Abstract
Background
There is scientific consensus that obesity increases the risk of cardiovascular diseases (CVD), including heart failure (HF). However, in CVD, many studies observed greater survival in overweight or class 1 obesity individuals. This counterintuitive observation was termed “obesity paradox” (OP).
Objective and methods
This article is a narrative overview of the relationship between OP and CVD, particularly HF. The sources used were MEDLINE/PubMed, CINAHL, EMBASE, and Cochrane Library, from 2001 to 31 May 2020, exception for a 1983 work of historical importance. Studies reporting association and prognostic impact of obesity in HF and the impact of body composition on cardiac structure and myocardial function in obesity were also included in this review. In addition, we examined references from the retrieved articles and explored several related websites. Ultimately, we chose 79 relevant documents. Fifty-three were specifically focused on OP and HF.
Results
In this review, we made a summary of the evidence coming from a series of studies investigating OP. Many of these studies do not take into consideration or underestimate some of the more important morpho-functional variables of patients suffering from HF: among these, body composition and visceral adiposity, sarcopenic obesity, muscle fitness (MF), and cardiorespiratory fitness (CRF). A high body mass index (BMI) represents a risk factor for HF, but it also seems to exert a protective effect under certain circumstances. Fat distribution, lean mass, and cardio fitness could play an essential role in determining the observed differences in the HF population.
Conclusion
BMI does not distinguish between the metabolically healthy and metabolically unhealthy obesity. The obesity impact on morbidity and premature mortality can be underestimated and, therefore, may lead to incorrect clinical courses.
Level of evidence
Level V, Narrative review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The health consequences of being overweight have been the subject of controversial discussion. Obesity has always been characterized only as an important, albeit modifiable, risk factor of premature mortality, morbidity, and disability [1, 2].
The American Association of Clinical Endocrinologists (AACE) and the American Medical Association (AMA) have already stated that obesity is to be considered a disease [3, 4].
The American Heart Association (AHA), the American College of Cardiology, and The Obesity Society have published guidelines according to which doctors must treat obesity as a disease and consider appropriate interventions for weight reduction [5, 6].
However, there are still conflicting opinions on the definition of obesity as a disease, in particular through the use of BMI as a clinical indicator [7]. The affirmation made by the AMA has been the subject of much debate [8]: the Council objected that recognizing obesity as a disease rather than a syndrome does not automatically lead to positive repercussions and benefits to the health of patients.
Due to the disturbing increased prevalence and the proven health risks, obesity is now recognized as the greatest global challenge to health; as a result, many medical associations concur that obesity should be considered and defined as a true disease [9].
Over the past 2 decades, however, there have been many reports that have complicated the obesity problem; in some diseases, particularly regarding CVD, the best survival rate has been observed in overweight or obese patients of grade 1. This contradictory observation has been termed "OP".
Methods
This article is a narrative overview about the relationship between OP and CVD, particularly HF. For this task, we have chosen the option of a narrative review because the matter is still undergoing extensive discussion. A systematic review would have proved a more rigid revision tool that would not lend itself to addressing a subject for which the contributions are still both modest and contradictory.
The narrative review consists of a critical analysis of the published literature and plays an important role in continuing to educate since it provides updated knowledge on a specific subject or theme.
The sources used were MEDLINE/PubMed, CINAHL, EMBASE, and Cochrane Library, from 2001 to 31 May 2019, with the exception of a 1983 work of historical importance.
Studies reporting association and prognostic impact of obesity in HF and the impact of body composition on cardiac structure and myocardial function in obesity were also included in this narrative review.
In addition, we personally examined references from the retrieved articles and explored a number of related web sites.
Several hundred studies have been reviewed and we have chosen 79 relevant documents, of these 53 were specifically focused on OP and HF (see Tables 1, 2).
We excluded those papers that although dealing with OP and CVD, did not however specifically discuss OP in HF patients.
The obesity paradox
Within the community in general, obesity is known as an independent risk factor for multiple chronic diseases: the lowest mortality risk is considered valid in a BMI range of 18.5–24.9 kg/m2 [10], but some epidemiological and clinical observations seem to indicate that the overweight or Grade 1 obesity could also give a better survival rate; this phenomenon is termed “OP”.
These observations, although widely discussed, were made relating to a series of chronic non-infectious disorders [11,12,13,14,15] and in particular to CVDs. Of the many cardiac disorders, the one that affects the population the most is HF.
There is actually convincing evidence that obesity is associated with advanced CVD; an increase in BMI is associated with a high risk of CVD and a reduction in life expectancy. Recent observations of protection achieved by overweight and grade 1 obesity have confused the views of clinicians and researchers, but the “paradox of obesity” terminology may be the consequence of the fact that we still know little about the multiple and complex pathophysiology of obesity and its complications, especially cardiovascular.
While within the general community, obesity remains associated with a higher risk of mortality, there is now the suggestion that among those that are already carriers of certain diseases it could offer a form of protection in relation to mortality [16, 17].
One should keep in mind that, seen from a metabolic point of view, overweight and obese people are quite heterogeneous; for example, the use of BMI as the only indicator of obesity does not distinguish between the metabolically healthy and metabolically unhealthy obese.
Furthermore, a review in 2015 failed to demonstrate any convincing evidences that BMI 25–35 kg/m2 alone, without taking into consideration metabolic changes, waist measurements [18], correlation between fat and muscular tissue, was a risk factor of higher mortality in the long-term prospect and that its decrease improved survival rate [19].
In this review, we made a summary of the evidence coming from a series of studies investigating “OP” in patients with HF.
