Abstract
Purpose
To explore the relationship between body weight status and neurocognitive functioning in soldiers.
Methods
U.S. soldiers (N = 109) answered survey questions and completed neurocognitive tests including simple reaction time, code substitution, procedural reaction time, go–no–go, matching to sample, code substitution recall, and four versions of the Stroop test including congruent (color and meaning of word agreed); incongruent (color and meaning of word differed); neutral (nonsense words appeared), and emotional (combat-related words such as “I.E.D” and “convoy” appeared). Self-reported heights and weights were used to calculate BMI. A BMI ≥ 30.00 kg/m2 was categorized as obese. Multivariate analysis of variance was used to analyze weight status differences (p ≤ 0.05) across neurocognitive variables. Binomial logistic regression analysis with obesity as the dependent variable was used to ascertain the contributions (p ≤ 0.05) of exercise and the neurocognitive measures that differed based on weight status.
Results
Twenty-nine participants (26.6%) were obese. The obese group had significantly lower scores on code substitution, and both neutral and emotional Stroop tasks. Only Stroop emotional scores, p = 0.022, OR = 0.97, and frequency of moderate/intense physical activity, p = 0.009, OR = 0.10, were significant predictors of weight status.
Conclusions
Obesity was associated with less frequent moderate/intense physical activity and compromised executive functioning, namely decrements in response inhibition. Given the design and sample size, additional research is needed to better understand the direction of the relationship between these variables and to inform research related to the treatment and prevention of obesity within military populations.
Level of evidence
Level III, case-control analytic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With 13% of the world adult population classified as obese, the prevalence of obesity is an important global health concern [1]. This concern has grown as the worldwide prevalence of obesity has increased nearly threefold since 2016 [1]. While adult obesity rates vary among the global regions, the rates are particularly high in the U.S. where 37% of adults are classified as obese [2]. Although the reported rate of obesity among military service members is lower than that of the overall U.S. adult population, obesity is nevertheless a concern for the military. Between 1995 and 2008, combined rates for overweight and obesity among active duty personnel rose from 50.6 to 60.8%, with most of this change due to an increase in the rates of obesity from 5.0 to 12.7% [3]. More recently, data from the 2015 Health Related Behaviors Survey suggest a continuation of this trend with an obesity rate of 14.7% among U.S. active duty personnel [4]. According to this survey, the Army, with an obesity rate of 18.0%, has the highest obesity rate among the branches of the armed services.
The primary concern about obesity in military service members is reduced force readiness. Military service is innately demanding, and body composition standards are thought to play an integral role with regard to physical fitness, overall health, and maintaining a military appearance [5]. A body mass index (BMI) of 30 kg/m2 or greater increases the risk of premature discharge from the Army [6]. In 2006, an estimated 1,200 first-term military service enlistees were prematurely discharged as a result of their failure to meet weight standards, and the cost associated with the early separation of these individuals was an estimated $61 million [7]. Compared to those with a normal BMI, soldiers who are obese have a 33% greater risk of lower extremity musculoskeletal injury or disorder (e.g., sprains, stress fractures, joint derangements, osteoarthritis) [8]. Service member with excessive body fat face an increased risk of heat injury [9], and those who are obese are twice as likely to fail their fitness readiness tests when compared to non-obese service members [10]. National security concerns have even been raised [11], as the U.S. armed services appear to be struggling to recruit eligible individuals who meet weight stands amidst the obesity epidemic [12, 13].
In addition to military-specific concerns, there are also concerns for the overall health of service members. An analysis of data from the Millennium Cohort Study, a large prospective study of service members and former service members, found that obesity was associated with hypertension, diabetes, sleep apnea, and coronary heart disease [14]. Within this study, those with obesity were also more likely to screen positive for depression and PTSD compared to participants with a normal body weight. A more recent study found the prevalence of prediabetes and diabetes to be increased among U.S. Air Force members with a BMI ≥ 30 [15].
There is a growing body of evidence suggesting an important relationship between body weight status and cognitive functioning [16]. A review by Smith et al. [17] found a clear association between obesity and neurocognitive deficits, particularly in executive functioning. Executive functions are a family of higher-order cognitive processes used in overriding instinct and in taking goal-directed action [18, 19]. Although there are three primary executive functions, namely cognitive inhibition, working memory, and cognitive flexibility [19], there are various approaches to measure each. Obesity is associated with deficits in numerous executive function outcomes, including inhibition, cognitive flexibility, working memory, decision-making, verbal fluency, and planning [16]. Among girls, poor executive function predicts greater increases in BMI from age 10 to 16 [20]; whereas, better working memory was found to predict a greater weight loss among individuals participating in a weight loss program [21]. Further, cognitive remediation therapy which targets executive functions and thinking style is linked with greater decreases in binge eating and weight loss [22]. Overall, executive functions appear to play a crucial role in regulating behaviors related to one’s BMI.
