Abstract
Background
The pediatric relative fat mass (RFM) has been recently presented and validated as an index for estimating percentage body fat (%BF) in North American children and adolescents. Similar to body mass index (BMI) and tri-ponderal mass index (TMI), RFM uses anthropometric measures (i.e., weight, height and waist circumference) to estimate body composition. The primary purpose of this study was to validate the newly developed RFM equation for %BF prediction in Southern Brazilian adolescents; as secondary objective, we compared %BF estimation from BMI- and TMI-derived equations.
Methods
A total of 631 individuals (434 boys) aged 11 to 18 were analyzed. Bland–Altman analyses were used to determine concordance between predicted equations and %BF measured by DXA; results are presented using mean difference (i.e., bias) and standard deviation. Sensitivity and specificity were calculated for %BF percentile classifications.
Results
RFM underestimated %BF in 65.2% of boys (− 4.3 ± 2.8%) and 84.8% of girls (− 5.3 ± 2.7%). In contrast, TMI overestimated %BF in 62.9% of boys (4.0 ± 2.9%) and 56.3% (3.5 ± 3.0%) of girls. The performance of BMI showed mixed results; %BF was overestimated in 68.4% of boys (5.0 ± 4.0%) and underestimated in 67.5% of girls (− 3.9 ± 2.6%), all p < 0.001. Although, RFM had the highest specificity for %BF percentile classifications, sensitivity was low and inferior to BMI and TMI.
Conclusion
TMI was superior to RFM and BMI in predicting %BF in Southern Brazilian adolescents. Using RFM, BMI or TMI equations for %BF prediction without a population-specific correction factor may lead to incorrect interpretations. We suggest that correction factors should be investigated to improve the accuracy of these surrogate indices for body composition assessment.
Level of evidence
Level V, cross sectional descriptive study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent obesity is considered a major public health threat as its prevalence continues to increase in many regions [1]. Overweight and obesity, or excess fat mass (FM), are often associated with adverse health outcomes among adolescents, including cardiometabolic and endocrinological disorders [2]. Thus, detecting excess FM by accurate and reliable techniques has the potential to inform more effective prevention and treatment strategies earlier in life, which may reduce the burden of obesity during adulthood.
Body mass index (BMI) is widely used as a surrogate measure of obesity. However, a well-known limitation of BMI is that it does not distinguish between FM and lean mass [3]. Indeed, BMI has been shown to be a poor predictor of percentage body fat (%BF) in children and adolescents [4]. To overcome these limitations and estimate %BF levels accurately, several equations based on anthropometric measures have been proposed. In 2017, Peterson et al. [5] presented the tri-ponderal mass index (TMI) using weight and height quadratic regression relations. More recently, the relative FM (RFM) equation based on height to waist circumference was validated in adults [6] and in a pediatric group of North Americans [7]. Compared to BMI and TMI, the linear model of the RFM was found to be more accurate to predict %BF in younger populations, suggesting its applicability in both clinical and epidemiological settings [7].
As such, given its simplicity and promising results, RFM may be used in adults as an alternative to estimate %BF when body composition techniques are not available [8]. Thus, the primary purpose of this study was to evaluate the validity of the newly RFM equation for %BF prediction in Southern Brazilian adolescents; as secondary objective, we compared %BF estimation from BMI and TMI derived equations.
Methods
Participants
This study included data from a cross-sectional survey assessing body composition in 11 to 18-year-old participants. The survey was conducted between 2014 and 2016 in Curitiba and surrounding cities in Brazil, with a sampling error of 4.5% for a confidence level of 91%. The sample consisted of adolescents who were not on calcium medication, did not undergo radiography/computed tomography in the 7 days prior to the evaluation and did not suspect pregnancy (self-reported) [9]. The study was conducted at Universidade Tecnológica Federal do Paraná, after parents signed a consent form. The study protocol was approved by the Plataforma Brasil system (protocol number: 11583113.7.0000.5547).
