Abstract
Background
No formal systematic review or meta-analysis was performed up to now to summarize the risk factors of delirium after hip surgery.
Aims
The present study aimed to quantitatively and comprehensively conclude the risk factors of delirium after hip surgery in elderly patients.
Methods
A search was applied to CNKI, Embase, Medline, and Cochrane central database (all up to August 2015). All studies assessing the risk factors of delirium after hip surgery in elderly patients without language restriction were reviewed, and qualities of included studies were assessed using the Newcastle–Ottawa Scale. Data were pooled and a meta-analysis was completed.
Results
A total of 24 studies were selected, which altogether included 5364 patients with hip fracture. One thousand and ninety of them were cases of delirium occurred after surgery, suggesting the accumulated incidence of 24.0 %. Results of meta-analyses showed that elderly patients with preoperative cognitive impairment [odds ratio (OR) 3.21, 95 % confidence interval (CI) 2.26–4.56), advanced age (standardized mean difference 0.50, 95 % CI 0.33–0.67), living in an institution (OR 2.94; 95 % CI 1.65–5.23), heart failure (OR 2.46; 95 % CI 1.72–3.53), total hip arthroplasty (OR 2.21; 95 % CI 1.16–4.22), multiple comorbidities (OR 1.37; 95 % CI 1.12–1.68) and morphine usage (OR 3.01; 95 % CI 1.30–6.94) were more likely to sustain delirium after hip surgery. Females were less likely to develop delirium after hip surgery (OR 0.83; 95 % CI 0.70–0.98).
Conclusions
Related prophylaxis strategies should be implemented in elderly patients involved with above-mentioned risk factors to prevent delirium after hip surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture constitutes a major health problem in elderly patients, and is an important cause of loss of function and increase need of care. A total of 13–55.9 % of hip fracture patients experience delirium [1–5], which is defined as a sudden onset and disturbances in attention, consciousness and other cognitive abilities. Although the exact underlying pathophysiology of delirium is elusive, delirium has been associated with a wide variety of predisposing factors, including older age [4, 6–14], male gender [3, 7, 15], dementia [3, 11], multiple medical comorbidities [3, 9, 14] and polypharmacy [7].
Because postoperative delirium is associated with longer hospital stay, poorer functional recovery, higher healthcare costs and 72.4 % of those died within 5 years [4, 16, 17], identification of individuals at high risk of delirium and development of early prevention and intervention strategies after hip fracture repair would have a great public health significance.
However, these studies had some limitations, such as a small sample size and containing a single or very few potential risk factors in the individual study. In addition, some results obtained from individual studies were inconsistent and even contradictory. Thus, it is still uncertain whether these identified factors from individual studies are able to predict delirium after hip surgery.
Until now, no formal systematic review or meta-analysis was performed to summarize the risk factors of delirium after hip surgery to obtain a definitive conclusion. Therefore, in this study, we summarized these risk factors from the previous original researches and conducted a meta-analysis. It would be most informative in guiding clinicians for identifying high risk patients and help them preventing postoperative delirium after hip surgery to improve the patients’ prognosis.
Materials and methods
Literature search
CNKI, Embase, Medline, and Cochrane central database were searched using a broad range of terms to identify original research, published all through August 2015 and selecting potential studies to consider. The main key words were as follows: “factor” or "predictor" or "risk" AND "delirium" or "acute confusional states" AND "hip" AND "fracture" AND "elderly". Also, a manual search of references in the identified articles and systematic reviews was performed for possible inclusion.
Eligibility criteria
Two reviewers (Xin Zhao and Zongyou Yang) independently evaluated the titles and abstracts of the identified studies. Only full-text articles without language restriction were included in this meta-analysis. The following inclusive selection criteria were applied: (1) a study was performed to explore risk factors for delirium occurrence after hip fracture surgery; (2) elderly people (≥60 years old) who underwent hip fracture repair; (3) cases and controls were defined based on the presence or absence of delirium, respectively; (4) Diagnostic and Statistical Manual of Mental Disorders (DSM) IV edition [18], or DSM-derived criteria such as Confusion Assessment Method [19] were used as diagnostic criteria; (5) sufficient data were published for estimating an odds ratio (OR) or hazard ratio (HR) or standardized mean difference (SMD) with 95 % confidence interval (95 % CI).
