Abstract
Purpose
Current study aimed to empirically test the Hemmingsson’s theoretical model of childhood obesity which emphasizing the importance of family environment and the emotional distress of parents as influential variables in the emotional distress of the child and subsequent weight gain. This study also tested the hypothesis that the emotional distress of the child triggers a weight gain-inducing behavior (loss of control eating) to suppress negative emotions.
Methods
Families of 220 Spanish children participated in the study (28.2% normal, 35.1% overweight and 32.2% obesity), aged between 8 and 12. The evaluation included a clinical interview and a battery of questionnaires.
Results
Structural equation models were computed according to the steps proposed by theoretical model. Fit indices were acceptable suggesting that the data adequately fit the hypothesized model. Path coefficients in the final model were statistically significant showing a relationship between socioeconomic status, the emotional distress of parents, family environment, the emotional distress of children, loss of control eating and child’s BMI Z-score.
Conclusion
Considering this relation between emotional distress and child weight status, childhood obesity intervention programs may benefit from targeting family environment and the potential role that food is playing in the regulation of children’s distress.
Level of evidence
Level III: Cohort analytic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is consensually understood as a multicausal illness that responds to the influence of a wide variety of closely related factors. The interest in emotional and family factors related to childhood obesity has increased over time [1]. Childhood obesity has been linked to dysfunctional family environments, characterized by expressed emotion (i.e., criticism and lack of emotional support) [2], high levels of family conflict [3] and family emotional distress [4]. Likewise, children with obesity more frequently present psychological disorders [5] and maladaptive emotional regulation strategies, such as the use of food as a way of reducing emotional distress [6].
A critical review of the literature, carried out by Hemmingsson [7, 8], proposed a theoretical model that relates these family and psychological variables with another factor commonly related to weight gain, the socioeconomic status.
In most industrialized countries, low socioeconomic status is associated with an increased risk of obesity [9]. To explain this relationship, the theoretical model proposes that socioeconomic disadvantage increases emotional distress in the family, affecting the family environment and the child’s psychological well-being. At the same time, child emotional distress triggers weight-gain inducing behaviors, such as eating to suppress negative emotions [10,11,12]. In this way, the child’s weight would increase causing obesity (see Fig. 1) [7, 8].
In the theoretical model, reverse causality is also considered in the last step. In this way, once obesity has developed, this generates an increase in psychological symptomatology and a worse family environment [8].
The relationship between the different steps of the model has been empirically verified. A low socioeconomic level is associated with a higher emotional distress and psychological problems in adults [13,14,15] and their children [16]. In the same way, parent’s psychological problems, as maternal depression [17, 18], have been related to emotional distress in their children [17,18,19], finding higher levels of internalizing (problems related with changes in sleep or appetite, crying, fear, anxiety), externalizing (problems related with fighting, yelling, stealing) and general psychopathology as well as higher levels of negative affect and lower levels of positive affect [17]. Likewise, the results of Crawford et al. (2010) showed how the relationship between maternal and child negative affect could be mediated by family functioning [18]. Focusing specifically on childhood obesity, both parent’s psychological problems and family environment have been related to the increase in the body mass index [20] and the development of eating disorders [21, 22].
In this regard, more and more evidence is provided of the importance of loss of control (LOC) eating as a disordered eating in childhood obesity. LOC eating has been defined as “eating with the associated experience of being unable to control how much one is eating independent of the amount of food consumed” [23]. Its prevalence is higher than 30% in childhood obesity [24] and it has also been related to many of the factors discussed previously. Specifically, previous studies have found in children with LOC eating a worse family environment [25, 26], higher psychological symptomatology [6, 27], higher body mass index (BMI) and greater risk for adiposity and adverse metabolic outcomes [6]. Likewise, it has been considered a maladaptive emotional regulation mechanism of the child [28]. Therefore, LOC eating could be one of the main forms of disordered eating to reduce the emotional distress that Hemmingsson pointed out in his model.
Finally, there are examples across the literature that show the inverse causality at the moment that obesity occurs, related, at least in part, to weight stigma and obesity discrimination in our society [34, 35]. Obesity has been linked in longitudinal studies as a risk factor for the development of low self-esteem [29, 30] and mental health problems, as eating disorders [31]. The long-term effects even affect the socioeconomic level, specifically at the educational level. Several studies have found that children with obesity had lower academic attainment, even controlling intelligence quotient [32, 33]. How the body mass index affects food intake has also been studied, finding that people with obesity find greater pleasure in food intake [36]. A recent revision also showed a vicious cycle in which ingestion of high-energy diets altered hippocampal function, which in turn increased size and frequency of the meals, causing and/or perpetuating obesity and possibly exacerbating hippocampal damage [37].