Relative to what is known regarding the relationship between neurocognitive function and body weight status within the general population, the topic remains essentially uncharted within the military. To better understand the relationship between obesity and neurocognitive function among service members, an analysis of the variables related to these constructs was performed using data collected as part of a cross-sectional study designed to investigate the relationship between lifestyle factors and psychological resilience among deploying U.S. soldiers. We hypothesized that obese soldiers will have significantly lower scores in executive functioning compared to non-obese soldiers.
Method
Subjects
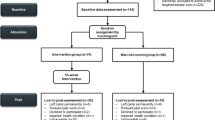
Data from a previous study to investigate the relationship between lifestyle factors and psychological resilience [23] were used for the analyses in the present study. Because of operational time constraints, not all participants in the original study were able to complete the neurocognitive assessment necessary for inclusion in the present study. Of the 260 Soldiers included in the original study, only 109 provided the data necessary for the present study. For two independent samples, based on a modest obesity prevalence rate in the U.S. of 31.8%, a total sample size of 65 would have provided sufficient power (95%) for detecting superiority in mean scores (two tailed) between groups with an alpha Type I error rate of 5% (0.05) and beta Type II error rate of 20% (0.20) [24]. Based on this sample size calculation, our sample of 109 participants (non-obese, n = 79 vs obese, n = 29) would have been sufficiently powered to reject the null hypothesis.
Participants were from two different brigade combat teams scheduled for deployment to Iraq between 2009 and 2010. Participants provide written informed consent. Compensation was not offered. Data collection occurred at the brigade combat teams’ Soldier Readiness Processing sites. The protocol was conducted in accordance with the Declaration of Helsinki and approved by the Committee on Research Involving Human Subjects, Institutional Review Board, at Kansas State University.
Materials
Demographic characteristics, health-related behaviors
Height, weight, demographic characteristics and health-related behaviors were self-reported using a questionnaire. A “fill-in-the-black” format was used to record height, weight, and age in years. Education level, sex, and race/ethnicity were measured using response option categories as reported in an earlier study describing the neuropsychological performance of an active duty military sample [25]. Smoking status was measured by asking, “Which of the following best describes your smoking habits?” and providing the following response options: “never smoked”, “current smoker”, or “ex-smoker”. Alcohol use was measured by asking, “Which of the following best describes your usual alcohol consumption during the last week?” and providing the following response options: “none”, “less than one drink per day”, “1–2 drinks per day”, “3–4 drinks per day”, and “more than 4 drinks per day”. Physical activity was measured using a question developed to take into account regular soldier physical training (i.e., PT). Participants were asked, “During the last 6 months, how many days per week have you done moderate or intense physical activities (including PT) for at least 10 minutes at a time?” with response options including “0”, “1”, “2–3”, and “4 or more.”
Neurocognitive battery
Neurocognitive functioning was measured using the Combat Stress Assessment [26], which was administered on a handheld computer. The cognitive tasks included, simple reaction time, code substitution, procedural reaction time, go–no–go, matching to sample, code substitution recall, and several versions of the Stroop test. Performance was quantified using throughput scores [27].
-
a.
For simple reaction time, a symbol appears on the screen and participants respond by tapping the symbol as quickly as possible.
-
b.
For code substitution, a key of symbols and numbers appear on the screen. A symbol and number pair also appears on the screen below the key. Participants respond by indicating whether or not the symbol and number pair matched the key.
-
c.
For procedural reaction time, numbers appear on the screen and participants respond by tapping the box that corresponded to each of the numbers.
-
d.
For go–no–go, an asterisk or a plus sign appears on the screen and participants respond by tapping the screen when the asterisk appears or not tapping the screen when the plus sign appears.
-
e.
For matching to sample, a pattern appears on the screen briefly. Participants are then presented with two patterns and respond by tapping the pattern that that matches the initial pattern.
-
f.
For code substitution recall, a number and symbol pair appear on the screen and participants indicate whether or not the pair match the key they were provided in the code substitution test.
