Abstract
Androgen Insensitivity Syndrome represents a disorder due to partial (PAIS), mild (MAIS) or complete (CAIS) resistance to androgens caused by X-linked mutations of androgen receptor gene. CAIS is characterized by a female phenotype and XY karyotype. Cases of patients with CAIS and associated obesity have been reported, while to date, there are no reports about the onset of an Eating Disorder (ED) in the carriers of this condition. We describe the case of a patient affected by CAIS and Anorexia Nervosa (AN) restricting type later shifted to Bulimia Nervosa (BN). A previous overweight was present since childhood, contributing to severe Body Dissatisfaction (BD) and consequent restrictive behaviour in adolescence. Beyond its peculiarity, this case highlights also the importance of diagnosing and monitoring the overweight and BD in CAIS patients to avoid the onset of an ED.
Level of Evidence: V, descriptive study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Androgen Insensitivity Syndrome (AIS) was initially known as "Morris Syndrome" from the name of the American gynecologist, John McLean Morris, who described it for first time in 1953 as "testicular feminisation" term no longer used [1].
AIS represents a spectrum of conditions characterized by resistance to androgens due to mutations involving the androgen receptor gene, situated in the Xq11–q12 region. The carriers of this mutation have a 46 XY karyotype with feminisation or under-masculinisation of external genitalia at birth, abnormal secondary sexual development in puberty, and infertility.
AIS is inherited in an X-linked manner.
According to the degree of androgen insensitivity, AIS is subdivided into three phenotypes:
-
Complete Androgen Insensitivity Syndrome (CAIS) with typical female external genitalia
-
Partial Androgen Insensitivity Syndrome (PAIS) with predominantly female, predominantly male, or ambiguous external genitalia
-
Mild Androgen Insensitivity Syndrome (MAIS) with typical male external genitalia.
CAIS is still considered a rare condition, with an estimated prevalence ranging from 2:100,000 to 5:100,000 [2] and from 1:20,400 to 1:99,100 [3] depending on the study.
Subjects with CAIS have a 46 XY karyotype but the complete resistance to androgen action, due to genetic mutations of the androgen receptor gene, leads to a female phenotype despite testosterone levels -within or above the male normal range [4]- produced by their abdominal undescended testes.
Normally, in presence of a 46 XY karyotype, the Sex-determining Region Y(SRY) gene situated in the Y chromosome will determine, in the embryo-fetal period, the development of functioning testes and absence of female internal genitalia. In CAIS, the complete resistance to androgens results in female external genitalia since testosterone and dihydrotestosterone produced by Leydig cells of testes will be transformed by aromatase into estrogen so resulting in development — between the 3rd week and 5th month of intrauterine development — of female sexual characteristics. Offspring will present therefore a feminine phenotype.
CAIS diagnosis is made either before puberty due to inguinal swellings resulting from ectopic testes or at puberty due to primary amenorrhea. Breasts and female adiposity develop normally and sparse or absent pubic or axillary hair is present. Sexual identity and orientation are typically female and heterosexual.
To prevent testicular malignancy, treatment of CAIS includes gonadectomy after puberty when feminilisation is complete or prepubertal gonadectomy associated to estrogen replacement therapy [5].
The gender identity, gender role and sexual orientation show a female pattern in CAIS individuals.
In fact, in CAIS, gender identity usually follows the sex of rearing, but quality of sexual life, sexual functioning and quality of life can be slightly compromised and these are important issues for keeping patients in psychological care [5]. Sexual functioning and sexual quality of life demonstrated less positive outcome in CAIS patients in comparison with normal women also in a previous report [6].
Gender reassignment is an unusual event in subjects with CAIS and has been described only in 4 cases [7].
Therefore, gender dysphoria in CAIS is considered as a truly transgenderism [8].
The coexistence of CAIS and Eating Disorders has not been described so far, on the contrary, association with overweight, a risk factor for unhealthy restrictive behaviours, has previously been reported.
In adolescents and young adults with ED, the prevalence of a history of overweight or obesity ranges from 19.3% to 36.7% [9].
Overweight adolescents report greater concern about their weight and more body dissatisfaction (BD) than their normal weight peers. They are, therefore, at risk of developing disordered eating behaviours, such as severe fasting to lose weight, and consequently onset of Binge Eating (BE).
Hereby, we present the case of a patient affected by CAIS and BN with a previous history of overweight and a subsequent episode of AN Restricting type.
We describe the psychopathological and medical picture as well as the quality of BD.
