Abstract
Purpose
Nutrient patterns have been associated with an increased risk for chronic disease. Evidence to confirm a direct relationship between nutrient patterns and obesity and metabolic syndrome (MetS) throughout population-based differences including cultural contexts add complexity is not well established yet. The aim of this study is to investigate the association between nutrient patterns and MetS among overweight and obese Iranian women.
Methods
Three hundred and sixty obese and overweight women (25 < BMI < 40) were included in this cross-sectional analysis. Dietary intake of 19 nutrients was evaluated by a semi-quantitative standard food frequency questionnaire (FFQ). MetS was determined by abdominal obesity > 88 (cm) in females, Triglycerides ≥ 150 (mg/dL), dyslipidemia (HDL < 50 mg/dL), systolic blood pressure > 130/85 (millimeters), and glucose > 100 (mg/dL). Body composition was assessed by a multi-frequency bioelectrical impedance analyzer, InBody 770 scanner. Principle components analysis was applied and four nutrient patterns were identified as following: Pattern 1 (thiamin, iron, carbohydrate, zinc, niacin, protein, magnesium, phosphorus, riboflavin), represented the carbo-vitamin group. Lipid group was showed in pattern 2 (PUFAs, MUFA, vitamin E, trans fatty acids, and Pattern 3 (beta-carotene, vitamin K, vitamin A, vitamin C) represented the anti-oxidant group, finally Pattern 4 was the indicator of the milk group (vitamin D, calcium).
Results
A significant positive association was observed between the anti-oxidant group and obesity (OR 1.40; 95% CI 1.09–1.8; P = 0.01). No relationship between other nutrient pattern and MetS was observed.
Conclusions
The nutrient patterns that are highly loading of beta-carotene, vitamin K, vitamin A, and vitamin C in nutrient patterns may be associated to higher risk of obesity in overweight and obese Iranian women.
Level of evidence
Level V, cross-sectional descriptive study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The increasing prevalence of obesity and related chronic diseases has become a challenge for global population health [1, 2]. Based on current trends, it has been estimated that by the year 2030, 1.2 billion individuals will be overweight and 16.2 billion will be obese globally [1, 3, 4]. Metabolic syndrome (MetS), the clustering of chronic disease risk factors, characterized by abdominal obesity, insulin resistance, dyslipidemia, high blood pressure, and high blood glucose levels is commonly identified among obese individuals [5]; however, not all obese people have MetS and not all individuals with MetS are obese. Many factors have been investigated to better understand the variability, but few studies have succeeded in uncovering a causal factor underlying etiology [6, 7].
Undoubtedly dietary factors are involved. However, it is well established the impact extends beyond simple energy imbalance. Dietary quality and by consequence the metabolic response is conceivably the mechanistic underpinning linking obesity and chronic diseases [8]. Therefore, attempts to elucidate the link may be better served by evaluating single foods and nutrients. Malnutrition in the context of dietary quality has been successfully integrated as a method for identifying the physiologic effect of deficiency. Conceivably overconsumption-related diseases and chronic diseases could also benefit [9] as nutrients patterns may help to provide more data about the mechanisms [10,11,12]. As opposed to quantitative energy analysis, dietary factors encompassing nutrient density takes into account diversity in culture and geographical status. [12, 13]. Most of clinical efforts have concentrated on the assessments single food or some nutrients, without taking account the whole diet which can be the responsible of higher risk factor for metabolic diseases and obesity, particularly for one of societies with a large number of chronic diseases and genomic heterogeneity, i.e., Iran. Moreover, the number of systematic clinical assessment of nutrient pattern in association to metabolic syndrome are not well enough in this region. The objective of this study is to investigate the relationship between the nutrient patterns and obesity markers and MetS component among Iranian overweight and obese women.
