Abstract
Purpose
Although a significant proportion of type 2 diabetes mellitus (T2DM) cases arose from normal-weight individuals, studies on indicators of T2DM in normal-weight people are limited. Accordingly, this study aims to investigate the predictive value of obesity indices and triglyceride glucose-related parameters (TyG-related parameters) in T2DM among normal-weight Chinese elderly.
Methods
A total of 24,215 normal-weight Chinese elderly (age ≥ 60 years) [body mass index–BMI (18.5–23.9 kg/m2)] were included. Obesity indices and triglyceride glucose-related parameters (TyG-related parameters) included waist circumference (WC), waist-to-height ratio (WHtR), visceral adiposity index (VAI), lipid accumulation product (LAP), and TyG-related parameters (TyG, TyG-BMI, TyG-WC, and TyG-WHtR). Multivariate logistic regression analysis was performed to examine the associations between obesity- and TyG-related indices and T2DM. The areas under the curve (AUC) of the receiver-operating characteristic (ROC) curve analyses were used to evaluate and compare the predictive value of the different indices.
Results
The prevalence of T2DM was 14.2% in normal-weight individuals. Among the indices, TyG was significantly associated with T2DM among men and women, respectively, (adjusted odds ratio–aOR per SD 3.46; 95% CI 3.23–3.71) and (aOR per SD 3.64; 95% CI 3.43–3.86). Compared with other indices, TyG had the highest AUC value for T2DM in men (AUC: 0.818, 95% CI 0.810–0.825) and women (AUC: 0.824, 95% CI 0.814–0.833).
Conclusions
TyG is an effective marker and outperforms other indices when predicting T2DM in the normal-weight Chinese elderly population.
Level of evidence
Level V: Opinions of authorities, based on descriptive studies, narrative reviews, clinical experience, or reports of expert committees.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a well-established risk factor for type 2 diabetes mellitus (T2DM) [1, 2]. Despite obesity typically being defined in terms of Body Mass Index (BMI) is frequently, obese BMI may not reliably predict patients with excess adiposity when used in a clinical setting [3, 4]. As such, it is not uncommon to find T2DM among normal-weight individuals [5,6,7]. To date, the majority of research into potential predictive indicators of T2DM has been limited to only overweight and obese people [11]. Previous research has estimated that the prevalence of T2DM among normal-weight persons (BMI: 18.5–25 kg/m2) ranges from 15 to 30% [8,9,10], but T2DM may go undetected in these individuals due to their apparently healthy BMI [12]. It is therefore important that the research community is able to identify clinical markers to aid the diagnosis of T2DM in normal-weight individuals.
Several parameters have recently had their potential as indicators of insulin resistance (IR), T2DM and cardiovascular metabolic diseases identified [13,14,15,16,17]. For example, waist circumference (WC) and waist-to-height ratio (WHtR) are widely used for approximating the risk of T2DM [13, 14]. Visceral adiposity index (VAI) and lipid accumulation product (LAP) are used as novel markers of visceral fat in the prediction of metabolic syndrome (MetS), T2DM and arterial stiffness [15, 16]; and the triglyceride glucose-related parameters (TyG, TyG-BMI, TyG-WC, TyG-WHtR) have been identified as excellent surrogate markers for T2DM [17].
Previous studies have reported that differences in the ability of obesity indices and TyG-related parameters to predict T2DM were mainly due to ethnic and geographical variation [18, 19]. In spite of this, no study has assessed the effectiveness of these indices for the prediction of T2DM in the normal-weight Chinese population to date. Advanced age is an important risk factor for T2DM; individuals aged 60 years or older are considered to be at higher risk of having T2DM [20]. Hence, choosing appropriate indicators to predict the T2DM in normal-weight Chinese elderly is of great public health importance. In this study, we aimed to investigate the clinical utility of several surrogate markers for the prediction of T2DM in normal-weight Chinese older adults.
Materials and methods
Participants
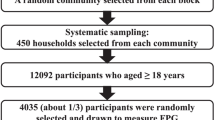
A total of 37,628 adults were recruited from a health screening program undertaken across six hospitals at the Center of Medical Examination from August to December 2019 in Shenzhen (i.e., Baoan Central Hospital, Baoan District Traditional Chinese Medicine Hospital, Fuyong People’s Hospital, Shajing Hospital, Shiyan Hospital and Songgang Hospital). Individuals who were aged ≥ 60 years and had provided informed consent were included. Exclusion criteria were: (1) did not fast for at least 8 h before the test; (2) corticosteroid use in the past 6 months; (3) refusal to participate in the study. A total of 13,413 individuals were excluded from the present analysis, including subjects with BMI < 18.5 kg/m2 (5588 individuals) and ≥ 24 kg/m2 (7825 individuals). The total number of participants included in the present analysis was 24,215.
