhi 49:1010–1014
Sproston NR, Ashworth JJ (2018) Role of C-reactive protein at sites of inflammation and infection. Front Immunol 9:754
Zhang Q, Zhou Y, Gao X et al (2013) Ideal cardiovascular health metrics and the risks of ischemic and intracerebral hemorrhagic stroke. Stroke 44:2451–2456
Wu S, Huang Z, Yang X et al (2012) Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern chinese industrial city. Circ Cardiovasc Qual Outcomes 5:487–493
Zheng X, Zhang R, Liu X et al (2017) Association between cumulative exposure to ideal cardiovascular health and arterial stiffness. Atherosclerosis 260:56–62
Yamashina A, Tomiyama H, Arai T et al (2003) Brachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular risk. Hypertens Res 26:615–622
Sun L, Li C, Liu J et al (2017) Predictive value for cumulative heart rate exposure in new-onset impaired fasting glucose and diabetes mellitus. Int J Clin Exp Med 10:3069–3078
Zemaitis P, Liu K, Jacobs DR Jr et al (2014) Cumulative systolic BP and changes in urine albumin-to-creatinine ratios in nondiabetic participants of the multi-ethnic study of atherosclerosis. Clin J Am Soc Nephrol 9:1922–1929
Domanski MJ, Mitchell GF, Norman JE et al (1999) Independent prognostic information provided by sphygmomanometrically determined pulse pressure and mean arterial pressure in patients with left ventricular dysfunction. J Am Coll Cardiol 33:951–958
Shroff GR, Cen YY, Duprez DA et al (2009) Relationship between carotid artery stiffness index, BNP and high-sensitivity CRP. J Hum Hypertens 23:783–787
Nagano M, Nakamura M, Sato Kenyu TF et al (2005) Association between serum C-reactive protein levels and pulse wave velocity: a population-based cross-sectional study in a general population. Atherosclerosis 180:189–195
McEniery CM, Spratt M, Munnery M et al (2010) An analysis of prospective risk factors for aortic stiffness in men: 20-year follow-up from the caerphilly prospective study. Hypertension 56:36–43
Wang X, Du Y, Fan L et al (2013) Relationships between HDL-C, hs-CRP, with central arterial stiffness in apparently healthy people undergoing a general health examination. PLoS One 8:e81778
Saijo Y, Utsugi M, Yoshioka E et al (2009) Inflammation as a cardiovascular risk factor and pulse wave velocity as a marker of early-stage atherosclerosis in the Japanese population. Environ Health Prev Med 14:159–164
Provan SA, Angel K, Semb AG et al (2011) Early prediction of increased arterial stiffness in patients with chronic inflammation: a 15-year followup study of 108 patients with rheumatoid arthritis. J Rheumatol 38:606–612
Jae SY, Heffernan KS, Yoon ES et al (2012) Pulsatile stress, inflammation and change in arterial stiffness. J Atheroscler Thromb 19:1035–1042
McEniery CM, Spratt M, Munnery M et al (2010) An analysis of prospective risk factors for aortic stiffness in men: 20-year follow-up from the Caerphilly prospective study. Hypertension 56:36–43
Johansen NB, Vistisen D, Brunner EJ et al (2012) Determinants of aortic stiffness: 16-year follow-up of the Whitehall II study. PLoS One 7:e37165
Cavalcante JL, Lima JA, Redheuil A et al (2011) Aortic stiffness: current understanding and future directions. J Am Coll Cardiol 57:1511–1522
Sugawara J, Hayashi K, Yokoi T et al (2005) Brachial-ankle pulse wave velocity: an index of central arterial stiffness? J Hum Hypertens 19:401–406
Tanaka H, Munakata M, Kawano Y et al (2009) Comparison between carotid-femoral and brachial-ankle pulse wave velocity as measures of arterial stiffness. J Hypertens 27:2022–2027
Vlachopoulos C, Aznaouridis K, Terentes-Printzios D et al (2012) Prediction of cardiovascular events and all-cause mortality with brachial-ankle elasticity index: a systematic review and meta-analysis. Hypertension 60:556–562
Takashima N, Turin TC, Matsui K et al (2014) The relationship of brachial-ankle pulse wave velocity to future cardiovascular disease events in the general Japanese population: the Takashima Study. J Hum Hypertens 28:323–327
Verma S, Kuliszewski MA, Li SH et al (2004) C-reactive protein attenuates endothelial progenitor cell survival, differentiation, and function: further evidence of a mechanistic link between C-reactive protein and cardiovascular disease. Circulation 109:2058–2067
Verma S, Badiwala MV, Weisel RD et al (2003) C-reactive protein activates the nuclear factor-kappaB signal transduction pathway in saphenous vein endothelial cells: implications for atherosclerosis and restenosis. J Thorac Cardiovasc Surg 126:1886–1891
Bucova M, Bernadic M, Buckingham T (2008) C-reactive protein, cytokines and inflammation in cardiovascular diseases. Bratisl Lek Listy 109:333–340
Taleb S (2016) Inflammation in atherosclerosis. Arch Cardiovasc Dis 109:708–715
Abe N, Osanai T, Fujiwara T et al (2006) C-reactive protein-induced upregulation of extracellular matrix metalloproteinase inducer in macrophages: inhibitory effect of fluvastatin. Life Sci 78:1021–1028
Cecelja M, Chowienczyk P (2010) Arterial stiffening: cause and prevention. Hypertension 56:29–30
Acknowledgments
This study was supported by the Group Company of Chinese Kailuan. The contributions of the general practitioners of the Kailuan Study are also gratefully acknowledged.
Funding
None.
Author information
Authors and Affiliations
Contributions
CN, JL, LS, and SW designed and initiated the study. CN, TY, LZ, LZ, and XZ assisted in data collection. CN, YG, and XW performed the statistical analysis. CN and LS wrote the first draft of the article. All authors made critical comments on the manuscript and took part in interpretation of the results. RZ, LS, and SW supervised the study.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared that there is no duality of interest associated with this manuscript.
Ethical approval
This study was approved by the Ethics Committee of the Kailuan Medical Group, Kailuan Company, Tangshan, Hebei Province. Research has been conducted in accordance with the Declaration of Helsinki and its later amendments.
Statement of human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Written informed consent was obtained from all the participants of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sun, L., Ning, C., Liu, J. et al. The association between cumulative C-reactive protein and brachial–ankle pulse wave velocity. Aging Clin Exp Res 32, 789–796 (2020). https://doi.org/10.1007/s40520-019-01274-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01274-8