This model has been partially tested in adults [38]. Their conclusion showed how psychological distress and subsequent emotional eating represent a serial pathway that links lower socioeconomic status with obesity. In their study, parental measures were not included. Likewise, McConley et al. (2011) tested a path model in which maternal depression, among others, were associated with parenting quality, which related to some risk factors for child obesity, as diet, and child BMI [20]. Thus, in spite of the evidence found in the literature, no study has evaluated all the factors of Hemmingsson’s model simultaneously.
For this reason, the current study aimed to empirically test Hemmingsson’s [8] theoretical model in a large sample of families of children with a range variety of weight status. Although the original model does not specifically include the LOC eating construct, its model could provide an ethological explanation of how this disordered eating develops in children. Since the correlates associated with LOC eating are similar to those exposed in Hemmingsson’s model and the loss of control in eating fits with the step “psychological and emotional overload” we consider that it is an appropriate construct to be introduced into the model. For this reason, a second aim of this study is to evaluate the effect of loss of control eating as a measure of emotional regulation eating.
Methods
Participants and design
A cross-sectional study was carried out, which included a clinical interview and a battery of questionnaires. Families were recruited for a bigger study (ANOBAS study, PSI2011-23,127) designed to assess early risk factors for childhood obesity, such as biological, environmental, familiar and individual factors in a sample of preadolescents aged 8–12 years from the region of Madrid, Spain. A total of 220 Spanish families were evaluated, and the data of the children (aged 8–12 years) and their main caregivers were evaluated between 2012 and 2017. Families from two Primary Care Centers and several public and subsidiary primary schools (all in geographical proximity) were invited to participate in the study. Those participants who presented secondary obesity, those who did not have an adequate oral or written command of Spanish and those who suffered from a developmental disorder were excluded from the study. Participants were summoned to their Primary Care Center or their primary school, where a trained interviewer carried out a semi-structured interview, with the main caregiver and the child separately, and provided the questionnaires. Both the primary caregiver and the child answered the questionnaires alone and handed them over to the interviewer at the time of the assessment. At this time, height and weight of parents and child were measured using a digitally calibrated scale. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Niño Jesus Children’s Hospital (No Ref. 0009/10), Central Committee of Research, Primary Care Commission (Ref. 11/12), and the corresponding University Committee (Autonomous University of Madrid) (CEI 27-673). Participation was voluntary and informed assent and informed consent was obtained from each participating family.
Instruments
Socioeconomic disadvantage
Socioeconomic Status was estimated with the Hollingshead Index of Socioeconomic Status [39], which is a survey designed to measure the social status of an individual based on education level (1 = primary level, 2 = secondary level, 3 = high school/technical School, 4 = university) and job position (range of 0–9 depending on economic gains). As an example, level 1 includes minor service jobs, such as dishwashers, and level 9 includes senior executives or owners of large companies.
Emotional distress
The State Trait Anxiety Inventory (STAI)–Trait Anxiety Subscale [40]. The Trait Anxiety Subscale of the Inventory reflects the existence of stable individual differences in the tendency to respond with state anxiety in the anticipation of threatening situations. Higher scores indicate higher levels of anxiety. The Spanish validation reported a Cronbach’s alpha of 0.90 for Anxiety–Trait. In the current study, reliability was similar (α = 0.92).
Beck Depression Inventory (BDI-II) [41]. This self-report scale contains 21 items measuring somatic and cognitive-affective symptoms. Higher scores indicate higher levels of depression. The BDI-II has demonstrated high internal consistency in the Spanish validation (α = 0.87) [41]. In the current study, it was high (α = 0.91).
Disharmonious family environment
Family Adaptability and Cohesion Evaluation Scales (FACES-III) [42]. This 20-item self-report measure contains two subscales: adaptability and cohesion, and a total score. The Adaptability scale measures the degree to which families can change depending on the demands of the situation and the Cohesion subscale assess the degree of separation or connection between family members. For the Spanish version, Cronbach’s alphas were of 0.72 and 0.68 for the Cohesion and Adaptability scales, respectively [42]. For the current study, it was 0.73 and 0.70, respectively.
Family Questionnaire (FQ) [43], which has 20 items that evaluate family members’ levels of Expressed Emotion (EE). The FQ is made up of two subscales: Criticism and Emotional Over-involvement. Higher scores indicate higher levels of EE. Acceptable reliability was found for the Spanish version ranging from 0.72 to 0.83 for each subscale, respectively [43]. For the current study, they were slightly higher (Criticism, α = 0.81 and Emotional Over-Involvement, α = 0.84).