There is also discussion of some important clinical and pathophysiological aspects, such as the relationship between the paradox of obesity and cardiorespiratory fitness (CRF).
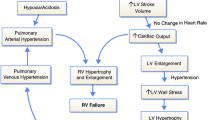
Obesity, obesity paradox, and heart failure
HF is an expanding heart disease: the increasing incidence of obesity in developed countries could well be considered a concomitant factor. However, there are observations showing that once a patient develops HF, overweight and grade 1 obesity seem to allow for greater survival rate.
Multiple interpretations of OP in HF have been examined by Chase et al., who have also assessed the possible impact when treating obese patients with HF [13, 20].
In overweight and moderately obese subjects compared to normal weight patients, the survival rate is sometimes better in the case of chronic HF.
In a review of Clark et al., various explanations for the OP were explored [21]. Gender differences seem to exist in this field. Vest et al. studied the different repercussions of BMI on survival in males and females with major HF. Survival in females is higher than in males, a mechanism that is still unclear. In overweight and moderately obese male patients, the risk of mortality was higher than in normal weight male patients [22]. The conclusion is that being overweight seems to give a survival benefit in female but not in male patients.
Oga et al. have systematically reviewed the relationship between HF mortality and weight status [23]. All studies included in the review used BMI, waist circumference (WC) or triceps thickness skinfold (TSF) for body fat (BF) measurement and NYHA classification for HF. Mortality was used as the sole result and as the study endpoint. The review included ten longitudinal studies: better results emerged in obese HF patients than in those with normal weight. The highest degree of obesity (BMI > 40) was the one that revealed the worst prognosis. These observations can be important when deciding whether obese patients with HF should lose weight. This decision requires a greater knowledge of the mechanisms of OP in relation to HF, especially after having excluded the possible methodological bias.
In patients with HF, but with preserved ejection fraction, Mandviwala et al. found a lower mortality rate than in normal weight subjects, even after matching for more risk factors. The improvement in the survival rate was also evident in patients with class III obesity. However, an increased risk of hospitalization for HF has also been observed in patients with higher BMI values [24].
A protective effect of obesity is suggested in patients that are already affected by HF, but refers to data from studies that have used only BMI as an index of obesity: it is known, however, that BMI does not measure fat mass and does not distinguish between fat-free mass and lean mass.
HF patients could benefit from an intervention that associates nutrition, capable of reducing the inflammatory state, with physical activity (PA), effective on lean body mass (LBM).
There is still no convincing explanation of the increased risk of HF in obesity on the one hand, and of the protective effects in subjects already suffering from HF on the other.
In the various results that emerged in HF patients, an important role can be played by PA. A stratification of the risks of patients with HF that use body composition instead of BMI alone [18] could help identify the most exposed subjects, dividing them into subjects with sarcopenia and subjects with sarcopenic obesity. In this way, strategic interventions on maintaining or improving lean mass could prove useful.
In patients with HF, interventions that are useful to improve CRF are recommended through exercise sessions, including exercise training (ET) to increase muscle mass and strength, especially lean appendiceal mass and its functionality [25].
Another study assessed the degree of myocardial injury pre-HF to understand the different mortality rates attributed to different degrees of weight excess. Although a greater pre-existing subclinical myocardial injury is associated with a higher mortality after hospitalization, this did not provide an explanation of the paradox of obesity in HF, observed independently of myocardial injury [26].
Acute heart failure (AHF)
In patients with AHF, it has been seen that a high body mass index can prove to be a protective factor. However, there is no convincing scientific evidence, coming from extensive studies and long-term follow-up that is effective in explaining the phenomenon of the “OP”. On the other hand, Littnerova et al. states that there are still no useful clinical elements to recommend weight reduction in obese patients with HF [27].
A study by Matsushita et al. found that severely lean patients with AHF were predominantly female with systolic pressure (SBP) < 100 mmHg and heart valvular disease. The overweight patients were younger than normal or underweight ones: the overweight group revealed SBP ≥ 140 mmHg and hypertensive heart disease. There was also an increased risk of mortality from any cause in severely thin patients compared to normal weight or overweight patients [28]. From these observations, it seems possible to conclude that overweight patients have the best prognosis, while the worst is that of very thin patients: these considerations can contribute in understanding the “OP” in patients with severe HF.
A hypothesis may be that the state of acute decompensation can produce alterations in the catabolic direction and favour patients who have greater energy reserves. In HF, the situation is more complicated because thinness can be an epiphenomenon of an unfavourable course linked to the low chronic cardiac output that determines cardiac cachexia.
There are also some suppositions that excess body weight in the elderly can be considered useful to protect against catabolic complications of HF and constitute a sort of “metabolic pillow” to make cachexia less serious [29, 30].
Chronic heart failure (HF)
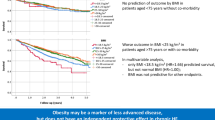
Even for chronic HF, there are clinical studies indicating the existence of an “OP”: meaning lower mortality in patients with high BMI than in subjects with normal weight. Sharma et al. with their study focused on the association between BMI and mortality for cardiovascular (CVD) and other causes, and the risk of hospitalization in patients with chronic HF. Underweight subjects had the highest risk of total mortality, CVD mortality, and hospitalization; in contrast, both CV mortality and hospitalization were lower in excess weight subjects [31].
Other CVDs
There are other cardiac pathologies in which the OP phenomenon has been observed, such as coronary artery disease (CAD) and percutaneous coronary intervention (PCI). However, in post-acute myocardial infarction (AMI) patients, excess weight is not associated with changes in the risk of mortality.[32].
