Abstract
Purpose
Patients with chemosensory dysfunction experience significant quality of life disruptions, including reduced enjoyment of eating. While chemosensory dysfunction has been associated with eating disorders, the relationship is poorly understood. This systematic review aims to characterize psychophysical gustation and olfaction in patients with eating disorders.
Methods
Systematic review of investigations assessing psychophysical chemosensory function in patients with organic eating disorders.
Results
26 studies were included. Five studies assessed both chemosenses, while 12 and 9 assessed exclusively gustation or olfaction, respectively. In total, 779 patients were included [72.4% anorexia nervosa (AN), 26.7% bulimia nervosa (BN), 0.8% combined AN/BN]. Patients with eating disorders experienced rates of hypogeusia up to 87% in AN and 84.6% in BN. There was evidence for alterations in psychophysical olfaction, but orientation of trends were less clear. Chemosensory dysfunction was more evident in AN patients. Treatment correlated with improved chemosensory function.
Conclusions
Despite heterogeneity in study methodology and results, this review demonstrates that patients with eating disorders experience some degree of chemosensory dysfunction, particularly in gustation. This symptomatology overlaps with those experienced by patients with other causes of chemosensory impairment. These findings suggest potential broad psychosocial, dietary, and mental health implications in patient populations experiencing chemosensory dysfunction.
Level of evidence
Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemosensory function affects many aspects of quality of life, including the ability to enjoy food and eating habits. It is also associated with serious health consequences including depression, generalized anxiety, and even frailty and mortality [1, 2]. Chemosensory dysfunction is incredibly common. Amongst the general population, approximately 1 in 4 people have complaints of smell disturbances while 1 in 5 people report disturbances in taste [3]. Though less is known about objective chemosensory dysfunction across the population, an estimated 20 million Americans exhibit objective evidence of chemosensory dysfunction [4]. As eating disorders are intimately linked with food intake and the experience of eating, it has been hypothesized that patients with eating disorders may also experience chemosensory dysfunction either contributing to the onset or maintenance of their disease process.
There is a mounting body of evidence describing abnormal physiologic and neurobiological responses to sensory stimuli in patients with eating disorders. Previous work has demonstrated that patients with anorexia nervosa (AN) salivate less than controls in response to olfactory stimuli, while patients with bulimia nervosa (BN) salivate more–these functional differences normalized after treatment [5]. Another group evaluated endocrine response to test meals and noted that patients with AN had decreased peak levels of blood glucose and insulin relative to controls [6]. Neurobiological alterations—both structural and functional—have also been demonstrated in patients with eating disorders. For instance, patients with AN have evidence of structural abnormalities including enlarged cortical sulci and ventricles and decreased volumes of gray and white matter [7]. In addition, dopamine signal is altered in AN, and serotonin signaling is dysregulated in both AN and BN [7, 8].
As clear alterations in physiologic response to food and sensory stimuli exist in AN, it has been hypothesized that these alterations may exist at the level of the perception of chemosensory stimuli in patients. As such, multiple investigations have assessed gustatory and olfactory function in patients with eating disorders. Though there is limited detail of disruptions in individual chemosensory functions in different eating disorders, there is cumulative evidence that some degree of impaired chemosensory function does exist in patients with eating disorders [9,10,11]. However, a comprehensive overview of chemosensory function—both olfaction and gustation—is still lacking, despite the intimate relationship between the often intertwined nature of olfaction and gustation. In an effort to better understand the role of chemosensory dysfunction in eating disorders and the potential role in other disease manifestations, this systematic review aims to characterize both psychophysical olfactory and gustatory function in patients with the two most common eating disorders, AN and BN.
Materials and methods
Literature source and search
A comprehensive literature review using five databases (PubMed, Cochrane Library, EMBASE, Web of Science and SCOPUS) was performed following Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [12]. The databases were searched for all available years—from the databases’ inception to the search date (May 3, 2019). Completed PRISMA guideline checklist is available as Online Resource 1. Records were obtained by a qualified data informationist. No additional records were identified following reference review. Search terms including “taste”, “gustation”, “smell”, “olfaction”, and “chemosensory” were combined with “feeding and eating disorders”, “anorexia”, and “bulimia”. Full search criteria can be reviewed in Online Resource 2. Records were imported and managed in Covidence (Veritas Health Innovation Ltd, Melbourne, Australia). Two authors independently reviewed articles. Disagreement on inclusion or exclusion was reached by consensus with senior author. Following abstract review, the remaining studies underwent full manual review. Studies were graded by quality in accordance with the Oxford Center for Evidence-based Medicine Criteria [13].
Inclusion and exclusion criteria
Inclusion and exclusion criteria are noted in Table 1. Studies assessing psychophysical gustatory and/or olfactory function with validated testing methods in adult or adolescent patients with AN or BN were included. Other eating disorders were excluded. Articles involving non-organic causes of eating disorders (e.g. anorexia cachexia, chemotherapy induced anorexia) were excluded. Articles focusing exclusively on hedonic response were excluded. Additional exclusion criteria included non-English language, subjective or non-validated measures of chemosensory function, research letters, abstracts, book chapters, and non-published studies.