Quality of included studies
The quality of the included studies was evaluated using the Newcastle–Ottawa Scale (NOS) [20]: based on the three main items: the selection of the study groups (0–4 points), the comparability of the groups (0–2 points) and the determination of either the exposure or the outcome of interest (0–3 points), with a perfect score of 9.
Data extraction
All the data were carefully extracted from all eligible studies independently by the two reviewers (Xin Zhao and Zongyou Yang). The following variables were extracted from each study: first author’s name, publication year, country, significant risk factors, definitions and numbers of cases and controls and numbers of citations for each potential risk factor for delirium after hip fracture surgery. Any disagreement was resolved by discussion and consensus.
Statistical analyses
ORs or SMDs and corresponding 95 % CI were estimated and pooled across studies to assess the association between different variables and the risk of delirium with a value of P < 0.05 as significance. Heterogeneity among studies was tested by Q-test statistics with significance set at P < 0.10 [21] and further measured by I 2 statistics with I 2 more than 50 % indicating significant inconsistency. A random-effect model was used to calculate pooled ORs in the case of significant heterogeneity (P < 0.10 or I 2 > 50 %); otherwise, a fixed-effect model was used [22]. The outcome of meta-analysis for variables was summarized graphically using a forest plot. If necessary, a sensitive analysis by excluding outlier study one by one was conducted to investigate the sources for heterogeneity. Potential publication bias was detected by Begg’s funnel plots, and P < 0.05 was judged as statistically significant. All analyses were performed by the software Stata 11.0 (Stata Corporation, College Station, TX).
Results
Characteristics of identified studies
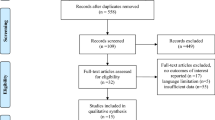
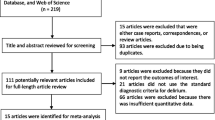
Figure 1 indicates the flowchart of the article screening and the detailed selection process. Initial search yielded 448 titles and abstracts from the electronic databases. After duplicates were removed, 143 abstracts were reviewed for initial screening and 78 for the next stage of review. After inclusion and exclusion criteria were applied, 24 full text articles were chosen for this meta-analysis. Of them, 20 were published in English and 4 in Chinese with publication time from 2000 to 2015. These 24 studies altogether included 5364 patients with hip fracture; 1290 cases of delirium occurred after surgery, suggesting the accumulated incidence of 24.0 %. Detailed information about these included studies is shown in Table 1.
Methodological quality assessment
The outcome of methodology quality assessment was as follows: four studies [2, 4, 23, 24] scored 9, eight studies [1, 5, 10, 15, 25–28] scored 8, seven studies [3, 6–9, 29, 30] scored 7 and five studies [11–14, 31] scored 6.
Age and gender
Fourteen studies reported the admission age of 82.0 years in postoperative delirium patients, which was 3.6 years older than that in nondelirium groups, and the pooled results for meta-analysis suggested a significant difference (SMD 0.50; 95 % CI 0.33–0.67; Fig. 2a), but with a significant heterogeneity (P = 0.001, I 2 = 62.1 %; Table 2). However, after sensitive analysis by excluding outlier studies, the I 2 value lowered to 48.8 %, and the significance did not change, indicating the result was reliable (Table S1). Sex difference of the occurrence of delirium after hip fracture surgery was reported in 20 studies. Results of meta-analysis showed that females were less likely to sustain delirium, and the combinable OR was 0.83 (95 % CI 0.70–0.98; Fig. 2b), with no heterogeneity (P = 0.697, I 2 = 0; Table 2). Begg’s funnel plot for publication bias investigated no sex difference between delirium and nondelirium after hip fracture surgery (P = 0.163; Fig. 3).