Definitions
Normal weight was defined as a BMI of 18.5–23.9 kg/m2, according to the recommendations of the Working Group on Obesity of China (WGOC) [21].
Participants were placed into one of two groups, “with T2DM” and “without T2DM”. “With T2DM” was defined as: (1) FPG ≥ 7.0 mmol/L [22]; (2) previous diagnosis of T2DM; (3) using antidiabetic medications. Socio-demographic information, risk factors, and relevant medical records of participants were collected in the study. The participants were asked the following lifestyle questions: (1) smoking: “Have you smoked a cigarette, cigar or pipe of tobacco in the last 30 days?” (Yes/No); (2) drinking: “Have you had an alcoholic drink of any kind in the last 12 months?” (Yes/No); (3) intensity of physical activity: ‘‘Do you exercise regularly a week, low (e.g., walking, Tai Chi) or moderate (e.g., biking, jogging) or high (e.g. playing badminton, swimming)?” The obesity- and TyG-related indices were calculated using the following formula:
-
1) WHtR = WC/Height [23].
-
With WC in cm, Height in cm.
-
2) VAI (Men) = [WC/39.68 + (1.88 × BMI)] × (TG/1.03) × (1.31/HDL-C) [24].
-
VAI (Women) = [WC/36.58 + (1.89 × BMI)] × (TG/0.81) × (1.52/HDL-C) [24].
-
With WC in cm, BMI in kg/m2, TG and HDL-C both in mmol/L.
-
3) LAP (Men) = [WC-65] × TG [25].
-
LAP (Women) = [WC-58] × TG [25].
-
With WC in cm and TG in mmol/L.
-
4) TyG = Ln [(TG × FPG)/2] [26]. With TG and FPG both in mg/dL.
-
5) TyG-BMI = TyG × BMI. TyG-WC = TyG × WC. TyG-WHtR = TyG × WHtR [17].
Anthropometric and Laboratory Measurement
Bodyweight (kg) and height (cm) were measured without hats and shoes. BMI (kg/m2) was calculated as weight (kg) divided by the square of height (m) [12]. WC (cm) was measured using non-elastic tape at the umbilical level at the end of normal expiration. Blood pressure (mmHg) was measured with a standardized mercury sphygmomanometer on the same arm three times after a resting period of at least 5 min. The average of the three measurements was recorded. Venous blood samples were collected after the participants had fasted for at least 8 h. Participants were asked to refrain from caffeine, alcohol, smoking, and strenuous activities for 8 h prior to blood collection. Plasma levels of fasting plasma glucose (FPG), triglyceride (TG), total cholesterol (TC), low-density lipid cholesterol (LDL-C) and high-density lipid cholesterol (HDL-C) were analyzed with an automated biochemical analyzer.
Statistical Analysis
Data analyses were performed with IBM SPSS Statistics, version 25 (IBM Corporation, Armonk, NY, USA) and MedCalc Statistical Software version 19.2 (MedCalc Software BVBA, Ostend, Belgium). Categorical variables were expressed in terms of frequency and percentage. Chi-squared tests were used to compare categorical variables between groups. Continuous variables were expressed as mean ± standard deviation (SD). Independent samples t-test was used to compare the difference between groups in continuous variables. Given the sexual dimorphism of body composition, multivariate logistic regression analysis and receiver-operating characteristic (ROC) curve analyses were presented stratified by sex. For binary logistic regression analysis, WC, WHtR,VAI,LAP, TyG, TyG-BMI, TyG-WC and TyG-WHtR were regarded as continuous variables, and odds ratios (OR) and 95% confident interval (95% CI) were calculated for a 1-SD increase of these parameters. The diagnostic value for T2DM was defined by area under the curve (AUC) in ROC curve analyses. The cut-off point was selected according to Youden index (sensitivity + specificity -1). All significance tests were two-tailed and p values less than 0.05 were considered statistically significant.
Results
Demographic and Clinical Characteristics of Participants
Subject characteristics are shown in Table 1. Of the 24,215 participants, 10,661 (44.02%) were men and 13,554 (55.98%) were women. The mean age was 71 years, and the prevalence of T2DM was 14.2%. Subjects with T2DM showed higher obesity indices and TyG-related parameters than those without T2DM (p < 0.05).
