Abstract
Purpose
To report on the mortality of DSM-IV eating disorders and predictors of premature death in males compared to females after inpatient treatment.
Methods
Crude mortality rate (CMR) and standardized mortality ratio (SMR) were computed for a large sample of males aged at treatment 16–61 years [N = 66 anorexia nervosa (AN), 52 bulimia nervosa (BN), 70 eating disorder not otherwise specified (ED-NOS)] and females aged 14–65 years (N = 2066 AN, 1880 BN, 1350 ED-NOS). In addition, a survival analysis and Cox regression analyses for identifying predictors of death were computed.
Results
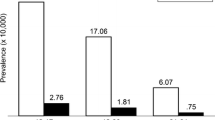
CMRs for males and females, respectively, were 15% and 5% in AN, 8% and 3% in BN, and 4% and 3% in ED-NOS. Compared to the general population, mortality was elevated in males with AN (SMR = 4.93) and in all female diagnostic groups (AN, BN, ED-NOS). No significant sex differences for SMR emerged in any diagnostic group. Compared to females with AN or BN, males with AN or BN showed a shorter survival time after onset (survival analysis). Being male, and having AN, increased the risk of premature death.
Conclusion
Mortality in inpatients with eating disorder is high, especially in AN. Males appear to have about the same outcome in terms of mortality as females with AN, BN, and ED-NOS. However, long-term survival was shorter in males with AN or BN compared to females. The need for intensive treatment in both males and females with an eating disorder remains an important issue.
Level of evidence
Level III, case–control analytic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A small minority of individuals presenting for treatment of anorexia nervosa (AN) or bulimia nervosa (BN) are males. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [1] estimates the male:female ratio in clinical populations of AN and BN as 1:10. The fourth edition of the DSM (DSM-IV) [2] combines less severe types of AN and BN and eating disorders (ED) with other described symptoms into the category ED not otherwise specified (ED-NOS). A special case is binge-eating disorder (BED) which in the DSM-IV is categorized as an ED-NOS and in the DSM-5 as a main ED. For the heterogeneous category of ED-NOS, no estimate of the male:female ratio is provided and the DSM-5 (page 351) simply states that the “gender ratio is far less skewed in BED than in BN”. Epidemiological studies confirm the lower prevalence of EDs in males compared to females. The National Comorbidity Survey Replication [3], a representative survey of households in the United States, found a lifetime prevalence of 0.3% of AN, 0.5% of BN, and 2.0% of BED in the male population. A more recent survey in Germany [4] reported a 12-month prevalence of 0.3% of AN, 0.1% of BN, and 0.1% of BED in males. As a consequence of the relative low prevalence, little is known about the outcome of EDs in males. A recent literature review of the outcome in male AN, the best-researched ED in males, concluded that only very limited evidence on the outcome of AN in males exists [5].
Still less knowledge exists on the worst possible outcome, mortality in males with ED. Only a very few studies on mortality in purely male samples exist. A simple measure of mortality is the crude mortality rate (CMR; percentage of deceased patients in a given sample) which depends heavily on sample size and varied widely between studies. Applying strict inclusion criteria, an overview of males with AN reported CMRs ranging from 0 to 17% after 1–10 years, and CMRs between 0 and 27% after 1–12 years in mixed samples of adolescent and adult males [5]. A CMR of 12.9% for male AN inpatients was reported by Quadflieg et al. [6]. Burns and Crisp [7], however, reported no deaths in 27 males with AN after 2–20 years. An older overview combining a large number of study samples with a small fraction of males reported a mean CMR of 5% in AN [8]. Another study reported a CMR of 4.0% in a mixed sample of outpatients with 5 male and 172 female participants with AN [9].
Several clinical studies published standardized mortality ratios (SMR; ratio of deceased patients versus expected deaths in the age- and sex-matched general population) for males with AN. Gueguen et al. [10] found a significant SMR of 8.08 in 23 male inpatients after 10 years. Another study identified a non-significant SMR of 0.79 in a large clinical male sample [11]. Quadflieg et al. reported an SMR of 5.91 (p < 0.05) in male AN inpatients [6]. Larger sample sizes were included in studies using national registers of treatment and of causes of death. In males treated for AN, SMRs were 2.7 in England [12], 4.1 in Sweden [13], and 8.2 in Denmark [14]. All SMRs were significantly elevated (p < 0.05). In a mixed sample of males and predominantly females, an SMR of 1.70 for AN (p < 0.05 for lifetime diagnosis and p > 0.05 for diagnosis at intake) was reported [9]. A meta-analysis of clinical studies including an unknown percentage of males computed an SMR of 5.86 for AN (p < 0.05) [15]. In females with AN, one group reported an SMR of 10.6 (p < 0.05) [16] and a national death register study [17] found an SMR of 4.37 (p < 0.05). Concluding from these data, males with AN carry a significantly increased risk of death from all causes compared to males from the general population. Compared to females with AN, however, there seems to be little difference in risk of death.
