Abstract
Objectives
The association between muscle mass and cognitive impairment (CI) is conflicting. We aimed to evaluate and compare the associations of muscle strength, muscle mass and CI risk in maintenance hemodialysis (MHD) patients.
Methods
We conducted a multicenter, cross-sectional study. Cognitive function was assessed with the Mini-Mental State Examination (MMSE) score. Muscle strength was assessed by hand grip strength (HGS), muscle mass was assessed by lean tissue mass (LTM). Education status was divided into two groups: lower education status (senior middle school and below) and higher education status (high school and above). Multivariable logistic regression models and subgroup analyses were performed. Receiver-operating characteristic (ROC) analyses were conducted to compare their predictive power in discriminating CI.
Results
2827 adult MHD patients were included in our final analysis. Patients in the lowest quartile of HGS was 2.82-fold as likely to have CI as compared to those in the highest quartile, while participants in the lowest quartile of LTM group were 1.52-fold as likely to have CI, when compared with the highest quartile group of LTM after adjusting for age, gender and education level. The association persisted in all subgroups except for women and well-educated participants. There was a significant interaction between HGS and education status on CI and age played an interactive role in the association between LTM and incident CI (P for interaction < 0.05). The AUC value of the HGS was significantly higher than that of LTM (0.69 VS 0.63, P < 0.001).
Conclusions
Muscle strength performed better than muscle mass in identifying individuals at high risk of CI, particularly in male and less educated Chinese MHD patients.
Level of evidence
Level V, cross-sectional study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cognitive impairment (CI) has become a growing concern worldwide and is causing increasing alarm as the incidence of CI continues to increase. It is estimated that currently nearly 50 million people are diagnosed with dementia worldwide. What’s more, the data is expected to rise to 75 million by 2030 [1]. Patients with impaired renal function are more likely to have CI, the prevalence of CI is much more higher in those requiring prevalent dialysis [2]. CI is associated with increased hospitalization and elevated cardiovascular disease risk and all-cause mortality [3]. No effective treatments for dementia are available currently, however, mild cognitive impairment (MCI), a precursory stage of dementia, is potentially recoverable and can be identified years before the onset of established dementia. Early identification of potentially modifiable risk factors and intervention at the MCI stage is therefore of great importance to facilitate prevention of MCI and dementia.
Protein-energy wasting (PEW), which is a common complication of chronic kidney disease (CKD), is highly prevalent in patients receiving maintenance hemodialysis (MHD) therapy, leading to loss of muscle strength and muscle mass. Several studies have demonstrated that poor handgrip strength (HGS), a simple and valid agent of muscle function, is associated with increased risk of CI in aged population [4]. Nevertheless, few studies have evaluated the relationship between HGS and CI in younger and MHD patients, who frequently experience CI and muscle weakness. Lean tissue mass (LTM) is an important nutritional indicator and can be used as a proxy for muscle mass. Although a few studies have reported the association between muscle mass and cognitive function, they are conflicting [5,6,7]. Moreover, the data for subgroup analysis of these relationships are lacking.
The aim of the present study was to evaluate and compare the associations of LTM measured by body composition monitor (BCM), muscle strength determined by HGS and CI risk in MHD patients. Furthermore, we conducted subgroup analyses based on gender, age and education status.
Methods
Participants
We conducted a multicenter, cross-sectional study in 20 hemodialysis centers of Guizhou Province, Southwest China. All adult MHD patients in the 20 hemodialysis centers from June 1, 2020 to September 30, 2020 were invited to take part in our study. The eligibility criteria in our study were as follows: (1) patients aged 18 or older, (2) patients who have been on regular hemodialysis for a minimum of three months, (3) agree to participate in our study. We excluded patients with visual and hearing disabilities, language barriers, mental disability and motor impairment. Patients with excessive volume load, such as those with ongoing heart failure or in critical condition, were excluded. The study was approved by the ethics committee of Guizhou Provincial People’s Hospital (GZPPHEC-2015-028) and written informed consents were obtained from the participants.
Data collection
A predesigned questionnaire was used to conduct a standardized, structured interview. We got demographic, socioeconomic information, medical history, dialysis vintage and details about lifestyle of the participants though the questionnaires. All patients were required to have regular examinations including routine blood tests, blood biochemistry, etc. monthly or once every 3 months at least. All regular examinations results came from fasting blood samples collected during the inter-dialysis period. Laboratory parameters, such as levels of pre-dialysis serum creatinine (Scr), C-reactive protein (CRP) and serum uric acid (SUA) were extracted from the medical records by physicians. Participants without laboratory parameters in the last 3 months were excluded from our final analysis.