Data extraction
Comprehensive study characteristics including patient population data, classification of eating disorder, and chemosensory testing methods and outcomes were recorded. For investigations studying outcomes after treatment or weight gain, both the pre-treatment and post-treatment testing outcomes were recorded. Risk of bias assessment was performed using the Methodological Index for Non-Randomized Studies (MINORS) as noted in Tables 2 and 3 [14]. MINORS criteria reported as scores from 0 to 24 for comparative studies and 0–16 for non-comparative studies, with higher score indicating lower risk of bias.
Results
Study characteristics
Literature review identified 6397 studies. After removal of 69 duplicates, 6328 underwent title and abstract screening. Full text was reviewed on 137 unique articles, and 26 met inclusion criteria (Fig. 1). Case–control studies comparing patients with eating disorders to healthy populations accounted for 25 of the included investigations (Tables 2, 3). The majority of studies assessing AN patients evaluated those diagnosed with restrictive (AN-R) and/or binge-eating/purge subtype (AN-B). AN-R is characterized by rapid weight loss through dieting, fasting, and excessive exercise, while AN-B is categorized by episodes of binge-eating and purging [15]. Five studies assessed both chemosenses, while 12 and 9 assessed exclusively gustation or olfaction, respectively. Mean MINORS score was 17.1/24 for comparative studies and 8.5/16 for non-comparative studies, suggesting at least a moderate risk of bias in this data.
Patient characteristics
In total, 779 patients were included (72.4% AN, 26.7% BN, 0.8% combined AN/BN), compared to 668 control patients. Mean patient age was 21.93 ± 6.67 years. Most studies utilized Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnostic criteria, with 6 studies (23.1%) using DSM-III, 11 (42.3%) using DSM-IV, and 2 (7.7%) using DMS-V [15]. Diagnostic criteria was not specified in four studies (15.4%). Three studies (11.5%) used alternate diagnostic criteria. The study population had a female predominance, with one included male patient with an eating disorder. Three studies included > 25% male healthy controls.
Gustation studies and evaluation methods
Gustation was evaluated in 375 patients (58.7% AN, 41.3% BN) across 14 studies, 13 of which were case–control design (Table 2). A wide variety of methodologies were utilized to assess gustatory identification or detection thresholds. Four studies utilized the commercially available taste strip kit for gustatory assessment [16,17,18,19], as previously validated by Mueller et al. [20] with published normative data available [21]. Two studies utilized filter disc paper [22, 23] based on Okuda et al. [24]. Five studies used a variety of non-validated measures with taste drops, sprays, or solutions to deliver varying concentrations of tastants [25,26,27,28,29]. Though the majority of studies evaluated participants with a combination of bitter, salty, sweet, and sour tastants, three studies utilized only sucrose for gustatory function assessment [30,31,32]. Further details on the gustatory testing methods are outlined in Table 2.
Gustation in patients with anorexia nervosa
Ten studies assessed gustation in 220 patients with AN, each demonstrating some element of impaired gustatory function in AN patients. Three studies demonstrated rates of hypogeusia ranging from 18 to 87% [16, 19, 23]. Impaired identification and threshold function were consistently reported in the majority of studies. Of seven studies assessing identification, 6 series reported decreased scores in patients with AN patients compared to controls [16, 18, 19, 23, 25, 26, 29]. All five studies evaluating threshold noted impaired function in AN versus controls in various tastants [16, 22, 26, 30, 32]. Perception of gustatory stimuli intensity was evaluated in two studies employing different methodologies with conflicting results [25, 29].
Gustation in patients with bulimia nervosa
Gustation was assessed in 155 BN patients across nine studies. In the setting of differing methodologies, overall gustatory function in BN patients varied with rates of hypogeusia ranging from 8.3 to 84.6% [17, 19, 23]. Five studies assessed gustatory identification [17,18,19, 23, 29], three studies assessed threshold [17, 27, 32], and three studies assessed intensity [28, 29, 31]. There were no clear trends in gustatory sensory measurements throughout the studies. Notably, BN patients had reduced scores in all four primary tastants when assessing the palate alone which was not seen on whole mouth testing, which authors hypothesized was related to damage to the palate from the purging behaviors [28]. There were no differences in bitter taste-receptor specific responses in patients with BN compared to controls [17, 28].
Effect of treatment and BMI on gustation
Multiple studies assessed effects of inpatient treatment, BMI, and weight gain with gustatory function. Three studies described improved gustatory scores for AN patients from admission to discharge for inpatient treatment, but gustation was still significantly poorer than healthy controls [19, 23, 26]. This improvement in gustatory scores was not seen in BN patients, but gustatory scores of these patients were not significantly lower than healthy controls at admission [19]. Another study assessed AN patient gustatory functionality at multiple points throughout hospitalization [22]. While AN patients initially demonstrated impairment compared to controls, the total gustatory scores were no longer different after one week of hospitalization [22].