-
g.
The Stroop test consist of a series of words of various colors appearing on the screen. Participants are instructed to respond to the words by tapping the color rather than the meaning of each word. Four different versions of the Stroop test were administered including the congruent version (color and meaning of word agreed), the incongruent version (color and meaning of word differed), the neutral version (nonsense words appeared), and the emotional version (combat-related words such as “I.E.D” and “convoy” appeared).
Statistical analysis
The data were analyzed using SPSS version 25.0 (IBM, Armonk, NY). Using the standard mathematical formula, weight (kg) / [height (m)]2 [28], BMI was calculated using the height and weight as recorded on the self-administered questionnaire. Body weight status was categorized as either obese (BMI ≥ 30 kg/m2) or non-obese (BMI ≤ 29.99 kg/m2) [29].
Descriptive analyses were performed to characterize the sample. Demographic and health-related behavior responses were collapsed into meaningful categories to allow for comparison of body weight status (i.e., obese vs non-obese) using Chi-square tests (Χ2). Data were inspected for the appropriate assumptions for the statistical test used. Fisher’s exact test values were examined in instances where the Chi-square expected cell counts were less than five. Multivariate analysis of variance (MANOVA) with Bonferroni adjusted pairwise comparisons was used to analyze body weight status differences across neurocognitive variables. Binary logistic regression analysis with backwards elimination (Wald) was used to ascertain the contribution of the frequency of weekly moderate-to-intense exercise (dummy coded) and scores on neurocognitive measures for which there were significant differences based on body weight category. Removal of variables from the regression analysis was based on a significance of p < 0.10; while, two-tailed tests and a significance level of p < 0.05 were used for all analyses.
Results
Sample characteristics
The majority of the participants were male (92.7%; n = 101) and married (56.9%; n = 62). Roughly, two-thirds (68.8%; n = 75) identified themselves as non-Hispanic Caucasian. The majority had not attained a college degree (72.5%; n = 79). Age in years ranged from 19 to 50 with a mean age of 29.0 (95% CI [27.6–30.5]). Few were current smokers (27.5%; n = 30), and few reported regularly consuming more than two alcoholic drinks per day (11.0%; n = 12). Sixty percent (59.6%; n = 65) reported completing moderate-to-intense physical activity four or more days per week. Additional sample characteristics are summarized in Table 1.
Body weight status
The BMIs ranged from 18.9 to 37.7 kg/m2 with a mean BMI of 27.4 kg/m2 (95% CI [26.7–28.2]). The prevalence of obesity was 26.6% (n = 29). Participants who reported moderate-to-intense physical activity two or more times per week were less likely to be classified as obese compared to those reporting less frequent physical activity, p = 0.004 Fisher's exact test. Body weight status did not differ significantly based on sex (p = 1.0 Fisher’s exact test), age (≤ 24, 25–32, or ≥ 33 years of age, p = 0.131), ethnic/racial category (non-Hispanic Caucasian or all others, p = 0.625), education level (college degree or less, p = 0.993), smoking status (current smoker, former smoker, or non-smoker, p = 0.882), marital status (married or not, p = 0.125), or alcohol use (one or more drinks per day or less than one drink per day p = 0.533).
Group differences in neurocognitive functioning
The results of the MANOVA for neurocognitive measure differences based on body weight status were significant, F(10) = 1.99, p = 0.043, ηp2 = 0.17 (Wilk’s Lambda), and there were no violations in homogeneity of variance, (Levene’s test, p > 0.05). There were significant group differences in throughput scores on the neutral, p = 0.023, and emotional, p = 0.013, versions of the Stroop, but not the congruent, p = 0.114, or incongruent versions, p = 0.176. In addition, there were significantly group differences in throughput scores on only one other subtest of the Combat Stress Assessment, the code substitution task, p = 0.020, but not simple reaction time, procedural reaction time, go–no–go, matching to sample, or code substitution recall. The results of pairwise comparisons (Bonferroni adjusted) revealed that scores on these subtests were significantly lower for the obese group compared to the non-obese group, p < 0.05 (Table 2).
Using a one-way ANOVA, there were no significant differences in cognitive scores between body weight categories in the frequency of weekly moderate-to-intense exercise (1 vs. 2–3 vs. 4 or more times per week), p > 0.05.