In patients undergoing percutaneous coronary intervention, the paradox of obesity is sometimes observed, but is still poorly understood. Although some studies appear to show a protective effect of overweight and obesity in this kind of patient, many other studies do not confirm any protection from excess weight, but reiterate the harmful consequences of overweight and obesity compared to normal weight subjects [33].
CVD mortality and fitness
The association of BMI with mortality is, therefore, very complex and seems affected by fitness levels [34]. The existence of healthy obesity has been contested by many researchers, who say that, in longitudinal studies, so-called healthy obesity is also associated with CVD and all-cause mortality [35, 36], as well as with target organ changes in cross-sectional studies or in community-based cohort studies [37, 38].
From some studies, which analyzed both independent and joint associations of CRF and obesity with all causes of mortality, CRF was seen to modify the paradox of obesity: in fact, in both obese and non-obese subjects with good CRF, the risk of mortality was significantly low [39].
The same result emerged in two studies with patients suffering from CAD which found that CRF significantly affected this OP [34, 40].
Carnethon et al. have observed that, in patients with CAD, high CRF fitness is associated with reduced mortality, while the increase in mortality is specifically related to physical fitness and central obesity when CAD patients undergo cardiac rehabilitation [41].
An above-average cardiorespiratory fitness is significantly associated with a lower mortality risk both in the general population [42] and CAD patients [43].
The joint impact on mortality of physical fitness and obesity in healthy and high-risk subjects has revealed that obese subjects with good CRF have a mortality risk similar to that of normal weight subjects but with poor physical fitness. However, these observations come from studies that used an estimation in exercise capacity in metabolic equivalents (MET) rather than an accurate indicator of exercise capacity and cardiorespiratory form represented by the absorption of the directly measured oxygen peak (VO2 peak) [44, 45].
Heart failure and fitness
Lavie et al. analyzed the impact of cardiorespiratory functions on survival in patients with systolic HF. Their results indicate that fitness influences the relationship between BMI and survival [46]. Therefore, looking for OP in systolic HF may be misleading unless fitness is also considered [47].
Carbone et al. emphasize that people with obesity generally have large amounts of LBM. This is an aspect that, at least in part, may explain the OP, especially when it is associated with better CRF, one of the main sources of clinical outcomes in the general population, but particularly in HF [48].
Uretsky et al. studied the interaction between obesity and survival in patients with normal resting stress photon emission computed tomography (SPECT). Being physically fit offers an obvious advantage at all weight levels, as well as not having good fitness has negative consequences [49].
A systematic review could show that subjects with high BMI and good aerobic fitness have a lower risk of both cardiovascular and all-cause mortality compared to subjects with normal weight and poor physical fitness [50].
Powerful predictors of both cardiovascular and all-cause mortality are, therefore, represented by physical fitness, especially the MF and the CRF [51].
Although CRF is rarely evaluated, unlike other CV risk factors, it is evident that low CRF levels represent the most significant CV risk factor [52].
A meta-analysis by Kodama et al. found that for each change in the exercise capacity of 1 MET, CV mortality and major CV events change by 13% and 15%, respectively [53].
In a study conducted on patients with CAD, Lavie et al. suggest that instead of a true paradox of obesity there may be a “lean paradox”, since the higher mortality is evident only in patients with low BMI and low weight BF [47, 54]. The phenomenon is particularly evident in patients with low BF and low levels of lean mass or low fat-free mass. Considering that MF is a powerful predictor of both CV prognosis and mortality [55], the skinny subjects probably have lower MF levels than people with higher weight.
Multiple research in patients with CAD and HF has shown that CRF significantly reduces the relationship between obesity and clinical prognosis [53]: patients with higher CRF levels revealed better prognosis. The same observation emerged recently from a study of over 2000 patients with systolic HF [53]. In addition, from various researches on around 10,000 patients with known or suspected CAD, an OP emerged only in those in the lowest 20% age group.[39, 40, 56, 57].
It is clinically predictable that patients undergoing pharmacological stress tests are less fit and, therefore, present a higher risk of mortality. In a group of over 4000 patients with normal results in a nuclear perfusion stress test, Uretsky et al. observed the OP regardless of the degree of CRF [49].
Patients with the best CRF degrees revealed an extremely low risk of mortality, less than 1% per year. Among these patients, those with normal weight showed higher mortality (1.4%/year) than those both overweight and obese (0.9%/year and 0.6%/year). In this study, CRF levels were not matched by age and gender, with the concrete risk of methodological bias. However, in a diversified analysis, BMI and mortality each maintained an independent role. These results, therefore, seem to demonstrate that an OP may be present in these selected patients undergoing nuclear perfusion scan at good CRF levels, with the CRF level always maintaining its strong impact on life expectancy.
Although many observations of HF patients, who have carefully analyzed the impact of BMI on outcomes, suggest the existence of an “OP”, Habbu et al. argue that a more in-depth examination and more detailed studies of this sort could raise doubts about the validity of the paradox. They also argue that prospective studies that measure the effect of severe obesity on the outcomes of HF patients are needed to definitively determine the existence of OP [58].
The management of HF in obese adult patients is not specifically mentioned in the guidelines for clinical practice of the American College of Cardiology and the American Heart Association [59], while the European Society of Cardiology recommends that overweight patients and obese people with HF lose weight [60].
It follows that obese patients with consolidated HF may be advised not to lose weight because of the potential clinical impact of an “OP”: this can have dangerous consequences. Also for this reason, the effect of intentional weight loss on HF has been studied [21]. Ultimately, it is very important to obtain a common clarity on the OP: whether it exists or does not exist.