The relationship between BMI and gustation was unclear. Of five studies evaluating BMI, three demonstrated an association between BMI and gustation [16, 19, 32]. However, two investigations failed to demonstrate a correlation [18, 29].
Olfaction studies and evaluation methods
Olfactory function was evaluated in 17 case–control studies (Table 3) which included 572 patients (79.9% AN, 18.9% BN, 1.2% combined AN/BN). Eleven studies utilized “Sniffin’ Sticks” for assessment of olfactory function [16,17,18,19, 25, 33,34,35,36,37,38]. Three studies utilized The University of Pennsylvania Smell Identification Test (UPSIT) [39,40,41]. Both the Sniffin’ Sticks and UPSIT tests are validated and commercially available. Three additional studies utilized odor solutions with various methods to assess olfactory measures [42,43,44]. Further details on the olfactory testing methods are outlined in Table 3.
Olfaction in patients with anorexia nervosa
Sixteen studies evaluated olfaction in 438 AN patients. Results were mixed on performance measures with the majority of studies noting no difference in olfaction between AN patients and controls. Prevalence of hyposmia in AN patients was directly reported three times, with a range from 0 to 44.4% [16, 18, 40].
Measures of the threshold [16, 18, 19, 33,34,35,36,37,38, 41,42,43,44], identification [16, 18, 19, 25, 33,34,35,36,37,38,39,40,41, 44], and discrimination [16, 18, 19, 33, 34, 36,37,38, 43] were examined in 13, 14, and nine studies, respectively, and composite TDI scores were reported in seven studies. For each measure there was evidence of superior, equivalent, or inferior function compared to healthy controls. In general, studies noted patients with AN performed better in odor threshold compared to controls, but patients with AN performed similarly or worse than controls in odor discrimination. Studies generally reported no difference in odor identification. Intensity scores were similar in all three studies where this was assessed [25, 38, 44]; meanwhile, one study demonstrated heightened sensitivity in AN patients versus controls [44].
Olfaction in patients with bulimia nervosa
Five studies assessed olfaction in 83 BN patients. Prevalence of hyposmia in BN patients was reported at 57.8% in one study, and rates of hyposmia were significantly higher than controls [18]. Overall, one study reported decreased olfactory function in multiple domains [18], but another study assessing detection threshold reported superior function in BN patients [42]. The remaining three studies reported no difference in various odor sensory domains [17, 19, 41].
Olfaction in combined patient populations
One investigation combined data for 20 patients with BN or eating disorder not otherwise specified (EDNOS) demonstrated increased thresholds in detection and discrimination compared to healthy controls [43]. Meanwhile, a study of 31 patients with BN and AN reported data collectively and demonstrated normosmia and no difference in UPSIT scores between patients and controls [39].
Effect of treatment and BMI on olfaction
Effects of treatment on olfactory function were assessed. In one study, AN-R patients—but not BN patients—demonstrated improved TDI scores after treatment, with post-treatment olfactory function similar to that of healthy controls [19]. Two studies did not note any significant improvement in olfactory scores for patients with eating disorders before or after treatment or weight gain [33, 43].
There were mixed results regarding BMI and olfactory performance, with three studies noting a positive correlation in at least one smell domain [16, 18, 34] and three studies noting no correlation [19, 33, 37]. Another study focusing on weight throughout their analysis found impairment in very low-weight anorexics in odor sensory domains with evidence for improvement after treatment [41]. Variance in olfactory scores at admission was affected by duration of illness (r = − 0.32, p < 0.01) in all ED patients and body weight at admission (r = − 0.50, p < 0.01) in AN-R groups. These effects were complicated by smoking status.
Discussion
There is a complex and ambiguous relationship between psychophysical chemosensory function and eating. Though it seems logical that disturbances in taste and smell would alter the experience of eating, there are few rigorous studies investigating chemosensory function in patients with eating disorders. This systematic review analyzed 26 studies assessing psychophysical gustatory and olfactory function in patients with organic AN and BN. Many investigations demonstrated some degree of chemosensory dysfunction compared to healthy controls, despite significant variation in methodology and conclusions. The findings of this current review suggest that patients with eating disorders most commonly exhibit gustatory dysfunction. This is most clearly identified in AN, in measures of gustatory identification and threshold. Meanwhile, despite less heterogeneity in olfactory testing methods, there is wide variation and lack of consistency in olfactory performance across the included studies, making clear trends in the relationship between eating disorders and olfaction difficult to concretely identify. Nonetheless, impairments in chemosensory function in patients with eating disorders has potentially significant implications both in understanding the pathogenesis and treatment of disease.