Materials and methods
Study population
A cohort of 360 obese and overweight women aged 18–50 years who referring to health centers in Tehran was recruited and examined. Individuals with body mass index (BMI) between 25 and 40 kg/m2, aged 18–48 years, an absence of any acute or chronic disease were included. In addition, they were excluded by following circumstances: menopause, pregnancy, lactation, smoking, any acute and chronic diseases including type I and II diabetes, cardiovascular disease, hypertension, cancer, liver or renal dysfunction, and thyroid disease. The subjects also were excluded if had special dieting during the last year, intake any medicine (lowering lipid, glucose and blood pressure) or any supplementation for weight loss. Furthermore, we excluded those women with weight loss history in recent years, and who reported total daily energy lower than 800 kcal/d (3347 kJ/d) or higher than 4200 kcal/d (17 573 kJ/d) [14]. All participants signed a written consent form before taking part in the study. The study was approved by ethics committee of the Tehran University of Medical Sciences with ethics number IR.TUMS.VCR.REC.1395.1597.
Biochemical assessment
Blood samples were collected in the nutrition and biochemistry laboratory at Tehran University of Medical Sciences. Venous blood was collected between 8: 00 and 10: 00 am following an overnight fasting. Then the serum was centrifuged, aliquoted, and analyzed using a single assay technique. Fasting blood glucose (FBS) was assessed by glucose oxidase–phenol 4-aminoantipyrine peroxidase (GOD-PAP) colorimetric method. Triglyceride (TG) and total cholesterol (TC) were measured by glycerol-3-phosphate oxidase–phenol 4-aminoantipyrine peroxidase (GPOPAP), enzymatic endpoint. Low-density-lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol were measured by direct enzymatic clearance assay. All measurements were done with the use of a Randox Laboratories kit (Hitachi 902).
Body composition analysis
Body compositions were assessed using of a bioelectrical impedance analyzer (BIA) (Inbody 770 Co., Seoul, Korea). According to the manufacturer’s protocol was applied such as removal of extra clothes and shoes [15]. Body weight was measured with a calibrated digital scale to the nearest 0.1 kg with minimum of clothes and without shoes. Height was measured using a strapless tape in the way that participants were shoeless and in a standing position beside the wall, the height was recorded at a precision of 0.5 cm. BMI was calculated by weight (kg)/height (m) squared. According to the definition of the world health organization, overweight as 25 ≤ BMI ≤ 29.9 kg/m2 and obesity is grading Grade 1, 2 and 3 as 30 ≤ BMI ≤ 34.9 kg/m2, 35 ≤ BMI ≤ 39.9 kg/m2 and BMI ≥ 40 kg/m2. Hip and waist circumference was measured by a strapless tape and without imposing any pressure on the body with a precision of 0.5 cm. The waist circumference of participants was evaluated by a Seca non-elastic tape, with exactness close to 0.5 cm. The waist circumference was measured in the smallest girth and on bare skin, without imposing any pressure on the person's body, while the person was at the end of the normal exhale. All measurements were taken the morning before breakfast and were performed by one person to reduce the measurement errors.
IPAQ assessment
International physical activity questionnaire-short form (IPAQ) was applied to assess physical activity (PA). This questionnaire recorded normal activities of daily living, time and frequency of PA each week, during the last 12 months. The level of PA was reported as metabolic equivalent hours per week (METs-h/week) [16].
Blood pressure assessment
Blood pressure was measured in a sitting position after 10 min of rest using an OMRON blood pressure monitor made in Germany.
Assessment of nutrient pattern
The usual food intake of participants was evaluated by the use of a semi-quantitative standard food frequency questionnaire (FFQ) over the past year [17]. The FFQ included 147 items with standard serving sizes commonly consumed by target population. Consumption frequency of each food item was classified as daily, weekly, monthly and yearly. The reported frequencies were converted to a daily intake. Data was converted into grams and milliliters. Dietary intake data were analyzed using the Nutritionist 4 (Hearst Corporation, San Bruno, CA) food analyzer. Nutritionist 4 software (Hearst Corporation, San Bruno, CA) [18] was used to calculate total energy, total fat, cholesterol, essential fat, carbohydrate, protein, vitamins and minerals. Reliability and validation of FFQ have been verified previously [19].