Associations between body weight status and measures of executive function
A binomial logistic regression analysis was performed with obesity as the dependent variable and physical activity and each of the neurocognitive tests for which there were significant differences based on weight status category. The results indicated that the model was significant; Χ2(5) = 15.18, p = 0.010, and accounted for approximately 19% of the variance (Nagelkerke R2 = 0.19) and correctly classified 73% of the participants. After extraction, only emotional Stroop scores, Wald Χ2(1) = 5.22, p = 0.022, B = − 0.04, and frequency of moderate-to-intense physical activity, Wald Χ2(1) = 6.85, p = 0.009, B = − 2.27, were significant predictors of weight status. The results suggest that when all other variables are held constant, with a unit increase in the frequency of weekly moderate-to-intense physical activity (greater than 1 × weekly), the odds of being obese is reduced by 0.10 times or 90% (OR = 0.10, 95% CI [0.02, 0.57]). The results also suggest, when all other variables are held constant, the odds of being obese is reduced by 0.97 times or 3% (OR = 0.97, 95% CI [0.94, 1.00]) with every unit increase on the emotional Stroop which for the full sample had a standard deviation of 16.14 points. Overall, the results suggest an inverse relationship between BMI status and both measures of executive functioning and frequency of exercise.
Discussion
In the current study, we found that U.S. soldiers who are categorized as obese compared to non-obese have poorer performance on tasks of executive functioning, namely both the neutral and emotional Stroop tests and the code substitution test, which supported our hypothesis. More specifically, those who were categorized as obese had lower scores in cognitive inhibition. The results also revealed that the odds of being obese was reduced by 3% with each unit increase on the emotional Stroop test. More impressively, increasing the frequency of moderate-to-intense exercise to greater than one time weekly reduced the odds of being obese by 90%.
Most certainly, obesity is linked to lifestyle factors, and the lifestyle changes concomitant with military service have been shown to be associated with a reduction in BMI and weight loss among overweight and obese individuals [30]. The results of the current study revealed that increasing the frequency of moderate-to-intense exercise weekly reduces the odds of being obese by 90%. This is consistent with earlier findings in which increased physical activity has been shown to be independently associated with lower fat mass [31]. As such, findings such as those presented in the present study support the importance of the Dietary Guidelines for Americans highlighting the need for regular physical activity in weight maintenance [32].
Measures of self-regulation of eating and physical activity have been found to be lower among obese individuals [33], and an increasing number of studies are finding an association between executive function and obesity-related behaviors. Cross-sectional surveys have shown impulsivity, measured by delay discounting, positively associated with frequent fast-food consumption [34] and symptoms of attention deficit hyperactivity disorder which are believed to arise from a deficit in executive functioning [35] positively associated with symptoms of binge eating [36]. Likewise, consumption of fruit and vegetables as well as saturated fat has been shown to be associated with various measures of executive function [37, 38].
Exercise has been shown to improve executive function in overweigh children [39] and children with attention deficit hyperactivity disorder [40]. In contrast, in the current study, we did not observe significant differences in cognitive scores between groups based on the frequency of weekly moderate-to-intense physical activity. While Guiney & Machado [41] outlined evidence supporting the cognitive benefits of regular exercise in healthy older adult, they point out the need for additional research to distinguish the cognitive benefits of exercise in young adults.
Although this study is unique in that it is the first to note this occurrence within a military population, the finding of an association between obesity and compromised executive functioning is consistent with a growing body of evidence [16]. A review by Smith et al. [17] found a clear association between obesity and deficits of executive function; however, the nature of the relationship remained unclear with the authors citing evidence suggesting several possibilities including: (a) obesity may be responsible for cognitive deficits, (b) cognitive deficits may contribute to the propensity for obesity, or (c) obesity and cognitive deficits may be linked by a shared genetic predisposition which can be triggered by lifestyle factors.
The cross-sectional design of the study is a limitation, as no causal or directional effect can be inferred. While the current study findings appear to build on what is known in general, research is needed to better understand the relationship between executive function and body weight among military personnel. Although body weight status classification estimates based on self-reported heights and weights were similar to those based on measured values for young adults [42], the use of self-reported anthropometric data to determine body weight status should be considered a potential limitation. In addition, while the cut-point used in this study is well established [29], the use of BMI to categorize service members as obese or non-obese is not without potential concerns [43]. Nonetheless, BMI has been shown to be an accurate discriminator for the classification of obesity among service members based on percent body fat [44].