Dyadic Adjustment Scale (DAS-13) [44]. This scale has 13 items that assesses the quality of the marital relationship. Higher scores indicate high marital adjustment. For the Spanish validation, reliability was high (α = 0.94) [44]. In the current sample, it was satisfactory (α = 0.83).
Children’ psychological and emotional distress
The State–Trait Anxiety Inventory for Children (STAIC)—Trait Anxiety Subscale [45], which is composed of two separate anxiety scales, which consist of 20 items each. The Trait Anxiety Subscale measures dispositional, or more stable, levels of anxiety. Cronbach’s alpha was 0.85 for trait–anxiety in the Spanish version [45]. In the current study, reliability was similar (Trait, α = 0.89).
Child Depression Inventory (CDI) [46] consists of 27 items that assess child depression symptoms. Higher scores indicate higher levels of depression. The internal reliability of the Spanish version was 0.69 [46]. In the current sample, Cronbach’s alpha was 0.79.
Lawrence’s Self-Esteem Questionnaire (LAWSEQ) [47] is composed of 16 items that assess a child’s self-esteem, excluding the assessment of body image and body satisfaction. Higher scores indicate higher levels of self-esteem. For the Spanish version, internal reliability was 0.67 [47]. In the current study, reliability was slightly higher (α = 0.72).
The Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS-PL) [48] is a semi-structured interview which is divided into 20 different diagnostic areas. Questions are directed at the children, and responses confirmed with the parents separately. For the current study, definitive clinical child diagnoses (scored 1 vs non-diagnoses scored as 0) were adapted to the DSM-5 criteria by the researchers.
Loss of Control Eating (LOC). The presence of episodes of loss of control eating has been evaluated through a semi-structured interview on the eating habits and eating behavior of the child. The interview was conducted first with the child alone. Subsequently, the information provided by the child was verified by the main caregiver alone. The presence of LOC episodes was determined following the criteria proposed by Tanosky-Kraff [23]: “(1) A sense of lack of control over eating and food seeking in the absence of hunger or after satiation and (2) three or more of the following: eating in response to negative affect, secrecy regarding the episode, feelings of numbness while eating, eating more (or perception of eating more than others) and negative affect following eating”. LOC eating was defined as present when the LOC eating episodes occur at least twice a month for 3 months.
Childhood obesity
Children’s Body Mass Index. During the evaluation, the height and weight of the children were collected using a Seca digital (Type 799 and 769) weighing scale (kg) and a tallimeter. The children’s Body Mass Index (BMI = weight in kilograms / height in meters squared) was calculated using Z-scores, the BMI compared to the average BMI of the population according to age and sex [49]. The range of Z-scores was between − 0.90 and + 5.15 (28.2% normal weight, 35.1% overweight and 32.2% obesity).
Statistical analysis
The analysis of the data was carried out using the SPSS 21.0 program for Windows and Mplus software. The results are expressed in terms of frequencies, means and standard deviations. For the analysis of continuous variables, one-way ANOVA was used for independent samples to compare the means between groups. To analyze differences between the frequencies of the categorical variables between groups, Chi-square test were used. This study aims to assess the plausibility of Hemmingsson’s model [8]. For that, several structural equation models (SEM) were computed according to the steps proposed by Hemmingsson. The different models were nested, including in each model a new factor following Hemmingsson’s proposal (see Table 1).
The maximum likelihood method (MLM) estimation was used given the non-normal distribution of the data. The model fit was assessed using the χ2 SB/DF (Chi-Square/Degrees of Freedom) ratio, root mean square error of approximation (RMSEA) with its 90% confidence interval, comparative fit index (CFI). χ2 SB/DF is first considered given that it is usually taken as a rule of thumb [50]. Values showing a good fit must be around 2.0. In the case of RMSEA, values of < 0.06 were expected, and for CFI values above 0.95 were considered a good fit [51].
Results
Differences in sociodemographic and psychopathological variables between groups
Table 2 shows the differences in sociodemographic and psychopathological variables of the 220 children and their parents. Children were divided into three groups by their weight status as a normal weight (15th–85th BMI percentile), overweight (between 85th and 97th percentiles) and obesity (percentile higher than 97th).
Statistically significant differences were observed in the three groups: the results of the one way ANOVA indicated that there was a difference in the mothers’ age, mother’s BMI and child Z-score BMI amongst the weight status groups. However, post-hoc comparisons using a Tukey Honestly Significant Difference test indicated that the differences in mean scores were significantly different only between the mothers’ BMI (higher in the obesity group than in the normal weight group) and child Z-score BMI (significant differences amongst the three groups). In addition, statistically significant differences were observed both in the proportion of loss of control eating episodes and in the proportion of DSM-5 diagnoses found between the three groups, being both higher in the obesity group.
