Abstract
Purpose
Bulimia nervosa (BN) is associated with increased risk of cardiovascular disease and arrhythmias. Some reports found abnormal electrocardiographic markers of arrhythmias in BN, while others did not. This study investigated novel parameters of T-wave morphology that were reported to be associated with adverse cardiovascular outcomes in other patient groups, among patients with BN under medical care.
Method
Thirty-five BN patients and 76 healthy controls were included. Total cosine R to T (TCRT) and T-wave Morphology Dispersion (TMD) parameters were computed according to accepted standards for an average beat and a random beat. Patients were followed for 11.1 ± 0.1 years for the emergence of arrhythmias or events of sudden death.
Results
Twenty-five (71.4%) BN patients were hospitalized when enrolled, for a mean duration of 1.1 ± 0.2 months. The rest were ambulatory patients. The BN group had lower blood pressure, more smokers, and used antidepressants, neuroleptic drugs and benzodiazepines more than controls did. Other demographic parameters were comparable between groups. TCRT and TMD parameters were statistically similar and within the normal ranges reported by other research groups. None of the BN patients had prolonged QTc interval or electrolyte abnormalities on inclusion. During the follow-up period, no clinical symptoms suggestive of arrhythmias were reported, and no cardiovascular-related hospitalizations or deaths occurred in either group.
Conclusion
Medically treated BN patients have normal T-wave morphology parameters and hence, low risk for repolarization-associated malignant ventricular arrhythmias. The prognostic importance of these novel repolarization parameters remains to be explored among untreated patients, those who ingest emetic substances and patients with electrolyte imbalance.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bulimia nervosa (BN) is a common eating disorder that mainly affects young women. It has a peak incidence at ages 21–24 years [1] and a lifetime prevalence of 1.5% [2]. BN is characterized by recurrent episodes of binge eating and recurrent, inappropriate compensatory behavior that occurs at least once a week for 3 months, to prevent weight gain. Mortality rate among BN patients is 49% higher than in the general population [3]. Moreover, standardized mortality ratio for specific age groups (e.g., 15–24 years) can be as high as 4.1-fold [4]. Cardiovascular disease has been reported to account for 12% of deaths in patients with BN [5]. Vomiting, use of laxatives, excessive exercise, or restricted oral intake, are all behaviors that have the potential to affect the cardiovascular system [2]. The overall incidence rate of cardiovascular disease in BN was found to be 10.34/1000 person-years, as compared with 1.02 in women with pregnancy-related hospitalizations. In patients with three or more admissions for bulimia, the incidence of cardiovascular disease was as high as 25.13/1000 person-years (95% CI 13.52–46.70) [2].
Serious arrhythmias occur relatively frequently in patients with BN, especially if electrolyte imbalance has developed. In addition, ingestion of ipecac to induce emesis may be associated with tachycardia or bradycardia, abnormal repolarization, interventricular conduction delays and ventricular arrhythmias [6]. Some studies reported increased QTc values in patients with BN, as compared with controls [7, 8], while others reported comparable [1] or lower QTc values [9]. QT dispersion (QTd), a marker of repolarization heterogeneity and a possible predictor of ventricular arrhythmias, was reported to be increased in BN patients [10,11,12]; although, study groups were generally small and, therefore, preclude definitive conclusions as to the association between QTd and BN, and its usefulness in predicting ventricular arrhythmias in these patients. Interestingly, Takimoto et al., reported that BN patients with higher depression and anxiety scores had higher QTd values [11]. In addition, medical treatment received during hospitalization was associated with a decrease in QTd values [12], suggesting a possible treatment-associated decrease in arrhythmia risk. BN was reported to be associated with the development of late ventricular potentials, a signal-averaged electrocardiographic marker for reentrant ventricular arrhythmias [13]; although, this association was disputed by another report [14].
Total cosine R to T (TCRT) is a novel electrocardiographic marker that reflects the spatial angle between ventricular depolarization and repolarization [15]. Negative TCRT values were found to be associated with increased risk of cardiac events and adverse prognosis [16, 17]. T-wave morphology dispersion (TMD), a marker of variation in T‐waves between individual leads, was also found to be predictive of cardiac death in various patient populations [18].