The use of self-reported health behaviors, including a measure of physical activity that has not been validated in a military population is also a limitation of the study. Lastly, the use of data from a previous study is a limitation. While differences between samples is a potential concern, the demographic characteristics of the participants in the present study were similar to those of the original study [23] as well as in earlier studies involving soldiers. In the present study, 92.7% were male, 56.9% were married, and the mean age was 29.0 years. In the original study [23], 90.8% of the participants were male, 55.8% were married, and the mean age was 29.0 years. In an earlier study of 88,235 soldiers, Milliken et al. [45] reported a sample in which 90.8% of the participants were male, 58.2% were married, and the mean age was 30.4 years. Overall, a strength of the study is that it appears the sample of soldiers in the present study is characteristic of the parent study as well as the larger population of soldiers. Additional strengths of the study include the use of a validated battery of tests [26] to assess neurocognitive functioning and the inclusion of an array of demographic variables. Being the first study to explore executive function and obesity with a military population adds to the strengths of the study as well.
The findings of this study should not be interpreted without consideration of the main ideas that comprise the Healthy at Every Size (HAES) paradigm. Developed as a means to conceptualize overall health independent of body weight, HAES encourages body acceptance, an intuitive or non-diet approach to eating, and a reasonable outlook regarding physical activity [46]. Weight stigma is associated with eating pathologies [47], and the concepts of HAES have proven their worth especially among female populations [48], including within a randomized controlled trial in which HAES interventions were found to decrease eating disinhibition [49].
The military population is predominately male, and male service members report eating for physical rather than emotional reasons [50]. Nonetheless, efforts to meet military weight requirements include unhealthy and extreme weight loss strategies [51]; while, normal body weight status among service members has been found to be associated with greater reliance on internal hunger and satiety cues [50]. Yet, restrained eating may not necessarily be detrimental [52]. A recent review concluded that military weight management interventions can be effective [53]. Although a full HAES approach has not been explored within the military, research exploring the intuitive or non-diet approach appears promising. While there are clearly military-specific risks associated with obesity, the “weight loss at any cost” mindset can result in unfavorable results as well.
Given the rising prevalence of obesity in the military, the results of this study are important in and of themselves. However, executive functions can be improved [19] and recent clinical studies have found that executive function training can foster weight loss. For example, Allom et al. [54] showed that patients receiving Cognitive Remediation Therapy achieved higher executive function scores, reduced habitual sedentary behavior, and potentially reduced habitual unhealthy eating.
In all, the finding of an association between obesity and executive functions is consistent with a growing body of evidence. Future studies are needed and should include researcher-measured anthropometric values and validated measures of physical activity. Studies designed to better understand the direction of the variable associations are also needed to establish better insight and to inform research related to the treatment and prevention of obesity within military populations.
What is already known on this subject?
An important relationship exists between body weight and cognitive functioning. In particular, decrements related to executive function are associated with less favorable body weight measurements.
What this study adds?
Among U.S Soldiers, obesity was associated with less frequent moderate-to-intense physical activity and compromised executive functioning, namely decrements in response inhibition.
Data availability
The dataset analyzed during the current study is available in the ResearchGate repository at https://www.researchgate.net/publication/331609207_EWD_DATA_SET.