Statistical analysis
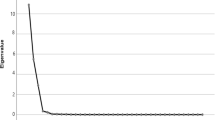
Data were analyzed using SPSS 22.0 software (SPSS, Chicago, IL, USA). For all tests, p values < 0.05 were considered significant. Normal distribution of data was checked by Kolmogorov–Smirnov test. Factor analysis, Kaiser–Meyer–Olkin (KMO) test was performed with a factor loading ≥ 0.4 to examine if the distribution of each nutrient variable for principal component analysis (PCA). PCA was performed and the data rotated using Varimax method. The screen plot with Eigen values ≥ 1.5 was used to determine the number of principal components. According to the nutrient patterns’ scores, participants were categorized into two groups, according to. An independent sample t test was used to compare characteristics of participants following the nutrient patterns. To compare quantitative variables, t student test and to compare qualitative variables, Chi-square test was used. Analysis of variance (ANOVA) was used to determine if there was a difference between the means of investigated variables across two groups of patterns. The association between the nutrient patterns with obesity and MetS were assessed by binary logistic regression adjusted for total calories intake (kcal) and age (year).
Results
Participants’ characteristics are demonstrated in Table 1. Accordingly, the mean age, weight, and BMI of the study participants were 36.49 years (SD ± 8.31), 78.97 kg (SD ± 10.77), and 30.31 kg/m2 (SD ± 3.62), respectively.
Four nutrient patterns were identified by factor analysis as demonstrated in Table 2. The KMO value was 0.841 indicating good sampling adequacy. These nutrient patterns were, respectively, loaded with; pattern 1 (thiamin, iron, carbohydrate, zinc, niacin, protein, magnesium, phosphorus, riboflavin), pattern 2 (PUFAs, MUFA, vitamin E, trans fatty acids), pattern 3 (beta-carotene, vitamin K, vitamin A, vitamin C) and pattern 4, (vitamin D, calcium). In total, these four nutrient patterns accounted for 84.75% of the variance.
The association between the general characteristics of participants and quintiles of nutrient intake patterns is shown in Table 3. The results obtained from the Chi-square test demonstrated a statistically significant difference between pattern 4 and education status (P = 0.02), and also pattern 2 and housing status (P = 0.01).
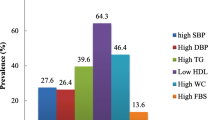
Table 4 and Supplementary Table represent dietary and nutrient intakes across quintiles of nutrient patterns’ scores. Moreover, Table 5, shows the general characteristics of the study population and also obesity and MetS components such as biochemical, anthropometric, and body composition measurements across the quintiles of identified nutrient patterns. A statistically significant association was found for weight (P = 0.01), fat-free mass (P = 0.01), waist circumference (P = 0.04), insulin (P = 0.02), and HOMA index (P = 0.05) across the quintiles of pattern 1. Additionally, body fat mass was marginally associated with the first pattern (P = 0.07). In the quintiles of pattern 2, only the waist-hip ratio showed a significant association (P = 0.01). Moreover, weight (P = 0.05) and triglyceride (P = 0.01) showed a correlation with the third pattern. Finally, there was a marginal but not significant association between BMI (P = 0.07) and pattern 3. This was the same for age (P = 0.07) and systolic blood pressure (P = 0.06) with pattern 4.
Odds of obesity and MetS with different nutrient patterns in two crude and adjusted models are presented in odds ratios (OR) and 95% confidence intervals (CI) (Table 6). Logistic regression analysis for the relationship between general obesity and MetS and the above-mentioned nutrient patterns showed that pattern 3 is associated with a 1.40 fold increased odds of obesity (OR 1.40; 95% CI 1.09–1.8; P = 0.01) and after adjusting for total energy intake and age, this association remained statistically significant (OR 1.32; 95% CI 1.03–1.7; P = 0.03). Regarding MetS, there was no association in both crude and adjusted models.
