Abstract
Objective
To examine whether a set of well-known predictors of mortality in younger elderly also maintain their importance in Chinese oldest old group.
Design
A cross-sectional study of 1401 inhabitants aged 90 and older were conducted in the area of Dujiangyan, China. 825 subjects participated and were followed up for vital status after 49 months. Professional interviewers collected baseline data concerning socio-demographic characteristics, lifestyle habits, physical factors and geriatric assessment. Bivariate analysis was conducted between survivors and deceased. Cox regression models were used to evaluate predictors of mortality.
Results
Four hundred and thirty-six (52.8 %) of 825 participants eligible for the analysis died during the 49 months of follow-up period. Older age, comorbidity, lower MMSE score, lower ADL and IADL scores increased the risk of mortality in the study group. Multivariate analyses showed older age (HR = 1.03, 95 % CI 1.01–1.07) and comorbidity (HR = 1.09, 95 % CI 1.02–1.17) were associated with mortality while female gender (HR = 0.61, 95 % CI 0.43–0.86), taking exercise (HR = 0.80, 95 % CI 0.64–1.01) and higher MMSE scores (HR = 0.96, 95 % CI 0.94–0.99) showed a positive effect on survival.
Conclusion
In Chinese nonagenarians and centenarians, age, gender, taking exercise, cognitive impairment and comorbidity at baseline show predictive power of oldest old mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The world population is aging. The nonagenarians and centenarians are the fast-growing segment of the population in recent decades both in developed country and China [1–3]. The oldest old are more prone to suffer from frailty, cognitive impairment, disability and chronic conditions compared with younger elderly [4–7].
A large body of research in elderly subjects had shown that several socio-demographic, lifestyle, physical, functional factors predicted mortality such as gender [8, 9], education [8, 10], marital status [11], self-rate health [9, 11, 12] smoking [11], drinking tea [13], depression [14], cognitive impairment [15], function status [9, 11, 16] and comorbidities [11]. Nevertheless, few studies have prospectively examined predictors of mortality in nonagenarian and centenarians and showed inconsistent results [3, 7, 17, 18]. The study of Danish 1905 cohort survey followed for 15 months reported that conventional risk factors such as socio-demographic factors, smoking, obesity lost importance in predicting death and have been replaced by disability and cognitive impairment [3]. Similarly in NonaSantfeliu study aged 90 and older, Charlson index and cognitive status were the independent risk factors for 5- and 7-year mortality [17, 19]. Whereas, conventional known factors such as gender, self-rate health in the Vitality 90+ study still predicted death after 9-year follow-up [18].
In the present study, we evaluated long-term follow-up (49 months) in a cohort of non-selected population sample aged 90 or older. The objective of this study was to identify whether a set of well-known predictors of mortality in younger elderly also maintain their importance in Chinese oldest old group.
Subjects and methods
Study participants
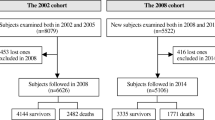
The data were taken from Project of Longevity and Aging in Dujiangyan (PLAD), which was a population-based study of nonagenarians and centenarian in the city of Dujiangyan (Sichuan province in southwest China) in July 2005. The method of this study had been reported in detail elsewhere [20]. In brief, all 1401 nonagenarian residents in this city were contacted, and 62 % (n = 870 participants) replied. Socio-demographic characteristics, lifestyle habits, physical conditions and geriatric assessment were recorded and performed by trained personnel during face to face interview. Informed consent was obtained from all participants (or their legal proxies). The Research Ethics Committee of the Sichuan University approved this study protocol.
Assessment of predictor variables
Socio-demographics
Questions about age, gender, marital status and education level.
Lifestyle habits
Participants were questioned whether they have habits (including current and past) of smoking, drinking alcohol, drinking tea and taking exercise.
Physical conditions
Self-rated health
Self-rated health was assessed by the answer to the question “How would you rate your own health” (very good, good, fair, poor, very poor). Because of low response, the ‘very good’ were combined with “good” and ‘very poor’ with “poor” separately for statistical analysis.