Due to the limited and occasionally conflicting information on repolarization abnormalities in patients with BN, the aim of the current study was to evaluate TCRT and TMD, previously unstudied repolarization markers for arrhythmias, in a cohort of patients with medically treated BN, without electrolyte abnormalities.
Materials and methods
BN was diagnosed by a psychiatrist, according to DSM-IV-TR criteria. Criteria were revisited following the publication of DSM-V and only those patients who fit the diagnosis of BN according to both systems and did not receive an alternative diagnosis, were included. The study group included 35 patients diagnosed with BN and 76 healthy controls. All BN patients were recruited from the in-patient Department of Eating Disorders and the Eating Disorders Outpatient Clinic at the Sheba Medical Center, Tel Hashomer, Israel from May 2008 to March 2010. None of the BN patients had a history of ischemic heart disease or myocardial infarction. During hospitalization and during the ambulatory follow-up, all patients underwent repeated blood tests. Any electrolyte abnormalities were corrected prior to inclusion in the study.
An age- and sex-matched control group was recruited from the hospital staff and their family members. Only patients who had no history of cardiovascular or systemic disorders were included. Mild dyslipidemia for which dietary modification was initiated and pharmacologically balanced hypothyroidism were not considered exclusion criteria.
Electrocardiograph procedure
Participants were asked not to smoke, drink caffeinated beverages, or take other stimulants starting 3 h before the ECG study and to avoid strenuous exercise for 24 h prior to it. In all cases, the test was conducted between 9:00 a.m. and 12:00 p.m. Room temperature was maintained at 23–24 °C. Before starting the test, participants were asked to lie motionless for 10 min. Resting ECG measurements were taken with a designated, high-resolution commercial ECG (1200HR PC-ECG, Norav Medical, Israel). The subject’s skin was cleansed with alcohol prior to electrode placement to decrease the noise level. Leads were positioned according to the standard 12-lead system. The patients were weighed and height measured to compute body mass index (BMI). Blood pressure was measured twice with an automated commercial sphygmomanometer (Welch Allyn 4200B-E1) and values were averaged.
Repolarization analysis
QT was calculated and corrected QT (QTc) were computed using commercial software (Rest ECG ver. 5.515, Norav Medical, Israel), according to the Bazett formula. According to acceptable standards, prolonged QTc was defined as values higher than 430 ms in males and 450 ms in females [19]. To compute T-wave morphology parameters, the time series was exported to a binary file format. The 3-dimensional vector representation of the electrical signal was accomplished by applying singular value decomposition to the eight independent surface ECG leads to produce a system of three independent orthogonal leads that contained 99% of the ECG energy [20]. TCRT and TMD were computed according to accepted standards [15]. TCRT is computed by calculating the cosine values between the 3-dimensional QRS and T-wave loop vectors within the optimized decomposition space. The variable does not have units and negative values correspond to large differences in the rotational orientation of the two loops. TMD is a measure of differences between T-wave shapes in individual leads, calculated as the average of angles between all possible pairs of reconstructed vectors of individual ECG leads created from the T-wave loop, with a small value indicating similar T-wave morphology between leads [21]. TMDpre (which describes the morphological changes from the start of the T-wave to the T-wave peak) and TMDpost (changes from peak T-wave to T-wave end) were also calculated [15]. All of the above parameters were derived from a single beat and from an averaged beat.
The repolarization analysis algorithm was written in Python 3.6 using NumPy and external python library BIOSPPy [22]. R-detection algorithm was used to separate individual beats. Measurements that contained displaced leads or high electrical interfaces despite filtering were excluded from the analysis. The Python library Matplotlib was used to visualize the tracings to ensure the technical quality of the ECG data.
Follow-up
BN patients had been periodically followed-up in the ambulatory eating disorder clinic and data were saved digitally. Data on symptoms (e.g., complaints of palpitation, syncope events, etc.), cardiovascular complications and mortality were retrospectively abstracted from the digital health records at the end of the follow-up period.
Statistical analyses
Data were analyzed with Microsoft Excel (Microsoft Corp., Seattle, WA) and JMP version 7.0 (SAS Institute, Cary, NC, USA). Results are presented as mean and standard error of mean (SEM). Between-group comparisons were carried out using Fisher’s exact test for categorical data and the non-parametric Wilcoxon Rank Sum test for numerical data. A p value of less than 0.05 was considered statistically significant.