Structural equation models
Table 3 shows the fit indices for each model computed. Hemmingsson model considered that once obesity has been established, there is a reverse causality of the factors. For this reason, two final models can be observed in Table 3 (Model 5a and 5b). Model 5a includes in the last step the prediction of child BMI through LOC eating, while model 5b would include inverse causality in which child BMI predicts the presence of LOC eating.
The fit indexes of the models were appropriated with Chi-Square/Degrees of Freedom ratio around 2.00; RMSEA values around 0.60 and CFI values higher to 0.90. However, the final model (Model 5) showed a non-satisfactory fit (Model 5a [LOC → Child’s BMI Z-score]: χ2 SB/DF = 1.959; RMSEA = 0.065; CFI = 0.866. Model 5b [Child’s BMI Z-score ← LOC]: χ2 SB/DF = 1.941; RMSEA = 0.068; CFI = 0.887).
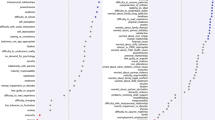
An inspection of the modification indexes (M.I.) depicted a correlation between the Dyadic Adjustment Scale (DAS) and the Family Adaptability and Cohesion Evaluation Scale (FACES). M.I. = 11.938 (Model 5a) and M.I. = 12.948 (Model 5b). Therefore, we computed a second model allowing the correlation between DAS and FACES for the two version of the Model 5. The correlation values between DAS and FACES were of r = 0.270; p < 0.001 (Model 5.a.1) and r = 0.285; p < 0.001 (Model 5.b.1). The fit indexes of the second version were better, but not totally satisfactory (Model 5a.1: χ2 SB/DF = 1.837; RMSEA = 0.061; CFI = 0.883. Model 5b.1: χ2 SB /DF = 1.813; RMSEA = 0.063; CFI = 0.903). Therefore, a second inspection of the M.I depicted a high association between the two depression measures [Children’s Depression Inventory (CDI) and Beck Depression Inventory (BDI) of parents]. The M.I. for the different models were of 10.927 (Model 5a.1) and 8.896 (Model 5b.1). Consequently, we carried out a third model allowing the correlation between CDI and BDI for the Model 5a.1 (r = − 0.34; p < 0.001) and for the Model 5b.1 (r = − 0.30; p = 0.002). The fit of this estimation was satisfactory for both models (Model 5a.2: χ2 SB/DF = 1.718; RMSEA = 0.057; CFI = 0.901. Model 5b.2: χ2 SB/DF = 1.728; RMSEA = 0.060; CFI = 0.914). Figure 2 depicts the standardized final values for the latent factors included in the Models 5a.2 and 5b.2. See Appendix 1 (See Table 4) with the standardized loading for each variable in the Model 5a.2 and Model 5b.2.
Structural equation models of the role of emotional distress promoting childhood obesity. SE Socioeconomic Status; EDP Emotional Distress of parents; DFE Disharmonious Family Environment; PEC Psychological and Emotional Children status; LOC Loss of Control Eating; BMI Body Mass Index; EL Educational Level; JP Job position; STAI Anxiety–Trait; BDI Beck Depression Inventory; FACES ; DAS Dyadic Adjustment Scale; EOI Emotional Overinvolvement; CC Criticism; STAIC Child Anxiety–Trait; LAWSEQ Lawrence’s Self-Esteem Questionnaire; CDI Child Depression Inventory; KSADS Child diagnoses
In both models, a low Socioeconomic status (SE) factor predicted a high Emotional Distress of parents (EDP) with a moderate value (around 0.20). This EDP was highly associated with a Disharmonious Family Environment (DFE) with values higher than 0.70. In the next stage, DFE predicted the Psychological and Emotional Children status (PEC) with medium values (around 0.50). The PEC factor predicted the Loss of Control Eating (LOC) in the Model 5a.2 (0.234; p = 0.001), but this part of the model was marginally statistically significant in the Model 5b.2 (0.148; p = 0.052). Finally, the outcomes of the Model 5a.2 depicted that the LOC predicted Child’s BMI Z-score (0.397; p < 0.001). Similar results were found in the Model 5b.2 when Child’s BMI Z-score predicted the LOC (0.372; p < 0.001).
Besides, a web platform (http://www.quantpsy.org/rmsea/rmsea.htm; Peacher and Coffman, 2006) was employed to compute the power level achieved with our data in the final SEM (Model 5a.2 and Model 5b.2). The data included in the estimation were: degree of freedom = 85, sample size = 220, alpha = 0.05; null RMSEA = 0.05; alternative RMSEA = 0.10. The power level was of 0.99 for both models.