Furthermore, this case offers the opportunity to speculate about gender differences of eating disorders and their genetic and epigenetic underpinnings in a condition where male karyotype XY is not congruent with testosterone effects. Testosterone plays a crucial part by inducing a sexual dysmorphic and permanent imprinting on developing brain areas, functionally linked to hunger and satiety control (such as increased size of nuclei involved in regulation of appetite), as well as on neuronal circuits involved in reward mechanisms and attitudes towards food and, finally, on the regulation of energy metabolism and body weight. Males have in general a prevalent orexic-orientated attitude and their metabolism is orientated versus anabolism. This male neurobiology is activated during puberty and it is considered to be the main protective factor against the development of eating disorders. The androgenic protective effect does not only depend on the hormonal level but also on its receptor sensitivity.
Case report
A 22-year-old patient with CAIS, female phenotype, asked for treatment for binge eating episodes.
At birth, her phenotype was consistent with female sex; therefore, she was raised as a girl, a gender in which the patient had always identified herself.
At the age of 15, she underwent an extensive assessment due to primary amenorrhea.
The following data emerged from the examination:
Body Mass Index (BMI) was 19.9 (weight 63 kg, height 1.78 m).
Sex Hormone values (reported in Table 1), were not consistent with female sex.
Lower abdomen ultrasound did not show a delimitable uterus; there was no ultrasound aspect compatible with ovarian tissue.
Nuclear Magnetic Resonance of the pelvis confirmed the absence of a structure compatible with the uterus and the absence of annex formations, while oval formations of 28 mm and 18 mm of maximum diameter of uncertain attribution were appreciated in the ilidal pits.
The patient was then sent for genetic evaluation. No dysmorphism was observed, weight and height were above 97th percentile; poor secondary sex characteristics, reduced pubic hair and armpit hair were described.
Karyotype from peripheral blood resulted 46 XY.
Molecular analysis of the androgen receptor gene (AR), Xq11, was carried out, showing a gene mutation, with a deletion of 61 nucleotides of exon 6 of the AR gene, consistent with a complete loss of function of androgenic receptor.
Diagnosis of Complete Androgen Insensitivity Syndrome (CAIS) was then formulated.
Lumbar and femoral bone density resulted in normal ranges. Undescended testis in ilidal pits was diagnosed and two years later, the patient underwent laparoscopic gonadectomy and hormonal replacement.
At first observation at our ED Center, the patient appeared in good nutritional conditions, BMI was 19.2; blood pressure was 105/74, heart rate 51 bpm. The signs of recent additive mastoplasty were present.
The previous values of sex hormones are shown in Table 1.
Current laboratory tests showed a basal insulin in normal ranges, an increased total cholesterol 238 mg/dl (normal value < 200), HDL cholesterol 63 mg/dl (normal value > 45), LDL cholesterol 134 mg/dl (normal value < 150), triglyceride 145 mg/dl (normal value < 150), glycaemia 75 mg/dl (normal ranges 70–110), ALT 17 U/L (normal value < 35), creatinine 0.83 mg/dl (normal ranges 0.50–1.20).
Haemoglobin (HB) value has decreased 11.8 g/dl (11.5–16.5) compared to 2 years earlier when the analysis documented HB 14 g/dl, despite a low ferritin at that time, 9 ng/ml (n.v.11–306).
Total cholesterol had increased but no other diagnostic element of altered metabolic pattern was present despite the previous overweight.
The patient reported overweight from childhood (from the age of 6) due to an increase in appetite and hyperphagia at meals, in absence of binge eating episodes or abuse of high-calorie or highly palatable foods. Weight progressively increased over the years up to 90 kg at the age of 19 (BMI 28.4).
She played volleyball and non-competitive sports up to the age of 18.
At 19 years old, during a routine check-up for CAIS syndrome, she showed a first weight loss (about 5 kg in a month) obtained through a slight self-managed restriction of caloric intake. This behaviour worsened over time leading to an episode of restrictive AN.
She had a strict control over calorie intake with elimination of phobic foods (e.g. pasta, bread, sweets, oil, butter) and a drastic reduction of portions. Furthermore, she continued to practice compulsive exercise as compensative method. The patient lost 30 kg in one and a half years, reaching the minimum weight of 55 kg (BMI 17.4) maintained for about 6 months; at the age of 19, weight stabilised approximately at 58 kg, BMI 18.3 (Fig. 1).
She showed daily episodes of binge eating a few months before she began the therapy in our ED center. The patient used at that time fasting and physical hyperactivity as compensative behaviour. Self-inducing vomiting or laxative misuse had never been present.
The presence of BE episodes and consequent progressive weight recovery (up to 63 kg, BMI 19.9) increased her BD and prompted her to contact our ED Center.
In first evaluation, the patient reported a severe BD exclusively related to weight recovery and referred to the stomach, thighs and breasts as critical points.