Associations of Indicators with T2DM risk
Two separate multivariate logistic regression models were fitted for each of the indicator variables, stratified by sex, to calculate the OR per SD with 95% CI for T2DM. After adjusting the factors of age, smoking, drinking and intensity of physical activity, the results showed an increased adjusted OR (aOR) for T2DM for WC, WHtR, VAI, LAP, TyG,TyG-BMI, TyG-WC and TyG-WHtR (See Table 2). In men, TyG had the highest aOR per SD for T2DM at 3.46 (95% CI 3.23–3.71), followed by TyG-WHtR (aOR per SD 3.11, 95% CI 2.89–3.33), TyG-WC (aOR per SD 2.86, 95% CI 2.68–3.05), TyG-BMI (aOR per SD 2.78, 95% CI 2.61–2.97), VAI (aOR per SD 1.39, 95% CI 1.31–1.49), LAP (aOR per SD 1.37, 95% CI 1.31–1.44), WHtR(aOR per SD 1.35, 95% CI 1.26–1.44) and WC (aOR per SD1.31, 95% CI 1.25–1.38). In women, the aOR per SD for T2DM was highest for TyG at 3.64 (95% CI 3.43–3.86), followed by TyG-BMI (aOR per SD 2.89, 95% CI 2.73–3.05), TyG-WC (aOR per SD 2.75, 95% CI 2.60–2.90), TyG-WHtR (aOR per SD 2.67, 95% CI 2.53–2.81), VAI (aOR per SD 1.42, 95% CI 1.33–1.52), LAP (aOR per SD 1.39, 95% CI 1.33–1.44), WHtR (aOR per SD 1.24, 95% CI 1.18–1.30) and WC (aOR per SD 1.19, 95% CI 1.15–1.24).
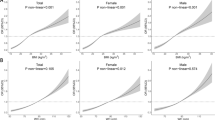
The Predictive value of Each Index for T2DM
The results of the ROC curve analyses for each index are shown in Table 3 and Fig. 1. The largest AUC observed in men corresponded to TyG (AUC: 0.818, 95% CI 0.810–0.825), followed by TyG-WC (AUC: 0.771, 95% CI 0.763–0.779) and TyG-WHtR (AUC: 0.768, 95% CI 0.760–0.776). The predictive values between the WC (AUC: 0.586, 95% CI 0.570–0.602) and WHtR (AUC: 0.571, 95% CI 0.555–0.587) were similar. In women, the AUC was largest for TyG (AUC: 0.824, 95% CI 0.814–0.833), followed by TyG-WC (AUC: 0.766, 95% CI 0.755–0.777). TyG-BMI and TyG-WHtR showed similar predictive ability (AUC: 0.760) when predicting the prevalence of T2DM in normal-weight Chinese older adults. In Table 3, when predicting T2DM, TyG had the highest sensitivity (men 76.09%, women 73.87%), specificity (men 72.38%, women 75.90%) and Youden index (men 0.48, women 0.50) in both sexes. We also compare the differences in the AUC of these indicators, the Table 4 showed that the AUC for TyG was significantly different from the AUC of other markers for both sexes.
ROC curves for each indices as predictors of T2DM in men and women. a Man and b Women. WC Waist Circumference, WHtR Waist Height-Ratio, VAI Visceral Adiposity Index, LAP Lipid Accumulation Product, TyG Triglyceride Glucose, TyG-BMI TyG related to BMI, TyG-WC TyG related to WC, TyG-WHtR TyG related to WHtR
Discussion
In this study, we compared the ability of obesity indices and TyG-related parameters to predict T2DM in Chinese elderly with normal weight. Our results showed that TyG performed most favorably with the highest OR and largest AUC, suggesting that TyG could be an effective marker to predict T2DM in older adults with normal weight. In addition, our results suggested that the optimal cut-off points for predicting T2DM using WC and WHtR in Chinese older adults with normal weight were WC ≥ 84.3 cm and WHtR ≥ 0.49 for men, and WC ≥ 79.8 cm and WHtR ≥ 0.52 for women.
According to the World Health Organization (WHO), a BMI of 18.5–23 kg/m2 is considered to correspond to a normal weight for Asian populations. Nevertheless, compared with European populations, Asian populations have a higher risk of T2DM even when BMI is less than 23.0 kg/m2 [27]. This suggests that even modest weight gain may lead to IR and significantly increase the risk of diabetes for East Asian people. Correspondingly, and due to differences in culture and lifestyle, the risk of T2DM among the normal weight (BMI: 18.5–23.9 kg/m2) population of China is higher than the risk found in many other countries [9]. Since the symptoms of T2DM may be overlooked or mistaken as symptoms of other conditions in older adults, efficacious indicators that can predict T2DM in normal-weight Chinese elderly are urgently required.