Despite these overarching themes, the significant variation in testing methods utilized contributed to conflicting data on overall chemosensory function in patients with eating disorders. It is known that psychophysical testing is generally more accurate than self-reported chemosensory function [45,46,47]. Previous studies have noted less than a third of people are able to predict their olfactory impairments [48], and self-reported questionnaires addressing gustatory dysfunction have low positive predictive value for each of the four primary tastants [49]. It is also likely that the validated, increasingly thorough metrics provide a more comprehensive picture of the chemosensory dysfunction present in patient populations. Notably, though previous studies have found good correlation between UPSIT and “Sniffin’ Sticks” results [50], studies solely using the UPSIT score to assess identification did not uncover differences between patients with eating disorder and controls, suggesting any olfactory dysfunction may be more highly pronounced in odor threshold or discrimination, as assessed in the “Sniffin’ Sticks” tests. In addition, recent data suggest low correlation between multiple gustatory function tests [51]. Therefore, impaired gustation in patients may be better detected by utilizing validated gustatory function tests, such as taste strips, over other methodologies solely assessing sweet tastants, for example. Future studies would benefit from using validated, commercially available tests such as the taste strips and “Sniffin’ Sticks” kits for gustatory and olfactory function assessment, respectively.
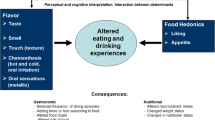
In addition to heterogenous methodologies, another confounding factor in many of these studies may be related to the interplay between gustatory and olfactory function in the larger experience of flavor. Though “taste” and “flavor” are often used interchangeably, they are influenced by different processes. The perception of flavor is related to gustation, trigeminal function, emotion, and both orthonasal and retronasal olfaction—highlighting the complex interplay between gustation and olfaction [52, 53]. Studies analyzing exclusively an isolated psychophysical chemosensory function (i.e. gustation or olfaction alone) likely do not accurately capture flavor perception and the experience of food, which may be uniquely altered in patients with eating disorders.
Although gustation and olfaction both contribute to the experience of eating, these two unique senses are also intimately linked, and patients may experience deficits in each chemosensory function. Previous studies have shown that gustatory and olfactory function are independent of each other in certain populations experiencing chemosensory dysfunction [54]. In this current report, five studies assessed both gustation and olfaction in the same population [16,17,18,19, 25]. Though these studies did not specifically address the relationship between gustation and olfaction, it does appear that this patient population experiences isolated dysfunction. This is in line with previous research suggesting the two forms of chemosensory dysfunction occur independently. However, future studies should consider assessing chemosensory function along with flavor assessments to better understand how these different chemosensory modalities may be related.
The etiology and manifestation of chemosensory dysfunction in patients with eating disorders is unknown. Multiple authors have hypothesized various etiologies for chemosensory deficits detected in patients. One hypothesis is related to decreased cell renewal in the olfactory epithelium secondary to long-term starvation in AN patients [33, 41], while others propose the olfactory microbiome may play a role [55]. On the contrary, research demonstrates that hunger (such as that experienced by patients with eating disorders) increases sensitivity to neutral odors, suggesting varying levels of satiety may affect olfactory testing and lead to varied results [56]. Meanwhile, the pathogenesis of gustatory dysfunction, may result from long-term purging affecting regional areas of the mouth and saliva composition [28, 57]. In addition, another hypothesis of the pathogenesis of chemosensory dysfunction is abnormalities in sensory processing pathways. Several authors have also explored the relationship between hedonics and functional magnetic resonance imaging (fMRI) in patients with eating disorders. Though not conclusive, there is evidence suggesting that neural processing may be disrupted in these patient populations [58].
It is also possible that BMI may affect chemosensory function. Though the distinction between BN versus AN is commonly thought of as behavioral (i.e. whether patients restrict or purge), it was traditionally made based on BMI, with a BMI < 18.5 defining AN in prior versions of the DSM criteria [15]. Considering AN and BN as two ends of a spectrum of eating disorders, it is unsurprising that these patients would display similar trends in chemosensory dysfunction, with more pronounced deficits in AN patients, given their more severe disease course and malnourishment. This also could explain differences in response to treatment: improvements in chemosensory function in response to treatment were more likely to be seen in AN patients over BN patients for both gustation and olfaction. Despite this, the relationship between BMI and chemosensory function was not definitively clear based on the studies in this current investigation.
The pathogenesis of chemosensory disturbances prompts an interesting question regarding the relationship of onset with development of the eating disorders. For individuals with impaired chemosensory function, dietary changes have been noted after onset of dysfunction, with almost a third of patients reporting decreased food intake [59]. The altered experience of eating may, therefore, promote disordered eating habits and lead to the development of more formalized eating disorders. On the other hand, the sequelae of eating disorders—such as purging or malnutrition—may contribute to chemosensory dysfunction. While intrinsic gustatory dysfunction may not have contributed to the onset of the disordered eating, it may consequently contribute to the maintenance of the behavior. Though this cause—effect relationship remains unclear, it may be elucidated in other populations with inherent chemosensory dysfunction.