For BN, there is still less evidence than for AN on mortality in males. Quadflieg et al. [6] reported a CMR of 11.1% in male inpatients treated for BN. On the other hand, Powers and Spratt [18] reported no deaths in five males with BN after two years. An overview, combining a large number of study samples with a small fraction of males, reported a mean CMR of 0.32% [19]. In a mixed outpatient sample of 39 males and 867 females treated for BN, the overall CMR was 3.9% [9].
The SMR for BN was 1.88 (p > 0.05) in male inpatients [6] and 2.2 in males with BN in a register study (p > 0.05) [12]. In a mixed sample of outpatients, the SMR was 1.57 (p < 0.05) [9]. The meta-analysis of clinical studies including an unknown percentage of males reported an SMR of 1.93 for BN (p < 0.05) [15], while Huas et al. [20] reported an SMR of 5.52 (p < 0.05) for BN in a purely female sample. A non-significantly elevated SMR of 2.33 in females with BN was found in a national death register study [17]. From what little is known, males with BN carry no increased risk of death compared to males from the general population, and a lower risk of death than females with BN.
Regarding ED-NOS, Quadflieg et al. [6] reported a CMR of 6.4% in male inpatients, while in a mixed sample of 49 male and 753 female outpatients, Crow et al. [9] found a CMR of 5.2%. The SMR was 3.40 (p < 0.05) in Quadflieg et al.'s study [6], and 1.6 (p < 0.05) in males with ED-NOS in a register study [12]. In mixed samples, SMRs of 1.81 (p < 0.05) [9] and 1.92 (p < 0.05) [15] for ED-NOS were reported.
To draw valid conclusions on males from this scarce evidence is nearly impossible. As in females, mortality seems to be elevated in males with AN. The existing evidence on BN and ED-NOS points at non-elevated mortality in BN and elevated mortality in ED-NOS compared to males from the general population.
One more recent study addressed predictors of death in male AN, and no studies exist on prediction of premature death for BN and ED-NOS in males. Gueguen et al. [10] compared dichotomized variables between 20 living and three deceased male inpatients treated for AN and identified a higher age and lower body mass index (BMI) at admission, as well as restrictive AN as predictors of death. Interestingly, no purging behavior was found in deceased patients but in 75% of surviving patients (p < 0.05). However, the very small number of deceased patients makes interpretation of this finding difficult. In this study, long-term survival did not differ between sexes.
So far, no clinical study has compared males and females with AN, BN, or ED-NOS directly regarding mortality and predictors of premature death. This lack of data also impedes comparison between samples from different studies. In addition, studies differ greatly in terms of type of treatment, clinical setting, and the participants’ age at initiation of treatment. In our study, we tried to account for these potential confounders. We also extended the data collection to BN and ED-NOS.
In the present study, we use data from two prior studies [6, 21] to examine our research question. Fichter and Quadflieg [21] reported on mortality for a large sample of inpatients with AN, BN, and ED-NOS, but the data were not separated by sex. Their sample included inpatients admitted from 1985 to 2005, with post-treatment observations ending in 2012. Quadflieg et al. [6] assessed mortality rates in a large, purely male sample from the same hospital, with data collection for admission and post-treatment observations extending over a much longer time period than in the study on the mixed sex sample. Our aim in this study was a direct comparison of premature death in male and female inpatients with AN, BN, or ED-NOS who had received a conceptually identical inpatient treatment in the same clinical setting and during the same calendar years. A second aim was to identify predictors of premature death in this large prospective clinical sample.
Methods
Participants
The female participants of the present study were selected from the females of the mixed sample of Fichter and Quadflieg [21] and the male participants of the present sample were selected from the sample of Quadflieg et al. [6]. These samples are described in detail in the original publications. In short, all participants were treated as inpatients for their ED according to the guidelines for cognitive–behavioral psychotherapy on specialized units. Inclusion criteria were a treatment duration of at least 21 days and a filled-out package of questionnaires at admission. Patients with acute psychosis or severe alcohol/drug-related disorders were excluded from treatment by the admission policy of the hospital.
To make males and females comparable regarding admission and post-treatment observation period, we restricted our male sample to the same limits of admission (treatment 1985–2005) and observation period (ending 2012) as Fichter and Quadflieg [21]. These restrictions resulted in a male sample of 66 AN, 52 BN, and 70 ED-NOS participants with vital status recorded. The ascertainment of vital status in this sample reached 93.6% in AN, 97.6% in BN, and 91.7% in ED-NOS. From the mixed sample, all results for the females only were re-calculated for comparison. Sample size for the female participants was 2066 for AN, 1880 for BN and 1350 for ED-NOS. Figure 1 presents a flowchart of the samples.