Forest plots of the meta-analyses of some variables comparing characteristics between delirium and nondelirium after hip fracture surgery. Patients with the risk factors of a advanced age, c preoperative cognitive impairment, d living in an institution, e medical comorbidities, f total hip arthroplasty, g use of morphine would be more likely to sustain the delirium after hip fracture surgery in elderly patients. b Females were less likely to develop delirium after hip surgery. The width of the horizontal line represents the 95 % CI of the individual studies, and the square proportional represents the weight of each study. The diamond represents the pooled OR or standardized mean difference and 95 % CI
Cognitive impairment
Postoperative delirium incidence was consistently higher in those who had cognitive impairment compared with those who did not. A total of 13 studies reported the preoperative cognitive impairment as a risk factor and meta-analysis of these studies showed that patients with cognitive impairment were more prone to develop delirium after hip fracture surgery (OR 3.21, 95 % CI 2.26–4.56), with observed heterogeneity (P = 0.001, I 2 = 71.6 %; Table 2; Fig. 2c).
Living in an institution
Seven studies have previously reported institution as a risk factor associated with delirium after hip fracture surgery, with a significant difference (OR 2.94; 95 % CI 1.65–5.23), resulting from randomed-effects model with high heterogeneity (P = 0.025, I 2 = 58.4 %; Table 2; Fig. 2d).
Heart failure
Four studies mentioned heart failure. The meta-analysis showed there was significant difference (OR 2.46; 95 % CI 1.72–3.53). There was no evidence of heterogeneity among studies (P = 0.889, I 2 = 0; Table 2).
Medical comorbidities
Eight studies reported medical comorbidities. Using a fixed-effects model, we observed a significant difference of this factor (OR 1.37; 95 % CI 1.12–1.68; Table 2; Fig. 2e), but with a significant heterogeneity (P = 0.001, I 2 = 70.2 %; Table 2). After sensitive analyses, heterogeneity was resolved and the significance did not change (Table S1).
Total hip arthroplasty
Five studies paid close attention to the relationship between total hip arthroplasty and delirium. Meta-analysis of these five studies showed that total hip arthroplasty patients were more likely to develop delirium (OR 2.21; 95 % CI 1.16–4.22; Table 2; Fig. 2f), with a significant heterogeneity. After sensitive analyses, heterogeneity was resolved and the significance did not change (Table S1).
Morphine
There were four included studies reporting the use of morphine after hip fracture surgery. The meta-analysis showed there was significant difference between morphine users and non-users (OR 3.01; 95 % CI 1.30–6.94; Table 2; Fig. 2g).
Discussion
Delirium is a common complication in elderly patients after hip fracture surgery. Lipowski [32] described three clinical subtypes of delirium based on verbal and nonverbal behavioral manifestation: hypoactive, hyperactive and mixed delirium subtype. Results in this meta-analysis suggested the overall prevalence of postoperative delirium was 24.0 %, which is comparable to the range of 13.0–55.9 % in hip-surgery patients reported by others [1–5]. This meta-analysis demonstrates that advanced age, male gender and cognitive impairment are the most consistently significant risk factors for postoperative delirium after hip fracture surgery, followed by living in an institution, heart failure, total hip arthroplasty, multiple comorbidities, morphine usage.
Although the exact underlying pathophysiology of delirium is elusive, the leading hypotheses are similar to those proposed for neurodegenerative processes such as dementia and other types of cognitive impairment. Cole et al. [33] explained the relationship between preoperative dementia and delirium, indicating both had similar symptoms and pathogenesis, which included reduced metabolic rates and impaired cholinergic function, and similar causative factors, such as excitotoxic neuronal damage and neuron death [34, 35]. The cognitive function of hip fracture patients was evaluated preoperatively using MMSE [36]. The reason why cognitive assessment is always not conducted prior to emergency hip fracture surgery is that there is not enough time to perform cognitive testing in pre-operation. However, many studies [1, 5, 8, 9], including those in this meta-analysis, prove the feasibility of preoperative cognitive testing in emergencies. Therefore, cognitive testing should become a part of the standardized program for preoperative clinical assessment for hip fracture surgeries [37]. Elucidation of linking mechanism between dementia and delirium could lead to the development of specific strategies for early detection, prevention and intervention strategies in individuals with preoperative dementia undergoing surgery. Impaired performance on cognitive tests was a risk factor for delirium. This study is consistent with other studies [4, 25, 31, 38], after resolving heterogeneity. In this meta-analysis, the average MMSE score of 20.7 emphasizes that even mild dementia increases the risk for delirium with hip surgery.