In order to better understand the prevalence of chemosensory dysfunction in eating disorders, as well as the role it may play in the pathogenesis or maintenance of the disease, studies must use more rigorous, validated chemosensory assessments. It is well established that chemosensory dysfunction is associated with both environmental and safety hazards [60] and measures of patient frailty and mortality [2, 61, 62], highlighting the need to follow affected populations to minimize these risks. As self-report of chemosensory dysfunction in patients may not be entirely accurate [45, 46], psychophysical assessment is incredibly important to identify patients at risk for these complications. Furthermore, though not addressed in included studies, there is significant evidence that quality of life is similarly impaired in populations affected by chemosensory dysfunction [1, 63,64,65,66,67,68]. Specifically addressing and understanding quality of life impairments as they relate to chemosensory dysfunction is crucial in this population, as this has potential to further complicate the already challenging interplay of mood disorders in patients with eating disorders. Though chemosensory dysfunction has long been an overlooked area in patient care, the disease states and impacts on patient quality of life are significant. Patients with eating disorders would greatly benefit from more targeted studies to elucidate the relationship between their disease process and these known associated risks, and further direct care towards minimizing risks and treating associated complications.
This systematic review benefits from many strengths, including a comprehensive review of psychophysical chemosensory function in patients with common eating disorders, which in turn has potentially broad implications for other disease states. Nonetheless, heterogeneity in data collection and testing methods contributes to result heterogeneity and some conflicting data on overall chemosensory function in patients with eating disorders. Furthermore, while variation in patient populations is expected, studies frequently combined eating disorder patients into one group for analysis (e.g. AN-R and AN-B), thereby limiting conclusions on differences between subgroups of eating disorders. In addition, as the studies ranged across decades, the DSM criteria for diagnosis of AN and BN have changed, further contributing to heterogeneity. The wide range of testing methodologies also limits conclusions about the chemosensory function of patient with eating disorders. It is clear that future studies would benefit from using validated, commercially available tests to assess chemosensory function and a more detailed assessment of other relevant patient factors that may influence their chemosensory function.
Conclusion
Though this qualitative systematic review is limited in its conclusions secondary to the available data, there is nonetheless compelling evidence that patients with eating disorders have measurable differences in chemosensory function compared to healthy controls, particularly in gustatory function, which has potential for improvement with treatment. There is significant need for further research with standardized, validated, objective measures of chemosensory function in order to better understand pathogenesis of disease, impact on quality of life, and implications for patient outcomes. This relationship between chemosensory dysfunction and eating habits warrants further investigation in other populations with psychophysical chemosensory dysfunction.
What is already known on this subject?
There is a mounting body of evidence describing abnormal physiologic and neurobiological responses to sensory stimuli in patients with eating disorders, including altered hormonal and salivary responses as well as both structural and functional CNS differences. There is also cumulative evidence that some degree of impaired olfactory and gustatory function does exist, which may contribute to these patients’ altered responses to chemosensory stimuli. However, the extent of these deficits remains unknown, and a comprehensive overview of chemosensory dysfunction in these patients is still lacking, despite the intimate relationship between the often-intertwined nature of olfaction and gustation.
What your study adds?
There is compelling evidence that patients with eating disorders have measurable differences in chemosensory function—particularly gustatory function—compared to healthy controls, and treatment and weight gain may lead to normalization in chemosensory function. This current report identifies the need for further investigation of chemosensory function with standardized and validated assessments to better understand the pathogenesis of disease, impact on quality of life, and implications for patient outcomes. In particular, the association between chemosensory function and eating disorder-related outcomes should be explored. The measured association between chemosensory dysfunction and eating disorders raises many questions for other populations with psychophysical chemosensory dysfunction.