Discussion
One of the beneficial ways for assessing the general quality of diet and its correlation with obesity indicators and MetS is the analysis of nutrient patterns. Therefore, this study was conducted to investigate the relationship of the diverse patterns of nutrient intake with obesity and MetS. Regarding the energy-adjusted intake of 19 nutrients, four nutrient patterns were extracted. A significant and positive association was found between adherence to the third nutrient pattern rich in beta-carotene, vitamin K, vitamin A, and vitamin C and odds of general obesity in the target population.
Nutrient patterns with the base of vegetables are associated with a lower risk of overweight and obesity [13, 20]. Previous studies showed that nutrients from plant food and vegetable sources such as fiber, vitamin C, beta-carotene, and folate are associated with less weight gain while protein, riboflavin, phosphorus, and calcium are associated with overweight and obesity [21]. However, nutrient patterns with the base of the high amount of fat and carbohydrate are related to a higher risk of overweight and obesity [22]. Moreover, dietary patterns with a high amount of vegetables, fruits, fish, dietary fiber, potassium, and vitamin are associated with reduced prevalence of MetS, high blood pressure, high serum TG, and low HDL cholesterol levels [23, 24].
Although numerous studies have focused on dietary patterns and the prevalence of non-communicable diseases, there is not enough data to show if nutrient patterns have any significant association with the risk of chronic disorders [10, 25, 26]. It is worth bearing in mind that the assessment of nutrient patterns rather than dietary patterns has significant advantages. First, they are universal and, second their structures are not affected by special traditional behavior such as food preparation. Besides, the evaluation of different nutrient patterns in various sectors of the world may bring about new perceptions into the correlation of nutrient patterns with common disorders across various geographic provinces [12, 27].
The markers of obesity and MetS characteristics were assessed across quintiles of each four nutrient patterns, separately to find the possible association between these patterns and study variables. Those with a greater adherence to the third pattern indicating a higher quartile had a higher correlation with TG concentration. Furthermore, the second pattern rich in PUFAs, MUFA, vitamin E, and trans fatty acids was positively related to the waist-hip ratio. In addition, it was found that the first nutrient pattern which was positively correlated with the intake of thiamin, iron, carbohydrate, zinc, niacin, protein, magnesium, phosphorus, and riboflavin was positively related to weight, fat-free mass, and waist circumference. Remarkably, the individuals who were in higher quintiles of this pattern had higher obesity indicators, such as weight, fat-free mass, and waist circumference. Previous studies showed that vitamin B and its synergistic effect play a significant role in fat synthesis. This pattern has a higher amount of both vitamin B1 and B2 as well as overloaded carbohydrates. These vitamins are tightly related to the synthesis of fat from carbohydrates and protein [28] and along with other types of vitamin B (B6 and B5) might result in a significant increase in body fat as was reported in a study on rats [29]. A previous animal study found that niacin may contribute to a greater daily feed intake, weight gain, and the percentage of abdominal fat [30]. Overall, a nutrient pattern with excess vitamins, specifically vitamin B which shows a synergist effect with other nutrients can be a major factor leading to the development of obesity and epigenetic changes.
The third nutrient pattern rich in beta-carotene, vitamin K, vitamin A, and vitamin C is related to a higher intake of vegetables, starchy vegetables, legumes, poultry, and grain. The research by Monica L et al. showed that numerous vegetables were reversely related to weight. However, a greater intake of starchy vegetables, including peas, potatoes, and corn with a positive association could be linked to weight gain which was in line with our study findings. It can be explained by the fact that despite having nutritional content, they also have a lower carbohydrate quality and a higher glycemic load (GL) which can result in weight change [31]. In addition, it was suggested that a higher intake of non-starchy vegetables and fruit can be related to obesity change [32]. This association might be due to particular components, such as the fiber of vegetables which prevent fat mass gain [33].
Indeed, it is suggested that higher consumption of fruit may result in weight control but the present study showed that patterns with a higher intake of vitamin C and fruits are positively associated with general obesity. Regarding this result, it was found that a higher intake of fruit had no association with obesity. Interestingly, there was no association with BMI even after adjusting for fruit intake [34]. This can be due to the fact that fruits and starchy vegetables also contain a remarkable amount of sugar and energy. On the other hand, the Iranian population mostly eats fruits at least two servings as snacks especially after dinner as well as vegetables particularly during dinner with mayonnaises sauce. This may explain our results with regard to their obesity-inducing effects.
