Abstract
Introduction
The Multidimensional Weight Locus of Control Scale (MWLCS) measures a individuals’ focus on body weight or their beliefs about a lack of locus of control.
Purpose
This study was carried out to determine the validity and reliability of the Turkish culture-adapted version of the Multidimensional Weight Locus of Control Scale in adults, which was originally developed by Cebolla et al.
Methods
The sample of the study consists of 700 individuals between the ages of 19–64 who voluntarily agree to participate in online survey. Validity and reliability analyses were performed for the Turkish version Multidimensional Weight Locus of Control Scale. Confirmatory factor analysis (CFA) was performed to evaluate the factor structure of the Turkish version Multidimensional Weight Locus of Control Scale. In addition, reliability analyses and Pearson correlations were also examined.
Results
Individuals were divided into two groups as those with normal (18.50–24.99 kg/m2; n = 432) and those with overweight–obese body mass index (≥ 25.0 kg/m2; n = 268) and measurement invariance tested in both the groups. The four-factor structure (internal, chance, doctors, and other people) describing the weight locus of control was supported by confirmatory factor analyses. The sub-factors of the Turkish version Multidimensional Weight Locus of Control Scale were positively associated with the sub-factors of Dutch Eating Behaviour Questionnaire (DEBQ). In addition, the scale showed configural invariance in different body mass index groups.
Conclusions
Findings from this study revealed that Turkish version Multidimensional Weight Locus of Control Scale is a valid and reliable measurement tool that can be applied in Turkish culture. It is thought that this scale will contribute to studies that will evaluate the focus of individuals in different body mass index groups related to weight control.
Level of evidence
Level V, descriptive study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity rates are increasing rapidly all over the world. Parallel to this, obesity-related health problems and the increase in health expenditures have led to intensification of research on factors affecting obesity [1]. It is recommended that obese individuals lose weight to improve their health conditions and increase their quality of life [2]. A 5% reduction in body weight improves health outcomes and a standard goal in weight loss programs [3]. Weight loss can be achieved with methods such as diet, physical activity, behavioral and pharmacological treatment [4]. Successful weight loss is observed in individuals with behavioral therapy aimed at increasing physical activity and/or reducing energy intake, but most individuals can regain weight months or years after the end of such programs, and some even return to their previous body weight [5]. To increase the effectiveness of weight loss programs, variables such as individuals’ weight loss goals, preferred treatment method, attitude, motivation level, and locus of control (LOC) should not be ignored [6]. For this reason, when planning weight loss programs, it is necessary to establish a correct relationship between individuals’ LOC and their tendency to maintain a healthy lifestyle [7].
LOC is defined as a person’s belief in a state of control regarding certain events in her/his life. It is an important concept in obesity and weight management as it indicates whether an individual believes their environment and choices are under their control [1]. If the individual believes that he/she can control certain events or results due to his/her own behaviors or personal characteristics that he/she maintains consistently, this situation is called “internal” LOC. If the individual has the belief that events or results are controlled by external forces, independent of her/his will, this is called an “external” LOC [8]. Internal LOC is an important variable in weight control as it is associated with high adherence to weight loss programs and less weight gain after the program ends, preferring healthy behaviors and healthy habits [9,10,11]. External LOC is associated with having a negative view of external situations such as physical activity or social support in relation to body weight gain [12]. An example of this is that individuals with an external LOC perceive their health status as bad, have difficulty in adapting to weight loss programs and performing physical activity [1, 10]. It is stated that individuals with an external locus are more prone to depression and anxiety and are more likely to give up instead of resisting difficult situations. These individuals have higher cortisol levels and stress levels. This situation causes individuals to tend to consume more nutrients and may adversely affect their long-term health status [13]. Another perspective on the importance of LOC on body weight is that individuals with external LOC may benefit more from the help of health care providers such as dietitians [14]. However, the fact that individuals with an internal LOC have more positive emotions compared to those with an external LOC enable them to be more successful in weight loss interventions [9, 12, 15].