References
Merkonidis C, Grosse F, Ninh T et al (2015) Characteristics of chemosensory disorders—results from a survey. Eur Arch Oto-Rhino-Laryngol 272:1403–1416. https://doi.org/10.1007/s00405-014-3210-4
Bernstein IA, Roxbury CR, Lin SY, Rowan NR (2020) The association of frailty with olfactory and gustatory dysfunction in older adults: a nationally representative sample. Int Forum Allergy Rhinol. https://doi.org/10.1002/alr.22718
Rawal S, Hoffman HJ, Bainbridge KE et al (2016) Prevalence and risk factors of self-reported smell and taste alterations: Results from the 2011–2012 US national health and nutrition examination survey (NHANES). Chem Senses 41:69–76. https://doi.org/10.1093/chemse/bjv057
Liu G, Zong G, Doty RL, Sun Q (2016) Prevalence and risk factors of taste and smell impairment in a nationwide representative sample of the US population: a cross-sectional study. BMJ Open 6:8–11. https://doi.org/10.1136/bmjopen-2016-013246
LeGoff DB, Leichner P, Spigelman MN (1988) Salivary response to olfactory food stimuli in anorexics and bulimics. Appetite 11:15–25. https://doi.org/10.1016/S0195-6663(88)80018-7
Kinzig KP, Coughlin JW, Redgrave GW et al (2007) Insulin, glucose, and pancreatic polypeptide responses to a test meal in restricting type anorexia nervosa before and after weight restoration. Am J Physiol Endocrinol Metab 292:1441–1446. https://doi.org/10.1152/ajpendo.00347.2006
Phillipou A, Rossell SL, Castle DJ (2014) The neurobiology of anorexia nervosa: a systematic review. Aust N Z J Psychiatry 48:128–152. https://doi.org/10.1177/0004867413509693
Kaye W (2008) Neurobiology of anorexia and bulimia nervosa. Physiol Behav 94:121–135. https://doi.org/10.1016/j.physbeh.2007.11.037
Kinnaird E, Stewart C, Tchanturia K (2018) Taste sensitivity in anorexia nervosa: a systematic review. Int J Eat Disord 51:771–784. https://doi.org/10.1002/eat.22886
Chao AM, Roy A, Franks AT, Joseph PV (2020) A systematic review of taste differences among people with eating disorders. Biol Res Nurs 22:82–91. https://doi.org/10.1177/1099800419872824
Islam MA, Fagundo AB, Arcelus J et al (2015) Olfaction in eating disorders and abnormal eating behavior: a systematic review. Front Psychol. https://doi.org/10.3389/fpsyg.2015.01431
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. https://doi.org/10.1136/bmj.b2700
Howick J, Chalmers I, Glasziou P et al (2011) The Oxford 2011 levels of evidence. Oxford Cent Evidence Based Medicine. http://www.cebm.net/index.aspx?o=5653
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (Minors): Development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
American Psychiatric Association (2013) Feeding and eating disorders. In: Diagnostic and statistical manual of mental disorders, 5th edn (DSM-5). Arlington, Virginia
Fernández-Aranda F, Agüera Z, Fernández-García JC et al (2016) Smell–taste dysfunctions in extreme weight/eating conditions: analysis of hormonal and psychological interactions. Endocrine 51:256–267. https://doi.org/10.1007/s12020-015-0684-9
Weiland R, Macht M, Ellgring H et al (2011) Olfactory and gustatory sensitivity in adults with attention-deficit/hyperactivity disorder. ADHD Atten Deficit Hyperact Disord 3:53–60. https://doi.org/10.1007/s12402-010-0052-9
Dazzi F, De Nitto S, Zambetti G et al (2013) Alterations of the olfactory-gustatory functions in patients with eating disorders. Eur Eat Disord Rev 21:382–385. https://doi.org/10.1002/erv.2238
Aschenbrenner K, Scholze N, Joraschky P, Hummel T (2008) Gustatory and olfactory sensitivity in patients with anorexia and bulimia in the course of treatment. J Psychiatr Res 43:129–137. https://doi.org/10.1016/j.jpsychires.2008.03.003
Mueller C, Kallert S, Renner B et al (2003) Quantitative assessment of gustatory function in a clinical context using impregnated “taste strips.” Rhinology 41:2–6
Landis BN, Welge-Luessen A, Bramerson A et al (2009) “Taste Strips”—a rapid, lateralized, gustatory bedside identification test based on impregnated filter papers. J Neurol 256:242–248. https://doi.org/10.1007/s00415-009-0088-y
Nozoe SI, Masuda A, Naruo T et al (1996) Changes in taste responsiveness in patients with anorexia nervosa during behavior therapy. Physiol Behav 59:549–553. https://doi.org/10.1016/0031-9384(95)02105-1
Nakai Y, Kinoshita F, Koh T et al (1987) Taste function in patients with anorexia nervosa and bulimia nervosa. Int J Eat Disord 6:257–265. https://doi.org/10.1002/1098-108X(198703)6:2%3c257::AID-EAT2260060209%3e3.0.CO;2-X