Even though a converse connection between vitamin A [35] and vitamin K status [36] and obesity was observed in preceding studies, the presence of sugar in fruits or high GL carbohydrate in starchy vegetables in this nutrient pattern may have accounted for an obesity-inducing consequence. Therefore, this suggests that sugar in fruits or high GL carbohydrate in starchy vegetables may raise the odds of general obesity even along with other nutrients which are recognized as possible protective factors against obesity. In addition, a prospective cohort study on 133,468 Americans illustrated that a higher intake of starchy vegetables was correlated with weight gain [37]. Also, most grains in the Iranian diet have been refined and their amount is very small. Studies have shown that refined grains and starchy vegetables are associated with obesity. Although the combination of these nutrients (both protective and stimulating ones regarding obesity) makes it difficult to interpret our findings, it emerges this hypothesis that there are interactions between highly loaded nutrients (both obesity-inducing and protective). Nevertheless, extra researches are warranted.
Based on the possible synergic effects of nutrients in the pattern, it could be helpful to clinically advise the clients to consume a balanced amount of fruits and starchy vegetables. In this context, S Bian et al. extracted four nutrients patterns in their study. They demonstrated that the nutrient pattern with a greater amount of vitamin B groups is inversely related to MetS in Chines adults. Moreover, no association was found between other dietary nutrient patterns and MetS [38]. Additionally, SS Khayyatzadeh et al. showed that a pattern rich in copper, selenium, vitamin A, riboflavin, and vitamin B12 was related to higher odds of MetS in women [39]. Unlike our prediction to find the same association between obesity and nutrient pattern 3, no relationship was observed with MetS. This observation can be attributed to a higher amount of fibers, beta-carotene, and vitamin C which are known as protective factors against MetS.
The present study aimed to assess the association of the nutrient patterns with obesity and MetS components among overweight and obese Iranian women. In this study, we included only women to reduce the heterogeneity effect of gender regarding food groups which is reported as the most personal characteristic difference related to intake measurement errors (40).
There are some inevitable limitations that need to be mentioned while explaining our outcomes. First, based on the cross-sectional study inference on the time sequence of the relationships between the onset of MetS or obesity is not available. Second, since the nutrient intake was evaluated using an FFQ, there may be possible errors in these calculations. Finally, due to the specificity of nutrient patterns in the target population, the results may not be accurate to be generalized to other populations with different ethnicities. Calculating the subject’s nutrient intake may encounter some errors due to the lack of a complete Iranian food composition table. Hence, the USDA nutrient databank was alternatively used. However, it had no impact on the individual’s classifications based on nutrient intakes. Although we controlled several potential confounders, the effects of remaining confounders cannot be ignored and must be considered in any future research. Our study population was women, classified as being overweight or obese. Therefore, our results should not be extended to other populations, including men, children, or the elderly. Therefore, further studies in specific populations are a pragmatic avenue for further research.
What is already known on this subject?
Nutrient patterns have been related to an increased risk for chronic disease. Evidence to confirm a direct association between nutrient patterns and obesity is not well established yet.
What do we now know as a result of this study that we did not know before?
Individuals with a high intake of foods containing beta-carotene, vitamin K, vitamin A, and vitamin C in nutrient patterns may be associated with a higher risk of obesity. Through our cross-sectional study, we described a nutrient pattern that may be related to an increased risk for obesity. This can be useful for dieticians and nutrition consultants who face the challenges posed by the treatment and improvement of obesity in the long term.