The first scale specifically developed to measure LOC associated with weight loss was the Weight Locus of Control Scale (WLOCS) [16]. Laters, the researchers developed the Dieting Beliefs Scale but this scale was only validated in a sample of women with normal body weight [17]. Another scale related to LOC is the Multidimensional Health Locus of Control Scale (MHLCS). This scale has two forms, A and B. High internal LOC reflects personal responsibility for health status, while chance and powerful others express external LOC [18]. The need for the assessment of individuals with different health-related conditions has led researchers to develop the C form of the MHLCS. This scale was administered to a sample of rheumatoid arthritis, chronic pain, diabetes, and cancer patients and was found to have acceptable internal consistency with a 4-factor structure (internal, chance, doctors, and other people) [19]. The MHLCS was not used to specifically assess weight LOC. Since internal obstacles such as lack of willpower, inadequacy in emotion regulation skills and negative thoughts or external obstacles such as difficulty in preparing food and obesogenic environment have led to different orientations that can affect the weight LOC in individuals [20]. Therefore, the MWLCS was adapted in a sample of Spanish individuals with different body mass indexes using the C form of the MHLCS [7]. In this study, it was aimed to adapt the MWLCS to Turkish culture in a sample of adults with and without normal body mass index.
Materials and methods
Adaptation protocol
To adapt the scale into Turkish, permission for the use and translation of the scale was obtained from Cebolla A. [7], one of the creators of the scale, via e-mail. To adapt the MWLCS to Turkish, first, the original form of the 18-item scale was translated into Turkish. The standard translation-back-translation method was used in the translation process of this questionnaire [21]. The consistency and semantic integrity of the translated forms were evaluated by experts in the field of Nutrition and Dietetics, and the adaptation process of the scale was finalized after necessary corrections were made. In addition, a pilot study was conducted on 30 people to determine the intelligibility of the items in the scale. Data collected in the pilot study were not included in the analyses of this study.
Participants
The sample of this study consists of 700 adult individuals, aged 19–64 years, living in Turkey and volunteering to participate in the study. In adapting a scale to a different language and culture, the recommended sample size to determine its validity and reliability should be at least 5–10 times the number of the items in the scale [22]. Data were collected between February and April 2021 with an online questionnaire using snowball sampling method to reach as many individuals as possible. 24 individuals with a BMI below 18.50 kg/m2 were not included in the study.
Measures
Questionnaire form
The first section of the questionnaire collected information about the demographic characteristics of the individuals such as age, gender, and body mass index (BMI). Height (cm) and body weight (kg) information were obtained based on the statements of individuals. Body mass index was calculated as body weight divided by height squared (kg/m2).
Multidimensional Weight Locus of Control Scale (MWLCS)
It is a scale specially adapted to measure weight LOC by Cebolla et al. [7]. It measures individuals’ beliefs about how they control their body weight. In this study, the 18-item Turkish adapted version of MWLCS, which composed of four factors (internal, chance, doctors, and other people) was used. The scale is scored as a 6-point Likert and there is no reverse coded item. In the study conducted by Cebolla et al. [7], the Cronbach alpha value calculated for the scale was specified as 0.72 for internal, 0.82 for chance, and 0.65 for powerful others. In this study, Cronbach’s alpha values calculated for the sub-factors of the T-MWLCS scale were found to be 0.72 for internal, 0.86 for chance, 0.66 for doctors, and 0.69 for people.
Dutch Eating Behaviour Questionnaire (DEBQ)
It is a scale developed to measure eating behaviors that may contribute to or weaken the overweight situation in individuals [23]. In this study, the Turkish version of DEBQ was used [24]. The scale consists of 33 items and 3 sub-factors (emotional eating, restrained eating, and external eating). It is scored on a 5-point Likert scale. Items 1–10 of the scale measure external, items 11–23 emotional, and items 24–33 measure restrained eating behavior. This scale Cronbach’s alpha value was specified as 0.97 for the emotional eating, 0.91 for the restrained eating, and 0.90 for the external eating. Within the scope of this study, the Cronbach alpha value calculated for the DEBQ scale was 0.96 for emotional eating, 0.90 for restrained eating and 0.82 for external eating.