Okuda Y (1980) The method of gustatory test by filter-paper disc (in Japanese with English summary). J Otolaryngol Jpn 83:1071–1082
Goldzak-Kunik G, Friedman R, Spitz M et al (2012) Intact sensory function in anorexia nervosa. Am J Clin Nutr 95:272–282. https://doi.org/10.3945/ajcn.111.020131
Casper RC, Kirschner B, Sandstead HH et al (1980) An evaluation of trace metals, vitamins, and taste function in anorexia nervosa. Am J Clin Nutr 33:1801–1808. https://doi.org/10.1093/ajcn/33.8.1801
Blazer T, Latzer Y, Nagler RM (2008) Salivary and gustatory alterations among bulimia nervosa patients. Eur J Clin Nutr 62:916–922. https://doi.org/10.1038/sj.ejcn.1602801
Rodin J, Bartoshuk L, Peterson C, Schank D (1990) Bulimia and taste: possible interactions. J Abnorm Psychol 99:32–39. https://doi.org/10.1037/0021-843X.99.1.32
Jirik-Babb P, Katz JL (1988) Impairment of taste perception in anorexia nervosa and bulimia. Int J Eat Disord 7:353–360. https://doi.org/10.1002/1098-108X(198805)7:3%3c353::AID-EAT2260070306%3e3.0.CO;2-Y
Lacey JH, Stanley PA, Crutchfield M, Crisp AH (1977) Sucrose sensitivity in anorexia nervosa. J Psychosom Res 21:17–21. https://doi.org/10.1016/0022-3999(77)90021-6
Franko DL, Wolfe BE, Jimerson DC (1994) Elevated sweet taste pleasantness ratings in bulimia nervosa. Physiol Behav 56:969–973. https://doi.org/10.1016/0031-9384(94)90331-X
Eiber R, Berlin I, De Brettes B et al (2002) Hedonic response to sucrose solutions and the fear of weight gain in patients with eating disorders. Psychiatry Res 113:173–180. https://doi.org/10.1016/S0165-1781(02)00232-9
Roessner V, Bleich S, Banaschewski T, Rothenberger A (2005) Olfactory deficits in anorexia nervosa. Eur Arch Psychiatry Clin Neurosci 255:6–9. https://doi.org/10.1007/s00406-004-0525-y
Tonacci A, Calderoni S, Billeci L et al (2019) Autistic traits impact on olfactory processing in adolescent girls with anorexia nervosa restricting type. Psychiatry Res 274:20–26. https://doi.org/10.1016/j.psychres.2019.02.026
Bentz M, Guldberg J, Vangkilde S et al (2017) Heightened olfactory sensitivity in young females with recent-onset anorexia nervosa and recovered individuals. PLoS ONE 12:1–17. https://doi.org/10.1371/journal.pone.0169183
Schecklmann M, Pfannstiel C, Fallgatter AJ et al (2012) Olfaction in child and adolescent anorexia nervosa. J Neural Transm 119:721–728. https://doi.org/10.1007/s00702-011-0752-0
Rapps N, Giel KE, Söhngen E et al (2010) Olfactory deficits in patients with anorexia nervosa. Eur Eat Disord Rev 18:385–389. https://doi.org/10.1002/erv.1010
Schreder T, Albrecht J, Kleemann AM et al (2008) Olfactory performance of patients with anorexia nervosa and healthy subjects in hunger and satiety. Rhinology 46:175–183
Kopala LC, Good KP, Honer WG (1994) Olfactory hallucinations and olfactory identification ability in patients with schizophrenia and other psychiatric disorders. Schizophr Res 12:205–211. https://doi.org/10.1016/0920-9964(94)90030-2
Kopala LC, Good K, Goldner EM, Birmingham CL (1995) Olfactory identification ability in anorexia nervosa. J Psychiatry Neurosci 20:283–286
Fedoroff IC, Stoner SA, Andersen AE et al (1995) Olfactory dysfunction in anorexia and bulimia nervosa. Int J Eat Disord 18:71–77. https://doi.org/10.1002/1098-108X(199507)18:1%3c71::AID-EAT2260180108%3e3.0.CO;2-5
Jiang T, Soussignan R, Carrier E, Royet JP (2019) Dysfunction of the mesolimbic circuit to food odors in women with anorexia and bulimia nervosa: a fMRI Study. Front Hum Neurosci 13:1–14. https://doi.org/10.3389/fnhum.2019.00117
Stein D, Gross-Isseroff R, Besserglick R et al (2012) Olfactory function and alternation learning in eating disorders. Eur Neuropsychopharmacol 22:615–624. https://doi.org/10.1016/j.euroneuro.2011.12.006
Lombion-Pouthier S, Vandel P, Nezelof S et al (2006) Odor perception in patients with mood disorders. J Affect Disord 90:187–191. https://doi.org/10.1016/j.jad.2005.11.012
Wrobel BB, Leopold DA (2004) Clinical assessment of patients with smell and taste disorders. Otolaryngol Clin North Am 37:1127–1142. https://doi.org/10.1016/j.otc.2004.06.010
Hummel T, Whitcroft KL, Andrews P et al (2017) Position paper on Olfactory dysfunction. Rhinol Suppl 54:1–30. https://doi.org/10.4193/Rhino16.248
Landis BN, Hummel T, Hugentobler M et al (2003) Ratings of overall Olfactory function. Chem Senses 28:691–694. https://doi.org/10.1093/chemse/bjg061
Philpott CM, Rimal D, Tassone P et al (2008) A study of olfactory testing in patients with rhinological pathology in the ENT clinic. Rhinology 46:34–39