Results
The clinical characteristics of the BN patients and control group are outlined in Table 1. Twenty-five BN patients were hospitalized (71.4%) when recruited to the study. Mean hospitalization duration at enrollment was 1.1 ± 0.2 months (range: 0–5 months). On the date of hospitalization, one patient was found to have mildly low potassium levels (3.2 mmol/L). Another patient was found to have low magnesium on admission (1.67 mmol/L) and two patients were found to have increased magnesium levels (3.9 and 4.4 mmol/L). All electrolyte disturbances were corrected shortly after hospitalization and prior to study inclusion. The mean age at diagnosis of BN was 18.4 ± 0.8 years (age at study enrollment was 24.3 ± 0.7 years). The groups were comparable in age, male to female ratio and height. None of the BN or control patients had a history of heart disease, diabetes mellitus, or hypertension. Mild dyslipidemia for which life-style modifications were initiated was found in 2.9% of BN patients and 6.6% of control patients (p> 0.05). None of the patients was treated with statins. BN patients had significantly lower systolic blood pressure (101.5 ± 2.0 vs. 111.2 ± 1.1 mmHg, p < 0.001) and diastolic blood pressure (63.3 ± 1.7 vs. 72.4 ± 0.9 mmHg, p < 0.001) compared with controls. In addition, the rate of smokers was significantly higher among BN than in control patients (60.0% vs. 19.7%, p < 0.001). BN patients were more likely to be taking antidepressants (57.1% vs. 0%, p < 0.001), neuroleptic drugs (14.2% vs. 0%, p < 0.001), and benzodiazepines (11.4% vs. 0%, p = 0.003), as compared with controls. Four patients were treated with risperidone and one patient was treated with a combination of clotiapine and quetiapine. Patients were treated with escitalopram (six patients), citalopram (four patients), sertraline (four patients), fluoxetine (two patients), fludoxetine (two patients), venlafaxine (two patients), trazodone (two patients), mirtazapine (one patient), and clomipramine (one patient). Four patients were taking a combination of two antidepressants. Four other patients (14.3% of BN patients) were prescribed clonazepam, and five patients were prescribed anti-epileptic therapy (two patients were treated with topiramate, two with carbamazepine, and one patient with lamotrigine).
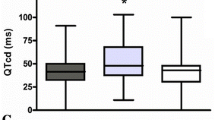
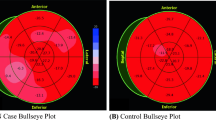
The T-wave morphology parameters are outlined in Table 2. Both groups had similar TCRT, TMD, TMD -pre and -post values, as compared with healthy controls (p > 0.05 for all comparisons), for a randomly selected beat and for an averaged beat. Average QT for the BN patients was 385.5 ± 1.7 ms, and QTc was 400.0 ± 3.8 ms. The QTc values of all BN patients were within the normal range. BN patients were followed for 11.1 ± 0.1 years for the emergence of cardiac symptoms, arrhythmias or events of sudden death. During the follow-up period, none of the BN (or control) patients developed cardiovascular complications or died. Also, none of the BN patients reported an event of syncope or palpitations. Four (11.4%) BN patients were hospitalized 3 times in the Eating Disorders Department during the follow-up period, and 7 (20%) had overall two hospitalizations. The others were hospitalized once or were only followed as outpatients.
Discussion
Cardiovascular disease commonly occurs in patients with BN [2, 5]. Yet, the controversy regarding the association of BN with markers of repolarization abnormalities and electrocardiographic markers for arrhythmias is ongoing. Specifically, the relation between BN and abnormal QTc duration [1, 7,8,9], as well as between BN and late ventricular potentials [13, 14] remains largely unknown.
TCRT and other T-wave morphology parameters have not been evaluated previously in BN despite their high reported efficacy in identifying patients who are likely to develop cardiac arrhythmias [16, 23,24,25]. Therefore, the current study endeavored to broaden the understanding of repolarization in medically treated BN patients. TCRT, in particular, was reported to be a powerful tool for predicting adverse outcomes in patients with cardiovascular risk factors or known cardiac disorders, even more so than that of clinical and traditional ECG parameters [17]. In addition, TMD parameters were reported to effectively distinguish patients with structural cardiac disorders from those with normal hearts [15].