Anthropometric measurement
Anthropometric measurements were performed by well-trained renal physicians and dialysis nurses after a routine HD session following standardized procedures. Body weight was measured with participants barefoot and in light clothing with an electronic scale. Height was acquired with participants barefoot and standing erect and measured to the nearest 1 cm. Body mass index (BMI) was calculated by the body weight in kilogram divided by the height squared in meters. LTM was measured by a trained dialysis nurse and renal physician with a portable body composition monitor (BCM, Fresenius Medical Care, Bad Homburg, Germany). The measurement was carried out approximately 30 min before the HD session according to the manufacturer’s instructions.
Handgrip strength measurement
HGS was measured twice by trained renal physicians for non-fistula hand with a handheld dynamometer (Camry Digital Hand Dynamometer, Model EH101, China) immediately before a dialysis session. The maximal grip strength was recorded. A single trial for each hand was conducted for participants with an indwelling dialysis catheter and the maximal score was used in the final analyses.
Assessment of cognitive function
Cognitive function was assessed by trained physicians and nurses using the Mini-Mental State Examination (MMSE) score, a widely used screening test for global cognitive impairment. All the physicians and nurses were centrally trained by neuropsychologists to conduct the assessments before the study was initiated. According to the recommended cutoffs [8], patients with a MMSE score less than 27 were considered to have CI.
Statistical analysis
The data were presented as median and interquartile range for continuous variables due to their skewed distribution and proportions for categorical variables.
To assess the association of grip strength, LTM and CI, participants were divided into four subgroups according to quartiles of HGS and LTM. The baseline characteristics of the different groups stratified by HGS and LTM quartiles were compared with Kruskal–Wallis tests or Chi-square tests. Multivariable logistic regression models were performed to assess the estimate odds ratios (ORs) and 95% confidence intervals (CIs) for the association of HGS, LTM with risk of CI. To evaluate the robustness of the primary results, we performed subgroup analysis to explore the potential effect modification by age, gender and education status. Education status was divided into two groups: lower education status (senior middle school and below) and higher education status (high school and above). Interaction across subgroups was tested using the likelihood ratio test.
Receiver-operating characteristic (ROC) analyses were also conducted to determine whether HGS performed better than LTM in identifying poor cognitive function in prevalent hemodialysis patients. The areas under the ROC curves (AUCs) with 95% confidence interval (CI) were calculated. The DeLong’s test was used to compare AUCs of HGS and LTM for predicting CI.
Statistical analyses were conducted using statistical packages R version 3.4.3 (The R Foundation, Vienna, Austria). The ROC analysis was performed with MedCalc version 13.0 for Windows (MedCalc Software, Mariakerke, Belgium). P values less than 0.05 (2-tailed) were considered statistically significant.
Results
Baseline characteristics
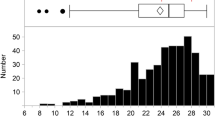
3312 participants were included in our initial study. 485 patients were excluded from our final analysis due to missing data for HGS, LTM or MMSE score. The final analysis included data obtained from 2827 adult MHD patients. The median age of our patients was 55 years (age range, 18–92 years). 58.6% participants in our study were males. Characteristics of the participants stratified by quartiles of HGS and LTM were shown in Table 1. Participants were younger, had higher levels of Scr, SUA, albumin, prealbumin and lower levels of CRP with increasing quartiles of LTM and HGS. Furthermore, participants in higher quartiles of LTM and HGS groups were more likely to be current cigarette smokers, current drinkers, had higher levels of education and MMSE score, compared to those in the lowest LTM and HGS quartile group. Participants in the lowest quartiles of LTM and HGS groups were more likely to have a history of diabetes and stroke, though no statistically significant difference among the groups stratified by LTM was noted.
Association between HGS, LTM and CI
As shown in Table 2, logistic regression analyses showed significant associations between HGS, LTM and CI. Patients in the lowest quartile of HGS was 2.82 fold as likely to have CI compared to those in the highest quartile, while participants in the lowest quartile of LTM group were 1.52 fold as likely to have CI, compared with the highest quartile group of LTM after adjusting for age, gender and education level. These associations persisted even after adjusting for potential confounders such as age, sex, education status, history of diabetes, hypertension, stroke, current smoker, current alcohol use, BMI and dialysis vintage.