Assessments
ED diagnoses according to the DSM-IV were computed by the standardized algorithm of the Structured Inventory for Anorexic and Bulimic Eating Disorders Self-rating Form (SIAB-S) [22]. This questionnaire covers a broad spectrum of symptoms usually associated with EDs and in 29 items covers all symptoms necessary for DSM-IV-ED diagnoses. In the validation sample, the diagnostic algorithm showed a PPV of 0.91, a sensitivity of 0.73, and a specificity of 0.63 [22]. Definition of ED-NOS followed the description of types 2–5 in the DSM-IV, (page 550): (1) AN with normal range BMI (upper limit 25); (2) BN with short duration or low frequency of symptoms; (3) Regular use of inappropriate compensatory behavior after consuming small amounts of food at normal weight; (4) Chewing and spitting out food. The fourth criterion of AN in the DSM-IV (amenorrhea) can only be met by females, and no alternative for males is provided. Thus, AN in males is identically defined to ED-NOS type 1 in females. To avoid assignment of the same symptoms to different diagnoses, we included ED-NOS type 1 in the AN category of females. Consequently, for both sexes, ED-NOS refers to types 2–5 as described in the DSM-IV. Patients also reported their BMI in the SIAB-S.
The early 64-item version of the Eating Disorder Inventory (EDI) [23] was used in this study. This questionnaire covers symptoms and psychological features of EDs in 64 items in eight subscales (Cronbach’s α for our sample in parentheses): drive for thinness (α = 0.84; 7 items), bulimia (α = 0.89; 7 items), body dissatisfaction (α = 0.90; 9 items), ineffectiveness (α = 0.88; 10 items), perfectionism (α = 0.76; 6 items), interpersonal distrust (α = 0.82; 7 items), interoceptive awareness (α = 0.79; 10 items), maturity fears (α = 0.76; 8 items). Answer format ranged from 1 (“always”) to 6 (“never”). As recommended by Garner et al. [23], for clinical samples, a recoded 0-to-3 format for answers was used for subscale building. Higher scores indicate more pathology.
General psychopathology was assessed by the nine subscales of the Brief Symptom Inventory (BSI) [24]: somatization (α = 0.81; 7 items), obsessive–compulsive symptoms (α = 0.83; 6 items), interpersonal sensitivity (α = 0.81; 4 items), depression (α = 0.86; 6 items), anxiety (α = 0.82; 6 items), anger–hostility (α = 0.71; 5 items), phobic anxiety (α = 0.76; 5 items), paranoid ideation (α = 0.76; 5 items), psychoticism (α = 0.73; 5 items) with higher values indicating more psychopathology. The answer format ranged from 0 (“not at all”) to 4 (“extremely”). The BSI comprises 53 items with four items not assigned to any subscale. These items were included in overall scores of the BSI which were not used in this study.
Individual characteristics of the patients were extracted from the hospital documentation: age at admission, age at onset of ED, duration of ED, legal status, partner situation, education, living situation, being a twin, and pre-treatment.
Design
The study included a baseline assessment at the time of inpatient treatment and a single outcome of death at follow-up. It was part of a larger study collecting extensive follow-up data as described in the prior studies [6, 21].
Procedure
As part of the admission routine, patients filled out a package of questionnaires including the EDI, SIAB-S and the BSI. They also provided the above-mentioned private information for the hospital documentation. Vital status at follow-up was ascertained by collecting information from close family members, registration agencies of the patient’s place of residence, or family doctors. Records are not updated by the authorities after moving permanently away from Germany, which was the main reason for failing ascertainment. Observation ended either with the return of the questionnaire or another contact to the patient, or with the end of all observations on December 1, 2012.
Statistical analysis
Descriptive results (means, standard deviations) with Levene tests for variance homogeneity and t-tests for sex differences are presented. Degrees of freedom were adjusted when the Levene test of variance homogeneity was significant (p < 0.05). Only cases with ascertained vital status entered the analyses. Crude mortality rate (CMR) is the percentage of deaths in the total or a subgroup of the sample [(Ndeceased/Nsample) × 100]. The standardized mortality ratio (SMR) was derived from dividing the number of recorded deaths by the number of expected deaths (SMR = Ndeceased/Nexpected). The expected number of deaths of the general German population, adjusted for age and sex, was extracted from the reports of the German Federal Office of Statistics [25]. An SMR greater than 1.0 indicates a higher number of deaths in patients than expected. SMRs and 95% confidence intervals were computed by PAMCOMP software [26]. A confidence interval including the value one indicates that the number of observed deaths does not differ significantly (p < 0.05) from the number of deaths expected in the general population. Overlapping confidence intervals indicate the lack of statistical significance (p > 0.05). The Kaplan–Meier method yielded data for survival curves, separately for males and females and diagnostic group, and log-rank tests compared males and females in each diagnostic group. A large number of potential predictors were available from the set of questionnaires completed by the patients at admission, and from the hospital documentation (see Fichter et al. [27]). Cox regression analyses yielded a hazard ratio (HR) for each predictor of survival time post treatment. HR indicates less likelihood to have a shorter time until death for values below one, no difference for a value of one, and a shorter time to death for values above one.