Another important risk factor was advanced age, with 3.1 years of admission age older in patients experiencing postoperative delirium than those without delirium. This may be due to the fact that elderly patients with high risk for developing delirium were more likely mediated by age-related physical and cerebral changes [39], such as poor organ compensative capacity, reduced body adaptability, declined adjustment ability, increased susceptibility to stressors and abnormally excited conductibility, underlying the different symptoms and clinical presentations of delirium. Several studies [9, 27] assessed preoperative physical condition as a risk factor of delirium after hip surgery by examining number of medical comorbidities and American Society of Anesthesiologists (ASA) rating scale [40]. Medical comorbidities were assessed using the modified Charlson’s Comorbidity Index [41]. In a study of 400 hip fracture patients, Mullen and Mullen [42] found that 94 % of delirium cases were associated with at least a medical complication and concluded that, deterioration in mental status postoperatively was in most cases a symptom of an organic complication that needed to be diagnosed. This meta-analysis found that number of medical comorbidities and ASA physical status class 2 and 3 were important factors in delirium risk assessment. The findings also suggest that patients with advanced age or those who were already functionally impaired before the fracture or who had premorbid psychiatric problems or a high number of medical complication should be closely monitored because they are at risk for developing delirium after hip surgery.
Patients who developed delirium postoperatively were more often males, had experienced perioperative hypotension or perioperative blood pressure falls and had more postoperative complications such as infections and depressed mood than those who remained lucid during their stay in hospital [43]. The poorer outcome for men might be at least partly caused by the higher incidence of delirium [43]. Recently, a systematic review of preoperative risk factors for delirium after noncardiac surgery demonstrated that there is insufficient evidence to support an association between male gender and delirium based on pooled analysis of ten studies [44].
Opioids could be psychotogenic by enhancing the activity of the ventral tegmental area dopamine neurons through μ-opioid receptors located on GABA neurons within the ventral tegmental area [45], thereby increasing dopamine release in the nucleus accumbens [46]. According to our results, patients exposed to the use of morphine were 3.01 times more at risk of developing delirium after hip fracture surgery than nonusers. Gaudreau et al. [47] found that patients exposed to daily doses of morphine higher than 90 mg were 2.1 times more at risk of developing delirium than patients who were exposed to smaller doses. Yet, the results of previous studies on the opioids–delirium association are inconsistent. Morrison et al. [29] found an increased risk of delirium for patients exposed to doses less than 10 mg of daily morphine equivalents, compared to patients exposed to more than 30 mg, whereas another study found an increased risk of delirium for patients exposed to doses ranging from 18.6 to 331.6 mg compared to nonusers [48]. The pattern of the opioids–delirium relationship obviously should be further investigated. Pain is one of the main reasons for the cause of postoperative delirium [49] and the effective analgesic action of venous self-control analgesic pump may be offset by the potential risk of opioid-induced delirium.
In the current study, total hip arthroplasty was a risk factor for postoperative delirium. Patients who undergo elective surgery are also impressionable [50] in spite of the relatively predictable perioperative course, the presence of fewer risk factors, and the relatively physical health of these patients. Other factors related to surgery, such as delay of the surgical procedure, anesthesia technique, duration of anesthesia and intraoperative blood loss in surgery were not found to be risk factors. This may also relate to the similarity in those factors between patients experiencing delirium and those non-delirious.
Because nursing home residents may be more likely than community-dwelling elderly people to sustain a fall and possibly a hip fracture [51], it was postulated a priori that, in studies with both hip fracture and elective orthopedic procedures, there might be a greater incidence of delirium in institutionalized patients than in single surgery-type studies.
Sensory impairment is a risk factor for falls [52] and could therefore possibly lead to a greater risk of hip fracture, but in our study hearing or visual loss did not result as risk factors for delirium after hip surgery.