Body mass index
Body mass index was calculated as weight in kilograms divided by height in meters squared.
Blood pressure
Systolic blood pressure and diastolic blood pressure were defined by the mean of two out of three measures using standard protocol.
Comorbidities
The prevalence of 18 common medical conditions (comorbidity) was determined using a checklist that followed the question: ‘‘Do you suffer, or were you ever told by a doctor that you suffer, from the following problems in the past 1 year?’’ Chronic diseases included cardiovascular disease and hypertension, diabetes mellitus, obstructive pulmonary disease, malignancy, Parkinson’s disease, arthritis or osteoarthritis, chronic kidney disease, etc. The number of the comorbidities was calculated for analysis.
Global geriatric assessment
Depression scores
Depression was measured by geriatrics depression scale Chinese-edition (GDS-CD). GDS-CD including 23 items (each has 2 options: yes or no) is commonly used for depression test in Chinese elderly and a score above 10 usually defined as depression, which has been shown to be both above 85 % sensitive and specific in previous studies [21, 22].
Cognitive function
Cognitive function was measured using the Chinese version of Mini-Mental State Examination (MMSE), Cognitive impairment was graded as severe (0–17 points), mild (18–23 points), and not present (24–30 points). This score has been shown to be 80–90 % sensitive and 80–100 % specific for a diagnosis of dementia [23].
Disability
Functional status was measured using the 6-item Barthel index (BI) for basic activities of daily living (BADL), and the 9-item Lawton and Brody index (LI) for instrumental activities of daily living (IADL). Competence is categorized on a 4-point scale ranging from complete disability (4), severe difficulty (3), some difficulty (2), or no difficulty (1). A summed score was calculated for BADL and IADL separately.
Overall 49-month mortality
Vital status for the total cohort was evaluated after 49 months in August 2009 and was confirmed by local civil affair department. Nevertheless, 47 patients (missing rate 5.4 %) lost contact because of various reasons. Patients who had survived were compared with those deceased.
Statistical analysis
SPSS 22.0 statistical software (SPSS Inc, Chicago, IL, USA) was used to perform the analyses. Normally, distributed continuous variables are reported as mean ± standard deviation (SD). Categorical variables are reported as frequency and proportions. Student’s t test was used to compare normally distributed continuous variables and the Chi-square statistic or Fisher’s exact test was used to compare categorical or dichotomous variables.
The 49-month survival rate was evaluated. Cox proportional-hazard regression analysis was used to model the time to death data to identify possible predictors of mortality. Adjusted hazard ratios using data on persons who only had no missing values in any of the variables were calculated. Gender, education, marital status, living alone, self-rate health, smoking, drinking alcohol, drinking tea, taking exercise were used as categorical variables in the analysis. Age, systolic BP, diastolic BP, BMI, comorbidities, MMSE, GDS-CD, BADL, IADL were used as continuous variables. First we estimated the unadjusted association between each variable and mortality, then conducted four mutually adjusted models with mortality: (1) Model 1: (age, gender, education, marital status, living alone and religion); (2) Model 2: model 1 + lifestyle habits (smoking, drinking alcohol, drinking tea, and taking exercise); (3) Model 3: model 2 + physical health (self-rated health, systolic pressure, diastolic pressure, BMI, and comorbidities); (4) Model 4: model 3 + geriatric assessment (GDS-CD, MMSE, BADL and IADL). The results were considered significant when P < 0.05.
Result
Baseline characteristics
The sample of 825 oldest nonagenarians was 90–108 years at baseline, comprising 561 (68 %) women and 264 (32 %) men, with a mean age of 93.6 ± 3.4 years and 27.9 % literacy rate. 11.3 % of sample (n = 93) had a living spouse and 51 (6.2 %) were living alone. With regard to lifestyle habits, 63.3 % (n = 508) of subjects had history (no matter past or current) of smoking, 44.6 % (n = 359) drinking alcohol, 48.4 % (n = 387) drinking tea and 45.0 % (355) taking exercise. Most of the subjects (n = 437, 56.8 %) rated their health good, 18.6 % (143) rated bad and 24.7 % (n = 190) acceptable. The mean values of geriatric assessment scales at the beginning of the follow-up study period were: MMSE 14.97 ± 5.9; GDS-CD 5.41 ± 4.4; BADL 7.10 ± 2.2, IADL 11.19 ± 6.7. The mean body mass index was 19.23 ± 3.6.