Clark et al. studied the relationships between the OP, CRF and HF prognosis. CRF was assessed as an oxygen uptake peak (VO2) or as ventilation per minute (VCO2): it was found that in HF patients, CRF proved to be a significant forecaster of survival [21].
Chase et al. examined 1728 HF patients and highlighted that obese patients had significantly reduced VE/VCO2 slopes when compared to normal weight or overweight patients, which brought to the conclusion that VE/VCO2 is both a strong and independent predictor of greater survival [61].
Lavie et al. were able to highlight that the level of CRF is capable of modifying the paradox of obesity: in 2066 patients with HF, they observed that BMI, adjusted for age and gender, proved to be a significant predictor of survival within the group of patients with low peak VO2 (< 14 ml/O2/kg) (P = 0.03) but outside the group with high CRF [25]. These observations suggest that favourable scores in cardiorespiratory exercise tests may significantly change the real meaning of OP in HF. Lavie et al. also suggest that training to improve CRF may also be helpful in subjects with a low degree of obesity [25].
These results would seem to highlight that OP is influenced by physical frailty in older patients with CVD disease [62].
Nakamura et al. showed that patients with high BMI associated with cardiovascular pathologies and with preserved gait speed consistently had a favourable prognosis unlike patients with the same high BMI but with slow gait speed [62].
Thomas et al. used bioelectrical impedance to evaluate body composition in chronic HF patients and confirmed that high LBM values are the best predictor of survival. They argue that although weight loss is often encouraged in patients with CVD, caution should be recommended in overweight HF subjects [63].
The increased amount of LM reported in individuals with the typical obesity phenotype is a major drive for increased CRF. Greater CRF is associated with an improved survival rate and may partially explain the beneficial effects of obesity. Individuals with reduced amounts of LM (i.e. sarcopenia), even in the context of obesity (i.e. sarcopenic obesity) present a worse CRF [48].
Further studies on the interrelationship between body composition and CRF may improve knowledge of the paradox of obesity in HF [14].
Discussion and conclusions
A high body mass index is associated with a higher incidence of HF [61, 64], but mortality after the development of HF appears to be lower in some obese patients than in normal weight subjects [61]. This phenomenon, referred to as the “OP”, is in contradiction with some animal studies, which show that increased adiposity is associated with myocardial fibrosis and increased apoptosis [65]. However, these obesity knockout genetic models do not take into account the environmental factors and the multiple aspects of obesity which humans have developed over time.
The complexity of myocardial pathophysiology is underlined by these results which highlight the fact that simple solutions are not easily available.
The low mortality risk observed in obese and overweight individuals compared to normal weight individuals after the development of HF cannot be explained by pre-existing subclinical myocardial injury. Multiple factors, including pre-existing HF, need to be studied to explain OP in HF patients.
The prevalence of overweight and obesity is on the rise worldwide. There is compelling evidence to support the adverse impact of obesity on cardiac performance and the morphology leading to HF. On the other hand, there are multiple observations supporting the existence of an OP, according to which obese patients with HF have a better prognosis than leaner ones.
A high BMI has been observed to confer greater survival even to patients with chronic complications of diabetes, particularly cardiovascular complications [66].
Consensus has yet to emerge as to whether OP is a true phenomenon. Many theories try to explain the mechanism of the OP, but have only been partially successful.
The role of weight reduction in the prognosis of HF patients has not yet been clarified and there are no guidelines with convincing recommendations. Further research is needed in this field, including the role of the autonomic nervous system, to explain the possible mechanisms of the paradox of obesity in HF.
Although overweight and moderate obesity may confer a protective effect on mortality compared to normal BMI conditions, greater morbidity is observed in severe obesity, with an increased risk of respiratory and cardiovascular complications that require particular therapeutic effort [67].
According to Aimo et al. a high BMI represents a risk factor for HF, but in certain circumstances, it can also exert protective effects: in their experience, the worst prognosis is observed in subjects with low body weight [68].
Gavaldà-Manso et al. studied vasopressin levels in patients with BMI < 35 and observed an inverse relationship between vasopressin and BMI levels. Based on this finding, they suspect that low vasopressin levels may represent an independent survival mechanism in obese subjects with CHF [69].
The mechanisms associated with the increased risk of HF and on the other hand the factors that appear protective in the post-HF diagnosis stages have not yet been clarified. However, LBM is a factor that decisively influences the clinical course of HF patients.
It is, therefore, important to correctly stratify the risk of HF patients considering also body composition instead of BMI alone. This methodology can be very effective to diagnose higher risk patients. A therapeutic strategy aimed at identifying subjects with sarcopenia and sarcopenic obesity can allow approaches aimed at preserving or increasing LBM and obtaining clinically positive results.
Chrysant and Chrysant state that the mere use of the body mass index for the purpose of OP leads to errors: it should always be used in association with other indices of excess weight and body distribution [70]. In response to a letter from Carbone and Lavie [71], the same authors suggest the use of more standardized obesity indices (BMI, WC, and WHR) to determine the real presence and incidence of OP [72].
In a group of Asian HF patients, the “OP” is manifested only using BMI as a weight parameter; when the height-to-waist ratio (WHtR) is applied, the opposite association emerges. The worst results were observed in normal weight patients with low BMI but high WHtR [73].
In patients with HF, in addition to medical care, it is recommended that the main therapeutic goal is to improve CRF through exercise (ET), including strength and endurance training to increase muscle mass and strength, appendicular lean mass and its functionality [72, 74, 75].