Anthropometric and body composition assessment
Standardized procedures to obtain anthropometric data were followed. Height was measured to the nearest 0.1 cm using a portable stadiometer with participants standing in bare feet. Body mass was assessed using a mechanical scale (Filizola, São Paulo, Brazil) with participants wearing light clothing. Waist circumference was measured at the smallest circumference of the abdomen with a flexible and inelastic tape. Body mass index was calculated as body weight (in kg) divided by squared height (in meters). To estimate %BF, anthropometric data were used in age-specific RFM equations and BMI- and TMI-derived equations, as proposed by Woolcott and Bergman [7] (Table 1).
Percentage body fat was measured using a DXA Hologic Discovery A fan-beam scan type (Hologic, Inc., Bedford, MA, USA), software version 13.3.0.1. The equipment was calibrated daily and all scans were performed by a single technician.
We used the classification proposed by Ogden et al. to identify participants with excess FM as those with %BF ≥ 85th percentile [10]. Additionally, the 25th, 50th, 75th, 85th and 95th percentiles established in the National Health Statistics Reports were employed as the reference data to evaluate the accuracy of each method to further classify adolescents into their correct %BF percentiles.
Data analysis
The study sample was characterized with position (median) and dispersion (interquartile range) measurements, as well as frequency distribution (%). Analyses were stratified by sex and age groups (11–14 and 15–18 years old), as the RFM equations proposed by Woolcott and Bergman are age specific [7]. Data distribution was verified by Kolmogorov–Smirnov test. To investigate the correlation between predicted %BF by TMI, BMI and RFM with DXA, we applied the nonparametric Spearman test. Bland–Altman graphical analyses were used to determined concordance between predicted equations and %BF measured by DXA. Differences between age groups were analyzed using Mann–Whitney U test. The Kappa coefficient was calculated to evaluate agreement between methods following the methodology proposed by Field [11]. In addition, sensitivity and specificity were calculated for %BF percentile classifications. To perform the analysis, we used the Statistical Package for the Social Sciences (SPSS), version 21.0 (SPSS Inc. Chicago, IL). The value of p < 0.05 was adopted as statistical significance.
Results
The study sample included 434 boys (68.7%) and 197 girls. Body weight, lean mass and height were higher in adolescents aged 15–18 years than in adolescents aged 11–14 years, independent of sex (all p = 0.001), (Table 2). In boys, %BF was lower in older participants compared to younger (p = 0.001). Although girls aged 15–18 years had higher FM (in kg) than 11–14 years girls (p = 0.001), no differences were observed in %BF (p = 0.152)”.
In boys, association analysis showed that measured %BF, evaluated by DXA, was moderately correlated with RFM in ages 11–14 years and 15–18 years (r = 0.745; r = 0.638, respectively). For TMI, correlation coefficients were 0.661 (11–14 years) and 0.627 (15–18 years). The values for BMI were: 11–14 years, r = 0.529 and 15–18 years, r = 0.651. In girls, RFM was moderately associated with %BF (11–14 years: r = 0.734; 15–18 years: r = 0.754) as well as TMI (11–14 years: r = 0.700; 15–18 years: r = 0.737) and BMI (11–14 years: 0.714; 15–18 years: r = 0.767). All correlations were significant, with a p value < 0.001.
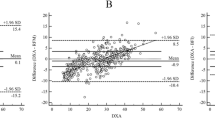
The agreement between estimated %BF by anthropometric equations (i.e., RFM, BMI, and TMI) and DXA (reference standard) was assessed using Bland–Altman plots (Figs. 1,2,3). RFM underestimated %BF in 65.2% of boys (mean difference ± SD = − 4.3 ± 2.8%) and 84.8% of girls (− 5.3 ± 2.7%). In contrast, TMI overestimated %BF in 62.9% (4.0 ± 2.9%) and 56.3% (3.5 ± 3.0%) in boys and girls. For BMI, %BF was overestimated in 68.4% of boys (5.0 ± 4.0%) and underestimated in 67.5% of girls (− 3.9 ± 2.6%).
