Abstract
Background
Given the progressive demographic ageing of the population and the National Health System reforms affecting care at the bedside, a periodic re-evaluation of in-hospital mortality rates and associated factors is recommended.
Aims
To describe the occurrence of in-hospital mortality among patients admitted to acute medical units and associated factors. Two hypotheses (H) were set as the basis of the study: patients have an increased likelihood to die H1: at the weekend when less nursing care is offered; H2: when they receive nursing care with a skill-mix in favour of Nursing Aides instead of Registered Nurses.
Methods
Secondary analysis of a prospective study of patients >65 years consecutively admitted in 12 Italian medical units. Data on individual and nursing care variables were collected and its association with in-hospital mortality was analysed by stepwise logistic regression analysis.
Results
In-hospital mortality occurrence was 6.8 %, and 37 % of the patients died during the weekend. The logistic regression model explained 34.3 % (R 2) of the variance of in-hospital mortality: patients were six times (95 % CI = 3.632–10.794) more likely at risk of dying at weekends; those with one or more AEDs admissions in the last 3 months were also at increased risk of dying (RR 1.360, 95 % CI = 1.024–1.806) as well as those receiving more care from family carers (RR = 1.017, 95 % CI = 1.009–1.025). At the nursing care level, those patient receiving less care by RNs at weekends were at increased risk of dying (RR = 2.236, 95 % CI = 1.270–3.937) while those receiving a higher skill-mix, thus indicating that more nursing care was offered by RNs instead of NAs were at less risk of dying (RR = 0.940, 95 % CI = 0.912–0.969).
Conclusions
Within the limitations of this secondary analysis, in addition to the role of some clinical factors, findings suggest redesigning acute care at weekends ensuring consistent care both at the hospital and at the nursing care levels.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Around 50–60 % of deaths occur in hospital. Although a large proportion of these are inevitable, detecting factors affecting the risk of dying and focusing on those that are avoidable remains crucial for national health services [NHS, 1, 2]. Studies focused on the occurrence of, and reasons for, in-hospital mortality have been on the agenda of researchers since 1990, when Viana and colleagues [3] analysed the discharge reports of 14,000 patients admitted to an internal medicine service from 1982 to 1988. According to their findings, there was an average mortality rate of 6.6 %, and the principal causes of mortality were pneumonia, cerebrovascular diseases and malignant tumours. Since then, several authors have studied mortality rates in medical settings [4–11], mainly analysing administrative data with retrospective study designs. More recently, two Italian studies [12, 13] have conducted a prospective design in medical settings focusing on clinical factors such as polypharmacology, adverse events and the length of stay; the in-hospital mortality occurrence reported was 5 % [12] and 4 % [13], respectively.
In the current international literature on predictors affecting the risk of in-hospital mortality, in addition to the acknowledged clinical factors, increased attention on quality of care factors is emerging. The higher amount of care provided by registered nurses (RNs) may improve patient’scomfort, increase the quality of care as well as the effectiveness of therapeutic processes decided by physicians, e.g. administering medications on time, providing appropriate surveillance, monitoring signs and symptoms. On the other hand, when the care offered by RNs is poor both in quantitative and qualitative terms, the risk of patients incurring safety issues may increase. Frail patients risking safety issues such as falls, pressure sores, unnecessary bed rest, may be at increased risk of mortality. As evidence of the above mentioned mechanism, in the latest large European study, an increase in nursing workloads by one patient per RN increased the likelihood of an in-patient dying within 30 days of hospital admission by 7 % (odds ratio 1.068, 95 % CI = 1.031–1.106); in addition, nursing staff including RNs educated at the university level, decreased patients risk of mortality [14].
To date, studies available have focused their attention mainly on surgical patients, aimed at understanding the relationship between nursing care and mortality rates [e.g. 14, 15] while medical patients, who are at need of more resources at the bedside due to their frailty [16], seem to be neglected. With regard to patients admitted to medical units, the attention of clinicians has recently been directed to the limited resources available at the bedside, especially in countries facing economic crisis and profound changes to their NHS [17]. The latter changes are affecting not only the amount of care provided by RNs, but also the staff skill-mix as the proportion of care offered by RNs on the amount of care offered by both RNs and nurses aides (NAs) [18]. Reducing the cost of care by reducing the amount of care offered by RNs (educated at the university level) in favour of that offered by NAs (educated with 1 year of training), is considered an attractive option in times of economic crisis.