All indicators of PA and physical fitness are independently associated with metabolic equivalents (MetS). Oga et al. demonstrated for the first time that physical fitness remains the strongest predictor of MetS and that the association does not change, if it is adapted simultaneously for both sedentary time (SED) and moderate to vigorous physical activity (MVPA) [23]. In the lower range of the PA spectrum, the triaxial accelerometry methodology is the most sensitive and therefore the most useful from a clinical point of view.
The assessment of the sedentary time is strategic for classifying patients with reduced PA (low MVPA). The results of the above study [23] confirm the clinical importance of recommending PA, even in patients characterized by MetS at risk.
Furthermore, Simonenko, in a recent editorial, argues that the association between obesity and survival improvement must be considered evident, also in light of the results obtained with multiple indicators of overweight subjects [74]. Simonenko, recognizing that the benefits of intentional weight loss on the hemodynamic function and myocardial structure of HF patients are equally evident, concludes that further research is needed to develop common guidelines for weight management in HF patients [74]. It should be emphasized that a systematic meta-analysis in obese patients has shown that intentional weight loss is associated with an improvement in structural and functional myocardial indices [75].
In a recent report on patients with type 1 diabetes, Edqvist et al. observed that patients with poor metabolic control and BMI < 25 had no increased risk of mortality, while BMI > 25 was associated with a small increase in risk of mortality, CVD and HF. The associations were more evident in men than in women. Weight gain resulted in increased risk of mortality and HF, while weight loss was not associated with greater risk. Authors concluded that the risk of CVD, HF, CVD mortality and all-cause mortality increase with increasing BMI. After excluding factors associated with reverse causality, they did not find evidence of an OP [76].
Table 1 reports the studies that observed the phenomenon of OP in patients with HF; Table 2 on the other hand shows reported studies that did not find this counterintuitive phenomenon.
In conclusion, there are observations that in some cases show that obesity may allow for a longer life expectancy even in patients with HF. On the other hand, these observations could be the result of the use of inadequate indicators of fat distribution or failure to assess physical fitness, regardless of the category of obesity. Further research should be directed to study and better understand the mechanisms of this possible protection given from excess weight. This will help improve the management of each individual patient, especially from a therapeutic point of view.
What is already known on this subject?
-
The prevalence and incidence of overweight and obesity are still increasing in all countries of the world and there is ample evidence of an association with premature mortality, morbidity and disability, particularly for CVD and especially for HF.
-
On the other hand, in some diseases, such as HF, the best survival is observed in overweight or obese grade 1 patients. This counterintuitive observation has been called the “obesity paradox”.
-
It is necessary to clarify this paradox, especially from a therapeutic point of view.
What does this study add?
-
Very detailed studies have shown that the simple use of the body mass index for the purpose of OP leads to errors: it should always be used in association with other indices of excess weight and body distribution.
-
All-cause and CVD mortality risk is lower in subjects with high BMI and good CRF compared with those with normal BMI and poor physical fitness.
-
Therefore, looking for OP in CVD, especially systolic HF, can be misleading unless physical fitness is considered
-
It must be recognized that OP can exist in selected patients and that obesity can be associated with better life expectancy even in patients with HF, but it is necessary to consider the distribution of adiposity and cardiorespiratory form.
-
Systematic reviews and meta-analyses observed that intentional weight loss is associated with improving myocardial function indices in obese patients.
-
There is a need to develop shared guidelines for managing body weight in overweight patients with HF.
Abbreviations
- AHF:
-
Acute heart failure
- AMI:
-
Acute myocardial infarction
- BIA:
-
Bioelectrical impedance analysis of body composition
- BF:
-
Body fat
- CAD:
-
Coronary artery disease
- CHF:
-
Chronic heart failure
- CRF:
-
Cardiorespiratory fitness
- CVD:
-
Cardiovascular disease
- ET:
-
Exercise training
- HF:
-
Heart failure
- HFpEF:
-
HF with preserved ejection fraction
- HFrEF:
-
HF with reduced ejection fraction
- LBM:
-
Lean body mass
- LM:
-
Lean mass
- MET:
-
Metabolic equivalent
- MI:
-
Myocardial infarction
- MF:
-
Muscular fitness
- MNOB:
-
Metabolically normal obese
- MAOB:
-
Metabolically abnormal obese
- MVPA:
-
Moderate to vigorous physical activity
- NTLR:
-
Non-target lesion revascularization
- NT-proBNP:
-
Natriuretic peptide
- OP:
-
Obesity paradox
- PA:
-