The average values of %BF for RFM, TMI and BMI are presented in Fig. 4a, according to sex and age groups. Additionally, results from paired analyses revealed that bias between index tests and DXA were different for RFM and BMI (independent of sex) and TMI only in boys (p = 0.005; TMI in girls: p = 0.075) (Fig. 4b). Bias across age groups are reported in Fig. 4b, demonstrating that TMI showed better agreement in both sexes.
Furthermore, RFM correctly categorized 54.1% of boys and 51.8% of girls into their respective %BF percentiles as assessed by DXA. For TMI, the percentage of correct classification was 55.1% for boys and 65.0% for girls. For BMI, the result was 53.7% for boys and 68.0% for girls, Supplementary Table 1.
RFM showed high specificity but low sensitivity to diagnose excess %BF in both boys and girls, Supplementary Table 2. Although specificity was slightly lower for BMI and for TMI compared to RFM, the sensitivity to identify excess %BF was higher in both methods. A concordance analysis was also performed using Kappa coefficients. The Kappa analysis showed moderate agreement with TMI (boys: 0.608 and girls: 0.507); the agreement between the %BF obtained with BMI was considered fair (boys = 0.448 and for girls = 0.507). For RFM, the agreement was moderate for boys (0.372) and fair for girls (0.117).
Discussion
We evaluated the performance of RFM, BMI and TMI to estimate %BF in Southern Brazilian adolescents. This study is the first to investigate the validity of these indices in a South America population. Compared to Woolcott and Bergman’s findings, who initially proposed the RFM-, BMI- and TMI-derived equations, the linear relationship between RFM and %BF by DXA for boys and girls was relatively weaker in our study [7]. Bland–Altman analysis revealed that RFM underestimated %BF, with exception for 14-year-old boys. In contrast, TMI overestimated %BF in boys and bias was close to zero in girls. The performance of BMI showed mixed results, overestimating %BF among boys and underestimating in girls.
The poor agreement between %BF estimated (by RFM) versus measured (by DXA) may be a result of anthropometric differences in the sample population from Woolcott and Bergman compared to our adolescents, as waist and height were components of the RFM equation. Although %BF in girls was similar across studies, adolescents in our study had relatively smaller waist circumferences. For example, the mean difference for waist circumference between studies was greater than 10 cm in the 15–19-year group [7]. Similarly, boys had smaller waist circumferences and whole-body %BF. Another important difference is in height; our sample of younger adolescents was taller (~ 10 cm for girls and ~ 20 cm for boys) than in Woolcott and Bergman. However, older adolescent boys were shorter and girls had a similar height. Future studies creating correction factors for RFM linear equations are needed to improve the accuracy of this surrogate measure for %BF estimation in Brazilian adolescents. Given its simplicity, the RFM equation may be a promising tool for assessing body composition in clinical and research settings.
TMI was developed as an alternative and more superior method to BMI for predicting %BF [5]. Research has suggested that TMI is also useful in screening for risk of abdominal fat accumulation in children (2–5 years) [12]. Our findings indicated that the TMI equation for %BF prediction is more accurate than RFM among Brazilian boys and girls. Similarly, Woolcoot and Bergman reported that TMI was more accurate than RFM in European-American girls (15–19 years of age) and equally high accurate among Mexican–American girls [7]. The better performance of TMI may be explained by the removal of waist circumference measurement from the equation, a variable with greater difference between studied populations. Finally, a recent cross-sectional study with 296 participants suggested the use of TMI as an index to discriminate metabolic disorders in Brazilian children and adolescents [13].