Previous studies have found that shorter individuals may have a higher risk for metabolic disorders than taller individuals, even for people with the same WC [28]. A meta-analysis reported that, compared to BMI and WC, WHtR was a superior tool for predicting diabetes [29], dyslipidemia, hypertension, and cardiovascular disease (CVD). Our study revealed that WHtR was more strongly positively associated with T2DM than WC among the normal-weight older Chinese population. The AUC values as determined by ROC curves showed that WC and WHtR had poorer diagnostic utility than LAP, VAI, and TyG-related indices. This finding suggested that the inclusion of these biochemical predictors increased the power to diagnose T2DM, as opposed to the use of the anthropometric parameters alone. The questions of where the appropriate WC and WHtR thresholds lie for the prediction of T2DM among Chinese adults are still points of contention. Currently, the recommended thresholds for overweight and abdominal obesity in China are WC ≥ 85 cm and 90 cm for males, and WC ≥ 80 cm and 85 cm for females [21]. Our observed cut-off values of WC for normal-weight people were lower than these recommendations. This result suggested that an initial measurement of WC at the routinely health check was helpful to prevent T2DM in the elderly with normal weight. Intriguingly, we found that WHtR was more sensitive (70.80%) than WC (50.22%) in men, despite WHtR having the lowest AUC (0.571 for men). This finding implies that WHtR may have a better predictive ability than WC and may therefore be used to screen for T2DM. According to previous reports, a WHtR ≥ 0.5 may be the best cut-point value for diagnosing T2DM [30]. Accordingly, a study of 996 older adults in China by Yang et al.[31] found that optimal WHtR cut-offs for the detection of T2DM were 0.512 for men and 0.514 for women. In contrast, we calculated optimal cutoffs of 0.49 for males and 0.52 for females. Our results suggest that a lower cut-off point of WHtR may be more appropriate for elderly Chinese men with normal weight than that which is appropriate for other populations, though care should be exercised when interpreting these findings since our sample was exclusively collected from Shenzhen–a single large city in southern China.
As a clinical marker of abdominal fat function, VAI was used to predict the risk of cardiometabolic disease in healthy individuals [32]. Our study showed that the OR of VAI was 1.39 per SD (95% CI 1.31–1.49) in men, and 1.42 per SD (95% CI 1.33–1.52) in women. One past study reported that Chinese VAI (CVAI) had a significant advantage over BMI and WC measurements in T2DM detection [33]. In contrast, Mohammadreza B et al. [34] found that, compared to BMI and WC, VAI was not a suitable index to predict T2DM. In our study, VAI was not an appropriate surrogate marker for identifying T2DM (AUC: 0.620, 0.625, sensitivity: 48.55% and 60.29% for men and women, respectively) in normal-weight older adults and the indicator had a lower relative discriminatory ability compared to TyG-related parameters. LAP is considered a better predictor of T2DM when compared to anthropometric indicators. Previous work in settings as varied as Germany [15], Japan [35] and Iran [36] has found that LAP is a good predictor of T2DM. Yet, one cohort study indicated that a high LAP index did not predict the development of T2DM in Indonesian women, despite being associated with a higher diagnostic risk of T2DM [37]. We found that LAP and VAI had similar low AUC values, which means that these indicators may not be effective surrogate markers for identifying T2DM in the normal-weight older adults in China.
A national Chinese prospective cohort study found that IR was more strongly associated with diabetic events than β-cell dysfunction in adults [38], suggesting that IR may be a vital indicator for predicting the development of T2DM in Chinese people. Recently, TyG-related parameters including TyG, TyG-BMI, TyG-WC and TyG-WHtR have become promising alternative biomarkers for IR due to their convenience and low cost of measurement [17]. Prior evidence regarding the relationship between TyG and T2DM in normal-weight individuals is limited, but S–H Lee et al. [39], Zhang et al. [40] and our research share similar findings. S–H Lee et al. found that TyG was a useful indicator of high risk of metabolic diseases among normal-weight individuals [39], while the findings of Zhang et al. imply that a high baseline TyG is associated with the development of T2DM, regardless of obesity status [40]. Indeed, our study found that TyG was more effective than other markers. Previous research has demonstrated that TyG has a strong predictive ability for IR [41, 42]. In fact, TyG appears to have a better predictive performance of IR than homeostatic model assessment (HOMA) in the Brazilian population [43]. The mechanism that accounts for the association between TyG and T2DM is yet to be revealed but several studies have provided clues. One clue exists in the observation that hepatic gluconeogenesis is promoted by glycerol and fatty acids, both products of TG lipolysis [44, 45]. Increased TG in islets can interfere with glucose metabolism, resulting in β-cell dysfunction and IR [46]. It is also hypothesized that, in being a composite measure of TG and FBG, TyG could reflect dual dimensions of IR. FBG primarily reflects liver IR, while fasting TG mainly reflects fat cell IR [47, 48]. Since the main pathophysiological basis of T2DM is IR[38], this may explain the high predictive power of TyG in people with T2DM. Given the limited data at the HOMA-IR level, this remains a hypothesised mechanism; consequently further studies are needed.