In the current study, we found that T-wave morphology parameters in medically-treated BN patients without electrolyte imbalance, and with relatively short-term diagnosis, were comparable to those of healthy controls. Moreover, TCRT results of both groups were comparable to those reported for healthy individuals [15, 26,27,28]. Although the normal range of TMD is less well defined in the medical literature, the results of both BN and control patients were similar to those reported by Ono et al. among healthy controls [29]. Various types of pharmacotherapies were prescribed to the BN patients in the study. Although it is well-acknowledged that neuroleptic drugs [30] and antidepressants [31] might cause QTc prolongation, this effect on traditional markers of repolarization was not found in any of our patients. Also, no adverse effects were found regarding T-wave morphology parameters. A review of the medical literature for all the medications prescribed to the BN study patients did not yield any reported associations that specifically affected TCRT. It is unknown whether an adverse association occurs after prolonged treatment. Also, the possible adverse effects in patients who are overdosed, a condition that did not occur in our patients at the time of inclusion or during the follow-up, remains to be determined.
The current study was mainly characterized by the inclusion of a large group of hospitalized patients. Also, it included patients with no electrolyte disturbances who were also periodically invited for an outpatient medical checkup and other periodic multidisciplinary supportive care following hospitalization. We cannot predict what the results would have been in the study had been conducted prior to or shortly after hospitalization, and whether patients with electrolyte abnormalities or those who recently ingested emetic substances were to be included. Also, during the follow-up period, only four patients were hospitalized on three occasions. It remains unknown whether the inclusion of patients with more severe BN, manifested by a higher rate of hospitalizations (and subsequently higher degree of cardiovascular involvement as reported [2]) would have resulted in abnormal T-wave morphology results.
As the study group included mostly young BN patients with short disease duration, it is unknown whether other patient characteristics, such as disease longevity or specific BN-related behaviors, are associated with adverse influences on repolarization parameters. Therefore, the association between T-wave morphology parameters in long-standing BN patients should be further evaluated in future studies.
In conclusion, this was the first study to evaluate T-wave morphology parameters among patients with BN. It was found that medically-treated BN patients have normal TCRT and TMD parameters, which reflects an overall low risk of repolarization-associated ventricular arrhythmias. Long-term follow-up studies should be conducted to evaluate the prognostic significance of these novel repolarization markers among patients with eating disorders, and especially those with untreated or long-lasting BN.
What is already known on this subject?
Heart disease and arrhythmias account for 12% of BN deaths. It is unknown whether BN patients have electrocardiographic signs of abnormal repolarization and altered T-wave morphology parameters; important markers for arrhythmia.
What this study adds?
Medically-treated BN patients have similar TCRT and TMD as healthy people do. This reflects a low risk for cardiovascular complications. The role of these variables in untreated BN or patients with frequent hospitalizations and electrolyte imbalance requires exploration.