Body mass index showed improved sensitivity (46.7%) compared to RFM (6.7%) among girls and boys (BMI = 41.2% / RFM = 23.5%) to distinguish adolescents with high FM. In Brazil, national-wide reference values for %BF using reliable and validated tools, such as DXA, are not available. Thus, employing the %BF classification proposed by National Health Statistics Reports [14], which was based on a foreign population, may partly explain the differences in the ability of the methods to correctly diagnose the high FM phenotype. Despite this, it is noteworthy that both males and females in our study had lower waist circumference, weight, height and lean mass in early ages (11–14 years). These anthropometric findings are similar to the literature, confirming age-dependent variation in anthropometric measurements during adolescence [7, 14]. Furthermore, the greater lean mass values observed in our sample of older adolescents are also in agreement with the literature, and it could be explained by hormone influences during sexual maturation [15, 16].
Some limitations should be considered in this study. First, DXA was used as a reference method which could have underestimated %BF compared to a multi-compartment method in children with overweight/obesity specifically [17]. However, the %BF classification proposed by Ogden et al. was computed using DXA, and this body composition technique has several advantages over other techniques (e.g., minimal radiation exposure, rapid body scan, and high precision) [18]. Second, the sample size was modest given that Brazil is a continental size country. On the other hand, the same methodology can be used in different regions to verify if our findings could be applicable. Last, the lack of sexual maturation data limited interpretation on the accuracy of index tests across adolescents’ developmental stages.
In summary, TMI was superior to RFM and BMI in predicting %BF in Southern Brazilian adolescents. Nevertheless, using RFM, BMI or TMI equations for %BF prediction without a correction factor that is specific to the population being assessed may lead to incorrect interpretations. Correction factors should therefore be investigated to improve the accuracy of these surrogate indices as they provide additional information of body composition compared to BMI. Finally, direct estimation of fat percentage from simple anthropometric values may represent an advance in clinical practice or epidemiological studies of body composition in locates where no technology is available.
What is already known on this subject?
When access to body composition assessment is unavailable, predictive equations using anthropometric measures may serve as surrogates for fat mass. For example, the relative fat mass (RFM) has been shown useful to estimate whole-body fat percentage and diagnose body fat-defined overweight or obesity.
What does this study add?
This work is the first study that evaluates the validity and accuracy of a newly developed equation, RFM. The study is contributing to the field by cross validating these newly developed equations in a Brazilian cohort of adolescents and emphasizing that caution is needed when choosing equations to be used in clinical and research settings.
Data availability
All relevant data are within the manuscript and its Supporting Information files.
References
Bentham J, Di Cesare M, Bilano V, Bixby H, Zhou B, Stevens GA et al (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390:2627–2642. https://doi.org/10.1016/S0140-6736(17)32129-3
Sharma V, Coleman S, Nixon J, Sharples L, Hamilton-Shield J, Rutter H et al (2019) A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes Rev 20:1341–1349. https://doi.org/10.1111/obr.12904
Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS (2005) The relation of childhood BMI to adult adiposity: the Bogalusa heart study. Pediatrics 115:22–27. https://doi.org/10.1542/peds.2004-0220
Vanderwall C, Randall Clark R, Eickhoff J, Carrel AL (2017) BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatr 17:4–9. https://doi.org/10.1186/s12887-017-0891-z
Peterson CM, Su H, Thomas DM, Heo M, Golnabi AH, Pietrobelli A et al (2017) Tri-ponderal mass index vs body mass index in estimating body fat during adolescence. JAMA Pediatr 171:629–636. https://doi.org/10.1001/jamapediatrics.2017.0460