Results
In all diagnostic groups, males were older than females at admission to inpatient treatment. Females with AN and ED-NOS reported an earlier onset of ED than males; this difference was not significant in BN. The number of treatment days did not differ between males and females in all diagnostic groups (Table 1).
Characteristics of deceased patients and mortality rates
Table 1 (lower part) presents results on the deaths of males and females. No patient died during inpatient treatment. Over the follow-up observation period, 10 males with AN, 4 males with BN, and 3 males with ED-NOS died. The number of deaths in females was 105 in AN, 47 in BN, and 42 in ED-NOS. The CMRs ranged from 3 to 15%. Mean age at death was nearly identical in males and females with AN (36 years). Males with ED-NOS were younger at the time of death than females; however, the low number of deaths in males (N = 3) in this group impairs statistical power.
Elevated SMRs (p < 0.05) were found in males with AN, and in all three female diagnostic groups; SMRs in males with BN and ED-NOS were not elevated, with large confidence intervals in these groups. SMRs for AN indicated about five-fold increased risk for premature death in females and males. However, the sex comparisons of SMRs between the diagnostic groups did not reach significance (p > 0.05).
The sum of person-years was 576, 507, and 448 in males, and 20,723, 22,311, and 13,465 in females (AN, BN and ED-NOS, respectively). Number of deaths per 1000 person-years indicates incidence of death and was 17.36 (95% confidence interval 6.60–28.12) and 5.07 (4.10–6.04) in AN, 7.89 (0.16–15.62) and 2.11 (1.50–2.71) in BN, and 6.70 (0.88–14.28) and 3.12 (2.18–4.06) in ED-NOS (males and females, respectively). Again, males with AN and all female diagnostic groups showed increased death rates. Incidence of death was higher in males than females with AN (p < 0.05), but not in BN and ED-NOS.
Survival analysis
For each diagnostic group, survival analysis compared survival time post-treatment between males and females. Figure 2 shows the cumulative survival time from admission, separately for males and females with AN, BN, and ED-NOS. Long-term survival was shorter in males than in females with AN (χ2 = 15.41; p < 0.001) or BN (χ2 = 8.68; p < 0.01). In ED-NOS (χ2 = 2.48; p > 0.05), no sex difference was found.
Predictors
In preliminary analyses, predictors of survival time post treatment were grouped into three domains (individual characteristics during treatment, eating-specific symptoms, and general psychopathology), and a Cox regression on survival time post treatment was conducted separately for each domain. In addition to domain-specific predictors, each analysis included ED diagnosis, sex, and age at admission (which differed between males and females) as covariates. ED diagnosis, being male, higher age at admission, having a partner at the time of treatment, the number of previous inpatient treatments, EDI-Ineffectiveness, and four BSI subscales (Somatization, Obsessive–compulsive, Depression, Anger-hostility) emerged from preliminary analyses as possible significant (p < 0.05) predictors of survival time.
Significant predictors of survival time post treatment from the domain-specific analyses were included in the final Cox regression analysis on survival time post treatment with the same covariates as described above. Although body mass index (BMI) did not emerge as a significant predictor in domain-specific analyses, we retained BMI as predictor in the final model because of its relevance for most EDs. Entering these variables in one step into a final model revealed seven significant (p < 0.05) and four non-significant predictors. Being male showed a 2.5-fold risk of premature death and having been treated for AN versus BN or ED-NOS about doubled the risk of premature death. Higher BSI-Somatization and BSI-Depression scores increased the risk of premature death about 1.4-fold. Higher age and more inpatient treatments prior to index treatment also increased the risk of premature death, although the risk was somewhat lower (HR = 1.057 and 1.135). Higher BSI-Obsessive–compulsive scores decreased the risk of premature death by one-third. BMI, having a partner, EDI-Ineffectiveness, and BSI-Anger-hostility were no predictors of premature death (Table 2).