When compared to other indices, we found that the TyG most accurately predicted T2DM in both males (aOR per SD 3.46, 95% CI 3.23–3.71) and females (aOR per SD 3.64, 95% CI 3.43–3.86). Our study shows that all TyG-related parameters are predictive of individuals with T2DM (AUC > 0.5) in our sample. TyG had the highest AUC value (0.818, 0.824 males and females, respectively) and Youden index (0.48, 0.50, males and females, respectively), suggesting that TyG was most strongly associated with T2DM risk in normal-weight Chinese elderly when compared with other markers. Moreover, Table 4 showed the AUC of TyG differs significantly from the AUC of other markers, meaning that TyG may have clinical significance in identifying T2DM.
Past research has not arrived on a single optimal cut-off TyG value for the diagnosis of T2DM. In a cohort study within a European population, subjects with a TyG level of 8.31 or higher had an increased risk of T2DM [49]; Lee JW et al. [50] observed an optimal cut-off value of 8.52 in a Korean study. In our Chinese population, we found optimal TyG cut-off values of 7.17 and 7.40 for males and females, respectively. With the knowledge that mean TG concentrations vary by ethnic group, future research to assess the prediction of T2DM using TyG measurement is warranted in other populations.
That is not to say that TyG is consistently found to be predictive of T2DM, however. In an Iranian study, the inclusion of TyG in a T2DM predictive model did not improve the predictive power [19]. TyG-BMI and TyG-WC were significantly better than TyG in predicting T2DM risk in the Korean population [51], in broad agreement with research from Shanghai, China finding that TyG-WC was the best marker for identifying the risk of prediabetes and T2DM in a study of overweight adults [52]. The diverse nature of results to date suggests that additional studies concerning TyG-related parameters and T2DM should be conducted across a variety of different age groups and ethnicities.
Strengths and limits
Interpretation of our results requires one to consider the strengths and limitations of our study. We begin by listing the strengths. First, the study sample was drawn from participants of a general health screening program, a strength when compared to the bulk of previous research into indices predictive of T2DM, which has largely focused on overweight and obese populations. Accordingly, to date, no published research has compared the ability of obesity indices and TyG-related parameters to predict T2DM in the normal-weight Chinese elderly population. Second, FPG and TG play a key role in the development of T2DM in elderly people with normal weight. Third, we found that TyG was the preferred indicator of T2DM of the indices we investigated. TyG could prove crucial for the identification of T2DM in individuals who may otherwise be considered a low risk due to being of normal weight. Fourth, we found the optimal cut-off points of WC and WHtR for predicting T2DM, which could serve to improve clinical practices for determining the risk of T2DM in elderly people with normal weight. Taken as a whole, these findings have important implications for the primary prevention of T2DM in the elderly population. This study was not without limitations. Firstly, the sample consisted exclusively of individuals attending hospitals in Shenzhen and therefore it may not be representative of the wider Chinese elderly population. Secondly, the true rate of T2DM among the study subjects may have been higher than was estimated. This is due to no data being available regarding some biomarkers commonly used to diagnose T2DM, such as 2 h post-challenge plasma glucose and HbA1c. Finally, the findings of the present study may not be generalizable to all populations due to the ethnic and geographic characteristics of the study population.
What is already known on this subject?
Overweight and obesity are well-known risk factors for T2DM. However, even at lower body mass index (BMI), the Chinese population is at higher risk of T2DM when compared to other populations. Several obesity and TyG-related parameters such as BMI, WC, WHtR, LAP, VAI, TyG and TyG-BMI are used to predict IR, MetS and CVD, yet no previous study has assessed the effectiveness of these indices as predictors of T2DM in the Chinese elderly normal-weight population.
What this study adds?
TyG was most strongly associated with T2DM in normal-weight elderly adults in China. The optimum cut-off points of WC and WHtR were WC ≥ 84.3 cm and WHtR ≥ 0.49 for men and WC ≥ 79.8 cm and WHtR ≥ 0.52 for women when screening for T2DM in the Chinese normal-weight elderly population.
Conclusion
When compared to several other biomarkers, TyG was the best predictor of T2DM in Chinese normal-weight elderly people. We propose that TyG be used in clinical practice as a supplementary indicator for the prediction of T2DM in the elderly population, for example as part of routine health check-ups. In light of the heterogeneity of the predictive value of obesity indices and TyG-related parameters across different populations, further studies are warranted on the associations of these measures with the risk of T2DM.