Four studies reported hospitalization after surgery of 11.2 days in postoperative delirium patients, which was 1.1 days longer than that in nondelirium groups, and at the same time, they were discharged more frequently to rehabilitation facilities or to other living arrangements than their pre-fracture residence [28].
Some limitations in this meta-analysis have to be mentioned. Firstly, a weakness exists in the analyses, in which not all the ORs regarding the potential risk factors applied for the meta-analysis were adjusted because a lot of reports could only provide the univariate rather than multivariate statistics.
Likewise, some studies might choose not to report insignificant results or results of no interest, potentially resulting in a considerable amount of missing data. Hence, our overall effect may be somewhat an overestimate. Secondly, most of the included studies were observational and therefore with inevitable recall and interviewer biases, which might affect the associations between the risk factor and delirium. Thirdly, the measurements of various risk factors differed from each other, and follow-up periods ranged widely from several months to several years. Therefore, a significant heterogeneity was unavoidable in this review. However, after sensitive analyses, heterogeneity was resolved (I 2 < 50 %), showing analyses were robust and the results reliable. Fourthly, there might be operator dependent and append subjective factors in the quality of assessment process. Nevertheless, the two reviewers evaluated the identified studies independently and any disagreement was resolved by discussion and consensus. Although this meta-analysis investigates some risk factors for postoperative delirium after hip fracture surgery, we should treat these results cautiously on the background of potential defects, and more research studies with larger sample size and better design should be conducted.
Although some limitations were unavoidable, this study has some merits. First, the search style based on the computer and manual search ensures a complete inclusion of relevant studies. Secondly, no significant heterogeneity was observed in most variables except for the item of active external rotation; even so, heterogeneity was diminished using sensitivity analysis and this did not alter the result. Last but most important, this is by far the first study to quantitatively summarize the risk factors for the development of delirium after hip fracture surgery in elderly patients.
References
Nie H, Zhao B, Zhang YQ et al (2012) Pain and cognitive dysfunction are the risk factors of delirium in elderly hip fracture Chinese patients. Arch Gerontol Geriatr 54:e172–e174. doi:10.1016/j.archger.2011.09.012
Wang NY, Hirao A, Sieber F (2015) Association between intraoperative blood pressure and postoperative delirium in elderly hip fracture patients. PLoS One 10:e0123892. doi:10.1371/journal.pone.0123892
Lee KH, Ha YC, Lee YK et al (2011) Frequency, risk factors, and prognosis of prolonged delirium in elderly patients after hip fracture surgery. Clin Orthop Relat Res 469:2612–2620. doi:10.1007/s11999-011-1806-1
Marcantonio ER, Flacker JM, Michaels M et al (2000) Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc 48:618–624
Santana Santos F, Wahlund LO, Varli F et al (2005) Incidence, clinical features and subtypes of delirium in elderly patients treated for hip fractures. Dement Geriatr Cogn Disord 20:231–237. doi:10.1159/000087311
Chen XW, Shi JW, Yang PS et al (2014) Preoperative plasma leptin levels predict delirium in elderly patients after hip fracture surgery. Peptides 57:31–35. doi:10.1016/j.peptides.2014.04.016
Dolan MM, Hawkes WG, Zimmerman SI et al (2000) Delirium on hospital admission in aged hip fracture patients: prediction of mortality and 2-year functional outcomes. J Gerontol Ser A Biol Sci Med Sci 55:M527–M534