Discussion
We assessed crude and standardized mortality in a larger sample of males separately for AN, BN, or ED-NOS, and compared them to females with the same diagnoses and treated during the same time period and in the same hospital. In addition, we analyzed the time from admission to the time of death, and searched for predictors of premature death. Compared to the (general) reference population, mortality was elevated in males with AN, and in females with AN, BN and EDNOS. SMRs never differed significantly between the two sexes. Males with AN or BN died earlier than females with AN or BN. A diagnosis of AN, being male, higher age at hospital admission, more previous admissions, and more depression and somatization increased the risk for premature death, while more obsessive–compulsive symptoms decreased it.
In our study, SMRs for AN were highest (4.93 in males and 5.29 in females), indicating about five-fold increase in mortality due to all causes compared to the general population for both sexes equally. BN and ED-NOS showed considerably lower, and in males non-significant, SMRs. Compared to our study, Hoang et al. [12] reported a lower SMR (2.7) in males and a similar SMR (5.0) in females with AN. Møller-Madsen et al. [14] found higher SMRs in both sexes (8.2 in females and 9.2 in males with AN). As in our study, sex differences were not significant in either study. The mortality reported by Møller-Madsen et al. [14] referred to the time period between 1970 and 1987 and comprised all psychiatric admissions that included AN as a primary or secondary diagnosis in Denmark. Our treatment period began in 1985, and the study focuses on patients with a primary diagnosis of AN at admission to a hospital unit specialized in psychotherapy of EDs. Thus, a more homogeneous diagnostic cohort and different, possibly more focused treatment approaches may account for a lower mortality.
Like for AN, Hoang et al. [12] reported higher SMRs than in our study for BN (2.2 in males and 4.8 in females versus 1.42 and 1.57 in our study). Again, as in our study, sex differences for BN and ED-NOS did not reach significance. Several reasons may account for different findings in Hoang et al.’s and our study. Hoang et al.’s [12] sample consisted of patients who died within one year after discharge from inpatient treatment. For the time immediately following intensive inpatient therapy, a deterioration of symptoms was reported in parts of our sample [28, 29]. This may also indicate a time of increased risk of death, as patients leave the protective hospital environment from which they had benefited at a time when their ED was especially severe. Length of observation was considerably longer in our study and included time periods with a possibly lower risk of death.
No data on the number of deaths per person-years separately for males and AN, BN or ED-NOS are available in the literature. From a study on AN only [10], we computed 13 deaths per 1000 person-years for a rather small sample of male patients with AN, a number only slightly lower than our results. In a mixed sample of male and female patients, the number of deaths per 1000 person-years was 3.45 for AN, 2.71 for BN, and 3.28 for BED [30]. A meta-analysis including female only and mixed samples (there were no male only studies) reported the number of deaths per 1000 person-years as 5.10 for AN, 1.74 for BN and 3.31 for ED-NOS [15]. This meta-analysis also reported death rates for studies with females only with the number of deaths per 1000 person-years 5.39 for AN, and 2.22 for BN. In our study, death rates for males were higher than those reported in these two studies. A possible reason for this discrepancy is the condition of treatment. Suokas et al.’s [30] patients were mostly treated in an outpatient setting, and the meta-analysis [15] included patients from inpatient and outpatient settings, while our patients were exclusively inpatients. Samples in these studies consisted predominantly of females and no conclusive comparison can be made with our male sample.
Survival analysis suggested a shorter time from admission to death in males compared to females with AN. A survival analysis reported by Gueguen et al. [10] found no sex differences in long-term survival but a shorter 3-year survival time in males with AN after discharge from treatment. Our sample size of males was larger than Gueguen et al.’s [10] sample of 23 males with three deaths. In a statistical sense, the ten deaths in our male AN sample are still a low number of events. Both Gueguen et al.’s and our study compared relatively few males to a large number of females. As the confidence interval decreases when the sample size increases, the large confidence intervals in the male samples may have concealed sex differences. Clearly, at this time, results are still inconclusive and further research on much larger clinical male samples is desirable.
Nearly nothing is known on predictors of death in males with ED. Our male sample is large for a male ED sample, but still rather small for a broad search of predictors of death. Therefore, the results should be considered as preliminary. They constitute initial evidence and should encourage further research on predictors as soon as larger sample sizes with male ED patients will become available.
Being male increased the risk of premature death in AN but not in BN or ED-NOS. From our preliminary findings, it seems that across sexes and EDs, males with AN carry the highest risk of premature death from all causes. The existing CBT treatment is effective for both sexes [31], but there seem to be higher barriers to seek treatment in males [32], resulting in a more deadly outcome from all causes. The male reluctance to seek help with psychological problems early on can be observed in other diagnostic groups (e. g. depression [33]), too.