Statistical analysis
For the analysis of the data obtained from the study, the Mplus 8.1 program was used as it was used in the original study. CFA was performed to examine the verification of both the three-dimensional structure of the scale found by Cebolla et al. [7] and the four-dimensional structure in its original form. Indicators of fit such as Chi-square (χ2) Goodness of Fit Index, Comparative Fit Index (CFI), Tucker Lewis Index (TLI) and Root Mean Squared Error of Approximation (RMSEA) were calculated. Cronbach’s alpha coefficient and McDonald’s Omega (ω) were calculated for the internal consistency estimates between the items in the scale [25]. Individuals were divided into two groups as normal BMI (18.50–24.99 kg/m2) and overweight–obese BMI (≥ 25.0 kg/m2). The use of the scale in different BMI groups was evaluated with measurement invariance. In addition, the correlation between T-MWLCS factors and age, BMI and DEBQ factors was examined with Pearson’s correlation. Before correlation analyses, skewness values were examined to evaluate the normal distribution for scale scores, age and BMI measurements. It was determined that the values varied between − 0.919 and 1.172. Considering the sample size (n = 700), it was determined that the skewness values did not deviate much from − 1 to + 1. Significance level was accepted as p < 0.05 in all the analyses.
Results
A total of 700 adult individuals between the ages of 19 and 64 participated in the study, 31.4% male and 68.6% female. The mean age of individuals is 30.01 ± 11.86 years and the mean BMI is 24.41 ± 4.49 kg/m2. It was determined that 61.7% of the individuals had normal BMI and 38.3% had a overweight–obese BMI.
Kaiser–Meier–Olkin (KMO) test was employed to test whether the sample size was adequate, and Bartlett’s Sphericity Test was used to determine whether there was a correlation between the items, which is a prerequisite for factor analysis. Accordingly, the results of the KMO test statistics showed that the sample size was adequate (KMO = 0.874). A KMO value of > 0.50 indicates that the sample size of the related scale data is sufficient. According to the Bartlett Sphericity Test result, the level of correlation between the items was found to be sufficient to do a factor analysis (χ2 = 4400.668; p < 0.0001).
The factor loading values and fit index values obtained as a result of the CFA of the four-factor structure of the T-MWLCS are given in Table 1. The items grouped under factor 1 were items 1, 6, 8, 12 and 17; those under factor 2 were items 2, 4, 9, 11, 15 and 16; those under factor 3 were items 3, 5, 13 and 14 and; those gathered under factor 4 were items 7, 10 and 18.
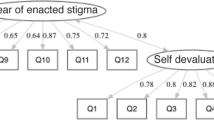
When Table 1 is examined, it is seen that factor loads are greater than 0.30. Therefore, it can be said that the items meet the sub-factor they are in. Cronbach’s alpha coefficient was 0.72 and McDonald’s omega coefficient was 0.72 for the “internal” 0.86 and 0.87 for the “chance”, 0.66 and 0.69 for the “doctors”, and 0.69 and 0.69 for the “other people” sub-factor. For reliability measurements, values below 0.50 are considered low reliability, values between 0.50 and 0.80 are considered moderately reliable, and values above 0.80 are considered high reliable [26]. Accordingly, it can be said that the reliability of the scores obtained from the chance sub-factor is high, and the reliability of the scores obtained from the internal, doctors and other people sub-factor is moderate. In addition, the fit index values obtained as a result of CFA were examined to evaluate the model data fit. The\({\chi }^{2}\)/sd value was determined to be 2.83, and since this value was less than 3, it was determined that the model fitted the data well. In addition, the CFI value was 0.91 and the TLI value was 0.90. If these values are above 0.90, it means that the model fits the data very well. When evaluated in terms of RMSEA, it was determined that this index was 0.051 for the model and it can be said that the model is compatible with the data according to this index. When the fit indices are evaluated in general, it is seen that the four-factor model fits the data. In other words, it can be said that the four-factor structure of the MWLCS is similarly provided in Turkish culture, as it was thought in the original form of the scale. The measurement model obtained by CFA of the four-factor structure is given in Fig. 1.
The fit scheme of T-MWLCS scale with CFA and the four-factor model. f1 (factor 1): Internal, f2 (factor 2): Chance, f3 (factor 3): Doctors, f4 (factor 4): Other people. #Standardised factor loadings: internal items; .515 for MWLCS1, .449 for MWLCS6, .552 for MWLCS8, .669 for MWLCS12, .572 for MWLCS17; chance items; .500 for MWLCS2, .706 for MWLCS4, .775 for MWLCS9, .786 for MWLCS11, .800 for MWLCS15, .767 for MWLCS16; doctors items; .625 for MWLCS3, .712 for MWLCS5, .329 for MWLCS13, .738 for MWLCS14; other people items; .626 for MWLCS7, .728 for MWLCS10, .594 for MWLCS18.