Soter A, Kim J, Jackman A et al (2008) Accuracy of self-report in detecting taste dysfunction. Laryngoscope 118:611–617. https://doi.org/10.1097/MLG.0b013e318161e53a
Wolfensberger M, Schnieper I, Welge-Lussen A (2009) Sniffin’Sticks®: a new Olfactory test battery. Acta Otolaryngol 120:303–306. https://doi.org/10.1080/000164800750001134
Kang M-G, Choi J-H, Kho H-S (2020) Relationships between gustatory function tests. Oral Dis 26:830–837. https://doi.org/10.1111/odi.13291
Landis BN, Frasnelli J, Reden J et al (2005) Differences between orthonasal and retronasal olfactory functions in patients with loss of the sense of smell. Arch Otolaryngol - Head Neck Surg 131:977–981. https://doi.org/10.1001/archotol.131.11.977
Rozin P (1982) “Taste-smell confusions” and the duality of the olfactory sense. Percept Psychophys 31:397–401. https://doi.org/10.3758/BF03202667
Xie DX, Leland EM, Seal SM et al (2020) A systematic review and meta-analysis of taste dysfunction in chronic rhinosinusitis. Laryngoscope. https://doi.org/10.1002/lary.28827
Koskinen K, Reichert JL, Hoier S et al (2018) The nasal microbiome mirrors and potentially shapes olfactory function. Sci Rep 8:1–11. https://doi.org/10.1038/s41598-018-19438-3
Stafford LD, Welbeck K (2011) High hunger state increases olfactory sensitivity to neutral but not food odors. Chem Senses 36:189–198. https://doi.org/10.1093/chemse/bjq114
Arlt JM, Smutzer GS, Chen EY (2017) Taste assessment in normal weight and overweight individuals with co-occurring Binge Eating Disorder. Appetite 113:239–245. https://doi.org/10.1016/j.appet.2017.02.034
Kot E, Kucharska K, Monteleone AM, Monteleone P (2020) Structural and functional brain correlates of altered taste processing in anorexia nervosa: a systematic review. Eur Eat Disord Rev 28:122–140. https://doi.org/10.1002/erv.2713
Aschenbrenner K, Hummel C, Teszmer K et al (2008) The influence of Olfactory loss on dietary behaviors. Laryngoscope 118:135–144. https://doi.org/10.1097/MLG.0b013e318155a4b9
Hoffman HJ, Rawal S, Li CM, Duffy VB (2016) New chemosensory component in the U.S. National Health and Nutrition Examination Survey (NHANES): first-year results for measured olfactory dysfunction. Rev Endocr Metab Disord 17:221–240. https://doi.org/10.1007/s11154-016-9364-1
Pinto JM, Wroblewski KE, Kern DW et al (2014) Olfactory dysfunction predicts 5-year mortality in older adults. PLoS ONE 9:1–9. https://doi.org/10.1371/journal.pone.0107541
Gopinath B, Sue CM, Kifley A, Mitchell P (2012) The association between Olfactory impairment and total mortality in older adults. J Gerontol 67A:204–209. https://doi.org/10.1093/gerona/glr165
Hummel T, Nordin S (2004) Olfactory disorders and their consequences for quality of life. Acta Otolaryngol 125:116–121. https://doi.org/10.1080/00016480410022787
Miwa T, Furukawa M, Tsukatami T et al (2001) Impact of Olfactory impairment on quality of life and disability. Arch Otolaryngol Head Neck Surg 127:497–503. https://doi.org/10.1001/archotol.127.5.497
Brämerson A, Nordin S, Bende M (2007) Clinical experience with patients with olfactory complaints, and their quality of life. Acta Otolaryngol 127:167–174. https://doi.org/10.1080/00016480600801357
Smeets MAM, Veldhuizen MG, Galle S et al (2009) Sense of smell disorder and health-related quality of life sense of smell disorder and health-related quality of life. Rehabil Psychol 54:404–412. https://doi.org/10.1037/a0017502
Rowan NR, Soler ZM, Storck KA et al (2019) Impaired eating-related quality of life in chronic rhinosinusitis. Int Forum Allergy Rhinol 9:240–247. https://doi.org/10.1002/alr.22242
Kohli P, Soler ZM, Nguyen SA et al (2016) The association between olfaction and depression: a systematic review. Chem Senses 41:479–486. https://doi.org/10.1093/chemse/bjw061
Russell G (1979) Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med 9:429–448. https://doi.org/10.1017/S0033291700031974
Funding
This research did not receive any specific grant or other support from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Literature search was performed by SS. EL and DX performed literature review, data extraction, and data analysis. The first draft of the manuscript was written by EL. NR, SL, and VK critically revised the work. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Leland, E.M., Xie, D.X., Kamath, V. et al. Psychophysical chemosensory dysfunction in eating disorders: a qualitative systematic review. Eat Weight Disord 27, 429–447 (2022). https://doi.org/10.1007/s40519-021-01189-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01189-2