References
World Health Organization (2018) Noncommunicable diseases country profiles 2018. Licence: CC BY-NC-SA 3.0 IGO. https://www.who.int/nmh/publications/ncd-profiles-2018/en/. Accessed 5 Feb 2020
Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL (2016) Trends in obesity among adults in the United States, 2005 to 2014. JAMA 315(21):2284–2291. https://doi.org/10.1001/jama.2016.6458
Reyes-Guzman CM, Bray RM, Forman-Hoffman VL, Williams J (2015) Overweight and obesity trends among active duty military personnel: a 13-year perspective. Am J Prev Med 48(2):145–153. https://doi.org/10.1016/j.amepre.2014.08.033
Meadows SO, Engel CC, Collins RL, Beckman RL, Cefalu M, Hawes-Dawson J, Doyle M, Kress AM, Sontag-Padilla L, Ramchand R, Williams KM (2015) Department of Defense Health Related Behaviors Survey (HRBS). https://www.rand.org/pubs/research_reports/RR1695.html. Accessed 8 March 2019
United States Department of Defense (2004) DOD physical fitness and body fat program. https://ndri.org/docs/DoDD%201308.1%20DoD%20Physical%20Fitness%20and%20Body%20Fat%20Program.pdf. Accessed 8 March 2019
Packnett ER, Niebuhr DW, Bedno SA, Cowan DN (2011) Body mass index, medical qualification status, and discharge during the first year of US Army service. Am J Clin Nutr 93(3):608–614. https://doi.org/10.3945/ajcn.110.007070
Dall TM, Zhang Y, Chen YJ et al (2007) Cost associated with being overweight and with obesity, high alcohol consumption, and tobacco use within the military health system's TRICARE prime-enrolled population. Am J Health Promot 22(2):120–139. https://doi.org/10.4278/0890-1171-22.2.120
Hruby A, Bulathsinhala L, McKinnon CJ, Hill OT, Montain SJ, Young AJ, Smith TJ (2016) BMI and lower extremity injury in US army soldiers, 2001–2011. Am J Prev Med 50(6):163–171. https://doi.org/10.1016/j.amepre.2015.10.015
Bedno SA, Urban N, Boivin MR, Cowan DN (2014) Fitness, obesity and risk of heat illness among army trainees. Occup Med 64(6):461–467. https://doi.org/10.1093/occmed/kqu062
Gantt CJ, Neely JA, Villafana IA, Chun CS, Gharabaghli SM (2008) Analysis of weight and associated health consequences of the active duty staff at a major naval medical center. Mil Med 173(5):434–440. https://doi.org/10.7205/MILMED.173.5.434
Maxey H, Bishop-Josef S, Goodman B (2018) Unhealthy and unprepared. https://strongnation.s3.amazonaws.com/documents/484/389765e0-2500-49a2-9a67-5c4a090a215b.pdf. Accessed 8 March 2019
Dickstein C (2018) Army misses 2018 recruiting goal, which hasn't happened since 2005. Stars and Stripes. Sep 21, 2018. https://search.proquest.com/docview/2110404816. Accessed 8 March 2019
Hsu LL, Nevin RL, Tobler SK, Rubertone MV (2007) Trends in overweight and obesity among 18-year-old applicants to the United States military, 1993–2006. J Adolesc Health 41(6):610–612. https://doi.org/10.1016/j.jadohealth.2007.07.012
Rush T, LeardMann CA, Crum-Cianflone NF (2016) Obesity and associated adverse health outcomes among US military members and veterans: findings from the Millennium cohort study. Obesity 24(7):1582–1589. https://doi.org/10.1002/oby.21513
Timboe A, Lystrup R, Ledford CJW, Crawford P (2019) Identifying a potential screening tool for prediabetes: the association of hemoglobin A1c and a test of physical fitness. Mil Med 184(3–4):e139–e142. https://doi.org/10.1093/milmed/usy207
Yang Y, Shields GS, Guo C, Liu Y (2018) Executive function performance in obesity and overweight individuals: a meta-analysis and review. Neurosci Biobehav Rev 84:225–244. https://doi.org/10.1016/j.neubiorev.2017.11.020
Smith E, Hay P, Campbell L, Trollor JN (2011) A review of the association between obesity and cognitive function across the lifespan: implications for novel approaches to prevention and treatment. Obes Rev 12(9):740–755. https://doi.org/10.1111/j.1467-789X.2011.00920.x
Dohle S, Diel K, Hofmann W (2018) Executive functions and the self-regulation of eating behavior: a review. Appetite 124:4–9. https://doi.org/10.1016/j.appet.2017.05.041
Diamond A (2013) Executive functions. Annu Rev Psychol 64(1):135–168. https://doi.org/10.1146/annurev-psych-113011-143750
Goldschmidt AB, Hipwell AE, Stepp SD, McTigue KM, Keenan K (2015) Weight gain, executive functioning, and eating behaviors among girls. Pediatr 136(4):e856–e863. https://doi.org/10.1542/peds.2015-0622
Dassen F, Houben K, Allom V, Jansen A (2018) Self-regulation and obesity: the role of executive function and delay discounting in the prediction of weight loss. J Behav Med 41(6):806–818. https://doi.org/10.1007/s10865-018-9940-9
Raman J, Hay P, Tchanturia K, Smith E (2018) A randomised controlled trial of manualized cognitive remediation therapy in adult obesity. Appetite 123:269–279. https://doi.org/10.1016/j.appet.2017.12.023
Hanson JA, Haub MD, Walker JJ, Johnston DT, Nelson Goff BS, Dretsch MN (2012) Attention deficit hyperactivity disorder subtypes and their relation to cognitive functioning, mood states, and combat stress symptomatology in deploying US soldiers. Mil Med 177(6):655–662. https://doi.org/10.7205/MILMED-D-11-00340
Georgiev GZ (2020) Sample size calculator. Available at: https://www.gigacalculator.com/calculators/power-sample-size-calculator.php Accessed 22 Jan 2020
Reeves DL, Bleiberg J, Roebuck-Spences T, Cernich AN, Schwab K, Salazar AM, Harvey SC, Brown FH, Warden D (2006) Reference values for performance on the automated neuropsychological assessment metrics V3.0 in an active duty military sample. Mil Med 171(10):982–994. https://doi.org/10.7205/MILMED.171.10.982
Elsmore TF, Reeves DL, Reeves AN (2007) The ARES® test system for palm OS handheld computers. Arch Clin Neuropsychol 22(S1):S135–144. https://doi.org/10.1016/j.acn.2006.10.009
Salthouse TA, Hedden T (2002) Interpreting reaction time measures in between-group comparisons. J Clin Exp Neuropsychol 24(7):858–872. https://doi.org/10.1076/jcen.24.7.858.8392
Centers for Disease Control and Prevention. About adult BMI, healthy weight. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Updated 2017. Accessed 7 March 2019.