The invariance of the scale items was tested according to these two groups (BMI 18.50–24.99 kg/m2; ≥ 25.0 kg/m2). For this purpose, configural, metric, scalar and strict invariance levels were examined. The results are in Table 2.
When Table 2 is examined, it is seen that the \({\chi }^{2}\)/sd (715.529/256) value is 2.80 and the RMSEA value is 0.072, and the model data fit is achieved. Accordingly, it was determined that configural invariance was supported according to BMI. When the configural invariance and metric invariance were compared in the normal and overweight–obese BMI groups in T-MWLCS, it was determined that \({\Delta \chi }^{2}\)(14) = 37.068 (p = 0.001), so it can be that metric invariance was not achieved. Scalar invariance was not supported in T-MWLCS since \({\Delta \chi }^{2}\)(14) = 69.886 (p = 0.00) when scalar invariance was compared with metric invariance. When the strict invariance and scalar invariance are compared, it is determined that there is no strict invariance since \({\Delta \chi }^{2}\)(14) = 423.155 (p = 0.000). Consequently, it was determined that while configural invariance was provided in T-MWLCS for normal and overweight–obese BMI groups determined according to BMI, metric, scalar and strict invariance were not provided.
Relationships between T-MWLCS sub-factors and age, BMI and DEBQ were calculated by Pearson correlation. The results are in Table 3.
When Table 3 is examined, it was observed that there was a low-level positive statistically significant relationship between age and the doctors sub-factors (r = 0.106; p < 0.05), while there was no statistically significant relationship between age and other sub-factors of the T-MWLCS (p > 0.05). A low-level positive statistically significant correlation was found between BMI and the internal, chance and doctors sub-factors T-MWLCS (r = 0.109; 0.112; 0.139; p < 0.05, respectively). No statistically significant correlation was found between BMI and other people sub-factor scores of MWLCS (p > 0.05). A low level of positive statistically significant correlations were found between DEBQ sub-factors and T-MWLCS sub-factors (p < 0.05). Accordingly, as the participants’ scores on the DEBQ sub-factors increase, the scores on the MWLCS sub-factors also increase.
Discussion
This study was conducted to adapt the MWLCS to Turkish in individuals with different BMIs. CFA results supported a four-factor structure internal, chance, doctors and other people, as in the C form of MHLCS, from which the MWLCS was adapted. In the C form of the MHLCS, the powerful others factor splits into doctors and other people [19]. This means that the implications for general health status differ between medically trained personnel and other people. The study of the MWLCS in a sample of Spanish individuals supported the three-factor structure internal, chance, and powerful others [7]. When the factor structure was examined in the MWLCS, it was stated that the factor loads of the fifth (I am directly responsible for the increase or decrease of my weight) and seventh (If my weight increases it is my own fault) items were low, therefore, the reliability of the powerful others sub-factor was limited [7]. In addition, this sub-factor is stated as the it is also stated that this sub-factor better supports BMI and the sub-factors of DEBQ. Cebolla et al. [7] suggested that the items that make up the scale should also be examined to better understand whether the weak loads in these items can be generalized to other populations. Therefore, both three- and four-factor structures were evaluated in our study.
In the three-factor analysis, since the factor load of the third item (If I visit health professionals regularly, I am less likely to have problems with my body weight) was low, the scores obtained from the chance sub-factor were found to be high reliable. It can be said that the scores obtained from the internal and powerful others factor are moderately reliable. Since the χ2/sd value was 4.38 in the three-factor structure, it was determined that the model had a moderate fit to the data. The CFI value is 0.84 and the TLI value is 0.81. Since the values were below 0.90, the model data fit could not be achieved in a three-factor structure. In the four-factor structure, the χ2/sd value was found to be 2.83, and since the value is less than 3, the model fits well with the data. The CFI value was 0.91 and the TLI value was 0.90. Since these values are above 0.90, the model fits the data very well. The RMSEA index was determined as 0.051, and according to this index, it can be said that the model is compatible with the data. When the fit indices are examined in general, it has been determined that the model in the four-factor structure fits the data, so it would be more appropriate to evaluate the four-factor structure in Turkish culture. This supports the MHLCS C form [20] to which the MWLCS is adapted.