Evaluation after 49-month follow-up
436 patients died during the 49-month follow-up period (52.8 %), giving in the overall cohort an annual average mortality of 17.1 %, distributed as follows: 9.9 % for the first year, 15.0 % for the second, 21.7 % for the third, 21.3 % for the last 13-month follow-up. The median survival rate was 45.5 months.
Predictor of mortality
The bivariate analysis of baseline variables associated with 49-month survival is shown in Table 1. Patients who did not survive were significantly older, had lower functional (BADL and IADL) and cognitive performance (MMSE), as well as higher comorbidity. The unadjusted Cox analysis identified age, habit of taking exercise, bad self-rated health, comorbidity, BADL and IADL as predictor of mortality (Table 2). In adjusted Cox multivariate analysis, age (HR = 1.03, 95 % CI 1.00–1.06) was the only risk factor associated with mortality in Model 1, and in Model 2 age (HR = 1.03, 95 % CI 1.01–1.06) was still the independent predictor of mortality and taking exercise (HR = 0.81, 95 % CI 0.66–0.99) was shown to be a protective factor (Table 2). When adding the variables of physical factors in Model 3, age (HR = 1.04, 95 % CI 1.01–1.08) and comorbidity (HR = 1.12, 95 % CI 1.05–1.20) were all positively and independently associated with subsequent mortality. Female gender (HR = 0.70, 95 % CI 0.51–0.97) and taking exercise (HR = 0.79, 95 % CI 0.63–0.98) showed protective effect. In the last model comprising all covariates, age (HR = 1.03, 95 % CI 1.01–1.07) and comorbidity (HR = 1.09, 95 % CI 1.02–1.17) were still associated with mortality while female gender (HR = 0.61, 95 % CI 0.43–0.86), taking exercise (HR = 0.80, 95 % CI 0.64–1.01) and MMSE scores (HR = 0.96, 95 % CI 0.94–0.99) showed a positive effect on survival (Table 2).
Discussion
The results of our study showed a lower 49-month mortality rate, estimated to be 52.8 % in these nonagenarians and centenarian compared with studies of similar follow-up period. In two previous studies after 4 years of follow-up, mortality was found to be 60 % in Finnish nonagenarian and 62.3 % in Spanish nonagenarian [19, 24]. This difference could partly be explained due to relatively low response rate of very old subjects (62.2 %) in this study and different genetic, functional and environmental factors among various aged cohorts.
The study also demonstrated that factors, often found to predict mortality in younger elderly, such as low education, marital status, smoking, BMI, self-rated health and depression, obviously lost their importance. Male gender, lack the habit of taking exercise, higher comorbidity and cognitive impairment at baseline were independently associated with 49-month mortality in this cohort of oldest.
Both age and sex are the common basic predictors of mortality in younger elderly and oldest old in the literatures [9, 12, 18, 25]. Similarly in our study, younger and female participants had a lower probability of dying. With regards to other socio-demographic factors, we found no significant influence on mortality according to literacy, marital status and living alone. These findings replicate results found in other nonagenarian cohorts [3, 17, 19, 26]. As for religion, our result showed no association with mortality, which contradicted the existing literature in the oldest old. A possible explanation may be attributed to different age range of study population, that one is aged 75–94 years and another 80–105 [27, 28].