Physical activity
- PBF:
-
Percent body fat
- PCI:
-
Percutaneous coronary intervention
- SBP:
-
Systolic blood pressure
- SPECT:
-
Single-photon emission computed tomography
- TLR:
-
Target lesion revascularization
- TSF:
-
Triceps skin fold
- WC:
-
Waist circumference
- WHR:
-
Waist-to-hip ratio
- WHtR:
-
Waist-to-height ratio
References
Hubert HB, Feinleib M, McNamara PM, Castelli WP (1983) Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham heart study. Circulation 67(5):968–977. https://doi.org/10.1161/01.cir.67.5.968
Capodaglio P, Liuzzi A (2013) Obesity: a disabling disease or a condition favoring disability? Eur J Phys Rehabil Med 49(3):395–398
American Association of Clinical Endocrinologists (AACE) (2011) American Association of Clinical Endocrinologists (AACE) Declares Obesity a Disease State. https://media.aace.com/press-release/american-association-clinical-endocrinologists-aace-declares-obesity-disease-state. Accessed 11 Nov 2014
American Medical Association House of Delegates (2013) Report of the Council on Science and Public Health (CSAPH). Recognition of Obesity as a Disease. Resolution 420 (A-13). 2013. https://www.ama-assn.org/assets/meeting/2013a/a13-addendum-refcomm-d.pdf-page=19. Accessed 11 Nov 2014
Jensen MD, Ryan DH, Apovian CM et al (2013) 2013 AHA/ACC/TOS Guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and The Obesity Society. Circulation. https://doi.org/10.1161/01.cir.0000437739.71477
Ravussin E, Ryan DH, The Obesity Society et al (2014) Expert panel report: guidelines (2013) for the management of overweight and obesity in adults. Obesity 22(S2):S41–S410. https://doi.org/10.1002/oby.20660
Allison DB, Downey M, Atkinson RL et al (2008) Obesity as a disease: a white paper on evidence and arguments commissioned by the Council of the Obesity Society. Obesity 16(6):1161–1177. https://doi.org/10.1038/oby.2008.231
MedPage Today (2013) AMA house votes against council, calls obesity a disease. https://www.medpagetoday.com/MeetingCoverage/AMA/39952
Editorial Lancet Diabetes Endocrinology (2017) Should we officially recognise obesity as a disease? Lancet Diabetes Endocrinol 5(7):483. https://doi.org/10.1016/S2213-8587(17)30191-2
Classification of Overweight and Obesity by BMI, Waist Circumference, and Associated Disease Risks (2012) https://www.nhlbi.nih.gov/health/public/heart/obesity/losewt./bmi.dis.htm
Bosello O, Donataccio MP (2013) Obesity paradox. Eat Weight Disord 8(4):447–448. https://doi.org/10.1007/s40519-013-0080-5 (Epub 2013 Oct 13)
Lechi A (2017) The obesity paradox: is it really a paradox? Hypertens Eat Weight Disord 22:43–48. https://doi.org/10.1007/s40519-016-0330-4
Ferrari M, Spelta F, Fratta Pasini AM, Cazzoletti L (2018) Obesity paradox in COPD. Eat Weight Disord 23:15–22. https://doi.org/10.1007/s40519-017-0456-z
Trestini I, Carbognin L, Bonaiuto C, Tortora G, Bria E (2018) The obesity paradox in cancer: clinical insights and perspectives. Eat Weight Disord Stud Anorexia Bulimia Obes 23:185–193. https://doi.org/10.1007/s40519-018-0489-y
Fassio A, Idolazzi L, Rossini M, Gatti D, Adami G, Giollo A, Viapiana O (2018) The obesity paradox and osteoporosis. Eat Weight Disord Stud Anorexia Bulimia Obes 23:293–302. https://doi.org/10.1007/s40519-018-0505-2
Flegal KM, Kit BK, Orpana H, Graubard BI (2013) Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. J Am Med Assoc 309(1):71–82. https://doi.org/10.1001/jama.2012.113905
Flegal KM, Kalantar-Zadeh K (2013) Overweight, mortality and survival. Obesity 21(9):1744–1745. https://doi.org/10.1002/oby.20588
Bosello O, Donataccio MP, Cuzzolaro M (2016) Obesity or obesities? Controversies on the association between body mass index and premature mortality. Eat Weight Disord 21(2):165–174. https://doi.org/10.1007/s40519-016-0278-4
Samorodskaja IV, Bolotova EV, Boytsov SA (2015) Paradox of obesity and cardiovascular mortality. Kardiologia 55(9):31–36. https://doi.org/10.1001/archinte.165.1.55
Chase PJ, Davis PG, Bensimhon DR (2014) The obesity paradox in chronic heart failure: what does it mean? Curr Heart Fail Rep 11(1):111–117. https://doi.org/10.1007/s11897-013-0184-2
Clark AL, Fonarow GC, Horwich TB (2014) Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis 56(4):409–414. https://doi.org/10.1016/j.pcad.2013.10.004
Vest AR, Wu Y, Hachamovitch R, Young JB, Cho L (2015) The heart failure overweight/obesity survival paradox: the missing sex link. JACC Heart Fail 3(11):917–926. https://doi.org/10.1016/j.jchf.2015.06.009
Oga EA, Eseyin OR (2016) The obesity paradox and heart failure: a systematic review of a decade of evidence. J Obes. https://doi.org/10.1155/2016/9040248
Mandviwala TM, Sukhdeep S, Basra SS et al (2020) Obesity and the paradox of mortality and heart failure hospitalization in heart failure with preserved ejection fraction. Int J Obes. https://doi.org/10.1038/s41366-020-0563-1
Lavie CJ, Alpert MA, Arena R et al (2013) Impact of obesity and the obesity paradox on prevalence and prognosis in heart failure. JACC Heart Fail 1:93–102. https://doi.org/10.1016/j.jchf.2013.01.006
Pokharel Y, Sun W, Virani SS et al (2017) Myocardial injury, obesity, and the obesity paradox. The ARIC study. JACC Heart Fail. https://doi.org/10.1016/j.jchf.2016.10.010