Subgroup analyses
It is well known that age, gender and education status are associated with cognitive function. To further test the robustness of association between HGS, LTM and risk of CI in different subgroups, subgroup analyses were performed after adjusting for age, sex, education status, history of diabetes, hypertension, stroke, current cigarette or alcohol use. As shown in Fig. 1, the lowest quartile (Q1) group of HGS or LTM was associated with a significantly higher risk for CI compared with the highest quartile (Q4) group in all subgroups except for women and well-educated participants. There was a significant interaction between HGS and education status on CI (P for interaction = 0.0006). Age played an interactive role in the association between LTM and incident CI (P for interaction = 0.002). The association between HGS, LTM and CI was more prominent in men and less educated group.
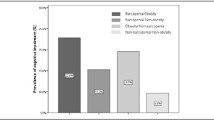
ROC analysis for identification of patients with risk of CI
ROC analysis was further performed to evaluate the diagnostic performance of HGS and LTM for identifying patients with high risk of CI. As shown in Fig. 2, both HGS and LTM were able to discriminate CI (area under the ROC curves (AUCs) > 0.6, P < 0.05). The AUC value of the HGS was 0.69 (95% CI 0.67–0.71, P < 0.001), which was significantly higher than that of LTM (AUC 0.63, 95% CI 0.61–0.65, P < 0.001). When the Youden Index reached the maximum, the optimal cut-off point of HGS was 19.5 kg, the corresponding sensitivity and specificity were 69.1% and 61.0% respectively while the cut off value of LTM was 38.55 kg with the corresponding sensitivity of 62.6% and specificity of 55.0%.
Discussion
To the best of our knowledge, this is the first study to investigate and compare the association of LTM and HGS with CI risk among Chinese MHD patients. Our study demonstrated that both low HGS and LTM were independently associated with increased CI risk in MHD patients even after adjusting for potential confounders. Moreover, our study demonstrated that the relation of HGS, LTM and risk of CI was more pronounced in less educated and male patients. There was a significant interaction between HGS and education status on CI. Age played an interactive role in the association between LTM and incident CI. Besides, the current study found that HGS was a better predictor of CI compared with LTM in MHD patients.
Though previous surveys evidenced a relationship between muscle strength or muscle mass with CI in general population, they are mainly focus on elderly patients [9]. Data supporting this relationship are still scarce in younger and MHD patients, who frequently experience CI and muscle weakness. Moreover, the reported associations between muscle mass and cognitive function are conflicting, thus definitive conclusions cannot be drawn from individual studies to date. The present study suggests that LTM is independently associated with increased risk of CI in MHD patients, even after adjustment for potential confounders. This is consistent with a previous study conducted in 7105 community-dwelling women aged 75 and older [5], but the previous study did not include males and younger participants. Another study conducted in hospitalized patients aged 70 years or older also suggested that lower cognitive functioning was associated appendicular lean mass assessed by segmental BIA [10]. However, a recent study suggested that lower DXA-assessed appendicular lean mass showed no association to cognition after adjusting for confounders in aged ≥ 60 men [7]. Another study comes to a similar conclusion that no correlation was found between lean tissue index and cognitive function in hemodialysis patients aged 65 years or older [6]. The conflicting conclusions may be attribute to differences in characteristics of study population, methods of measuring LTM, age distribution and research methods. Participants mentioned in the above studies were older, while participants were relatively younger in our study. The median age of our patients was 55 years. Our subgroup analysis showed that though age played an interactive role in the association of LTM on CI, the association persisted after adjusting for possible confounders in patients older or younger than 65 years (Fig. 1). In the study of Abdulan et al. [6], they just evaluated the linear relation between lean tissue mass index with CI and obtained a negative result, thus the nonlinear relationships between LTM and CI might be ignored. Previous studies have suggested that there is large inter-individual variation between bedside BIA and DXA [11]. LTM estimated by DXA may be confounded by intramuscular fat [12]. Conventional BIA is reported to overestimate lean body mass in overhydrated subjects [13]. In our study, LTM was measured by BCM, a portable whole body multifrequency bioimpedance spectroscopy device, which has been widely used and accepted as an ideal tool for assessing body composition and nutritional status in dialysis patients as it is not affected by overhydration [14, 15]. Thus, LTM assessed by different methods might come to different conclusions.