She reported body and food checking behaviour (e.g. checking if the thighs touch each other, trying on very tight clothes, comparing with other girls, counting kcals, weighing foods, controlling the diet of family members, eating very slowly), poor perception of physiological signs of hunger and satiety, high cognitive restriction (dietary rules, allowed and forbidden foods etc.).
As regards psychiatric history, the patient reported a normal psychological development with good school and social relationships, without particular difficulties in the evolutionary process.
Family support was of great help, but it could not protect her from the stress of communication about her genetic disorder; unfortunately, she never accepted psychological help. Her main concern was the infertility caused by CAIS.
The awareness of her condition did not alter a normal development of affective relationships.
Gender and role identity had always been female with heterosexual orientation.
She had a satisfactory emotional relationship with a boyfriend with whom she had regular and satisfying sexual relations.
She reported that BD, begun during adolescence, was related to overweight and mainly due to peers’ teasing. She tried to lose weight through a self-managed dietary restriction.
BD was referred exclusively to the desire for thinness.
The following tests were performed:
-
Eating Disorder Inventory (EDI 2): a self-report questionnaire used to assess the presence of ED [10].
-
Beck Depression Inventory (BDI), a self-report inventory for measuring the severity of depression [11].
-
Binge Eating Scale (BES), a self-report questionnaire used to assess the presence of binge eating behaviour [12].
-
Symptom Check List-90-Revised (SCL-90-R), a checklist measuring the severity of self-reported psychopathological symptoms [13].
-
Body Uneasiness Test (BUT), a questionnaire to evaluate ED and abnormal body image attitudes [14].
Significant test scores are listed in Table 2.
Discussion
We describe for the first time a case of Complete Androgen Insensitivity syndrome (CAIS) presenting an ED consisting of a previous episode of Restrictive AN shifted to BN over time.
It is well known that BD — especially when associated with overweight — is a risk factor for an ED onset.
In the case of a subject with CAIS and overweight, it is possible that the related BD promotes an unhealthy restrictive behaviour.
Peng Yang et al. reported a case of CAIS with obesity and metabolic syndrome, but weight-related BD was not investigated [15].
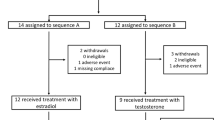
Wisniewski et al. assessed physical and psychosexual status in a sample of 14 subjects (median age 45) with a diagnosis of CAIS, using a questionnaire and medical examination.
BD was evaluated through a questionnaire with three response options (mainly satisfied, somewhat dissatisfied, mainly dissatisfied) regarding the degree of satisfaction with physical appearance.
The results showed that 57% reported a good degree of body satisfaction, while 43% of the sample reported varying degrees of BD both related to physical appearance (such as inadequate body hair, looking younger than actual age etc.) and linked to the presence of obesity [8].
Overweight and hypercholesterolemia, present in our patient, were already reported in CAIS since the alteration in AR receptor can result in increased body fat and increase of cholesterol (total and LDL) [16]. The diagnostic criteria for the definition of metabolic syndrome or diabetes were not present in our patient, but a link between impaired androgen receptor signaling and metabolic regulation has been described by Yang et al. [8].
In our patient, gender identity and gender role showed a female pattern consistent with a normal and healthy psychosexual development as suggested in literature [17].
The co-occurrence of these two rare conditions offers the opportunity to discuss about the reasons of gender dysmorphism of Eating Disorders in general and to speculate on the phenotype of the ED in this subject.
Sexual dysmorphism appears, according to a wide body of literature, to be mostly related to the prenatal exposure to maternal and fetal testosterone.
Their action, starting from the seventh week of intrauterine development determines a male morpho-functional organization.
In puberty, the activational effect of testosterone on a male brain will produce a protective effect against the occurrence of ED [18,19,20]. Masculinisation of the brain is also due to a direct expression of SRY region of Y chromosome. This region — involved in testis differentiation and subsequent testosterone secretion — is chiefly expressed in the testes but, to some extent, it is also expressed in other tissues (e.g. heart, liver and kidneis) and in certain brain regions so influencing the development of male-specific neurobiology and brain function in a direct cell-autonomous manner.
This function, together with others, related for example to the growth-controlling region on the long arm of the Y chromosome, should be present also in CAIS subjects.
Even if the lack of testosterone action determines a female phenotype, it is not possible to exclude brain masculine modifications [21].
Finally, our patient did not present psychiatric symptoms, even though research studies highlight that among women with CAIS, the psychiatric morbidity — especially anxiety and depressive disorders — had significantly increased [22].
We cannot compare our case with other similar cases since CAIS has never been described in association with an ED.
In our patient, the development of an ED was initially linked to the presence of overweight and BD, but “feeling fat” persisted despite the weight loss, representing the typical pathological nucleus of an ED.