Higher age at admission constituted a predictor of a shorter time until death. This is similar to the findings of Gueguen et al. [10] who reported an age at admission of 26 or higher as a predictor of death in AN. Higher age may be an indicator of a more chronic condition that is associated with a decreased probability to respond to treatment. This would be supported by our finding that a higher number of previous inpatient treatments was associated with a shorter time to death. However, as the probability to die increases with age, the finding regarding age at admission could also simply reflect the natural course of life. In any case, the high SMR clearly points to a risk of all-cause death in AN beyond the natural course of life. We could not confirm the finding of purging behavior being a protective factor in males with AN [10], in fact, it did not emerge as predictor in either direction. In addition, general psychopathology subscales emerged as predictors of premature death. Higher depression and somatization scores plausibly increased the risk, while higher obsessive–compulsive scores decreased the risk of death. Possibly, being more obsessive–compulsive leads to more strict adherence to therapeutic recommendations and helps with avoiding the worst consequence of death.
There is an ongoing discussion on diagnosis of AN in males [34] with yet inconclusive results. At this time, it is not known if males need a specific treatment which is different from the treatment of females. Even our large sample (large for a sample of males with ED) may still have been too small to detect all significant and relevant differences between males and females. Such differences could be important to develop sex-specific intervention strategies. It seems that extant interventions are suitable for both sexes, but there is a need to make male patients with ED more comfortable in an environment where most patients are female [35].
Important limitations of our study are firstly that ED diagnoses were made at admission to treatment, and we have no knowledge on the further course of symptoms after discharge for those patients who died later on. Another limitation is that our samples originated from inpatients in one single hospital with a specialized treatment program. We have no evidence if and how this affects the generalizability of our findings. A third limitation is that males were mostly older than females at admission and exhibited a later onset of ED. The onset of illness also occurred later in the male sample of Gueguen et al. [10], and this probably reflects the sex-specific natural course of the ED. Higher age in itself may increase the risk of death; therefore, we controlled the influence of age in our analyses. In Cox regression analyses, age and sex were included as covariates, and in the computation of SMR, age and sex were standardized. However, we cannot dismiss the notion that the shorter survival time of males was primarily due to males being older than females. A further limitation is the use of a self-report for determining ED diagnoses at admission. However, for all ED diagnoses, we applied the well-validated [22] and empirically based standardized diagnostic algorithms for the SIAB-S. In addition, all patients were treated on units specialized for the treatment of ED and were pre-diagnosed by the external physician as having ED as primary diagnosis. A fifth limitation is that during the years of assessment for this study decades ago, a detailed concept of the “drive for muscularity” in men did not exist. We, therefore, cannot comment on this more recent issue. A final limitation is our not being able to collect causes of death and their connection to ED symptoms. There are no central registers for causes of deaths in Germany, and such information is rarely available from other sources.
On the other hand, our study has several important strengths: The first strength is that our sample size was large for a study on males with ED. Additionally, all ED diagnoses including ED-NOS were defined strictly according to the DSM-IV. A third strength is that by combining data of males and females from the same hospital, we could provide a direct sex comparison in a homogeneous sample from the same treatment period and for a similar follow-up period. A further strength is we being able not only to report on sample size-dependent crude mortality, but also on SMRs that allow comparison to the normal reference population of the same sex and age. A final strength is the very high ascertainment rate of vital status (89–96%). This index is rarely reported in the ED literature.
Conclusion
SMR in ED is high in males and females, especially in AN. No significant differences of SMR between males and females emerged in our study. Survival after treatment for AN was shorter for males than for females. Sample size was larger than in other studies but possibly still not large enough for detecting small differences between males and females. Such differences can be highly relevant for effective treatment planning. From our results, it seems that EDs are not too different in terms of mortality rates in males and females, and our results allow the important conclusion that males need the same intensive treatment as females with an ED. This applies especially to the dangerous process of developing AN and remaining in this disease condition for years. Our research referred to patients with ED diagnoses according to the DSM-IV. Meanwhile, the DSM-5 was published. It modified the diagnostic criteria moderately and added new ED diagnoses. Future research should address mortality in prospective studies of DSM-5 EDs.
What is already known on this subject?
Mortality in males and females with ED is higher than in the general population, especially for AN. For BN and ED-NOS no direct comparison of mortality between sexes exists.
What this study adds
Our study adds a direct comparison of mortality in males and females with AN, BN, or ED-NOS treated at the same hospital in the same calendar years. From our data no sex differences emerged.