Goldenberg G, Kiselev P, Bharathan T et al (2006) Predicting post-operative delirium in elderly patients undergoing surgery for hip fracture. Psychogeriatrics 6:43–48. doi:10.1111/j.1479-8301.2006.00146.x
Lee HB, Mears SC, Rosenberg PB et al (2011) Predisposing factors for postoperative delirium after hip fracture repair in individuals with and without dementia. J Am Geriatr Soc 59:2306–2313. doi:10.1111/j.1532-5415.2011.03725.x
Meziere A, Paillaud E, Belmin J et al (2013) Delirium in older people after proximal femoral fracture repair: role of a preoperative screening cognitive test. Ann Fr Anesth Reanim 32:e91–e96. doi:10.1016/j.annfar.2013.06.006
Muangpaisan W, Wongprikron A, Srinonprasert V et al (2015) Incidence and risk factors of acute delirium in older patients with hip fracture in Siriraj Hospital. J Med Assoc Thail 98:423–430
Shen Y, Shen H, Zhang W et al (2013) Risk factors for delirium of elderly patients undergoing hip fracture operation. Natl Med J China 93:3276–3279
Wang X, Miao W, Huang G (2008) CHnical investigation of postoperative delirium in elderly hip-surgery patients. Chin J Geriatr 27:99–102
Wu D, Hao H, Zhu J et al (2015) Risk factors analysis for postoperative delirium of elderly hip fracture patients. Chin J Geriatr Orthop Rehabil 1:34–38
Moerman S, Tuinebreijer WE, de Boo M et al (2012) Validation of the risk model for delirium in hip fracture patients. Gen Hosp Psychiatry 34:153–159. doi:10.1016/j.genhosppsych.2011.11.011
Gruber-Baldini AL, Zimmerman S, Morrison RS, Grattan LM et al (2003) Cognitive impairment in hip fracture patients: timing of detection and longitudinal follow-up. J Am Geriatr Soc 51:1227–1236
Lundstrom M, Edlund A, Bucht G et al (2003) Dementia after delirium in patients with femoral neck fractures. J Am Geriatr Soc 51:1002–1006
DSMIV-RD (2000) Statistical manual of mental disorders, text revision (DSM IV-R). American Psychiatric Association, Washington
Inouye SK, van Dyck CH, Alessi CA et al (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 113:941–948
Stang A (2010) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. doi:10.1007/s10654-010-9491-z
Lau J, Ioannidis JP, Schmid CH (1997) Quantitative synthesis in systematic reviews. Ann Intern Med 127:820–826
Wei J, Yang TB, Luo W et al (2013) Complications following dorsal versus volar plate fixation of distal radius fracture: a meta-analysis. J Int Med Res 41:265–275. doi:10.1177/0300060513476438
Kalisvaart KJ, Vreeswijk R, de Jonghe JF et al (2006) Risk factors and prediction of postoperative delirium in elderly hip-surgery patients: implementation and validation of a medical risk factor model. J Am Geriatr Soc 54:817–822. doi:10.1111/j.1532-5415.2006.00704.x
Westhoff D, Witlox J, Koenderman L et al (2013) Preoperative cerebrospinal fluid cytokine levels and the risk of postoperative delirium in elderly hip fracture patients. J Neuroinflamm 10:122. doi:10.1186/1742-2094-10-122
Galanakis P, Bickel H, Gradinger R et al (2001) Acute confusional state in the elderly following hip surgery: incidence, risk factors and complications. Int J Geriatr Psychiatry 16:349–355
Juliebo V, Bjoro K, Krogseth M et al (2009) Risk factors for preoperative and postoperative delirium in elderly patients with hip fracture. J Am Geriatr Soc 57:1354–1361. doi:10.1111/j.1532-5415.2009.02377.x
Schuurmans MJ, Duursma SA, Shortridge-Baggett LM et al (2003) Elderly patients with a hip fracture: the risk for delirium. Appl Nurs Res (ANR) 16:75–84
Duppils GS, Wikblad K (2000) Acute confusional states in patients undergoing hip surgery. a prospective observation study. Gerontology 46:36–43. doi10.1159/000022131
Morrison RS, Magaziner J, Gilbert M et al (2003) Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol Ser Biol Sci Med Sci 58:76–81
Torbergsen AC, Watne LO, Frihagen F et al (2015) Vitamin deficiency as a risk factor for delirium. Eur Geriatr Med 6:314–318. doi:10.1016/j.eurger.2014.09.002