Woolcott OO, Bergman RN (2018) Relative fat mass (RFM) as a new estimator of whole-body fat percentage—a cross-sectional study in American adult individuals. Sci Rep 8:1–11. https://doi.org/10.1038/s41598-018-29362-1
Woolcott OO, Bergman RN (2019) Relative fat mass as an estimator of whole-body fat percentage among children and adolescents: a cross-sectional study using NHANES. Sci Rep. https://doi.org/10.1038/s41598-019-51701-z
Paek JK, Kim J, Kim K, Yeong LS (2019) Usefulness of relative fat mass in estimating body adiposity in Korean adult population. Endocr J 66:723–729. https://doi.org/10.1507/endocrj.ej19-0064
Ulbricht L, De Campos MF, Esmanhoto E, Ripka WL (2018) Prevalence of excessive body fat among adolescents of a south Brazilian metropolitan region and State capital, associated risk factors, and consequences. BMC Public Health 18:1–11. https://doi.org/10.1186/s12889-018-5216-0
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM (2016) Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 315:2292–2299. https://doi.org/10.1016/j.physbeh.2017.03.040
Field A (2009) Descobrindo a estatística utilizando o SPSS, 1st edn. Artmed, Porto Alegre
Nascimento VG, Bertoli CJ, Gallo PR, de Abreu LC, Leone C (2019) Tri-ponderal mass index: a screening tool for risk of central fat accumulation in brazilian preschool children. Medicina (B Aires) 55:577. https://doi.org/10.3390/medicina55090577
Neves FS, de Oliveira Alvim R, Zaniqueli D, Pani VO, Martins CR, de Souza Peçanha MA et al (2020) Tri-ponderal mass index is useful for screening children and adolescents with insulin resistance. Rev Paul Pediatr 38:e2019066. https://doi.org/10.1590/1984-0462/2020/38/2019066
Ogden CL, Li Y, Freedman DS, Borrud LG, Fleegan KM (2011) Smoothed percentage body fat percentiles for U.S. children and adolescents, 1999–2004. Natl Health Stat Report 43:1–7
Liu J, Yan Y, Xi B, Huang G, Mi J (2019) Skeletal muscle reference for Chinese children and adolescents. J Cachexia Sarcopenia Muscle 10:155–164. https://doi.org/10.1002/jcsm.12361
Jeddi M, Dabbaghmanesh MH, Ranjbar Omrani G, Ayatollahi SMT, Bagheri Z, Bakhshayeshkaram M (2015) Relative importance of lean and fat mass on bone mineral density in iranian children and adolescents. Int J Endocrinol Metab. https://doi.org/10.5812/ijem.25542v2
Silva D, Ribeiro A, Pavão F (2013) Validity of the methods to assess body fat in children and adolescents using multi-compartment models as the reference method: a systematic review. Rev Assoc Med Bras 59:475–486. https://doi.org/10.1016/j.ramb.2013.03.006
Prado CMM, Heymsfield SB (2014) Lean tissue imaging: a new era for nutritional assessment and intervention. J Parenter Enter Nutr 38:940–953. https://doi.org/10.1177/0148607114550189
Funding
WLR and LU received funding from Programa de Pesquisa para o Sistema Único de Saúde: Gestão Compartilhada em Saúde PPSUS—edition 04/2012, Project number: 41614—FA, agreement 982/2013 with Universidade Tecnológica Federal do Paraná. CEO is supported by the Alberta Diabetes Institute and a recipient of the 2018 Alberta SPOR Graduate Studentship in Patient-Oriented Research, which is jointly funded by Alberta Innovates and the Canadian Institutes of Health Research. NL is researcher of Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). The funding body had no role in the design, collection, analysis, and interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
WLR contributed in designing, writing, and statistical analysis of this study. CO was responsible for data interpretation and writing. LU contributed with statistical analysis and conducting the study. AMQ, CMP, NL are responsible to data interpretation and manuscript revision. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
The study protocol has been approved by the ethics committee of the Universidade Tecnológica Federal do Paraná (Plataforma Brasil system, nº11583113.7.0000.5547).
Informed consent
All of the participants signed and approved a written informed consent before participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ripka, W.L., Orsso, C.E., Haqq, A.M. et al. Validity and accuracy of body fat prediction equations using anthropometrics measurements in adolescents. Eat Weight Disord 26, 879–886 (2021). https://doi.org/10.1007/s40519-020-00918-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-020-00918-3