Therefore, given the progressive demographic ageing of the population and the increased burden of chronic diseases, as well as several NHS reforms and austerity measures affecting care at the bedside in terms of both quantity and quality [19], a periodic re-evaluation of in-hospital mortality rates and associated factors is recommended. Thus, the general intent of the study was to update knowledge on mortality rates in elderly patients admitted to acute medical units, exploring the possible contribution of nursing care factors behind the clinical factors already acknowledged.
Aims and hypotheses
The aims were to describe the occurrence of in-hospital mortality among patients admitted to acute medical units and the associated factors. Two different hypotheses (H) were set as the basis of the study: patients admitted to acute medical units in addition to the clinical conditions:
-
H1: have an increased likelihood of dying at weekend when less nursing care is offered;
-
H2: have an increased likelihood of dying when they receive nursing care with a skill-mix in favour of NAs instead of RNs.
The study was approved by the Clinical Research Ethics Committee of Verona University Hospital (Italy).
Methods
Study design and setting
A secondary analysis from a pragmatically [20] longitudinal observational study (ESAMED) [21] was performed. The original study was conducted over a 7-month period between 2011 and 2012, involving 12 acute internal medicine units (average number of beds 39; range 20–90) located in 12 NHS hospitals in the North-East of Italy. With regard to the hypotheses under study,
-
at weekends (from Saturday to Sunday—night included), the amount of nursing care offered by RNs to the included patients was from −4 to −25 min day/patient (average −11, ±7) less than that offered during the week. During the week, the amount was also variable according to the rules of the hospital (from 133 to 268.8 min/per day each patient).
-
the skill-mix defined as the proportion (%) of care offered by RNs to the total care offered to patients [RNs + nursing aides (NAs)] [22] was variable, from 48 % (less RNs more NAs) to 78.9 % (more care offered by RNs and a minimal part from NAs) but stable at the unit level between the week and the weekend.
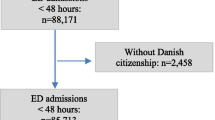
Participants
All patients consecutively admitted to the involved acute medical units during the study period as urgent or scheduled cases, from home or a nursing home (NH), and willing to participate, were included. Those patients transferred from units of the same or other hospitals, or refusing to participate in the study, were excluded.
A total of 2080 patients were admitted during the study period, of which 1464 were included in the study (70.4 %). Among the excluded patients, 385 (62.5 %) were transferred from other hospitals/units and 233 (37.8 %) did not agree to participate. Patients not willing to participate reported the desire of not being disturbed during in-hospital stay or contacted after the discharge with regard to the amount of resources used (e.g. nursing home care); they also did not feel in a condition to participate, due to fatigue or the presence of stressful symptoms.
Variables studied
The main outcome was in-hospital mortality occurrence. Data were collected at three different levels:
-
1.
At the patient level, in addition to the demographic data (age, gender), the type of hospital admission (i.e. urgent or scheduled), the day of admission (i.e. during the week or weekend), and the provenance (from home or NH), were collected.
-
At hospital admission: data were collected on previous access to Accident and Emergency Departments (AEDs) in the last 3 months; co-morbidities; the number of problems or devices [e.g. vascular or pressure sores, enterostomy, tracheostomy, percutaneous endoscopic gastrostomy (PEG)]; the functional status, as measured by the Barthel Index (BI) [23]; and the risk of developing pressure sores as assessed using the Braden Scale for Predicting Pressure Ulcer Risk [24]. The tool score ranges from 6 (severe risk) to 23 (no risk) and a cut-off of ≤14 was fixed for identifying those patients at moderate/high risk of pressure sores. Not lastly, within 24 h of hospital admission, data were collected also on the need for discharge planning using the Blaylock Risk Assessment Screening Score (BRASS) [25] in its Italian validated version [26]. Using the BRASS tool, the following groups were identified: a low-risk group with post-discharge problems and limited need for discharge planning (scores ranging from 0 to 10), a medium-risk group (11–20) and a high-risk group comprising those patients that required extensive discharge planning such as institutional (NH)/post-acute care (scores >20);
-
during the in-hospital stay: data were collected daily at the bedside or from the nursing records as the occurrence of confusion/agitation measured by the assessment of changes of either a subtle or noticeable degree in awareness, alertness, attention, orientation, thinking, perception and recent/immediate memory [27]; the occurrence of pressure sores (yes/no), falls (yes/no) and physical restraints (yes/no). Researchers also recorded the number of care shifts offered by family carers at the patient’s bedside during morning, afternoon or night periods;
-
at the discharge: functional decline, stability or recovery was measured as the difference between the BI at admission and the BI at discharge. Functional decline/recovery at discharge was defined as a decrease/improvement of at least five points in the BI score [28]. The length of stay (LOS), the day of discharge (during the week vs. weekend) and the Diagnosis-Related Group (DRG), were also collected.