Discussion
The study aimed to test the theoretical model proposed by Hemmingsson [8] regarding the “role of psychological and emotional distress in promoting obesity”. Our findings showed a relationship between socioeconomic status, the emotional distress of parents, family environment, the emotional distress of children, loss of control eating and child’s BMI Z-score.
In the first step of the model, as expected, low socioeconomic status predicted high emotional distress of parents. Arguably, people of a low socioeconomic level may be exposed to more stressful experiences [13, 14] and are more likely to generate a higher level of psychological distress when exposed to these stressors [14]. One of the variables that are taken into account to establish the socioeconomic level is the educational level. It has been proven that a low educational level is related to lower levels of resilient resources (i.e., perceived control and social support) [14]. When dealing with problematic situations, having fewer personal resources creates a higher level of psychological distress.
In the second step of the model, the emotional distress of parents was highly associated with a disharmonious family environment. For the adequate adjustment of the model, it was necessary to include a correlation between the variables of marital adjustment and family adaptability and cohesion. The measure of family adaptability and cohesion (FACES) measures cohesion among family members, and therefore it is also related to the quality of the marital relationship. Depression is significantly associated in the literature with more disengaged parenting and less warm interactions [52]. This relationship is explained by the characteristics associated with these disorders. Parental behaviors reflect the symptoms that characterize emotional distress (loss of interest, fatigue, lack of concentration, feelings of self-reproach). Therefore, they may be “emotionally unavailable” and may exhibit behavioral deficits, including difficulties attending to a child’s needs or responding effectively [20, 52].
The third step of the model was “emotional distress in the offspring”, where a significant relationship between the maladjusted family environment and the child’s psychological and emotional distress were found. This relationship has been previously found across the literature [17, 18, 53]. One possible explanation for this relationship is the presence of a family member with dysfunctional patterns that affects the child’s environment as a repeated daily stressor, possibly creating deficits in the expression of the child’s emotions and reducing the development of his/her social competence, or presenting inadequate cognitive/emotional maturity to cope with these stressors [22, 54]. Another possible explanation is that children tend to internalize family values and frustrations, in the form of negative emotions, anxiety or depression, thus promoting an increase in psychological and emotional distress [19]. Concerning this, in our study, a significant inverse correlation was found between the family’s depressive symptomatology and the child’s depressive symptomatology. This result, despite the incongruence with the literature, suggested that maternal depression is related to the psychological and emotional discomfort of the child and not specifically to depressive symptomatology, but to a range of symptoms or disorders of the child. Previous studies found that parental mental illness has been related to lower levels of monitoring, which in turn are related to externalizing problems in children [54]. Children with these diagnoses could score lower on the CDI questionnaire. In future studies, it would be convenient to evaluate other aspects of the family environment, as parent monitoring that could explain this relationship.
The next step of the model is the Psychological and emotional overload. In the present study, a significant relationship between the psychological and emotional discomfort of the child and the presence of LOC episodes were observed. Previous studies find the precedence of psychological discomfort to the presence of loss of control eating [6, 12]. These results are consistent with the affect regulation model [10]. This model proposes that increases in negative emotions trigger loss of control episodes, and that this disordered eating serves as a means to relieve negative affect using food for comfort and distraction [55]. This model has been previously proved in binge eating [55] and presents an initial evidence on loss of control eating [6, 12].
Finally, the LOC variable was directly and significantly related to the child’s weight status. This is congruent with previous longitudinal studies that showed that LOC episodes during childhood increased the risk of adult obesity [11].
The last model studied presented inverse causality, in which the body mass index predicted the presence of LOC episodes. A model with an appropriate fit was obtained. These results indicate that the increase in BMI can also be a predictor of the occurrence of episodes of over-eating and LOC episodes, as found in other studies in humans and animals [36, 37]. However, one of the model parts (psychological and emotional child status –> LOC) was only marginally statistically significant. Therefore, model 5a.2 (LOC –> BMI) seems more plausible than this second model. The onset of LOC episodes has been evaluated in populations with similar ages to those in this study (8–12 years), so it appears reasonable to assume that they are present in an early stage of the development of this problem. It would be necessary to conduct longitudinal studies with an older population to evaluate more thoroughly how their behavior evolves.
The results of this study must be interpreted considering the following shortcomings. First, due to the cross-sectional nature of our study, causality and temporal precedence cannot be inferred. These results are only indicative and must be verified in longitudinal studies. Second, Hemmingsson’s model focused on the role of emotional distress as a link between socioeconomic status and childhood obesity. For this reason, other risk factors (genetic, epigenetic, diseases, others) have not been taken into account. For example, psychological distress variables of parents and their children may be due in part to the shared genetics between both of them. Despite this, studies have found an environmental link between the psychological symptoms of parents and children regardless of whether parents and their children were genetically related [56]. Finally, the age range of the participants is narrow (8–12 years), so the results obtained may not be generalizable to other age groups, such as adolescence.