Lifestyle factors, such as smoking, alcohol consumption and taking exercise, had been reported to influence mortality in older population but seldom investigated in 90+ or older age [29–31]. In Danish 1905-cohort survey, both smoking and alcohol consumption had no significant effect on mortality in nonagenarian, which was consistent with our findings [3]. This suggests that persons who step into their 90s have the genetic and/or environmental factors in protecting them against toxicity of cigarette and alcohol. Taking exercise had a beneficial effect on mortality in our study, which parallels the results from two Chinese and Israel aged cohorts [9, 28]. An elderly who has the habit of taking exercise is less likely to be frail, disabled, cognition impaired or with fewer chronic diseases which may interplay the result. With regards to tea consumption, a Chinese study of 80+ oldest old demonstrated a 10 % mortality risk reduction associated with consistent frequent tea, but this was not shown in our analysis [9]. A possible explanation might be attributed to different age range and lack of prominent predictors, such as comorbidity and cognitive status in its adjusted model, which strengthened its predictive power in tea consumption [9]. A limitation in this study is that we did not collect more detailed information on the types and quantity of lifestyle factors in estimating the effects on mortality.
Comorbidity is commonly present in the oldest old population. In our study, comorbidity was measured by self-reported number of 17 diseases and shown to be independently associated with 49-month mortality, which was in accordance with NonaSantfeliu study after 5- and 7-year follow-up [17, 19]. Nevertheless, this finding was not consistent with Danish 1905-cohort survey and Vitality 90+ study [3, 18]. These contradictory results might be explained by difference in calculating diseases among studies, for example, in Danish 1905-cohort it contained 31 diseases in the list but in Vitality 90+ study only 7 diseases. Furthermore, these findings should be interpreted with caution, because the severity of each disease was not taken into account. Greater BMI is often found to be a protective factor on mortality in older people [32, 33], but less investigated in nonagenarian or older [34]. In our study, no relationship between BMI and mortality was found after adjusting all covariates, which parallels the results from the 1905-cohort study [3]. With regards to self-rated health, it is a common predictor of mortality in the younger elderly [9, 11, 35]. In this study, poor self-rated health was associated with mortality in unadjusted model in the whole group, but did not reach significance in multivariate analysis, which is in line with results only on male gender in studies of nonagenarian [3, 18].
Low cognitive functioning has been one of the most consistent and sustaining predictors of mortality in old age regardless of different measurement in studies [3, 15, 17, 19, 25]. In our survey, we used MMSE score as a measure of cognitive functioning and also found protective effect (HR = 0.96, 95 % CI 0.94–0.99). A decline in functional status has been reported as a significant predictor for mortality in oldest old [3, 9, 18, 36]. Although ADL and IADL were also found to be predictors of mortality in the univariate analyses in our study, they lost predictive value after adjustment for common confounders. A likely explanation is that disability in the oldest old is interplayed between gender difference, sedentary lifestyle, cognitive functioning and comorbidity [3, 37, 38]. It is possible that the unique predictive aspects of disability are diffused in the presence of other prominent predictors of mortality. Depressive symptom, measured by brief 23-item geriatric depression scale Chinese-edition in our study, was not found to make a unique contribution to the set of mortality, which parallels the results from the Israel old–old population using the Center for Epidemiologic Studies Depression Scale after 6-, 8-, 10- and 12-year follow-up [9].
In contrast to what is known of well-established mortality risk factors among younger elderly, such as education, marital status, smoking, BMI and depression, our findings seem to support the “common cause” theory in the oldest old that degenerative biological processes lead to the deterioration of physical and mental functioning [39]. Age, gender difference and comorbidity might be influential factors to biological deterioration. Taking exercise is likely to postpone the degenerative processes. Another possible explanation is demographic selection that only persons with favorable genetic makeup and adaptive environmental characteristics could survive, the frailest persons die.
Several limitations of this study should be considered. First, the longitudinal cohort provides evidence of predictive association with oldest old population from Dujiangyan city; therefore, the results should be cautious to generalize to all Chinese nonagenarians. Second, the multivariate analytical strategy using only persons who had no missing data may have introduced some bias. For example, 232 subjects were excluded in model 4 in comparison with model 1 because of missing data, which may influence the predictive value of geriatric assessment variables. Third, the result has partly been affected in a non-generalisable way by 2008 Wenchuan earthquake near Dujiangyan [40]. Finally, causes of death were not recorded.