-
-
2.
At the nursing care level, the amount of care offered by RNs in min/day, by NAs and the total amount of care offered by the nursing team (RNs + NAs), were assessed on a daily basis. In accordance with the average amount of nursing care received from RNs at weekend compared to that received during the week, two groups of patients were identified: those receiving from −12 to −24 min/day at weekend, and those receiving from −4 to −11 min/day. In addition, the skill-mix as the proportion (%) of care offered from RNs to the total care offered to patients (RNs + NAs) was calculated [22]. Moreover, the occurrence of missed nursing care was measured with the MISSCARE Survey [29], in its Italian validated version [30]. Nursing staff consisting of 252 RNs and 165 NAs were eligible in the units as those caring for the patients during the study period. A total of 314 (75.2 %) nursing staff members participated, specifically 205 (81.3 %) RNs and 109 (66 %) NAs. The instrument includes a list of 24 nursing interventions; using a five-point Likert scale (1—never, 5—always), respondents have to indicate how often during the last shift each intervention was missed, such as: medication not given within 30 min, missed communication to physician of altered vital sign, missed pain assessment, missed surveillance of patient receiving high-risk medication and missed patient repositioning. The total score of the MISSCARE Survey may range from 24 (no intervention has ever been omitted) to 120 (all interventions were always omitted).
Statistical analysis
Data analysis was performed using the Statistical Package for Social Sciences (SPSS for Windows—version 22.0, SPSS Inc., 233 South Wacker Drive, Chicago) for statistical analysis. Descriptive statistical analyses were performed calculating averages and 95 % confidence intervals (CIs) for continuing variables or sums and percentage for categorical variables. Given that a total of 212 different DRGs emerged, the comparisons were made only among the major DRGs. Comparisons between surviving and deceased patients were performed using the χ 2 test and t test according to the nature of the variables. Stepwise logistic regression analysis aimed at identifying the factors (Relative Risk, RR; CI 95 %) affecting the outcome (mortality) was performed introducing in the model only those variables significantly associated at the bivariate analysis (p < 0.05). The Hosmer–Lemeshow goodness of fit test for logistic regression analysis was evaluated (Chi Square = 4.946; p = 0.763). The criterion for statistical significance was set at p < 0.05.
Results
Occurrence of in-hospital mortality
The in-hospital mortality rate was 6.8 % (100 individuals died/1464) and 37 patients died at the weekend. The LOS was, on average, around 9.3 days (range 1–40). On the 1st day after admission, 11 patients (on 1464; 0.7 %) died; on the 2nd day, another seven patients died reaching a mortality rate of 1.2 % within the first 24 h after hospital admission. While the majority of patients died on the 3rd day (14; 0.9 %) in the remaining days (from the 4th to the 10th day after admission), from 4 to 6 patients died/day; the remaining (44; 44 %) patients with >11 LOS, died from 1 to 2 per day.
The most frequent causes of death, as reported by the Diagnosis–Related Group (DRG) system, were heart failure and shock (DRG 127, 16 %), simple pneumonia and pleurisy (DRG 089, 8 %), septicaemia without mechanical ventilation (DRG 576, 6 %), pulmonary oedema and respiratory failure (DRG 087, 6 %), and digestive malignancy (DRG 172, 5 %).