Our case report emphasises the importance of performing a correct diagnostic framework of overweight, BD and eating behaviours which are risk factors for ED onset, also in CAIS subjects.
What is already known on this subject?
Cases of patients with CAIS and associated obesity have already been reported, while, to date, there are no reports regarding the onset of an ED in CAIS patients.
What does this study add?
We describe for the first time a case of a patient with CAIS and a previous episode of AN restricting type later shifted to BN.
Our case report emphasises the importance of performing a correct diagnostic framework of overweight, BD, eating behaviours in CAIS patients as risk factors for ED onset.
References
Morris JM (1953) The syndrome of testicular feminization in male pseudohermaphrodites. Am J Obstet Gynecol 65:1192–1211
Gottlieb B, Trifiro MA (2017) Androgen Insensitivity Syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al. (ed). GeneReviews® [Internet]. Seattle (WA) 1993–2020
Oakes MB, Eyvazzadeh AD, Quint E, Smith YR (2008) Complete androgen insensitivity syndrome – a review. J Pediatr Adolesc Gynecol 21(6):305–310
Lanciotti L et al (2019) Different clinical presentations and management in complete androgen insensitivity syndrome (CAIS). Int J Environ Res Public Health 16:1268. https://doi.org/10.3390/ijerph16071268
Petroli RJ, Hiort O et al (2018) Functional impact of novel androgen receptor mutations on the clinical manifestation of androgen insensitivity syndrome. Sex Dev 11:238–247
de Vries AL, Doreleijers TA, Cohen-Kettenis PT (2007) Disorders of sex development and gender identity outcome in adolescence and adulthood: understanding gender identity development and its clinical implications. Pediatr Endocrinol Rev 4(4):343–351
Bermúdez de la Vega JA, Fernández-Cancio M, Bernal S, Audí L (2015) Complete androgen insensitivity syndrome associated with male gender identity or female precocious puberty in the same family. Sex Dev 9(2):75–79
Wisniewski AB et al (2000) Complete androgen insensitivity syndrome: long-term medical, surgical, and psychosexual outcome. J Clin Endocrinol Metab 85(8):2664–2669
Rastogi R, Rome ES (2020) Restrictive eating disorders in previously overweight adolescents and young adults. Clev Clin J Med 87(3):165–171
Garner DM (1991) EDI-2. Eating disorder inventory-2. Professional manual. https://doi.org/10.1007/bf03327738
Beck AT et al (1961) An inventory for measuring depression. Arch Gen Psychiatry 4(6):561–571
Gormally J, Black S, Daston S, Rardin D (1982) The assessment of binge eating severity among obese persons. Addict Behav 7(1):47–55
Symptom Checklist-90-Revised". Pearson: Clinical Psychology. Pearson Education, Inc. Archived from the original on 13 May 2016
Cuzzolaro M, Vetrone G, Marano G, Garfinkel PE (2006) The body uneasiness test (BUT): development and validation of a new body image assessment scale. Eat Weight Disord-St 11:1–13
Yang P, Liu X, Gao J, Qu S, Zhang M (2018) Complete androgen insensitivity syndrome in a young woman with metabolic disorder and diabetes: A case report. Medicine 97(33):e11353. https://doi.org/10.1097/MD.0000000000011353
Dati E et al (2009) Body composition and metabolic profile in women with complete androgen insensitivity syndrome. Sex Dev 3:188–193
Batista RL (2018) Androgen insensitivity syndrome: a review. Arch Endocrinol Metab 62(2):227–235
Procopio M, Marriott P (2007) Intrauterine hormonal environment and risk of developing Anorexia Nervosa. Arch Gen Psychiatry 64(12):1402–1407
Culbert KM et al (2013) The emergence of sex differences in risk for disordered eating attitudes during puberty: a role for prenatal testosterone exposure. J Abnorm Psychol 122:420–432
Lombardo MV et al (2012) Fetal programming effects of testosterone on the reward system and behavioral approach tendencies in humans. Biol Psychiatry 72:839–847
Kopsida E et al (2009) The Role of the Y Chromosome in Brain Function. J neuroendocrinol 2:20–30. https://doi.org/10.2174/1876528900902010020
Engberg H et al (2017) Increased psychiatric morbidity in women with complete androgen insensitivity syndrome or complete gonadal dysgenesis. J Psychosom Res 101:122–127
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Disclosure of potential conflicts of interest: The authors declare that they have no conflict of interest.
Ethical standards
Research involving Human Participants and/or Animal: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from the patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Manzato, E., Gualandi, M. & Roncarati, E. Complete androgen insensitivity syndrome (CAIS) and eating disorders: a case report. Eat Weight Disord 26, 2421–2426 (2021). https://doi.org/10.1007/s40519-020-01069-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-020-01069-1