References
Frederiksen TC, Christiansen MK, Ostergaard PC, Thomsen PH, Graff C, Clausen L, Jensen HK (2018) The QTc interval and risk of cardiac events in bulimia nervosa: a long-term follow-up study. Int J Eat Disord 51:1331–1338. https://doi.org/10.1002/eat.22984
Tith RM, Paradis G, Potter BJ, Low N, Healy-Profitós J, He S, Auger N (2019) Association of bulimia nervosa with long-term risk of cardiovascular disease and mortality among women. JAMA Psychiatry. https://doi.org/10.1001/jamapsychiatry.2019.2914
Fichter MM, Quadflieg N (2016) Mortality in eating disorders results of a large prospective clinical longitudinal study. Int J Eat Disord 49:391–401. https://doi.org/10.1002/eat.22501
Hoang U, Goldacre M, James A (2014) Mortality following hospital discharge with a diagnosis of eating disorder: national record linkage study, England, 2001–2009. Int J Eat Disord 47:507–515. https://doi.org/10.1002/eat.22249
Suokas JT, Suvisaari JM, Gissler M, Lofman R, Linna MS, Raevuori A, Haukka J (2013) Mortality in eating disorders: a follow-up study of adult eating disorder patients treated in tertiary care, 1995–2010. Psyc Res 210:1101–1106. https://doi.org/10.1016/j.psychres.2013.07.042
Brown CA, Mehler PS (2013) Medical complications of self-induced vomiting. Eat Disord 21:287–294. https://doi.org/10.1080/10640266.2013.797317
Panagiotopoulos C, McCrindle BW, Hick K, Katzman DK (2000) Electrocardiographic findings in adolescents with eating disorders. Pediatrics 105:1100–1105. https://doi.org/10.1542/peds.105.5.1100
Buchanan R, Ngwira J, Amsha K (2011) Prolonged QT interval in bulimia nervosa. BMJ Case Rep. https://doi.org/10.1136/bcr.01.2011.3780
Vaurs C, Rollin A, Bérard E, Valet M, Saulnier A, Hazane F, Ritz P, Maury P (2014) QT interval is not prolonged in patients with eating disorders. Int J Cardiol 177:134–135. https://doi.org/10.1016/j.ijcard.2014.09.055
Takimoto Y, Yoshiuchi K, Kumano H, Yamanaka G, Sasaki T, Suematsu H, Nagakawa Y, Kuboki T (2004) QT interval and QT dispersion in eating disorders. Psychother Psychosom 73:324–328. https://doi.org/10.1159/000078850
Takimoto Y, Yoshiuchi K, Akabayashi A (2008) Effect of mood states on QT interval and QT dispersion in eating disorder patients. Psyc Clin Neuros 62:185–189. https://doi.org/10.1111/j.1440-1819.2008.01753.x
Nahshoni E, Yaroslavsky A, Varticovschi P, Weizman A, Stein D (2010) Alterations in QT dispersion in the surface electrocardiogram of female adolescent inpatients diagnosed with bulimia nervosa. Compr Psychiatry 51:406–411. https://doi.org/10.1016/j.comppsych.2009.10.005
Takimoto Y, Yoshiuchi K, Kumano H, Kuboki T (2006) Bulimia nervosa and abnormal cardiac repolarization. J Psychosom Res 60:105–107. https://doi.org/10.1016/j.jpsychores.2005.06.063
Nussinovitch M, Gur E, Kaminer K, Volovitz B, Nussinovitch N, Nussinovitch U (2012) Normal late ventricular potentials in hospitalized patients with eating disorders. Int J Eat Disord 45:900–904. https://doi.org/10.1002/eat.20949
Acar B, Yi G, Hnatkova K, Malik M (1999) Spatial, temporal and wavefront direction characteristics of 12-lead T-wave morphology. Med Biol Eng Comput 37:574–584. https://doi.org/10.1007/bf02513351
Batchvarov V, Hnatkova K, Ghuran A, Poloniecki J, Camm AJ, Malik M (2003) Ventricular gradient as a risk factor in survivors of acute myocardial infarction. Pace 26:373–376. https://doi.org/10.1046/j.1460-9592.2003.00052.x
Tse G, Gong M, Wong CW, Chan C, Georgopoulos S, Chan YS, Yan BP, Li G, Whittaker P, Ciobanu A, Ali-Hasan-Al-Saegh S, Wong SH, Wu WKK, Bazoukis G, Lampropoulos K, Wong WT, Tse LA, Baranchuk AM, Letsas KP, Liu T (2018) International health informatics study N total cosine R-to-T for predicting ventricular arrhythmic and mortality outcomes: a systematic review and meta-analysis. Ann Noninvasive Electrocardiol 23:e12495. https://doi.org/10.1111/anec.12495