Profile of in-hospital deceased patients
At the individual level, comparing the characteristics of the participants, a statistically significant difference between the group of patients who died and those who survived was found for the majority of variables as reported in Table 1. Deceased patients were older (81 years vs. 73.9, p = 0.000), with more AED accesses (≥1) in the last 3 months (56 vs. 36.1 %, p = 0.001); and more co-morbidities (on average 2.4 vs. 2.1, p = 0.013). Patients who died were admitted mainly as urgent cases (97 vs. 90.1 %, p = 0.023), more often from NHs (30 vs. 10.9 %, p = 0.000) and they were more dependent on the nursing care as measured by the Barthel Index (28.9 vs. 53.6, p = 0.000) and at an increased risk of pressure sores as measured by the Braden tool (80 vs. 34.2 %, p = 0.000).
Deceased patients were also at an increased need of resources at discharge as measured with the BRASS index in the first 24 h after admission (19.9 vs. 11.7 p = 0.000). Patients who died were under medication with more molecules/day (>5) compared to those who survived (58 vs. 45.2 %, p = 0.025) and they reported more often problems/devices (16.0 vs. 11.1 %, p = 0.001) at admission; in addition, they more often reported behavioural disturbances (37 % vs. 14.8, p = 0.000) and agitation/confusion (65 vs. 18.6 %, p = 0.000).
During the length of stay, deceased patients reported higher occurrence of pressure sores compared to those who survived (43 vs. 16.9 %, p = 0.000), and they were also more often restrained, on average 0.23 % of their LOS as compared to those who survived (0.06 %; p = 0.000). Family carers were at the bedside more often in those patients who died (on average 38.4 % of shifts vs. 12.1 %, p = 0.000). On the day of discharge, functional decline was reported more often by deceased patients (30 vs. 15.8 %, p = 0.000).
No differences were found at the individual level in other variables such as gender (p = 0.210), the day of hospital admission (during the week 75 vs. 77.4 %; at the weekend 25 vs. 22.6 %, p = 0.831), the LOS (9.0 vs. 9.7 days, p = 0.313), the occurrence of confusion/agitation during the in-hospital stay (29 vs. 12.8 %, p = 0.067) and falls (2 vs. 2.1 %, p = 0.971).
At the nursing care level, 46 deceased patients received from −12 to −29 min/day at the weekends while the remaining 54 received from −11 to −4 min/day, thus indicating a stable amount of nursing care received during the entire week. Patients who died received significantly more care from NAs (85.1 min/day on average) than those who survived (77.6 min/day), as reported in Table 1: in fact, the skill-mix was significantly in favour of NAs in deceased patients (60.3 vs. 63.4 %, p = 0.003).
A significant difference has emerged also in the occurrence of missed nursing care which was slightly inferior for those patients who died (on average 51.1 vs. 52.6, p = 0.042). No statistical significant difference was found between groups for the amount of care received from the nursing team (RNs + NAs) (211.6 vs. 207.9 min/day, p = 0.316) or from only RNs (125.8 vs. 129.8 min/day, p = 0.072).
Factors affecting in-hospital mortality
In the logistic regression analysis reported in Table 2, which explained 34.3 % (R 2) of the variance of elderly in-hospital mortality, patients were six times (95 % CI = 3.632–10.794) more likely at risk of dying at weekends; those with one or more AED admissions in the last 3 months were also at increased risk of dying (RR 1.360, 95 % CI = 1.024–1.806) as well as those receiving more care from family members (RR = 1.017, 95 % CI = 1.009–1.025).
At the nursing care level, those patients receiving less than −12 min/day of care from RNs at weekends as compared to that received during the week, were at increased risk of dying (RR = 2.236, 95 % CI = 1.270–3.937); in addition, a higher skill-mix indicating that more nursing care was offered by RNs instead of NAs, was associated with a decreased risk of dying (RR = 0.940, 95 % CI = 0.912–0.969).
Discussion
Occurrence and causes of in-hospital mortality
The occurrence of in-hospital mortality was 6.8 %, higher when compared to the 4 and 5 % reported in previous Italian multicenter studies, involving 1201 [13] and 1,332 patients [12], respectively. Recently, Leshem–Rubinow and colleagues [11] reported lower rates of in-hospital mortality (3.9 %) in a smaller sample (=259) of patients admitted to one medical department [11]. Previously, lower rates of in-hospital mortality were also documented in younger patients (from 4.3 % [4] to 6.7 % [3]). Nevertheless, our study was conducted during the winter period, when an increased risk of in-hospital death has already been acknowledged [31], as also confirmed by the fact that the second cause of death was pneumonia. However, the occurrence of in-hospital mortality observed in our study was broadly lower than that reported by Barba Martín et al. (9.9 %) [9] and by Barba et al. (12.2 %) [32], thereby still confirming a great variability in the in-hospital mortality rate of medical patients.