Conclusion
In conclusion, we found that the nutrient patterns rich in beta-carotene, vitamin K, vitamin A, and vitamin C were associated with higher odds of general obesity while this correlation was not seen between MetS and adiposity with the other three patterns. Analysis of nutrient patterns may be useful to assess the overall diet and its association with obesity and also to set dietary guidelines or clinical advice for obesity and overweight prevention. These findings should be approved by future studies to identify any causal association between adherence to specific nutrient patterns and obesity.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Kelly T, Yang W, Chen C-S, Reynolds K, He J (2008) Global burden of obesity in 2005 and projections to 2030. Int J Obes 32:1431–1437. https://doi.org/10.1038/ijo.2008.102
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384:766–781. https://doi.org/10.1016/S0140-6736(14)60460-8
Phillips CM, Dillon C, Harrington JM, McCarthy VJ, Kearney PM, Fitzgerald AP, Perry IJ (2013) Defining metabolically healthy obesity: role of dietary and lifestyle factors. PLoS ONE 8:e76188. https://doi.org/10.1371/journal.pone.0076188
Barzin M, Hosseinpanah F, Motamedi MA, Shapoori P, Arian P, Daneshpour MA, Asghari G, Teymoornejad A, Eslamifar A, Khalili D (2016) Bariatric surgery for morbid obesity: Tehran Obesity Treatment Study (TOTS) rationale and study design. JMIR Res Protoc. https://doi.org/10.2196/resprot.5214
Alberti KGM, Zimmet P, Shaw J (2005) The metabolic syndrome—a new worldwide definition. Lancet 366:1059–1062. https://doi.org/10.1016/S0140-6736(05)67402-8
Rasaei N, Sajjadi SF, Mirzababaei A, Pooyan S, Rashidbeygi E, Yekaninejad MS, Imani H, Mirzaei K (2019) Association between Resting Metabolic Rate (RMR) Respiratory Quotient (RQ) and Dietary Energy Density (DED) in overweight and obese women. Prog Nutr 21:145–151
Rasaei N, Kashavarz SA, Yekaninejad MS, Mirzaei K (2019) The association between sarcopenic obesity (SO) and major dietary patterns in overweight and obese adult women. Diabetes Metab Syndr Clin Res Rev 13:2519–2524. https://doi.org/10.1016/j.dsx.2019.06.023
WCRF/AICR: World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Amer Inst for Cancer Research, 2007.
Jacobs DR Jr, Steffen LM (2003) Nutrients, foods, and dietary patterns as exposures in research: a framework for food synergy. Am J Clin Nutr 78:508S-513S. https://doi.org/10.1093/ajcn/78.3.508S
Gnagnarella P, Maisonneuve P, Bellomi M, Rampinelli C, Bertolotti R, Spaggiari L, Palli D, Veronesi G (2013) Nutrient intake and nutrient patterns and risk of lung cancer among heavy smokers: results from the COSMOS screening study with annual low-dose CT. Eur J Epidemiol 28:503–511. https://doi.org/10.1007/s10654-013-9803-1
Samieri C, Coupez VG, Lorrain S, Letenneur L, Allès B, Féart C, Paineau D, Barberger-Gateau P (2013) Nutrient patterns and risk of fracture in older subjects: results from the Three-City Study. Osteoporos Int 24:1295–1305
Freisling H, Fahey MT, Moskal A, Ocké MC, Ferrari P, Jenab M, Norat T, Naska A, Welch AA, Navarro C (2010) Region-specific nutrient intake patterns exhibit a geographical gradient within and between European countries. J Nutr 140:1280–1286. https://doi.org/10.3945/jn.110.121152
Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L, Keshteli AH, Feizi A, Feinle-Bisset C, Adibi P (2016) Nutrient patterns and their relation to general and abdominal obesity in Iranian adults: findings from the SEPAHAN study. Eur J Nutr 55:505–518. https://doi.org/10.1007/s00394-015-0867-4
Estruch R, Martinez-Gonzalez MA, Corella D, Basora-Gallisá J, Ruiz-Gutierrez V, Covas MI, Fiol M, Gómez-Gracia E, Lopez-Sabater MC, Escoda R (2009) Effects of dietary fibre intake on risk factors for cardiovascular disease in subjects at high risk. J Epidemiol Community Health 63:582–588. https://doi.org/10.1136/jech.2008.082214
TspBC A.: Body composition analyzer; BC-418. Instruction Manual, 2015.