Data availability
Data available from the authors on qualified request.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Arlington
American Psychiatric Association (1994) Diagnostic and statistical manual for mental disorders, 4th edn. American Psychiatric Association, Washington, DC (DSM-IV)
Hudson JI, Hiripi E, Pope HG Jr, Kessler RC (2007) The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biol Pychiatry 61:348–358. https://doi.org/10.1016/j.biopsych.2006.03.040
Jacobi F, Höfler M, Strehle J, Mack S, Gerschler A, Scholl L, Busch MA, Maske U, Hapke U, Gaebel W, Maier W, Wagner M, Zielasek J, Wittchen H-U (2014) Psychische Störungen in der Allgemeinbevölkerung. Nervenarzt 85:77–87. https://doi.org/10.1007/s00115-013-3961-y
Strobel C, Quadflieg N, Voderholzer U, Naab S, Fichter MM (2018) Short- and long-term outcome of males treated for anorexia nervosa: a review of the literature. Eat Weight Disord 23:541–552. https://doi.org/10.1007/s40519-018-0538-6
Quadflieg N, Strobel C, Naab S, Voderholzer U, Fichter MM (2019) Mortality in males treated for an eating disorder—a large prospective study. Int J Eat Disord 52:1365–1369. https://doi.org/10.1002/eat.23135
Burns T, Crisp AH (1984) Outcome of anorexia nervosa in males. BJPsych 145:319–325. https://doi.org/10.1192/bjp.145.3.319
Steinhausen HC (2002) The outcome of anorexia nervosa in the 20th century. Am J Psychiatry 159:1284–1293. https://doi.org/10.1176/appi.ajp.159.8.1284
Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, Mitchell JE (2009) Increased mortality in bulimia nervosa and other eating disorders. Am J Psychiatry 166:1342–1346. https://doi.org/10.1176/appi.ajp.2009.09020247
Gueguen J, Godart N, Chambry J, Brun-Eberentz A, Foulon C, Divac SM, Huas C (2012) Severe anorexia nervosa in men: comparison with severe AN in women and analysis of mortality. Int J Eat Disord 45(4):537–545. https://doi.org/10.1002/eat.20987
Crisp A et al (2006) Death, survival and recovery in anorexia nervosa: a thirty five year study. Eur Eat Disord Rev 14:168–175. https://doi.org/10.1002/erv.704
Hoang U, Goldacre M, James A (2014) Mortality following hospital discharge with a diagnosis of eating disorder: national record linkage study, England, 2001–2009. Int J Eat Disord 47(5):507–515. https://doi.org/10.1002/eat.22249
Kask J, Ramklint M, Kolia N, Panagiotakos D, Ekbom A, Ekselius L, Papadopoulos FC (2017) Anorexia nervosa in males: excess mortality and psychiatric co-morbidity in 609 Swedish in-patients. Psychol Med 47:1489–1499. https://doi.org/10.1111/j.2044-8341.1986.tb02676.x
Møller-Madsen S, Nystrup J, Nielsen S (1996) Mortality in anorexia nervosa in Denmark during the period 1970–1987. Acta Psychiatr Scand 94:454–459. https://doi.org/10.1111/j.1600-0447.1996.tb09890.x
Arcelus J, Mitchell AJ, Wales J, Nielsen S (2011) Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psychiatry 68(7):724–731. https://doi.org/10.1001/archgenpsychiatry.2011.74
Huas C, Caille A, Godart N, Foulon C, Pham-Scottez A, Divac S, Falissard B (2011) Predictors of ten-year mortality in severe anorexia nervosa patients. Acta Psychiatr Scand 123:62–70. https://doi.org/10.1111/j.1600-0447.2010.01627.x
Franko DL, Keshaviah A, Eddy KT, Krishna M, Davis MC, Keel PK, Herzog DB (2013) A longitudinal investigation of mortality in anorexia nervosa and bulimia nervosa. Am J Psychiatry 170:917–925. https://doi.org/10.1176/appi.ajp.2013.12070868
Powers PS, Spratt EG (1994) Males and females with eating disorders. Eating Disorders 2:197–214. https://doi.org/10.1080/10640269408249116
Steinhausen HC, Weber S (2009) The outcome of bulimia nervosa: findings from one-quarter century of research. Am J Psychiatry 166:1331–1341. https://doi.org/10.1176/appi.ajp.2009.09040582
Huas C, Godart N, Caille A, Pham-Scottez A, Foulon C, Divac SM, Rouillon F (2013) Mortality and its predictors in severe bulimia nervosa patients. Eur Eat Disorders Rev 21:15–19. https://doi.org/10.1002/erv.2178
Fichter MM, Quadflieg N (2016) Mortality in eating disorders—results of a large prospective clinical longitudinal study. Int J Eat Disord 49:391–401. https://doi.org/10.1002/eat.22501
Fichter MM, Quadflieg N (2000) Comparing self- and expert rating: A self-report screening version (SIAB-S) of the Structured Interview for Anorexic and Bulimic Syndromes for DSM-IV and ICD-10 (SIAB-EX). Eur Arch Psychiatry Clin Neurosci 250:175–185. https://doi.org/10.1007/s004060070022 (diagnostic algorithm available at https://www.klinikum.uni-muenchen.de/Klinik-und-Poliklinik-fuer-Psychiatrie-und-Psychotherapie/de/forschung/forschungsfelder/essstoerungen/evaluation/SIAB/index.html)
Garner DM, Olmstedt MP, Polivy J (1983) Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eat Disord 2:14–34. https://doi.org/10.1002/1098-108X(198321)2:2<15:AID-EAT2260020203>3.0.CO;2-6
Derogatis LR, Melisaratos N (1983) The brief symptom inventory: an introductory report. Psychol Med 13:595–605. https://doi.org/10.1017/S0033291700048017
German Federal Office of Statistics, Mortality figures. https://www.destatis.de/DE/Publikationen/Thematisch/Bevoelkerung/Bevoelkerungsbewegung/PeriodensterbetafelnPDF_5126202.pdf?__blob=publicationFile, Accessed 6 December 2018.