The occurrence of death within the second day after admission was around 1.2 %, lower than the 3 % and 2.5 % reported by Barba and colleagues [32] and Marco and colleagues [10]. However, their sample size was higher (1,135,423 and 429,880, respectively) and patients’ characteristics were different from ours: those included by Barba and colleagues were older (8 % of whom were >90 years) [32] whilst those included by Marco and colleagues were all admitted as urgent cases [10]. In the last decade, NHs have improved primary care services, allowing terminally ill patients to die at home: community health care resources may influence place-of-death patterns, thereby reducing in-hospital death [33].
The most frequent causes of in-hospital death were heart failure, septicaemia and respiratory failure, as reported in previous studies [1, 5, 10, 13].
Profile of in-hospital deceased patients
Consistently with previous studies, deceased patients were older [1, 10, 12, 13, 32], admitted as urgent cases [34] from NHs. The clinical condition of NH residents is generally worse than that of those living at home [35] and they are transferred into acute care settings when clinical conditions are not manageable in low medical and nursing care contexts such as in NHs.
Despite the cumulative evidence reported by previous studies [7, 10, 34, 36–38], no difference in in-hospital mortality has emerged with regard to those patients admitted during the weekend and during the week. However, the previous studies mentioned above were conducted in countries other than Italy with different health care services and organization of medical and nursing staff.
At admission, patients who later died reported significantly more AED accesses in the last 3 months, a higher number of co-morbidities, and more problems/devices as compared to survived patients. They were also receiving more medications/day and they showed more often agitation/confusion and behavioural problems at hospital admission. They were also screened as being at increased risk of developing pressure sores and of having post-discharge problems as well as in need of extensive discharge planning; in addition, they were also more dependent on activities of daily living (ADLs), as reported previously by other authors [28]. Therefore, at admission, the profile of patients who later died was frailer and in increased need of medical and nursing care.
During their in-hospital stay, a higher occurrence of negative outcomes sensitive to nursing care was reported among deceased patients, such as pressure sores, the use of physical restraints, and functional decline [12, 34] thereby suggesting suboptimal nursing care possibly due to a lack of resources [39]. Those patients who died were cared for by family carers with around 40 % of shifts as compared with those that survived (12 %) and this might suggest their willingness to assist their loved ones as well as the request by medical and nursing staff to be at the bedside given the unstable conditions and the lack of resources available.
At the nursing care level, deceased patients received on average less care from RNs and more from NAs than those who survived, thus affecting the skill-mix that was in favour of NAs. Nursing aides are educated in providing basic care such as hygiene, nutrition and mobility, which is important in elderly patients admitted to medical units [40]. However, acute medical patients require competent care such as strict surveillance and continuing assessment: the skill-mix expresses the strength of RN care in the dose of nursing and when insufficient has been already associated with poor patients’ outcomes [41].
With regard to the amount of missed care, there was a significant statistical difference between the groups (average 51.5 in deceased patients vs. 52.6 in surviving patients) but the practical meaning of this difference is limited, indicating that in the perception of nurses involved, the amount of care missed was similar among the groups. The total amount of nursing care missed is consistent with previous studies in the field conducted at the international level [29].
Factors affecting in-hospital mortality
The overall model, including individual and nursing care variables, explained a total variance of in-hospital elderly mortality of 34.3 % (R 2): therefore, further research should produce evidence on other clinical and organisational factors aimed at explaining the variance in mortality rates of patients admitted to medical units.