Littnerova S, Parenica J, Spinar J et al (2015) Positive influence of being overweight/obese on long term survival in patients hospitalised due to acute heart failure. PLoS ONE 10(2):e0117142. https://doi.org/10.1371/journal.pone.0117142.eCollection2015
Matsushita M, Shirakabe A, Hata N et al (2017) ) Association between the body mass index and the clinical findings in patients with acute heart failure: evaluation of the obesity paradox in patients with severely decompensated acute heart failure. Heart Vessel 32(5):600–608. https://doi.org/10.1007/s00380-016-0908-9
Hall ME (2018) Body mass index and heart failure mortality. More is less? ACC Heart Fail 6(3):243–245. https://doi.org/10.1016/j.jchf.2017.12
Bosello O, Vanzo A (2019) Obesity paradox and aging. Eat Weight Disord. https://doi.org/10.1007/s40519-019-00815-4 (Online ahead of print. PMID: 31865598)
Sharma A, Lavie CJ, Borer JS et al (2015) Meta-analysis of the relation of body mass index to all-cause and cardiovascular mortality and hospitalization in patients with chronic heart failure. Am J Cardiol 115(10):1428–1434. https://doi.org/10.1016/j.amjcard.2015.02.024
Wang L, Liu W, He X et al (2016) Association of overweight and obesity with patient mortality after acute myocardial infarction: a meta-analysis of prospective studies. Int J Obes (Lond) 40(2):220–228. https://doi.org/10.1038/ijo.2015.176
Wolny R, Maehara A, Liu Y et al (2020) The obesity paradox revisited: body mass index and long-term outcomes after PCI from a large pooled patient-level database. EuroIntervention 15:1199–1208. https://doi.org/10.4244/EIJ-D-19-00467
Goel K, Thomas RJ, Squires RW et al (2011) Combined effect of cardiorespiratory fitness and adiposity on mortality in patients with coronary artery disease. Am Heart J 161:590–597. https://doi.org/10.1016/j.ahj.2010.12.012
Kuk JL, Ardern CI (2009) Are metabolically normal but obese individuals at lower risk for all-cause mortality? Diabetes Care 32:2297–2299. https://doi.org/10.2337/dc09-0574
Arnlov J, Ingelsson E, Sundstrom J et al (2010) Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation 121:230–236. https://doi.org/10.1161/CIRCULATIONAHA.109.887521
Lind L, Siegbahn A, Ingelsson E et al (2011) A detailed cardiovascular characterization of obesity without the metabolic syndrome. Arterioscler Thromb Vasc Biol 31:e27–e34. https://doi.org/10.1161/ATVBAHA.110.221572
Lee SK, Kimb SH, Choc GY et al (2013) Obesity phenotype and incident hypertension: a prospective community-based cohort study. J Hypertens 31:145–151. https://doi.org/10.1097/HJH.0b013e32835a3637
McAuley PA, Smith NS, Emerson BT et al (2012) The obesity paradox and cardiorespiratory fitness. J Obes. https://doi.org/10.1155/2012/951582
McAuley PA, Kokkinos PF, Oliveira R et al (2010) Obesity paradox and cardiorespiratory fitness in 12,417 male veterans aged 40–70 years. Mayo Clin Proc 85:115–121. https://doi.org/10.4065/mcp.2009.0562
Carnethon MR, de Chavez PJ, Biggs ML et al (2012) Association of weight status with mortality in adults with incident diabetes. JAMA 308(6):581–590. https://doi.org/10.1001/jama.2012.9282
Myers J, Prakash M, Froelicher V et al (2002) Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 346:793–801. https://doi.org/10.1056/NEJMoa011858
Kavanagh T, Mertens DJ, Hamm LF et al (2003) Peak oxygen intake and cardiac mortality in women referred for cardiac rehabilitation. J Am Coll Cardiol 42:2139–2144. https://doi.org/10.1016/j.jacc.2003.07.028
Fletcher GF, Balady GJ, Amsterdam EA et al (2001) Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation 104:1694–1697. https://doi.org/10.1161/hc3901.095960
Carbone S, Lavie CJ, Arena R (2017) Obesity and heart failure: focus on the obesity paradox. Mayo Clin Proc 92(2):266–279. https://doi.org/10.1016/j.mayocp.2016.11.001
Lavie CJ, Milani RV, Ventura HO et al (2010) Body composition and heart failure prevalence and prognosis: getting to the fat of the matter in the “obesity paradox”. Mayo Clin Proc 85:605–608. https://doi.org/10.4065/mcp.2010.0336
Lavie CJ, Cahalin LP, Chase P et al (2013) Impact of cardiorespiratory fitness on the obesity paradox in patients with heart failure. Mayo Clin Proc 88:251–258. https://doi.org/10.1016/j.mayocp.2012.11.020
Carbone S, Canada JM, Billingsley HE et al (2019) Obesity paradox in cardiovascular disease: where do we stand? Vasc Health Risk Manag 15:89–100
Uretsky S, Supariwala A, Gurram S et al (2013) The interaction of exercise ability and body mass index upon long-term outcomes among patients undergoing stress-rest perfusion SPECT imaging. Am Heart J 166:127–133. https://doi.org/10.1016/j.ahj.2013.03.027
Lavie CJ, De Schutter A, Patel DA et al (2012) Body composition and survival in stable coronary heart disease: impact of lean mass index and body fat in the “obesity paradox”. J Am Coll Cardiol 60:1374–1380. https://doi.org/10.1016/j.jacc.2012.05.037
Swift DL, Lavie CJ, Johannsen NM et al (2013) Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention. Circ J 77:281–292. https://doi.org/10.1253/circj.cj-13-0007
Lavie CJ, De Schutter A, Patel DA et al (2013) Does fitness completely explain the obesity paradox? Am Heart J 166:1–3. https://doi.org/10.1016/j.ahj.2013.03.026