Hu W, Zhou M, Tan Z et al (2014) Analysis on the risk factors of postoperative delirium in aged hip fracture patients. J Trauma Surg 16:324–327
Lipowski ZJ (1983) Transient cognitive disorders (delirium, acute confusional states) in the elderly. Am J Psychiatry 140:1426–1436. doi:10.1176/ajp.140.11.1426
Cole MG, Ciampi A, Belzile E et al (2009) Persistent delirium in older hospital patients: a systematic review of frequency and prognosis. Age Ageing 38:19–26. doi:10.1093/ageing/afn253
Cole MG, McCusker J, Dendukuri N et al (2002) Symptoms of delirium among elderly medical inpatients with or without dementia. J Neuropsychiatry Clin Neurosci 14:167–175. doi:10.1176/jncn.14.2.167
Blass JP, Gibson GE (1999) Cerebrometabolic aspects of delirium in relationship to dementia. Dement Geriatr Cogn Disord 10:335–338. doi:10.1159/000017165
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Hanson MR, Galvez-Jimenez N (2004) Management of dementia and acute confusional states in the perioperative period. Neurol Clin 22:vii–viii, 413–422. doi:10.1016/j.ncl.2004.01.001
Sato N, Sanuki M, Matsumoto C et al (2000) Perioperative temporal profile of cognitive function in elderly patients undergoing hip surgery. J Geriatr Psychiatry Neurol 13:206–209
van der Mast RC (1998) Pathophysiology of delirium. J Geriatr Psychiatry Neurol 11:138–145 (discussion 157-138)
Owens WD, Felts JA, Spitznagel EL Jr (1978) ASA physical status classifications: a study of consistency of ratings. Anesthesiology 49:239–243
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Mullen JO, Mullen NL (1992) Hip fracture mortality. A prospective, multifactorial study to predict and minimize death risk. Clin Orthop Relat Res 280:214–222
Edlund A, Lundstrom M, Brannstrom B et al (2001) Delirium before and after operation for femoral neck fracture. J Am Geriatr Soc 49:1335–1340
Dasgupta M, Dumbrell AC (2006) Preoperative risk assessment for delirium after noncardiac surgery: a systematic review. J Am Geriatr Soc 54:1578–1589. doi:10.1111/j.1532-5415.2006.00893.x
Tomkins DM, Sellers EM (2001) Addiction and the brain: the role of neurotransmitters in the cause and treatment of drug dependence. Can Med Assoc J (CMAJ) 164:817–821
Cowen MS, Lawrence AJ (1999) The role of opioid–dopamine interactions in the induction and maintenance of ethanol consumption. Prog Neuropsychopharmacol Biol Psychiatry 23:1171–1212
Gaudreau JD, Gagnon P, Harel F et al (2005) Psychoactive medications and risk of delirium in hospitalized cancer patients. J Clin Oncol 23:6712–6718. doi:10.1200/jco.2005.05.140
Dubois MJ, Bergeron N, Dumont M et al (2001) Delirium in an intensive care unit: a study of risk factors. Intensive Care Med 27:1297–1304
Vaurio LE, Sands LP, Wang Y et al (2006) Postoperative delirium: the importance of pain and pain management. Anesth Analg 102:1267–1273. doi:10.1213/01.ane.0000199156.59226.af
Jankowski CJ, Trenerry MR, Cook DJ et al (2011) Cognitive and functional predictors and sequelae of postoperative delirium in elderly patients undergoing elective joint arthroplasty. Anesth Analg 112:1186–1193. doi:10.1213/ANE.0b013e318211501b
Rao SS (2005) Prevention of falls in older patients. Am Fam Phys 72:81–88
Williams-Russo P, Urquhart BL, Sharrock NE et al (1992) Post-operative delirium: predictors and prognosis in elderly orthopedic patients. J Am Geriatr Soc 40:759–767
Acknowledgments
We are grateful to C.W. and Y.Z. of the Department of Orthopedics, and to D.T. and Z.L. of the Department of Statistics and Applications for their kind assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Y. Yang and X. Zhao contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yang, Y., Zhao, X., Dong, T. et al. Risk factors for postoperative delirium following hip fracture repair in elderly patients: a systematic review and meta-analysis. Aging Clin Exp Res 29, 115–126 (2017). https://doi.org/10.1007/s40520-016-0541-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0541-6