The first hypothesis (H1), postulating that patients admitted to medical units are more likely to die at weekend, was confirmed by logistic regression analysis. Two findings supported this hypothesis: at an overall level, patients reported a higher risk of dying at weekend; in addition, those patients receiving less care (from −12 min to −29/day) by RNs at weekend were also at an increased risk of dying. Therefore, two different mechanisms seem to be implicated in the increased risk of mortality at weekends: in accordance with the hypothesis, in units offering less nursing care at weekends, when new patients are also admitted and poor unit support by the hospital is offered, patients may be less monitored and cared for. In addition to this mechanism, weekends were also at risk of increased mortality in all units independently of the amount of nursing care offered: possibly, fewer available physicians and limited available diagnostic and therapeutic procedures may negatively influence responses to the increased acuity of patients [18, 42, 43]. The “weekend effect” already mentioned in previous studies [18], in particular, as the risk of dying in those patients admitted to hospital at weekend, seems also to affect the mortality risk in those already admitted to hospital.
The second hypothesis (H2) postulated that patients receiving care with a skill-mix in favour of NAs instead of RNs were more at risk for mortality. Nurses aides receive limited training aimed at developing basic competences of nursing care; instead, RNs are educated at the university level aimed at developing critical thinking and decision-making competences, to perform continuing surveillance and to detect early signs of deterioration, thus requiring the intervention of physicians. The reduced risk of mortality associated with an increased dose of care offered by RNs is supported also by previous evidence [14, 15, 41] but has never been assessed in the Italian context.
The remaining predictors of in-hospital mortality emerged were (a) the number of previous AED admissions in the last 3 months, indicating that patients with acute conditions and/or with recurring relapses of chronic illness were more likely to die during hospitalization [12]; and (b) the higher amount of care delivered by family carers. This may be considered a reverse causation biases: in terminally ill patients, the therapeutic approach is generally turned into a comfort approach and the medical and nursing team may require family carers to stay at the bedside [44]. Therefore, those patients in their terminal stage received more care from family carers. Differently from the prognostic significance of functional decline found by Socorro García and colleagues [28], being admitted with greater dependence and reporting a decline during hospitalization was not associated with the risk of dying possibly because the majority of elderly patients admitted to medical units, are functionally dependent.
Several limitations affect our study. Among others, such as its exploratory nature, and the proportion of patients who refused to participate, it was based on secondary analysis; therefore some data (e.g. medical staff availability, the terminally ill condition at admission as well as the severity of the disease) was not collected. Only some adverse clinical events were recorded by RNs during hospitalization: among of these, patient cognition both at admission and during the entire LOS was not assessed through a validated tool while the clinical judgment of RNs was considered, and this may have introduced intra-unit and inter-units biases. In addition, the medical staff resources were not assessed. Moreover, the study was performed during the autumn–winter period and this might have influenced rates due to seasonal variations in mortality; in addition, some Confidence of Intervals (e.g. between mortality and weekends in the multivariate analysis), were large; therefore, in light of the above mentioned limitations, more research in needed in the field aimed at testing the findings on a large scale.
Conclusion
Our study found an in-hospital mortality rate of 6.8 %, and heart failure, septicaemia and respiratory failure to be the most frequent causes of inpatient death. The deceased patients were older, frailer and mainly admitted from NHs, with a higher risk of difficult discharge, and reported a higher occurrence of negative outcomes sensitive to nursing care.
Two independent factors were associated with in-hospital mortality: weekends were at risk of increasing mortality rates when less care is offered both at the nursing and at the hospital levels; an increased dose of care offered by RNs, was, instead, a protective factor, thus reducing the risk of mortality. Within the limitations of this secondary analysis, suggesting that more studies are needed in the field, in addition the role of some clinical factors, findings suggest redesigning hospital care at weekends, ensuring consistent amount of care and support at nursing and at hospital levels, such as that offered during the week. In addition, the skill-mix should also be re-defined, increasing the proportion of care offered by RNs, aimed at monitoring and detecting early signs and symptoms of clinical deterioration of frail elderly patients admitted to acute settings.