In conclusion, this model provides further evidence that the causality of obesity is complex. Likewise, trying to understand the potential role that food plays in the regulation of children’s distress, as well as, the emotional barriers that can impede the implementation of strategies aimed at changing some eating patterns (e.g. reduce the amount of food or eat slower) suggests further directions of enquiry. Taking into consideration the results of this study, it is recommended to evaluate the family environment, psychological distress and the presence of LOC eating in the population with childhood obesity, as well as to introduce identification and emotional regulation strategies within childhood obesity intervention programs, with the aim of achieving more effective interventions.
1. What is already known on this subject?
Obesity is understood as a multicausal illness that responds to the influence of a wide variety of closely related factors, including family and psychological variables.
2. What this study adds?
A model of the development and maintenance of childhood obesity that combines social, family and psychological variables.
References
Puder JJ, Munsch S (2010) Psychological correlates of childhood obesity. Int J Obes (Lond) 34:S37–S43. https://doi.org/10.1038/ijo.2010.238
Çolpan M, Eray Ş, Eren E, Vural AP (2018) Perceived expressed emotion, emotional and behavioral problems and self-esteem in obese adolescents: a case-control study. J Clin Res Pediatr Endocrinol. https://doi.org/10.4274/jcrpe.0101
Halliday JA, Palma CL, Mellor D, Green J, Renzaho AMN (2014) The relationship between family functioning and child and adolescent overweight and obesity: a systematic review. Int J Obes 38:480–493. https://doi.org/10.1038/ijo.2013.213
Benton PM, Skouteris H, Hayden M (2015) Does maternal psychopathology increase the risk of pre-schooler obesity? A systematic review. Appetite 87:259–282. https://doi.org/10.1016/j.appet.2014.12.227
Kalarchian MA, Marcus MD (2012) Psychiatric comorbidity of childhood obesity. Int Rev Psychiatry 24:241–246. https://doi.org/10.3109/09540261.2012.678818
Byrne ME, LeMay-Russell S, Tanofsky-Kraff M (2019) Loss-of-Control Eating and obesity among children and adolescents. Curr Obes Rep 8:33–42. https://doi.org/10.1007/s13679-019-0327-1
Hemmingsson E (2018) Early childhood obesity risk factors: socioeconomic adversity, family dysfunction, offspring distress, and junk food self-medication. Curr Obes Rep 7:204–209. https://doi.org/10.1007/s13679-018-0310-2
Hemmingsson E (2014) A new model of the role of psychological and emotional distress in promoting obesity: conceptual review with implications for treatment and prevention. Obes Rev 15:769–779
Frederick CB, Snellman K, Putnam RD (2014) Increasing socioeconomic disparities in adolescent obesity. Proc Natl Acad Sci 111:1338–1342. https://doi.org/10.1073/pnas.1321355110
Leehr EJ, Krohmer K, Schag K, Dresler T, Zipfel S, Giel KE (2015) Emotion regulation model in binge eating disorder and obesity -a systematic review. Neurosci Biobehav Rev 49:125–134
Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA (2009) A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. Int J Eat Disord 42:26–30. https://doi.org/10.1002/eat.20580
Goossens L, Braet C, Van Vlierberghe L, Mels S (2009) Loss of control over-eating in overweight youngsters: the role of anxiety, depression and emotional eating. Eur Eat Disord Rev 17:68–78. https://doi.org/10.1002/erv.892
Haushofer J, Fehr E (2014) On the psychology of poverty. Science (80) 344:862–867. https://doi.org/10.1126/science.1232491
Matthews KA, Gallo LC (2011) Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol 62:501–530. https://doi.org/10.1146/annurev.psych.031809.130711
Braveman P, Gottlieb L (2014) The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 129:19–31. https://doi.org/10.1177/00333549141291s206
Reiss F (2013) Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med 90:24–31. https://doi.org/10.1016/j.socscimed.2013.04.026
Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D (2011) Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev 14:1–27. https://doi.org/10.1007/s10567-010-0080-1
Crawford NA, Schrock M, Woodruff-Borden J (2011) Child internalizing symptoms: contributions of child temperament, maternal negative affect, and family functioning. Child Psychiatry Hum Dev 42:53–64. https://doi.org/10.1007/s10578-010-0202-5