In conclusion, factors predicting mortality in the oldest old differ from findings in studies of younger elderly. Our study highlights the importance of age, gender, sedentary lifestyle, poor cognition and comorbidity as predictors of long-term mortality among the Chinese population aged 90 and older.
References
Formiga F, Pujol R, Perez-Castejon JM et al (2005) Low comorbidity and male sex in nonagenarian community-dwelling people are associated with better functional and cognitive abilities: the NonaSantfeliu study. J Am Geriatr Soc 53(10):1836–1837
Administry Ca (2007) The research report of Chinese aging trend. Chinese Women’s Movement 2007(2)
Nybo H, Petersen HC, Gaist D et al (2003) Predictors of mortality in 2,249 nonagenarians—the Danish 1905-Cohort Survey. J Am Geriatr Soc 51(10):1365–1373
Nybo H, Gaist D, Jeune B et al (2001) Functional status and self-rated health in 2,262 nonagenarians: the Danish 1905 Cohort Survey. J Am Geriatr Soc 49(5):601–609
Xie J, Matthews FE, Jagger C et al (2008) The oldest old in England and Wales: a descriptive analysis based on the MRC Cognitive Function and Ageing Study. Age Ageing 37(4):396–402
Yue JR, Dong BR, Huang CQ et al (2009) Cognitive impairment and medical illness in Chinese nonagenarians and centenarians. J Am Geriatr Soc 57(4):734–736
Lee SJ, Go AS, Lindquist K et al (2008) Chronic conditions and mortality among the oldest old. Am J Public Health 98(7):1209–1214
Crimmins EM, Hayward MD, Saito Y (1996) Differentials in active life expectancy in the older population of the United States. J Gerontol B Psychol Sci Soc Sci 51(3):S111–S120
Ben-Ezra M, Shmotkin D (2006) Predictors of mortality in the old-old in Israel: the cross-sectional and Longitudinal Aging Study. J Am Geriatr Soc 54(6):906–911
Liu X, Hermalin AI, Chuang YL (1998) The effect of education on mortality among older Taiwanese and its pathways. J Gerontol B Psychol Sci Soc Sci 53(2):S71–82
Simons LA, McCallum J, Friedlander Y et al (1996) Predictors of mortality in the prospective Dubbo study of Australian elderly. Aust N Z J Med 26(1):40–48
Benyamini Y, Blumstein T, Lusky A, Modan B (2003) Gender differences in the self-rated health-mortality association: is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist 43(3):396–405 (discussion 372–395)
Ruan R, Feng L, Li J et al (2013) Tea consumption and mortality in the oldest-old Chinese. J Am Geriatr Soc 61(11):1937–1942
Cuijpers P, Smit F (2002) Excess mortality in depression: a meta-analysis of community studies. J Affect Disord 72(3):227–236
Dewey ME, Saz P (2001) Dementia, cognitive impairment and mortality in persons aged 65 and over living in the community: a systematic review of the literature. Int J Geriatr Psychiatry 16(8):751–761
Scott WK, Macera CA, Cornman CB et al (1997) Functional health status as a predictor of mortality in men and women over 65. J Clin Epidemiol 50(3):291–296
Formiga F, Ferrer A, Chivite D et al (2011) Survival after 7 years of follow-up at ninety. The NonaSantfeliu study. Eur J Intern Med 22(6):e164–165
Tiainen K, Luukkaala T, Hervonen A et al (2013) Predictors of mortality in men and women aged 90 and older: a nine-year follow-up study in the Vitality 90+ study. Age Ageing 42(4):468–475
Formiga F, Ferrer A, Chivite D et al (2011) Predictors of long-term survival in nonagenarians: the NonaSantfeliu study. Age Ageing 40(1):111–116
Zhou Y, Flaherty JH, Huang CQ et al (2010) Association between body mass index and cognitive function among Chinese nonagenarians/centenarians. Dement Geriatr Cogn Disord 30(6):517–524
Chan AC (1996) Clinical validation of the Geriatric Depression Scale (GDS): Chinese version. J Aging Health 8(2):238–253
Liu CY, Lu CH, Yu S et al (1998) Correlations between scores on Chinese versions of long and short forms of the Geriatric Depression Scale among elderly Chinese. Psychol Rep 82(1):211–214
Tombaugh TN, McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 40(9):922–935