Exact mechanisms accounting for the association between low HGS, LTM and poor cognitive function are unknown. The presence of shared pathogenesis like chronic inflammation, malnutrition, insulin insensitivity, physical inactivity, high oxidative stress, which may contribute to strength or muscle loss and cognitive decline may be responsible [16,17,18,19]. Nutritional markers such as levels of albumin, prealbumin, Scr, SUA were significantly lower, while inflammatory biomarker CRP levels and the proportion of patients with a history of diabetes or stroke was significantly higher in patients with the lowest HGS or LTM (quartile 1) than those in quartile 4 who were less likely to have CI, suggesting that low LTM, HGS and CI might share common pathological pathways.
Subgroup analyses in our study showed that the associations between the lowest quartile of HGS, LTM and increased risk for CI were particularly prominent in men and less educated patients. This finding suggests that utility of HGS and LTM as predictors of CI may be more valid in these subpopulations. A previous study has come to a similar conclusion that association between low HGS and CI was stronger in men [20]. Sex differences regarding inflammatory load and oxidative stress may to some extent contribute to the sex-dependent associations between low HGS, LTM and CI. Some inflammatory factors and biomarkers of oxidative stress are significantly higher in men than in women [21], as mentioned above, both chronic inflammation and high oxidative stress contribute to strength or muscle loss and cognitive decline, which could explain the gender-independent effect observed in our study. Another possible explanation might attribute to the smaller sample size on the subgroup analysis. As shown in Table 1, most participants in the highest quartile of LTM/HGS were male (above 90%). Further studies with a larger sample size, especially for subgroup analysis stratified by sex are needed to investigate this association. Previous studies have proposed that greater school year length was associated with better cognitive function [22]. Education may influence life style, socioeconomic condition and access to healthcare [23], which in turn result in balanced nutrition, regular exercise and physical and mental health. This may to some extent responsible for the insignificant relation between HGS, LTM and CI in well-educated patients.
We found that HGS had a stronger association with CI and a greater ROC AUC, indicating that HGS is a better marker for identification of CI compared with LTM in MHD patients. This is in accordance with the view of the revised European definition of sarcopenia, which suggest that muscle strength is a better predictor of negative health outcomes compared with muscle mass [24]. Isoyama et al. have also demonstrated that low muscle strength is more strongly associated with aging, physical inactivity, inflammation, and mortality than low muscle mass in dialysis patients [25]. Previous studies have demonstrated that muscle strength declines more rapidly than muscle mass with aging. Muscle mass does not fully explain variability in muscle strength [26], moreover, maintaining muscle mass does not prevent aging-related declines in muscle strength, highlighting the importance of muscle strength.
The strengths of the current study were the relatively large sample size, multicenter representation, diversity in sex and the subgroup analyses. However, several limitations of the current study should be considered. First, the cross-sectional nature of our study disenabled us to make causal inferences. Second, though many potential confounding variables have been assessed in our study, physical activity was not adjusted as it could have affected the association between HGS, LTM and CI. Third, LTM was measured using the BCM. Though imaging technology such as magnetic resonance imaging and computed tomography are the most valid and reliable clinical methods for measuring muscle mass, however, they are costly and bulky. BCM has been widely accepted to assess body composition in hemodialysis patients. There are so many studies that evaluate LTM with BCM in dialysis patients [15, 27]. It is reported that its measurement is not affected by overhydration [28]. Furthermore, in comparison with DXA, muscle mass measured by bioimpedance was reasonably accurate in ESRD patients [29]. Moreover, BIA has been accepted by the European Group on Sarcopenia in Older People as an option for muscle mass assessment [24]. In addition, patients with excessive volume load, such as those with ongoing heart failure or in critical condition had excluded from our study. Fourth, cognitive function was assessed with the MMSE. Though MMSE has several limitations such as having limited sensitivity in detecting early CI, influenced by age, education level, it is the most widely used tool for screening of CI worldwide [30] and we had conducted subgroup analyses based on age, sex, and educational status. The associations were nearly similar across different subgroups.
Conclusions
Both low HGS and LTM were associated with increased CI risk in MHD patients and the associations were more pronounced in males and less educated participants. Muscle strength performed better than muscle mass in identifying individuals at high risk of CI, particularly in male and less educated Chinese MHD patients. Our results support an emphasis on objective measures of grip strength in assessment of risk for CI in MHD patients.