Taeger D, Sun Y, Keil U, Straif K (2000) A stand-alone Windows application for computing exact person-years, standardized mortality ratios and confidence intervals in epidemiological studies. Epidemiology 11:607–608. https://doi.org/10.1097/00001648-200009000-00019
Fichter MM, Quadflieg N, Crosby RD, Koch S (2017) Long-term outcome of anorexia nervosa—results from a large clinical longitudinal study. Int J Eat Disord 50:1018–1030. https://doi.org/10.1002/eat.22736
Fichter MM, Quadflieg N (1997) Six-year course of bulimia nervosa. Int J Eat Disord 22:361–384. https://doi.org/10.1002/(SICI)1098-108X(199712)22:4<361:AID-EAT2>3.0.CO;2K
Fichter MM, Quadflieg N (1999) Six-year course and outcome of anorexia nervosa. Int J Eat Disord 26:359–385. https://doi.org/10.1002/(SICI)1098-108X(199912)26:43.3.CO;2-Z
Suokas JT, Suvisaari JM, Gissler M, Löfman R, Linna MS, Raevuori A, Haukka J (2013) Mortality in eating disorders: a follow-up study of adult eating disorder patients treated in tertiary care, 1995–2010. Psychiatry Res 210:1101–1106. https://doi.org/10.1016/j.psychres.2013.07.042
Fernández-Aranda F, Krug I, Jiménez-Murcia S, Granero R, Núñez A, Penelo E, Solano R, Treasure J (2009) Male eating disorders and therapy: a controlled pilot study with one year follow-up. J Behav Ther Exp Psychiatry 40:479–486. https://doi.org/10.1016/j.jbtep.2009.06.004
Griffiths S, Mond JM, Li Z, Gunatilake S, Murray SB, Sheffield J, Touyz S (2015) Self-stigma of seeking treatment and being male predict an increased likelihood of having an undiagnosed eating disorder. Int J Eat Disord 48:775–778. https://doi.org/10.1002/eat.22413
Smith KLW, Matheson FI, Moineddin R, Dunn JR, Lu H, Cairney J, Glazier RH (2013) Gender differences in mental health service utilization among respondents reporting depression in a national health survey. Health 5:1561–1571. https://doi.org/10.4236/health.2013.510212
Murray SB, Griffiths S, Mond JM (2016) Evolving eating disorder psychopathology: conceptualising muscularity-oriented disordered eating. Brit J Psychiatry 208:414–415. https://doi.org/10.1192/bjp.bp.115.168427
Kinnaird E, Norton C, Pimblett C, Stewart C, Tchanturia K (2019) “There’s nothing there for guys”. Do men with eating disorders want treatment adaptations? Qual Study Eat Weight Disord 24:845–852. https://doi.org/10.1007/s40519-019-00770-0
Acknowledgements
We thank the Christina Barz Stiftung and the Swiss Anorexia Nervosa Foundation (SANS grant no. 51-15) for supporting this study. We also thank all the members of the project staffs who were involved in data collection and management.
Funding
The study was funded by the Christina Barz-Stiftung and the Swiss Anorexia Nervosa Foundation (SANS Grant no. 51–15).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was reviewed and approved by the Ethics Committee of the Bavarian Medical Association (No. 16033). All procedures were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The article is part of the Topical Collection on Males and Eating and Weight Disorders.
Rights and permissions
About this article
Cite this article
Fichter, M.M., Naab, S., Voderholzer, U. et al. Mortality in males as compared to females treated for an eating disorder: a large prospective controlled study. Eat Weight Disord 26, 1627–1637 (2021). https://doi.org/10.1007/s40519-020-00960-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-020-00960-1