Hurme M, Paavilainen PM, Pertovaara M et al (2005) IgA levels are predictors of mortality in Finnish nonagenarians. Mech Ageing Dev 126(6–7):829–831
Lima-Costa MF, Peixoto SV, Matos DL et al (2011) Predictors of 10-year mortality in a population of community-dwelling Brazilian elderly: the Bambui Cohort Study of Aging. Cad Saude Publica 27(Suppl 3):S360–369
Enroth L, Raitanen J, Hervonen A et al (2015) Is socioeconomic status a predictor of mortality in nonagenarians? The vitality 90+ study. Age Ageing 44(1):123–129
Walter-Ginzburg A, Shmotkin D, Blumstein T et al (2005) A gender-based dynamic multidimensional longitudinal analysis of resilience and mortality in the old-old in Israel: the cross-sectional and longitudinal aging study (CALAS). Soc Sci Med 60(8):1705–1715
Zhang W (2008) Religious participation and mortality risk among the oldest old in China. J Gerontol B Psychol Sci Soc Sci 63(5):S293–S297
Ferrucci L, Izmirlian G, Leveille S et al (1999) Smoking, physical activity, and active life expectancy. Am J Epidemiol 149(7):645–653
Simons LA, McCallum J, Friedlander Y et al (1996) Alcohol intake and survival in the elderly: a 77 month follow-up in the Dubbo study. Aust N Z J Med 26(5):662–670
Fried LP, Kronmal RA, Newman AB et al (1998) Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA 279(8):585–592
Nagai M, Kuriyama S, Kakizaki M et al (2010) Effect of age on the association between body mass index and all-cause mortality: the Ohsaki cohort study. J Epidemiol 20(5):398–407
Stevens J, Cai J, Pamuk ER et al (1998) The effect of age on the association between body-mass index and mortality. N Engl J Med 338(1):1–7
Dahl AK, Fauth EB, Ernsth-Bravell M et al (2013) Body mass index, change in body mass index, and survival in old and very old persons. J Am Geriatr Soc 61(4):512–518
Jylha M (2009) What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 69(3):307–316
Taekema DG, Gussekloo J, Westendorp RG et al (2012) Predicting survival in oldest old people. Am J Med. 125(12):1188–1194 e1181
Ferrucci L, Guralnik JM, Simonsick E et al (1996) Progressive versus catastrophic disability: a longitudinal view of the disablement process. J Gerontol A Biol Sci Med Sci 51(3):M123–130
Beckett LA, Brock DB, Lemke JH et al (1996) Analysis of change in self-reported physical function among older persons in four population studies. Am J Epidemiol 143(8):766–778
Christensen H, Mackinnon AJ, Korten A et al (2001) The “common cause hypothesis” of cognitive aging: evidence for not only a common factor but also specific associations of age with vision and grip strength in a cross-sectional analysis. Psychol Aging 16(4):588–599
Flaherty JH, Dong B, Wu H et al (2011) Observational study of 1-year mortality rates before and after a major earthquake among Chinese nonagenarians. J Gerontol A Biol Sci Med Sci A (3):355–361
Acknowledgments
This work was supported by the Discipline Construction Foundation of Sichuan University and by grants from the Project of Science and Technology Bureau of Sichuan Province (2006Z09-006-4), and in part by the Center of Coordination and Innovation for Aging Care and Health Promotion of Sichuan. The authors thank the staff of the Department of Geriatrics Medicine, West China Hospital and Dujiangyan Hospital, and all participants (as well as their legal proxies) for their great contribution.
Conflict of interest
The authors indicate no potential conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Research Ethics Committee of the Sichuan University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants (or their legal proxies).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zou, C., Zhou, Y., Dong, B. et al. Predictors of 49-month mortality in Chinese nonagenarians and centenarians in PLAD study. Aging Clin Exp Res 27, 821–827 (2015). https://doi.org/10.1007/s40520-015-0355-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-015-0355-y