Siegenthaler E, Munder T, Egger M (2012) Effect of preventive interventions in mentally ill parents on the mental health of the offspring: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 51:8-17.e8. https://doi.org/10.1016/j.jaac.2011.10.018
McConley RL, Mrug S, Gilliland MJ, Lowry R, Elliott MN, Schuster MA, Bogart LM, Franzini L, Escobar-Chaves SL, Franklin FA (2011) Mediators of maternal depression and family structure on child bmi: parenting quality and risk factors for child overweight. Obesity 19:345–352. https://doi.org/10.1038/oby.2010.177
López CC, Raimann TX, Gaete PMV (2015) Prevención de los trastornos de conducta alimentaria en la era de la obesidad: rol del clínico. Rev Médica Clínica Las Condes 26:24–33. https://doi.org/10.1016/j.rmclc.2014.12.003
Peris TS, Miklowitz DJ (2015) Parental expressed emotion and youth psychopathology: new directions for an old construct. Child Psychiatry Hum Dev 46:863–873. https://doi.org/10.1007/s10578-014-0526-7
Tanofsky-Kraff M, Marcus MD, Yanovski SZ, Yanovski JA (2008) Loss of control eating disorder in children age 12 years and younger: proposed research criteria. Eat Behav 9:360–365. https://doi.org/10.1016/j.eatbeh.2008.03.002
He J, Cai Z, Fan X (2017) Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: an exploratory meta-analysis. Int J Eat Disord 50:91–103. https://doi.org/10.1002/eat.22661
Hilbert A, Tuschen-Caffier B, Czaja J (2010) Eating behavior and familial interactions of children with loss of control eating: a laboratory test meal study. Am J Clin Nutr 91:510–518. https://doi.org/10.3945/ajcn.2009.28843
Czaja J, Hartmann AS, Rief W, Hilbert A (2011) Mealtime family interactions in home environments of children with loss of control eating. Appetite 56:587–593. https://doi.org/10.1016/j.appet.2011.01.030
Hilbert A, Hartmann AS, Czaja J, Schoebi D (2013) Natural course of preadolescent loss of control eating. J Abnorm Psychol 122:684–693. https://doi.org/10.1037/a0033330
Kelly NR, Tanofsky-Kraff M, Vannucci A, Altschul AM, Ranzenhofer LM, Schvey NA, Shank LM, Brady SM, Galescu O, Kozlosky M, Yanovski SZ, Yanovski JA (2016) Emotion dysregulation and loss-of-control eating in children and adolescents. Heal Psychol 35:1110–1119. https://doi.org/10.1037/hea0000389
Puhl RM, Heuer CA (2010) Obesity stigma: important considerations for public health. Am J Public Health 100:1019–1028. https://doi.org/10.2105/AJPH.2009.159491
Andreyeva T, Puhl RM, Brownell KD (2008) Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. Obesity 16:1129–1134. https://doi.org/10.1038/oby.2008.35
Wang F, Veugelers PJ (2008) Self-esteem and cognitive development in the era of the childhood obesity epidemic. Obes Rev 9:615–623. https://doi.org/10.1111/j.1467-789X.2008.00507.x
Wang F, Wild TC, Kipp W, Kuhle S, Veugelers PJ (2009) The influence of childhood obesity on the development of self-esteem. Health Rep 20:21–27
de Portela Santana ML, da Costa RH, Mora Giral M, Raich RM (2012) La epidemiología y los factores de riesgo de los trastornos alimentarios en la adolescencia; una revisión. Nutr Hosp 27:391–401
Booth JN, Tomporowski PD, Boyle JME, Ness AR, Joinson C, Leary SD, Reilly JJ (2014) Obesity impairs academic attainment in adolescence: findings from ALSPAC, a UK cohort. Int J Obes (Lond) 38:1335–1342. https://doi.org/10.1038/ijo.2014.40
Karnehed N, Rasmussen F, Hemmingsson T, Tynelius P (2006) Obesity and attained education: cohort study of more than 700,000 Swedish men. Obesity 14:1421–1428. https://doi.org/10.1038/oby.2006.161
Miller AC, Polgreen LA, Segre EM, Polgreen PM (2019) Variations in marginal taste perception by body mass index classification: a randomized controlled trial. J Acad Nutr Diet. https://doi.org/10.1016/j.jand.2019.05.018
Parent MB, Darling JN, Henderson YO (2014) Remembering to eat: Hippocampal regulation of meal onset. Am J Physiol Regul Integr Comp Physiol 306:R701–R713. https://doi.org/10.1152/ajpregu.00496.2013
Spinosa J, Christiansen P, Dickson JM, Lorenzetti V, Hardman CA (2019) From socioeconomic disadvantage to obesity: the mediating role of psychological distress and emotional eating. Obesity 27:559–564. https://doi.org/10.1002/oby.22402
Hollingshead AB (2011) Four factor index of social status. Yale J Sociol 8:21–53