References
Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, Hill JO, Brancati FL, Peters A, Wagenknecht L (2011) Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 34(7):1481–1486. https://doi.org/10.2337/dc10-2415
Chatterjee S, Khunti K, Davies MJ (2017) Type 2 diabetes. Lancet 389:2239–2251. https://doi.org/10.1016/S0140-6736(17)30058-2
Okorodudu DO, Jumean MF, Montori VM, Romero-Corral A, Somers VK, Erwin PJ, Lopez-Jimenez F (2005) Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int J Obesity 2010(34):791–799. https://doi.org/10.1038/ijo.2010.5
Gurevich KG, Poston WS, Anders B, Ivkina MA, Archangelskaya A, Jitnarin N, Starodubov VI (2017) Obesity prevalence and accuracy of BMI-defined obesity in Russian firefighters. Occup Med-Oxford 67:61–63. https://doi.org/10.1093/occmed/kqw136
Han SJ, Boyko EJ (2018) The evidence for an obesity paradox in type 2 -ellitus. Diabetes Metab J 42:179–187. https://doi.org/10.4093/dmj.2018.0055
Malone JI, Hansen BC (2019) Does obesity cause type 2 diabetes mellitus (T2DM)? Or is it the opposite? Pediatr Diabetes 20:5–9. https://doi.org/10.1111/pedi.12787
Thomas G, Khunti K, Curcin V, Molokhia M, Millett C, Majeed A, Paul S (2014) Obesity paradox in people newly diagnosed with type 2 diabetes with and without prior cardiovascular disease. Diabetes Obes Metab 16:317–325. https://doi.org/10.1111/dom.12217
Eckel N, Mühlenbruch K, Meidtner K et al (2015) Characterization of metabolically unhealthy normal-weight individuals: risk factors and their associations with type 2 diabetes. Metabolism 64:862–871. https://doi.org/10.1016/j.metabol.2015.03.009
Wang B, Zhang M, Wang S, Wang C, Wang J, Li L, Zhang L, Ren Y, Han C, Zhao Y et al (2018) Dynamic status of metabolically healthy overweight/obesity and metabolically unhealthy and normal weight and the risk of type 2 diabetes mellitus: a cohort study of a rural adult Chinese population. Obes Res Clin Pr 12:61–71. https://doi.org/10.1016/j.orcp.2017.10.005
Taylor R, Holman RR (2015) Normal weight individuals who develop type 2 diabetes: the personal fat threshold. Clin Sci 128:405–410. https://doi.org/10.1042/CS20140553
Abdullah A, Peeters A, de Courten M, Stoelwinder J (2010) The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Obes Res Clin Pr 89:309–319. https://doi.org/10.1016/j.diabres.2010.04.012
Claessen H, Brenner H, Drath C, Arndt V (2012) Repeated measures of body mass index and risk of health related outcomes. Eur J Epidemiol 27:215–224. https://doi.org/10.1007/s10654-012-9669-7
Siren R, Eriksson JG, Vanhanen H (2012) Waist circumference a good indicator of future risk for type 2 diabetes and cardiovascular disease. BMC Public Health 12:631. https://doi.org/10.1186/1471-2458-12-631
Elizalde-Barrera CI, Rubio-Guerra AF, Lozano-Nuevo JJ, Olvera-Gomez JL (2019) Triglycerides and waist to height ratio are more accurate than visceral adiposity and body adiposity index to predict impaired fasting glucose. Diabetes Res Clin Pr 153:49–54. https://doi.org/10.1016/j.diabres.2019.05.019
Ahn N, Baumeister SE, Amann U, Rathmann W, Peters A, Huth C, Thorand B, Meisinger C (2019) Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci Rep-UK 9:9693. https://doi.org/10.1038/s41598-019-46187-8
Dong L, Lin M, Wang W, Ma D, Chen Y, Su W, Chen Z, Wang S, Li X, Li Z et al (2020) Lipid accumulation product (LAP) was independently associated with obstructive sleep apnea in patients with type 2 diabetes mellitus. BMC Endocr Disord 20:179. https://doi.org/10.1186/s12902-020-00661-x
Lim J, Kim J, Koo SH, Kwon GC (2019) Comparison of triglyceride glucose index, and related parameters to predict insulin resistance in Korean adults: an analysis of the 2007–2010 Korean National Health and Nutrition Examination Survey. PLoS ONE 14:e0212963. https://doi.org/10.1371/journal.pone.0212963
Kavaric N, Klisic A, Ninic A (2018) Are visceral adiposity index and lipid accumulation product reliable indices for metabolic disturbances in patients with type 2 diabetes mellitus? J Clin Lab Anal 32(3):e22283. https://doi.org/10.1002/jcla.22283
Janghorbani M, Almasi SZ, Amini M (2015) The product of triglycerides and glucose in comparison with fasting plasma glucose did not improve diabetes prediction. Acta Diabetol 52:781–788. https://doi.org/10.1007/s00592-014-0709-5
Moreno G, Mangione CM (2013) Management of cardiovascular disease risk factors in older adults with type 2 diabetes mellitus: 2002–2012 literature review. J Am Geriatr Soc 61:2027–2037. https://doi.org/10.1111/jgs.12513