Ekelund U, Sepp H, Brage S, Becker W, Jakes R, Hennings M, Wareham NJ (2006) Criterion-related validity of the last 7-day, short form of the International Physical Activity Questionnaire in Swedish adults. Public Health Nutr 9:258–265. https://doi.org/10.1079/PHN2005840
Barak F, Falahi E, Keshteli AH, Yazdannik A, Esmaillzadeh A (2015) Adherence to the dietary approaches to stop hypertension (DASH) diet in relation to obesity among Iranian female nurses. Public Health Nutr 18:705–712. https://doi.org/10.1017/S1368980014000822
Hearst C, First D (1995) Nutritionist IV: diet analysis. First DataBank, San Bruno
Mollahosseini M, Rahimi MH, Yekaninejad MS, Maghbooli Z, Mirzaei K (2019) Dietary patterns interact with chromosome 9p21 rs1333048 polymorphism on the risk of obesity and cardiovascular risk factors in apparently healthy Tehrani adults. Eur J Nutr. https://doi.org/10.1007/s00394-018-1872-1
Fulgoni VL, Dreher M, Davenport AJ (2013) Avocado consumption is associated with better diet quality and nutrient intake, and lower metabolic syndrome risk in US adults: results from the National Health and Nutrition Examination Survey (NHANES) 2001–2008. Nutr J 12:1. https://doi.org/10.1186/1475-2891-12-1
Freisling H, Pisa PT, Ferrari P, Byrnes G, Moskal A, Dahm CC, Vergnaud A-C, Boutron-Ruault M-C, Fagherazzi G, Cadeau C (2016) Main nutrient patterns are associated with prospective weight change in adults from 10 European countries. Eur J Nutr 55:2093–2104. https://doi.org/10.1007/s00394-015-1023-x
Mazidi M, Kengne AP (2017) Nutrient patterns and their relationship with general and central obesity in US adults. Eur J Clin Invest. https://doi.org/10.1111/eci.12745
Bahari T, Uemura H, Katsuura-Kamano S, Yamaguchi M, Nakamoto M, Miki K, Ishizu M, Arisawa K (2018) Nutrient-derived dietary patterns and their association with metabolic syndrome in a Japanese population. J Epidemiol 28:194–201. https://doi.org/10.2188/jea.JE20170010
Iwasaki Y, Arisawa K, Katsuura-Kamano S, Uemura H, Tsukamoto M, Kadomatsu Y, Okada R, Hishida A, Tanaka K, Hara M (2019) Associations of nutrient patterns with the prevalence of metabolic syndrome: results from the baseline data of the Japan multi-institutional collaborative cohort study. Nutrients 11:990. https://doi.org/10.3390/nu11050990
Kanis J, McCloskey E, Johansson H, Cooper C, Rizzoli R, Reginster J (2013) Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57. https://doi.org/10.1007/s00198-018-4704-5
Palli D, Russo A, Decarli A (2001) Dietary patterns, nutrient intake and gastric cancer in a high-risk area of Italy. Cancer Causes Control 12:163–172. https://doi.org/10.1023/A:1008970310963
Newby P, Tucker KL (2004) Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev 62:177–203. https://doi.org/10.1111/j.1753-4887.2004.tb00040.x
McHenry E, Gavin G (1938) The B vitamins and fat metabolism. 1. Effects of thiamine, riboflavin, and rice polish concentrate upon body fat. J Biol Chem 125:653–660. https://doi.org/10.1016/S0021-9258(18)73957-4
McHenry E, Gavin G (1941) The B vitamins and fat metabolism. 4. The synthesis of fat from protein. J Biol Chem 188:471–475
Jiang R, Zhao G, Chen J, Zheng M, Zhao J, Li P, Hu J, Wen J (2011) Effect of dietary supplemental nicotinic acid on growth performance, carcass characteristics and meat quality in three genotypes of chicken. J Anim Physiol Anim Nutr 95:137–145. https://doi.org/10.1111/j.1439-0396.2010.01031.x
Bertoia ML, Mukamal KJ, Cahill LE, Hou T, Ludwig DS, Mozaffarian D, Willett WC, Hu FB, Rimm EB (2015) Changes in intake of fruits and vegetables and weight change in United States men and women followed for up to 24 years: analysis from three prospective cohort studies. PLoS Med. https://doi.org/10.1371/journal.pmed.1001878