Expert panel on the identification, evaluation, and treatment of overweight in adults (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Am J Clin Nutr 68(4):899–917. https://doi.org/10.1093/ajcn/68.4.899
Mikkola I, Jokelainen JJ, Timonen MJ et al (2009) Physical activity and body composition changes during military service. Med Sci Sports Exerc 41(9):1735–1742. https://doi.org/10.1249/MSS.0b013e31819fcd3c
Ekelund U, Neovius M, Linne Y, Brage S, Wareham NJ, Rossner S (2005) Associations between physical activity and fat mass in adolescents: the Stockholm weight development study. Am J Clin Nutr 81(2):355–360. https://doi.org/10.1093/ajcn.81.2.355
U.S. Department of Health and Human Services and U.S. Department of Agriculture (2015) 2015–2020 Dietary Guidelines for Americans. https://health.gov/dietaryguidelines/2015/guidelines/. Accessed 7 March 2019
Campos-Uscanga Y, Gutiérrez-Ospina G, Morales-Romero J, Romo-González T (2017) Self-regulation of eating and physical activity is lower in obese female college students as compared to their normal weight counterparts. Eat Weight Disord 22(2):311–319. https://doi.org/10.1007/s40519-016-0338-9
Garza KB, Ding M, Owensby JK, Zizza CA (2016) Impulsivity and fast-food consumption: a cross-sectional study among working adults. J Acad Nutr Diet 116(1):61–68. https://doi.org/10.1016/j.jand.2015.05.003
Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF (2005) Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry 57(11):1336–1346. https://doi.org/10.1016/j.biopsych.2005.02.006
Hanson JA, Phillips L, Hughes S, Corson K (2019) Attention-deficit hyperactivity disorder symptomatology, binge eating disorder symptomatology, and body mass index among college students. J Am Coll Health. https://doi.org/10.1080/07448481.2019.1583651
Wyckoff EP, Evans BC, Manasse SM, Butryn ML, Forman EM (2017) Executive functioning and dietary intake: neurocognitive correlates of fruit, vegetable, and saturated fat intake in adults with obesity. Appetite 111:79–85. https://doi.org/10.1016/j.appet.2016.12.039
Allom V, Mullan B (2014) Individual differences in executive function predict distinct eating behaviours. Appetite 80:123–130. https://doi.org/10.1016/j.appet.2014.05.007
Davis CL, Tomporowski PD, McDowell JE, Austin BP, Miller PH, Yanasak NE, Allison JD, Naglieri JA (2011) Exercise improves executive function and achievement and alters brain activation in overweight children: a randomized, controlled trial. Health Psychol 30(1):91–98. https://doi.org/10.1037/a0021766
Chang Y, Liu S, Yu H, Lee Y (2012) Effect of acute exercise on executive function in children with attention deficit hyperactivity disorder. Arch Clin Neuropsychol 27(2):225–237. https://doi.org/10.1093/arclin/acr094
Guiney H, Machado L (2012) Benefits of regular aerobic exercise for executive functioning in healthy populations. Psychonomic Bull Rev 20(1):73–86. https://doi.org/10.3758/s13423-012-0345-4
Kuczmarski MF, Kuczmarski RJ, Najjar M (2001) Effects of age on validity of self-reported height, weight, and body mass index: findings from the third national health and nutrition examination survey, 1988–1994. J Am Diet Assoc 101(1):28–34. https://doi.org/10.1016/S0002-8223(01)00008-6
Gasier HG, Hughes LM, Young CR, Richardson AM (2015) Comparison of body composition assessed by dual-energy X-ray absorptiometry and BMI in current and former US Navy service members. PLoS ONE. https://doi.org/10.1371/journal.pone.0132157
Heinrich KM, Jitnarin N, Suminski RR, Berkel L, Hunter CM, Alvarez L, Brundige AR, Peterson AL, Foreyt JP, Haddock K, Poston WSC (2008) Obesity classification in military personnel: a comparison of body fat, waist circumference, and body mass index measurements. Mil Med 173(1):67–73. https://doi.org/10.7205/MILMED.173.1.67