Zhou BF (2002) Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 15:83–96
Weng J, Ji L, Jia W, Lu J, Zhou Z, Zou D, Zhu D, Chen L, Chen L, Guo L et al (2016) Standards of care for type 2 diabetes in China. Diabetes-Metab Res 32:442–458. https://doi.org/10.1002/dmrr.2827
Hsieh SD, Yoshinaga H, Muto T (2003) Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes Relat Metab Disord 27:610–616. https://doi.org/10.1038/sj.ijo.0802259
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, Galluzzo A (2010) Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 33:920–922. https://doi.org/10.2337/dc09-1825
Kahn HS (2005) The “lipid accumulation product performs” better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disor 5:26. https://doi.org/10.1186/1471-2261-5-26
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F (2008) The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat D 6:299–304. https://doi.org/10.1089/met.2008.0034
WHO Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363:157–163. https://doi.org/10.1016/S0140-6736(03)15268-3
Hsieh SD, Yoshinaga H (1999) Do people with similar waist circumference share similar health risks irrespective of height? Tohoku J Exp Med 188:55–60. https://doi.org/10.1620/tjem.188.55
Ashwell M, Gunn P, Gibson S (2012) Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev 13:275–286. https://doi.org/10.1111/j.1467-789X.2011.00952.x
Song P, Li X, Bu Y, Ding S, Zhai D, Wang E, Yu Z (2019) Temporal trends in normal weight central obesity and its associations with cardiometabolic risk among Chinese adults. Sci Rep-UK 9:5411. https://doi.org/10.1038/s41598-019-41986-5
Yang J, Wang F, Wang J, Han X, Hu H, Yu C, Yuan J, Yao P, Miao X, Wei S et al (2018) Using different anthropometric indices to assess prediction ability of type 2 diabetes in elderly population: a 5 year prospective study. BMC Geriatr 18:218. https://doi.org/10.1186/s12877-018-0912-2
Dong H, Xu Y, Zhang X, Tian S (2017) Visceral adiposity index is strongly associated with hyperuricemia independently of metabolic health and obesity phenotypes. Sci Rep-UK 7:8822. https://doi.org/10.1038/s41598-017-09455-z
Wei J, Liu X, Xue H, Wang Y, Shi Z (2019) Comparisons of visceral adiposity index, body shape index, body mass index and waist circumference and their associations with diabetes mellitus in adults. Nutrients 11(7):1580. https://doi.org/10.3390/nu11071580
Bozorgmanesh M, Hadaegh F, Azizi F (2011) Predictive performance of the visceral adiposity index for a visceral adiposity-related risk: type 2 diabetes. Lipids Health Dis 10:88. https://doi.org/10.1186/1476-511X-10-88
Wakabayashi I, Daimon T (2014) A strong association between lipid accumulation product and diabetes mellitus in japanese women and men. J Atheroscler Thromb 21:282–288. https://doi.org/10.5551/jat.20628
Bozorgmanesh M, Hadaegh F, Azizi F (2010) Diabetes prediction, lipid accumulation product, and adiposity measures; 6-year follow-up: tehran lipid and glucose study. Lipids Health Dis 9:45. https://doi.org/10.1186/1476-511X-9-45
Nusrianto R, Ayundini G, Kristanti M, Astrella C, Amalina N, Muhadi Riyadina W, Tahapary DL, Soewondo P (2019) Visceral adiposity index and lipid accumulation product as a predictor of type 2 diabetes mellitus: the Bogor cohort study of non-communicable diseases risk factors. Diabetes Res Clin Pr 155:107798. https://doi.org/10.1016/j.diabres.2019.107798
Wang T, Lu J, Shi L, Chen G, Xu M, Xu Y, Su Q, Mu Y, Chen L, Hu R et al (2020) Association of insulin resistance and β-cell dysfunction with incident diabetes among adults in China: a nationwide, population-based, prospective cohort study. Lancet Diabetes Endo 8:115–124. https://doi.org/10.1016/S2213-8587(19)30425-5
Lee SH, Han K, Yang HK, Kim HS, Cho JH, Kwon HS, Park YM, Cha BY, Yoon KH (2015) A novel criterion for identifying metabolically obese but normal weight individuals using the product of triglycerides and glucose. Nutr Diabetes 5:e149. https://doi.org/10.1186/s12933-017-0514-x
Zhang M, Wang B, Liu Y, Sun X, Luo X, Wang C, Li L, Zhang L, Ren Y, Zhao Y et al (2017) Cumulative increased risk of incident type 2 diabetes mellitus with increasing triglyceride glucose index in normal-weight people: the Rural Chinese Cohort Study. Cardiovasc Diabetol 16:30. https://doi.org/10.1186/s12933-017-0514-x