When scales are applied in different countries, measurement invariance is examined to eliminate linguistic differences or to ensure that measurements obtained from different groups have equal/equivalent psychometric properties. In other words, measurement invariance is an important condition for the meaningfulness of the comparison in intergroup comparisons [27, 28]. As in the original study, measurement invariance was examined in this study to evaluate whether there was measurement bias when groups with different BMI were compared. The measurement invariance of the MWLCS was first performed by Cebolla et al. [7], and it was found that there was no measurement bias in the comparison of individuals with different BMIs in the scale. In addition, the scale showed scalar invariance. In our study, it was observed that configural invariance was achieved according to BMI. In other words, it can be said that the scale is suitable for individuals with different BMIs.
Age is one of the factors affecting the body weight of individuals. Considering that the elderly and individuals with high BMI may have received more help from health professionals, it can be thought that their attitudes towards body weight may be affected by health professionals [29]. In this study, a low-level positive correlation was found between age and the doctors’ sub-factor of T-MWLCS. From the point of view of health workers, it has been reported that the obesity problem is caused by the imbalance between energy intake and expenditure and the lack of willpower of individuals [30]. In a study, it was stated that personality traits are associated with body weight gain and weight maintenance, and success is higher in individuals with internal LOC. While individuals with internal LOC try to control their own weight, individuals with external LOC tend to lose weight by getting expert support [10].
Individuals with a high internal LOC think that their own behavior can have an impact on their health. This point of view leads them to take the necessary measures to lose weight on their own or not to regain the lost weight. On the contrary, individuals with high body weight who regain weight have an external LOC and believe that external factors affect their weight. Therefore, they want to get support from a health professional. In a study, LOC was evaluated in a weight loss program in obese and healthy individuals. It was determined that individuals with obese BMI had a higher external LOC compared to healthy ones [15]. In this study, the low level of positive correlation between BMI and both internal LOC and external LOC such as chance and doctors supports the literature. In other words, successful body weight loss may depend on both internal and external LOC. Those who follow a weight loss-related nutrition program should be internal LOC enough to believe that they can control their own body weight, but external LOC enough to comply with the recommendations of health professionals [15].
Besides, internal LOC and restrained eating behaviors are related to each other. While emotional eating is an increase in the tendency towards food intake in response to stress or negative emotional states [31], restrained eating refers to the deliberate restriction of food intake to control food intake on one’s own will or to maintain body weight control [32]. In a study, it was determined that the “powerful others” factor of MWLCS was positively related to BMI and the restrained eating factor of DEBQ [7]. In this study, sub-factors of MWLCS and sub-factors of DEBQ were positively related. Eating behavior interacts with physiological, psychological and social factors that affect food preferences and the amount of food intake [33]. Therefore, the tendency to consume food in response to negative emotions or based on the presence of environmental food cues may be related to individuals' LOC regarding their body weight. There are some limitations of the study. Test–retest analysis was not conducted. The use of self-reported measurements when evaluating BMI is another limitation of this study. In addition, it is recommended to evaluate the LOC in more detail in a larger sample including overweight and obese individuals.
What is already known on this subject?
The MWLCS is a scale adapted from the C form of the MHLCS consisting of four factors to assess body weight LOC. The scale has been validated in Spanish only and there is currently no Turkish version of this scale.
What does this study add?
This study shows that the Turkish version of the MWLCS is a valid and reliable tool to measure weight LOC in the adult population of Turkey. As far as we know, this is the first study in which weight LOC was evaluated in a sample of Turkish individuals with different body mass indexes. T-MWLCS also correlated with sub-factors of DEBQ.
Conclusion
The results obtained from a sample using the Turkish version of the MWLCS revealed that the weight LOC consists of a four-factor structure and is a multidimensional and valid LOC criterion. It has been determined that the scale shows configural invariance in individuals with different BMIs, so it seems appropriate to use it different BMI group. It can be a useful tool in the evaluation of individuals' body weight attitudes and locus of control to increase the effectiveness of weight loss interventions. In future studies, it is recommended to expand both age and BMI groups and to include not only BMI but also variables related to body composition of individuals. Adding a scale to evaluate the quality of life will bring a different perspective to the study.