Milliken CS, Auchterlonie JL, Hoge CW (2007) Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA 298(18):2141–2148
Penney TL, Kirk SF (2015) The health at every size paradigm and obesity: missing empirical evidence may help push the reframing obesity debate forward. Am J Public Health 105(5):e38–e42. https://doi.org/10.2105/AJPH.2015.302552
Vartanian LR, Porter AM (2016) Weight stigma and eating behavior: a review of the literature. Appetite 102:3–14. https://doi.org/10.1016/j.appet.2016.01.034
Bruce LJ, Ricciardelli LA (2016) A systematic review of the psychosocial correlates of intuitive eating among adult women. Appetite 96:454–472. https://doi.org/10.1016/j.appet.2015.10.012
Provencher V, Bégin C, Tremblay A et al (2009) Health-at-every-size and eating behaviors: 1-year follow-up results of a size acceptance intervention. J Am Diet Assoc 109(11):1854–1861. https://doi.org/10.1016/j.jada.2009.08.017
Cole RE, Clark HL, Heileson J, DeMay J, Smith MA (2016) Normal weight status in military service members was associated with intuitive eating characteristic. Mil Med 181(6):589–595. https://doi.org/10.7205/MILMED-D-15-00250
Masheb RM, Kutz AM, Marsh AG, Min KM, Ruser CB, Dorflinger LM (2019) "Making weight" during military service is related to binge eating and eating pathology for veterans later in life. Eat Weight Disord 24(6):1063–1070. https://doi.org/10.1007/s40519-019-00766-w
Schaumberg K, Anderson DA, Anderson LM, Reilly EE, Gorrell S (2016) Dietary restraint: what's the harm? A review of the relationship between dietary restraint, weight trajectory and the development of eating pathology. Clin Obes 6(2):89–100. https://doi.org/10.1111/cob.12134
Malkawi AM, Meertens RM, Kremers SPJ, Sleddens EFC (2018) Dietary, physical activity, and weight management interventions among active-duty military personnel: a systematic review. Mil Med Res 5(1):43. https://doi.org/10.1186/s40779-018-0190-5
Allom V, Mullan B, Smith E, Hay P, Raman J (2018) Breaking bad habits by improving executive function in individuals with obesity. BMC Public Health 18(1):1–8. https://doi.org/10.1186/s12889-018-5392-y
Acknowledgements
We would like to thank the military leadership and the soldiers for their support and participation.
Funding
Funding for this project was provided by the Kansas State University Research Foundation and the Herbert D. and Nylda Gemple Award, Academy of Nutrition and Dietetics. Neither funding sources had any involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Disclaimer
Material has been reviewed by the Walter Reed Army Institute of Research. There is no objection to its presentation and/or publication. The opinions or assertions contained herein are the private views of the author, and are not to be construed as official, or as reflecting true views of the Department of the Army or the Department of Defense. The investigators have adhered to the policies for protection of human subjects as prescribed in AR 70-25.
Ethical approval
The work has been approved by and performed according to the ethical standards of the Committee on Research Involving Human Subjects, Institutional Review Board, at Kanas State University.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Exercise and Eating and Weight Disorders.
Rights and permissions
About this article
Cite this article
Hanson, J.A., Wagner, G. & Dretsch, M. Cognitive disinhibition and infrequent moderate-to-intense physical activity linked with obesity in U.S. soldiers. Eat Weight Disord 26, 973–981 (2021). https://doi.org/10.1007/s40519-020-00932-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-020-00932-5