Dikaiakou E, Vlachopapadopoulou EA, Paschou SA, Athanasouli F, Panagiotopoulos L, Kafetzi M, Fotinou A, Michalacos S (2020) Triglycerides-glucose (TyG) index is a sensitive marker of insulin resistance in Greek children and adolescents. Endocrine 70:58–64. https://doi.org/10.1007/s12020-020-02374-6
Fritz J, Bjørge T, Nagel G, Manjer J, Engeland A, Häggström C, Concin H, Teleka S, Tretli S, Gylling B, Lang A, Stattin P, Stocks T, Ulmer H (2020) The triglyceride-glucose index as a measure of insulin resistance and risk of obesity-related cancers. Int J Epidemiol 49:193–204. https://doi.org/10.1093/ije/dyz053
Vasques AC, Novaes FS, de Oliveira MS, Souza JR, Yamanaka A, Pareja JC, Tambascia MA, Saad MJ, Geloneze B (2011) TyG index performs better than HOMA in a Brazilian population: a hyperglycemic clamp validated study. Diabetes Res Clin Pr 93:e98–e100. https://doi.org/10.1016/j.diabres.2011.05.030
Perry RJ, Camporez JG, Kursawe R, Titchenell PM, Zhang D, Perry CJ, Jurczak MJ, Abudukadier A, Han MS, Zhang XM et al (2015) Hepatic acetyl CoA links adipose tissue inflammation to hepatic insulin resistance and type 2 diabetes. Cell 160:745–758. https://doi.org/10.1016/j.cell.2015.01.012
Samuel VT, Shulman GI (2016) The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. J Clin Invest 126:12–22. https://doi.org/10.1172/JCI77812
Unger RH (1995) Lipotoxicity in the pathogenesis of obesity-dependent NIDDM. Genet Clin Implic Diabetes 44:863–870. https://doi.org/10.2337/diab.44.8.863
Low S, Khoo KCJ, Irwan B, Sum CF, Subramaniam T, Lim SC, Wong TKM (2018) The role of triglyceride glucose index in development of Type 2 diabetes mellitus. Diabetes Res Clin Pr 143:43–49. https://doi.org/10.1016/j.diabres.2018.06.006
Taylor R (2013) Type 2 diabetes: etiology and reversibility. Diabetes Care 36:1047–1055. https://doi.org/10.2337/dc12-1805
González ND, Íñigo SL, Delgado JP, Montero FA, Martinez JA (2016) Triglyceride-glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: The Vascular-Metabolic CUN cohort. Prev Med 86:99–105. https://doi.org/10.1016/j.ypmed.2016.01.022
Lee JW, Lim NK, Park HY (2018) The product of fasting plasma glucose and triglycerides improves risk prediction of type 2 diabetes in middle-aged Koreans. BMC Endocr Disord 18:33. https://doi.org/10.1186/s12902-018-0259-x
Er LK, Wu S, Chou HH, Hsu LA, Teng MS, Sun YC, Ko YL (2016) Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals. PLoS ONE 11:e0149731. https://doi.org/10.1371/journal.pone.0149731
Zheng S, Shi S, Ren X, Han T, Li Y, Chen Y, Liu W, Hou PC, Hu Y (2016) Triglyceride glucose-waist circumference, a novel and effective predictor of diabetes in first-degree relatives of type 2 diabetes patients. cross-sectional and prospective cohort study. J Trans Med 14(1):260. https://doi.org/10.1186/s12967-016-1020-8
Acknowledgements
The authors are grateful to all subjects, Baoan Central Hospital, Baoan District Traditional Chinese Medicine Hospital, Fuyong People's Hospital, Shajing Hospital, Shiyan Hospital, and Songgang Hospital in the study.
Funding
ZXL was supported by the National Social Science Foundation of China (Grant No. 18ZDA085). HJ was supported by the Australian National Health Medical Research Council Project (GNT1141325) and Australian Research Council Discovery Project (DP200101781) grants. The funders had no role in study design, data collection, writing, or the decision to submit this manuscript.
Author information
Authors and Affiliations
Contributions
ZXL and HJ conceived of the study. MZX, JF, HBX, YG, CW, ZYD and XL were responsible for the collection and cleaning of the data, and assisted in the writing of the manuscript. KP and XW wrote the manuscript. WNF, QFT, YH, LRZ provided advice on methodology and contributed to the review and revision of the study. All authors read and approved the final manuscript. ZXL is the guarantor of this work. As such, ZXL had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in this study.
Ethical approval
The study was approved by the Ethics Committees of each of the six hospitals. No animal studies were described in the present article.
Informed consent
Informed consent was obtained from each participant enrolled in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ke, P., Wu, X., Xu, M. et al. Comparison of obesity indices and triglyceride glucose-related parameters to predict type 2 diabetes mellitus among normal-weight elderly in China. Eat Weight Disord 27, 1181–1191 (2022). https://doi.org/10.1007/s40519-021-01238-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01238-w