References
Alacreu M, Pardo J, Azorín M, Climent MT, Gasull V et al (2019) Importance of increasing modifiable risk factors knowledge on Alzheimer’s disease among community pharmacists and general practitioners in Spain. Front Pharmacol 10:860. https://doi.org/10.3389/fphar.2019.00860 (eCollection 2019)
Wang C, Lu H, Yang C, Luo Y (2014) Progress on the M-type phospholipase A2 receptor in idiopathic membranous nephropathy. Chin Med J (Engl) 127(10):1960–1963
An J, Li H, Tang Z, Zheng D, Guo J et al (2018) Cognitive impairment and risk of all-cause and cardiovascular disease mortality over 20-year follow-up: results from the BLSA. J Am Heart Assoc 7(15):e008252
McGrath R, Vincent BM, Hackney KJ, Robinson-Lane SG, Downer B et al (2020) The longitudinal associations of handgrip strength and cognitive function in aging Americans. J Am Med Direct Assoc 21(5):634–639. https://doi.org/10.1016/j.jamda.2019.08.032 (e631)
Nourhashémi F, Andrieu S, Gillette-Guyonnet S, Reynish E, Albarède JL et al (2002) Is there a relationship between fat-free soft tissue mass and low cognitive function? Results from a study of 7,105 women. J Am Geriatr Soc 50(11):1796–1801. https://doi.org/10.1046/j.1532-5415
Abdulan IM, Onofriescu M, Stefaniu R, Mastaleru A, Mocanu V et al (2019) The predictive value of malnutrition for functional and cognitive status in elderly hemodialysis patients. Int Urol Nephrol 51(1):155–162. https://doi.org/10.1007/s11255-018-2000-0 (Epub 2018 Dec 4)
Sui SX, Holloway-Kew KL, Hyde NK, Williams LJ, Leach S et al (2020) Muscle strength and gait speed rather than lean mass are better indicators for poor cognitive function in older men. Sci Rep 10(1):1–9. https://doi.org/10.1038/s41598-020-67251-8
Zhong C, Bu X, Xu T, Guo L, Wang X et al (2018) Serum matrix metalloproteinase-9 and cognitive impairment after acute ischemic stroke. J Am Heart Assoc 7(1):e007776. https://doi.org/10.1161/JAHA.117.007776
Chou M, Nishita Y, Nakagawa T, Tange C, Tomida M et al (2019) Role of gait speed and grip strength in predicting 10-year cognitive decline among community-dwelling older people. BMC Geriatr 19(1):186. https://doi.org/10.1186/s12877-019-1199-7
Van Dam R, Van Ancum JM, Verlaan S, Scheerman K, Meskers CG et al (2018) Lower cognitive function in older patients with lower muscle strength and muscle mass. Dement Geriatr Cogn Disord 45:243–250. https://doi.org/10.1159/000486711
van Venrooij LM, Verberne HJ, de Vos R, Borgmeijer-Hoelen MM, van Leeuwen PA et al (2010) Preoperative and postoperative agreement in fat free mass (FFM) between bioelectrical impedance spectroscopy (BIS) and dual-energy X-ray absorptiometry (DXA) in patients undergoing cardiac surgery. Clin Nutr 29(6):789–794
Osawa Y, Chiles Shaffer N, Shardell MD, Studenski SA, Ferrucci L (2019) Changes in knee extension peak torque and body composition and their relationship with change in gait speed. J Cachexia Sarcopenia Muscle 10(5):1000–1008. https://doi.org/10.1002/jcsm.12458
Buckinx F, Landi F, Cesari M, Fielding RA, Visser M et al (2018) Pitfalls in the measurement of muscle mass: a need for a reference standard. J Cachexia Sarcopenia Muscle 9(2):269–278. https://doi.org/10.1002/jcsm.12268
Lin TY, Wu MY, Chen HS, Hung SC, Lim PS (2021) Development and validation of a multifrequency bioimpedance spectroscopy equation to predict appendicular skeletal muscle mass in hemodialysis patients. Clin Nutr 40(5):3288–3295. https://doi.org/10.1016/j.clnu.2020.10.056
Kim C, Kim JK, Lee HS, Kim SG, Song YR (2021) Longitudinal changes in body composition are associated with all-cause mortality in patients on peritoneal dialysis. Clin Nutr 40(1):120–126. https://doi.org/10.1016/j.clnu.2020.04.034
Zheng K, Wang H, Hou B, You H, Yuan J et al (2017) Malnutrition-inflammation is a risk factor for cerebral small vessel diseases and cognitive decline in peritoneal dialysis patients: a cross-sectional observational study. BMC Nephrol 18(1):1–10. https://doi.org/10.1186/s12882-017-0777-1