References
Toscani F, Di Giulio P, Brunelli C et al (2005) How people die in hospital general wards: a descriptive study. J Pain Symptom Manag 30:33–40
Campbell MJ, Jacques RM, Fotheringham J et al (2012) Developing a summary hospital mortality index: retrospective analysis in English hospitals over five years. BMJ 344:e1001. doi:10.1136/bmj.e1001
Viana A, Carballo F, Beato I et al (1990) An analysis of 14,000 patients admitted to an internal medicine service during 1982–1988. An Med Interna 7:459–462
Escolar Castellón F, Sampériz Legarre AL, Pérez Poza A et al (1993) Morbidity, mortality and other indicators of health care activities, at a General Internal Medicine Service. An Med Interna 10:327–332
Del Río Fernández MC, Fernández Renedo A, de Frutos Arribas JF et al (1998) Mortality in an internal medicine department within a third-level hospital; twenty years experience. An Med Interna 15:197–201
Delgado Morales JL, Alonso del Busto R, Pascual Calleja I et al (2004) Observational study of patients admitted to an Internal Medicine service. An med Interna 21:3–6
Barba R, Losa JE, Velasco M et al (2006) Mortality among adult patients admitted to the hospital on weekends. Eur J Intern Med 17:322–324
Rayego Rodríguez J, Rodríguez-Vidigal FF, Mayoral Martín L et al (2006) Hospital Mortality in the Internal Medicine Services of a first level center. An Med Interna 23:406–410
Barba Martín R, Marco Martínez J, Emilio Losa J et al (2009) Two-year analysis of internal medicine activity in the National Health Care System hospitals. Rev Clin Esp 209:459–466
Marco J, Barba R, Plaza S et al (2010) Analysis of the mortality of patients admitted to internal medicine wards over the weekend. Am J Med Qual 25:312–318. doi:10.1177/1062860610366031
Leshem-Rubinow E, Vaknin A, Sherman S et al (2013) Norton scale, hospitalization length, complications, and mortality in elderly patients admitted to internal medicine departments. Gerontology 59:507–513. doi:10.1159/000353710
Nobili A, Licata G, Salerno F et al (2011) Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. The REPOSI study. Eur J Clin Pharmacol 67:507–519. doi:10.1007/s00228-010-0977-0
Marengoni A, Nobili A, Romano V et al (2013) Adverse clinical events and mortality during hospitalization and 3 months after discharge in cognitively impaired elderly patients. J Gerontol A Biol Sci Med Sci 68:419–425. doi:10.1093/gerona/gls181
Aiken LH, Sloane DM, Bruyneel L et al (2014) Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet 383:1824–1830. doi:10.1016/S0140-6736(13)62631-8
Tourangeau AE, Cranley LA, Jeffs L (2006) Impact of nursing on hospital patient mortality: a focused review and related policy implications. Qual Saf Health Care 15:4–8
Meschi T, Ticinesi A, Prati B et al (2016) A novel organizational model to face the challenge of multimorbid elderly patients in an internal medicine setting: a case study from Parma Hospital, Italy. Intern Emerg Med (in press)
La Regina M, Orlandini F, Ligurian Internal Medicine Group (2014) Internal medicine wards and the chronic diseases epidemic: it is time to change the standards. Intern Emerg Med 9:483–485. doi:10.1007/s11739-013-1029-4
Huang C-C, Huang Y-T, Hsu N-C et al (2016) Effect of weekend admissions on the treatment process and outcomes of internal medicine patients a nationwide cross-sectional study. Medicine (Baltimore) 95:e2643. doi:10.1097/MD.0000000000002643
Organization for Economic Co-operation and Development (OECD) (2015). http://stats.oecd.org/. Accessed 29 Dec 2015
Palese A, Bevilacqua MG, Dante A et al (2010) Do randomized controlled nursing trials have a pragmatic or explanatory attitude? Findings from the Pragmatic-Explanatory Continuum Indicator Summary (PRECIS) tool exercise. J Nurs Res 22:216–220. doi:10.1097/jnr.0000000000000045
Palese A, Ambrosi E, Prosperi L et al (2015) Missed nursing care and predicting factors in the Italian medical care setting. Intern Emerg Med 10:693–702. doi:10.1007/s11739-015-1232-6
Palese A, Cuel M, Zambiasi P et al (2013) Nursing care received by older patients in Italian medical units: findings from an explorative study. Aging Clin Exp Res 25:707–710
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Bergstrom N, Braden BJ, Laguzza A et al (1987) The Braden Scale for predicting pressure sore risk. Nurs Res 36:205–210