References
Neymotin F, Nemzer LR (2014) Locus of control and obesity. Front Endocrinol (Lausanne) 5:159. https://doi.org/10.3389/fendo.2014.00159
Montesi L, El Ghoch M, Brodosi L, Calugi S, Marchesini G, Dalle Grave R (2016) Long-term weight loss maintenance for obesity: a multidisciplinary approach. Diabetes Metab Syndr Obes 9:37–46. https://doi.org/10.2147/DMSO.S89836
Varkevisser RDM, van Stralen MM, Kroeze W, Ket JCF, Steenhuis IHM (2019) Determinants of weight loss maintenance: a systematic review. Obes Rev 20(2):171–211. https://doi.org/10.1111/obr.12772
Alamuddin N, Wadden TA (2016) Behavioral treatment of the patient with obesity. Endocrinol Metab Clin North Am 45(3):565–580. https://doi.org/10.1016/j.ecl.2016.04.008
Lowe MR (2015) Dieting: proxy or cause of future weight gain? Obes Rev 16(1):19–24. https://doi.org/10.1111/obr.12252
Elfhag K, Rössner S (2005) Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 6(1):67–85. https://doi.org/10.1111/j.1467-789X.2005.00170.x
Cebolla A, Botella C, Galiana L, Fernández-Aranda F, Toledo E, Corella D et al (2020) Psychometric properties of the Weight Locus of Control Scale (MWLCS): study with Spanish individuals of different anthropometric nutritional status. Eat Weight Disord 25(6):1533–1542. https://doi.org/10.1007/s40519-019-00788-4
Rotter JB (1966) Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr Gen Appl 80(1):1–28. https://doi.org/10.1037/h0092976
Ross MW, Kalucy RS, Morton JE (1983) Locus of control in obesity: predictors of success in a jaw-wiring programme. Br J Med Psychol 56:49–56. https://doi.org/10.1111/j.2044-8341.1983.tb01531.x
Anastasiou CA, Fappa E, Karfopoulou E, Gkza A, Yannakoulia M (2015) Weight loss maintenance in relation to locus of control: The MedWeight study. Behav Res Ther 71:40–44. https://doi.org/10.1016/j.brat.2015.05.010
Steptoe A, Wardle J (2001) Locus of control and health behaviour revisited: a multivariate analysis of young adults from 18 countries. Br J Psychol 92:659–672. https://doi.org/10.1348/000712601162400
Holt CL, Clark EM, Kreuter MW (2001) Weight locus of control and weight-related attitudes and behaviors in an overweight population. Addict Behav 26(3):329–340. https://doi.org/10.1016/s0306-4603(00)00108-8
Gale CR, Batty GD, Deary IJ (2008) Locus of control at age 10 years and health outcomes and behaviors at age 30 years: the 1970 British Cohort Study. Psychosom Med 70(4):397–403. https://doi.org/10.1097/PSY.0b013e31816a719e
Stone O, Werner P (2012) Israeli dietitians’ Professional stigma attached to obese patients. Qual Health Res 6:768–776. https://doi.org/10.1177/1049732311431942
Adolfsson B, Andersson I, Elofsson S, Rossner S, Unden A (2005) Locus of control and weight reduction. Patient Educ Couns 56:55–61. https://doi.org/10.1016/j.pec.2003.12.005
Saltzer EB (1982) The Weight Locus of Control (WLOC) scale: a specific measure for obesity research. J Pers Assess 46(6):620–628. https://doi.org/10.1207/s15327752jpa4606_11
Stotland S, Zuroff DC (1990) A new measure of weight locus of control: the Dieting Beliefs Scale. J Pers Assess 54(1–2):191–203. https://doi.org/10.1080/00223891.1990.9673986
Wallston KA, Strudler Wallston B, DeVellis R (1978) Development of the multidimensional health locus of control (MHLC) scales. Health Educ Behav 6:160–170. https://doi.org/10.1177/109019817800600107
Wallston KA, Stein MJ, Smith CA (1994) Form C of the MHLC scales: a condition-specific measure of locus of control. J Personal Assess 63:534–553. https://doi.org/10.1207/s15327752jpa6303_10