Kodama S, Kazumi S, Tanaka S et al (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women—a meta-analysis. JAMA 301(19):2024–2035. https://doi.org/10.1001/jama.2009.681
Lavie CJ, De Schutter A, Patel D et al (2011) Body composition and coronary heart disease mortality: an obesity or a lean paradox? Mayo Clin Proc 86(9):857–864. https://doi.org/10.4065/mcp.2011.0092
Artero EG, Lee DC, Lavie CJ et al (2012) Effects of muscular strength on cardiovascular risk factors and prognosis. J Cardiopulm Rehabil Prev 32:351–358. https://doi.org/10.1097/HCR.0b013e3182642688
McAuley PA, Blair SN (2011) Obesity paradoxes. J Sports Sci 29:773–782. https://doi.org/10.1080/02640414.2011.553965
McAuley PA, Artero EG, Sui X et al (2012) The obesity paradox, cardiorespiratory fitness, and coronary heart disease. Mayo Clin Proc 87:443–451. https://doi.org/10.1016/j.mayocp.2012.01.013
Habbu A, Lakkis NM, Dokainish H (2006) The obesity paradox: factor or fiction? Am J Cardiol 98:944–948. https://doi.org/10.1016/j.amjcard.2006.04.039
Hunt SA, Abraham WT, Chin MH, American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation, and Management of Heart Failure) et al (2005) ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult. J Am Coll Cardiol 2005(46):1116–1143. https://doi.org/10.1161/CIRCULATIONAHA.105.167586
Remme WJ, Swedberg K (2001) Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J 22:1527–1560. https://doi.org/10.1053/euhj.2001.2783
Chase PJ, Kenjale A, Cahalin LP et al (2013) Effects of respiratory exchange ratio on the prognostic value of peak oxygen consumption and ventilatory efficiency in patients with systolic heart failure. JACC Heart Fail 1(5):427–432. https://doi.org/10.1016/j.jchf.2013.05.008
Nakamura T, Kamiya K, Matsunaga A et al (2019) Impact of gait speed on the obesity paradox in older patients with cardiovascular disease. Am J Med. https://doi.org/10.1016/j.amjmed.2019.06.047
Thomas E, Gupta PP, Fonarow GC et al (2019) Bioelectrical impedance analysis of body composition and survival in patients with heart failure. Clin Cardiol 42:129–135. https://doi.org/10.1002/clc.23118
Gruberg L, Weissman NJ, Waksman R et al (2002) The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol 39:578–584. https://doi.org/10.1016/s0735-1097(01)01802-2
Uretsky S, Supariwala A, Singh P et al (2010) Impact of weight on long-term survival among patients without known coronary artery disease and a normal stress SPECT MPI. J Nucl Cardiol 17:390–397. https://doi.org/10.1007/s12350-010-9214-6
Rajiv Singla R, Murthy M, Singla S et al (2019) Friendly fat theory—explaining the paradox of diabetes and obesity. Eur Endocrinol 15(1):25–28. https://doi.org/10.17925/EE.2019.15.1.25
Schetz M, De Jong A, Deane AM et al (2019) Obesity in the critically ill: a narrative review. Intensive Care Med 45(6):757–769. https://doi.org/10.1007/s00134-019-05594-1
Aimo A, Januzzi JL Jr, Vergaro G et al (2019) Revisiting the obesity paradox in heart failure: per cent body fat as predictor of biomarkers and outcome. Eur J Prev Cardiol 1:2047487319852809. https://doi.org/10.1177/2047487319852809
Gavaldà-Manso M, Jimenez-Marrero S, Cainzos-Achirica M et al (2018) Reduced levels of vasopressin, an independent mechanism in the obesity paradox in patients with chronic heart failure: Insights from the DAMOCLES study. Int J Cardiol 276:171–176. https://doi.org/10.1016/j.ijcard.2018.10.094
Chrysant SG, Chrysant GS (2019) The single use of body mass index for the obesity paradox is misleading and should be used in conjunction with other obesity indices. Postgrad Med 131(2):96–102. https://doi.org/10.1080/00325481.2019.1568019
Carbone S, Lavie CJ (2019) An opposing point of view on the obesity paradox. Postgrad Med 131(5):333–334. https://doi.org/10.1080/00325481.2019.1612150
Chrysant SG, Chrysant GS (2019) In response to in: opposing point of view on the obesity paradox. Postgrad Med. https://doi.org/10.1080/00325481.2019.1643637
Chandramouli C, Tay WT, Bamadhaj NS et al (2019) Association of obesity with heart failure outcomes in 11 Asian regions: a cohort study. PLoS Med. https://doi.org/10.1371/journal.pmed.1002916
Simonenko M (2019) Obesity paradox in heart failure: a matter of debate. Eur J Prev Cardiol. https://doi.org/10.1177/2047487319861473
Mahajan R, Stokes M, Elliott A (2019) Complex interaction of obesity, intentional weight loss and heart failure: a systematic review and meta-analysis. Heart. https://doi.org/10.1136/heartjnl-2019-314770
Edqvist J, Rawshani A, Adiels M et al (2019) BMI, mortality, and cardiovascular outcomes in type 1 diabetes: findings against an obesity paradox. Diabetes Care 42(7):1297–1304. https://doi.org/10.2337/dc18-1446(Epub 2019 May 2)
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The article is a review article and does not require ethics approval.
Informed consent
The article is a review article and does not require informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The article is part of the Topical collection on Obesity paradox.
Rights and permissions
About this article
Cite this article
Donataccio, M.P., Vanzo, A. & Bosello, O. Obesity paradox and heart failure. Eat Weight Disord 26, 1697–1707 (2021). https://doi.org/10.1007/s40519-020-00982-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-020-00982-9