Phy JL, Pohlmeier AM, Cooper JA, Watkins P, Spallholz J, Harris KS, Berenson AB, Boylan M (2015) Low starch/low dairy diet results in successful treatment of obesity and co-morbidities linked to polycystic ovary syndrome (PCOS). J Obes Weight Loss Ther. https://doi.org/10.4172/2165-7904.1000259
Pereira MA, Ludwig DS (2001) Dietary fiber and body-weight regulation: observations and mechanisms. Pediatr Clin North Am 48:969–980. https://doi.org/10.1016/S0031-3955(05)70351-5
te Velde SJ, Twisk JW, Brug J (2007) Tracking of fruit and vegetable consumption from adolescence into adulthood and its longitudinal association with overweight. Br J Nutr 98:431–438. https://doi.org/10.1017/S0007114507721451
Jeyakumar SM, Vajreswari A (2015) Vitamin A as a key regulator of obesity & its associated disorders: evidences from an obese rat model. Indian J Med Res 141:275. https://doi.org/10.3746/pnf.2017.22.3.172
Shea MK, Booth SL, Gundberg CM, Peterson JW, Waddell C, Dawson-Hughes B, Saltzman E (2010) Adulthood obesity is positively associated with adipose tissue concentrations of vitamin K and inversely associated with circulating indicators of vitamin K status in men and women. J Nutr 140:1029–1034. https://doi.org/10.3945/jn.109.118380
Bertoia ML, Mukamal KJ, Cahill LE, Hou T, Ludwig DS, Mozaffarian D, Willett WC, Hu FB, Rimm EB (2015) Changes in intake of fruits and vegetables and weight change in United States men and women followed for up to 24 years: analysis from three prospective cohort studies. PLoS Med 12:e1001878. https://doi.org/10.1371/journal.pmed.1001956
Bian S, Gao Y, Zhang M, Wang X, Liu W, Zhang D, Huang G (2013) Dietary nutrient intake and metabolic syndrome risk in Chinese adults: a case–control study. Nutr J 12:106. https://doi.org/10.1186/1475-2891-12-106
Khayyatzadeh SS, Moohebati M, Mazidi M, Avan A, Tayefi M, Parizadeh SMR, Ebrahimi M, Heidari-Bakavoli A, Azarpazhooh MR, Esmaily H (2016) Nutrient patterns and their relationship to metabolic syndrome in Iranian adults. Eur J Clin Invest 46:840–852. https://doi.org/10.1111/eci.12666
Marks GC, Hughes MC, van der Pols JC (2006) Relative validity of food intake estimates using a food frequency questionnaire is associated with sex, age, and other personal characteristics. J Nutr 136:459–465. https://doi.org/10.1093/jn/136.2.459
Acknowledgements
The authors thank the directors of the school of Nutritional and Dietetics at Tehran University of medical sciences for allowing them to conduct a comparative cross-sectional study. This study was supported by grants (ID: 97-03-161-41144, 97-03-161-40081 and 97-02-161-38999) from the Tehran University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
LS conducted research; KhM and HY analyzed data; HY, LS, NR, SM and RE wrote the paper; KhM had primary responsibility for final content. NM revised the manuscript. KC revised and improve grammar. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All participants signed a written informed consent before taking part in the study. The study was approved by the ethics committee of the Tehran University of Medical Sciences with ethics number IR.TUMS.VCR.REC.1395.1597.
Informed consent
Participation was voluntary and anonymous and completing the survey was accepted as consent by the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yarizadeh, H., Setayesh, L., Majidi, N. et al. Nutrient patterns and their relation to obesity and metabolic syndrome in Iranian overweight and obese adult women. Eat Weight Disord 27, 1327–1337 (2022). https://doi.org/10.1007/s40519-021-01268-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01268-4