Carrière K, Khoury B, Günak MM, Knäuper B (2018) Mindfulness-based interventions for weight loss: a systematic review and meta-analysis. Obes Rev 19(2):164–177. https://doi.org/10.1111/obr.12623
Beaton DE, Bombardier C, Guillemin F, Ferraz MB (2000) Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 25(24):3186–3191. https://doi.org/10.1097/00007632-200012150-00014
Osborne JW, Costello AB (2004) Sample size and subject to item ratio in principal components analysis. Pract Assess Res Eval 9:1–9. https://doi.org/10.7275/ktzq-jq66
Van Strien T, Frijters JER, Bergers GPA, Defares PB (1986) The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behaviour. Int J Eat Disord 5(2):295–315. https://doi.org/10.1002/1098-108X(198602)5:2%3c295::AID-EAT2260050209%3e3.0.CO;2-T
Bozan N, Bas M, Asci FH (2011) Psychometric properties of Turkish version of Dutch Eating Behaviour Questionnaire (DEBQ) A preliminary results. Appetite 56(3):564–566. https://doi.org/10.1016/j.appet.2011.01.025
Revelle W, Zinbarg RE (2009) Coefficients alpha, beta, omega, and the glb: comments on Sijtsma. Psychometrika 74(1):145–154. https://doi.org/10.1007/s11336-008-9102-z
Salvucci S, Walter E, Conley V, Fink S, Saba M (1997) Measurement Error Studies at the National Center for Education Statistics, NCES 97–464. U.S. Department of Education. National Center for Education Statistic, Washington D.C.
Cheung GW, Rensvold RB (2000) Assessing extreme and acquiescence response sets in cross-cultural research using structural equations modeling. J Cross Cult Psychol 31(2):187–212. https://doi.org/10.1177/0022022100031002003
Bryne BM, Watkin D (2003) The issue of measurement invariance revisited. J Cross Cult Psychol 34(2):155–175. https://doi.org/10.1177/0022022102250225
Wang Y, Ding Y, Song D, Zhu D, Wang J (2016) Attitudes toward obese persons and weight locus of control in chinese nurses: a cross-sectional survey. Nurs Res 65(2):126–132. https://doi.org/10.1097/NNR.0000000000000145
Sikorski C, Luppa M, Glaesmer H, Brähler E, König HH, Riedel-Heller SG (2013) Attitudes of health care professionals towards female obese patients. Obes Facts 6:512–522. https://doi.org/10.1159/000356692
Mason C, de Dieu TJ, Duggan C, Wang CY, Alfano CM, McTiernan A (2019) Eating behaviors and weight loss outcomes in a 12-month randomized trial of diet and/or exercise intervention in postmenopausal women. Int J Behav Nutr Phys Act 16(1):113. https://doi.org/10.1186/s12966-019-0887-1
De Lauzon-Guillain B, Basdevant A, Romon M, Karlsson J, Borys JM, Charles MA, FLVS Study Group (2006) Is restrained eating a risk factor for weight gain in a general population? Am J Clin Nutr 83(1):132–138. https://doi.org/10.1093/ajcn/83.1.132
Micanti F, Iasevoli F, Cucciniello C, Costabile R, Loiarro G, Pecoraro G et al (2017) The relationship between emotional regulation and eating behaviour: a multidimensional analysis of obesity psychopatholog. Eat Weight Disord 22(1):105–115. https://doi.org/10.1007/s40519-016-0275-7
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For the study, ‘Research Board Approval’ was obtained from the Alanya Alaaddin Keykubat University Faculty of Medicine Clinical Research Ethics Committee with the decision number 10354421-2021/01-31 and dated 13.01.2021.
Informed consent
Informed consent was obtained from all the individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kahraman, C.Ş., Ayhan, N.Y. Investigation of the psychometric properties of the Turkish version Multidimensional Weight Locus of Control Scale (T-MWLCS) in individuals with different body mass index. Eat Weight Disord 27, 1847–1854 (2022). https://doi.org/10.1007/s40519-021-01328-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01328-9