Blaylock A, Cason CL (1992) Discharge planning predicting patients’ needs. J Gerontol Nurs 18:5–10
Saiani L, Zanolin ME, Dalponte A et al (2008) Sensibility and specificity of a screening instrument for patients at risk of difficult discharge. Assist Inferm Ric 27:184–193
Registered Nurses Association of Ontario (RNAO) (2003) Screening for delirium,dementia and depression in older adults. Registered Nurses Association of Ontario (RNAO), Toronto
Socorro García A, de la Puente M, Perdomo B et al (2015) Functional status and mortality at month and year in nonagenarians hospitalized due to acute medical illness. Eur J Intern Med 26:705–708. doi:10.1016/j.ejim.2015.08.007
Kalisch BJ, Williams RA (2009) Development and psychometric testing of a tool to measure missed nursing care. J Nurs Adm 39:211–219. doi:10.1097/NNA.0b013e3181a23cf5
Sist L, Cortini C, Bandini A et al (2012) Il concetto di missed nursing care: una revisione narrativa della letteratura. Assist Inferm Ric 31:234–239. doi:10.1702/1211.13414
Callaly E, Mikulich O, Silke B (2013) Increased winter mortality: the effect of season, temperature and deprivation in the acutely ill medical patient. Eur J Intern Med 24:546–551. doi:10.1016/j.ejim.2013.02.004
Barba R, Martínez JM, Zapatero A et al (2011) Mortality and complications in very old patients (90+) admitted to departments of internal medicine in Spain. Eur J Intern Med 22:49–52. doi:10.1016/j.ejim.2010.11.001
Teno JM, Gozalo PL, Bynum JP et al (2013) Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 309:470–477. doi:10.1001/jama.2012.207624
Smith S, Allan A, Greenlaw N et al (2013) Emergency medical admissions, deaths at weekends and the public holiday effect. Cohort study. Emerg Med J 31:30–34. doi:10.1136/emermed-2012-201881
Barba R, Losa JE, Canora J et al (2009) The influence of nursing homes in the functioning of internal medicine services. Eur J Intern Med 20:85–88. doi:10.1016/j.ejim.2008.04.001
Sharp AL, Choi H, Hayward RA (2013) Don’t get sick on the weekend: an evaluation of the weekend effect on mortality for patients visiting US EDs. Am J Emerg Med 31:835–837. doi:10.1016/j.ajem.2013.01.006
Handel AE, Patel SV, Skingsley A et al (2012) Weekend admissions as an independent predictor of mortality: an analysis of Scottish hospital admissions. BMJ Open 2:e001789. doi:10.1136/bmjopen-2012-001789
Aylin P, Yunus A, Bottle A et al (2010) Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 19:213–217. doi:10.1136/qshc.2008.028639
Palese A, Beltrame ER, Bin A et al (2008) Esiti sensibili alle cure infermieristiche: analisi critica della letteratura. Assist Inferm Ric 27:33–42
Steinhauser KE, Christakis NA, Clipp EC et al (2000) Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 284:2476–2482
Tourangeau AE, Giovannetti P, Tu JV et al (2002) Nursing-related determinants of 30-day mortality for hospitalized patients. Can J Nurs Res 33:71–88
Goldstein SD, Papandria DJ, Aboagye J et al (2014) The “weekend effect” in pediatric surgery—increased mortality for children undergoing urgent surgery during the weekend. J Pediatr Surg 49:1087–1091. doi:10.1016/j.jpedsurg.2014.01.001
Suissa S, Dell’Aniello S, Suissa D et al (2014) Friday and weekend hospital stays: effects on mortality. Eur Respir J 44:627–633. doi:10.1183/09031936.00007714
Ambrosi E, Biavati C, Guarnier A et al (2015) Factors affecting in-hospital informal caregiving as decided by families: findings from a longitudinal study conducted in acute medical units. Scand J Caring Sci. doi:10.1111/scs.12321 (in press)
Acknowledgments
The researchers would like to thank both the patients and the clinical teams of the involved hospitals for their participation in the research process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors confirm that there are no conflicts of interest.
Ethical approval
Ethical approval was granted by the Clinical Research Ethics Committee of Verona University Hospital.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Rights and permissions
About this article
Cite this article
Ambrosi, E., De Togni, S., Guarnier, A. et al. In-hospital elderly mortality and associated factors in 12 Italian acute medical units: findings from an exploratory longitudinal study. Aging Clin Exp Res 29, 517–527 (2017). https://doi.org/10.1007/s40520-016-0576-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0576-8