Souweine J-S, Kuster N, Chenine L, Rodriguez A, Patrier L et al (2018) Physical inactivity and protein energy wasting play independent roles in muscle weakness in maintenance haemodialysis patients. PLoS One 13(8):e0200061. https://doi.org/10.1371/journal.pone.0200061
Nakakubo S, Makizako H, Doi T, Tsutsumimoto K, Lee S et al (2017) Impact of poor sleep quality and physical inactivity on cognitive function in community-dwelling older adults. Geriatr Gerontol Int 17(11):1823–1828. https://doi.org/10.1111/ggi.12973
Beetham KS, Howden EJ, Small DM, Briskey DR, Rossi M et al (2015) Oxidative stress contributes to muscle atrophy in chronic kidney disease patients. Redox Rep 20(3):126–132. https://doi.org/10.1179/1351000214Y.0000000114 (Epub 2014 Nov 13)
Liu X, Chen J, Geng R, Wei R, Xu P et al (2020) Sex-and age-specific mild cognitive impairment is associated with low hand grip strength in an older Chinese cohort. J Int Med Res 48(6):0300060520933051. https://doi.org/10.1177/0300060520933051
Watarai R, Suzuki K, Ichino N, Osakabe K, Sugimoto K et al (2014) Association between serum levels of carotenoids and serum asymmetric dimethylarginine levels in Japanese subjects. J Epidemiol 24(3):250–257
Crowe M, Clay OJ, Martin RC, Howard VJ, Wadley VG et al (2013) Indicators of childhood quality of education in relation to cognitive function in older adulthood. J Gerontol Ser A 68(2):198–204. https://doi.org/10.1093/gerona/gls122
Seblova D, Berggren R, Lövdén M (2020) Education and age-related decline in cognitive performance: systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev 58:101005. https://doi.org/10.1016/j.arr.2019.101005
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48(1):16–31. https://doi.org/10.1093/ageing/afy169
Isoyama N, Qureshi AR, Avesani CM, Lindholm B, Bàràny P et al (2014) Comparative associations of muscle mass and muscle strength with mortality in dialysis patients. Clin J Am Soc Nephrol 9(10):1720–1728. https://doi.org/10.2215/CJN.10261013
Lengelé L, Moehlinger P, Bruyère O, Locquet M, Reginster J-Y et al (2020) Association between changes in nutrient intake and changes in muscle strength and physical performance in the SarcoPhAge cohort. Nutrients 12(11):3485. https://doi.org/10.3390/nu12113485
Parthasarathy R, Oei E, Fan S (2019) Clinical value of body composition monitor to evaluate lean and fat tissue mass in peritoneal dialysis. Eur J Clin Nutr 73(11):1520–1528. https://doi.org/10.1038/s41430-019-0391-3
Lin T, Wu M, Chen H, Hung S, Lim P (2021) Development and validation of a multifrequency bioimpedance spectroscopy equation to predict appendicular skeletal muscle mass in hemodialysis patients. Clin Nutr (Edinburgh, Scotland) 40(5):3288–3295. https://doi.org/10.1016/j.clnu.2020.10.056
Popovic V, Zerahn B, Heaf J (2017) Comparison of dual energy X-ray absorptiometry and bioimpedance in assessing body composition and nutrition in peritoneal dialysis patients. J Renal Nutr 27(5):355–363. https://doi.org/10.1053/j.jrn.2017.03.003
Devenney E, Hodges JR (2017) The mini-mental state examination: pitfalls and limitations. Pract Neurol 17(1):79–80. https://doi.org/10.1136/practneurol-2016-001520
Acknowledgements
The Special Fund for Basic Scientific Research Operating of Central Public Welfare Research Institutes, the Chinese Academy of Medical Sciences (2019PT320003) supported our study (Grant QKHPTRC[2020]2201).
Author information
Authors and Affiliations
Contributions
CMZ, LZ and LS contributed to the design, analysis, and interpretation of the data and drafted the manuscript; YZ provided guidance in the writing of this paper; JY, HPH contributed to the acquisition of the data.
Corresponding author
Ethics declarations
Conflict of interest
We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Ethical statement
Ethics Committee of The People’s Hospital of Guizhou province approved the study.
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zha, Y., Zhou, C., Liao, S. et al. Muscle strength performed better than muscle mass in identifying cognitive impairment risk in maintenance hemodialysis patients. Eat Weight Disord 27, 2533–2540 (2022). https://doi.org/10.1007/s40519-022-01375-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-022-01375-w