Guillén-Riquelme A, Buela-Casal G (2011) Actualización psicométrica y funcionamiento diferencial de los ítems en el State Trait Anxiety Inventory (STAI). Psicothema 23:510–515
Sanz J, Vazquez C (2003) Adaptación española del Inventario para la depresión de Beck-II: propiedades psicométricas en población general. Análisis y Modif Conduct 29:239–288
Martínez-Pampliega A, Iraurgi I, Galíndez E, Sanz M (2006) Family Adaptability and Cohesion Evaluation Scale (FACES): Desarrollo de una versión de 20 ítems en español. Int J Clin Heal Psychol 6:317–338
Sepulveda AR, Anastasiadou D, Rodríguez L, Almendros C, Andrés P, Vaz F, Graell M (2014) Spanish validation of the Family Questionnaire (FQ) in families of patients with an eating disorder. Psicothema 26:321–327. https://doi.org/10.7334/psicothema2013.310
Cano-Prous A, Martín-Lanas R, Moyá-Querejeta J, Beunza-Nuin MI, Lahortiga-Ramos F, García-Granero M (2014) Psychometric properties of a Spanish version of the Dyadic Adjustment Scale. Int J Clin Heal Psychol 14:137–144. https://doi.org/10.1016/S1697-2600(14)70047-X
Seisdedos N (1990) STAIC, Cuestionario de autoevaluación. Madrid TEA Ediciones, SA
Davanzo P, Kerwin L, Nikore V, Esparza C, Forness S, Murrelle L (2004) Spanish translation and reliability testing of the child depression inventory. Child Psychiatry Hum Dev 35:75–92. https://doi.org/10.1023/B:CHUD.0000039321.56041.cd
De Gracia M, Marcó M, Trujano P (2007) Factores asociados a la conducta alimentaria en preadolescentes. Psicothema 19:646–653
Ulloa RE, Ortiz S, Higuera F, Nogales I, Fresán A, Apiquian R, Cortés J, Arechavaleta B, Foulliux C, Martínez P, Hernández L, Domínguez E, De La Peña F (2006) Interrater reliability of the Spanish version of schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL). Actas Esp Psiquiatr 34:36–40
Sánchez-Cruz JJ, Jiménez-Moleón JJ, Fernández-Quesada F, Sánchez MJ (2013) Prevalencia de obesidad infantil y juvenil en España en 2012. Rev Esp Cardiol 66:371–376. https://doi.org/10.1016/j.recesp.2012.10.016
Jöreskog KG (1993) Testing structural equation models. Testing structural equation models. Sage, pp 294–316
Hu LT, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model 6:1–55. https://doi.org/10.1080/10705519909540118
National Research Council, Institute of Medicine (2009) Associations between depression in: parents and parenting child health, and child psychological functioning in depression in parents, parenting, and children: opportunities to improve identification, treatment, and prevention. National Academies Press, USA
Duclos J, Vibert S, Mattar L, Godart N (2012) Expressed emotion in families of patients with eating disorders: a review of the literature. Curr Psychiatry Rev 8:183–202. https://doi.org/10.2174/157340012800792975
Hanington L, Heron J, Stein A, Ramchandani P (2012) Parental depression and child outcomes—is marital conflict the missing link? Child Care Health Dev 38:520–529. https://doi.org/10.1111/j.1365-2214.2011.01270.x
Dingemans A, Danner U, Parks M (2017) Emotion regulation in binge eating disorder: a review. Nutrients 9:1274. https://doi.org/10.3390/nu9111274
Lewis G, Rice F, Harold GT, Collishaw S, Thapar A (2011) Investigating environmental links between parent depression and child depressive/anxiety symptoms using an assisted conception design. J Am Acad Child Adolesc Psychiatry 50:451-459.e1. https://doi.org/10.1016/j.jaac.2011.01.015
Funding
This study was funded by the Ministry of Science and Innovation, National Plan R + D + I 2008/11 (PSI2011-23127).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures were approved by the Ethics Committee of the Faculty of Psychology (Autonomous University of Madrid), Child Hospital Niño Jesus and Primary Care Commission.
Informed consent
All participants gave their written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Appendix 1
See Table 4
Rights and permissions
About this article
Cite this article
Sepúlveda, A.R., Lacruz, T., Solano, S. et al. Using structural equation modeling to understand family and psychological factors of childhood obesity: from socioeconomic disadvantage to loss of control eating. Eat Weight Disord 27, 1809–1819 (2022). https://doi.org/10.1007/s40519-021-01323-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01323-0