Pirkola JM, Konttinen M, Kentta TV, Holmstrom LTA, Junttila MJ, Ukkola OH, Huikuri HV, Perkiomaki JS (2018) Prognostic value of T-wave morphology parameters in coronary artery disease in current treatment era. Ann Noninvas Electro 23:e12539. https://doi.org/10.1111/anec.12539
Goldenberg I, Moss AJ, Zareba W (2006) QT interval: how to measure it and what is “normal”. J Cardiovasc Electrophysiol 17:333–336. https://doi.org/10.1111/j.1540-8167.2006.00408.x
Poulikakos D, Hnatkova K, Banerjee D, Malik M (2018) Association of QRS-T angle and heart rate variability with major cardiac events and mortality in hemodialysis patients. Ann Noninvasive Electrocardiol 23:e12570. https://doi.org/10.1111/anec.12570
Nayyar S, Hasan MA, Roberts-Thomson KC, Sullivan T, Baumert M (2017) Effect of loss of heart rate variability on T-wave heterogeneity and QT variability in heart failure patients: implications in ventricular arrhythmogenesis. Cardiovasc Eng Technol 8:219–228. https://doi.org/10.1007/s13239-017-0299-9
Kentta T, Karsikas M, Junttila MJ, Perkiomaki JS, Seppanen T, Kiviniemi A, Nieminen T, Lehtimaki T, Nikus K, Lehtinen R, Viik J, Kahonen M, Huikuri HV (2011) QRS-T morphology measured from exercise electrocardiogram as a predictor of cardiac mortality. Europace 13:701–707. https://doi.org/10.1093/europace/euq461
Huang HC, Lin LY, Yu H, Ho YL (2009) Risk stratification by T-wave morphology for cardiovascular mortality in patients with systolic heart failure. Europace 11:1522–1528. https://doi.org/10.1093/europace/eup294
Porthan K, Viitasalo M, Toivonen L, Havulinna AS, Jula A, Tikkanen JT, Vaananen H, Nieminen MS, Huikuri HV, Newton-Cheh C, Salomaa V, Oikarinen L (2013) Predictive value of electrocardiographic T-wave morphology parameters and T-wave peak to T-wave end interval for sudden cardiac death in the general population. Circ-Arrhythmia Elec 6:690–696. https://doi.org/10.1161/Circep.113.000356
Batchvarov V, Kaski JC, Parchure N, Dilaveris P, Brown S, Ghuran A, Farbom P, Hnatkova K, Camm AJ, Malik M (2002) Comparison between ventricular gradient and a new descriptor of the wavefront direction of ventricular activation and recovery. Clin Cardiol 25:230–236. https://doi.org/10.1002/clc.4950250507
Friedman HS (2007) Determinants of the total cosine of the spatial angle between the QRS complex and the T wave (TCRT): implications for distinguishing primary from secondary T-wave abnormalities. J Electrocardiol 40:12–17. https://doi.org/10.1016/j.jelectrocard.2006.05.008
Hyytinen-Oinas MK, Ylitalo K, Karsikas M, Seppanen T, Raatikainen MJP, Uusimaa P, Huikuri HV, Perkiomaki JS (2010) Electrocardiographic abnormalities and ventricular tachyarrhythmias after myocardial infarction. Scand Cardiovasc J 44:15–23. https://doi.org/10.3109/14017430902998658
Ono T, Saitoh H, Yi G, Hnatkova K, Kobayashi Y, Atarashi H, Katoh T, Takano T, Malik M (2005) Clinical implication of T-wave morphology analysis as a new repolarization descriptor. Circ J 69:666–670. https://doi.org/10.1253/circj.69.666
Nielsen J, Graff C, Kanters JK, Toft E, Taylor D, Meyer JM (2011) Assessing QT interval prolongation and its associated risks with antipsychotics. CNS Drugs 25:473–490. https://doi.org/10.2165/11587800-000000000-00000
Okayasu H, Ozeki Y, Fujii K, Takano Y, Shinozaki T, Ohrui M, Shimoda K (2019) Investigation of the proarrhythmic effects of antidepressants according to QT Interval, QT dispersion and T wave peak-to-end interval in the clinical setting. Psychiatry Investig 16:159–166. https://doi.org/10.30773/pi.2018.12.11
Acknowledgements
We thank Prof. Malik from the Department of Cardiological Sciences, St. George’s Hospital Medical School, London, for providing us computational outputs that enabled us to test the reliability of our algorithm. We also thank Faye Schreiber, MS from Meir Medical Center for editorial assistance.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have any conflict of interest. No industry supported trial data or relationships influenced the collection or analysis of these data.
Ethical approval
The study was approved by the Sheba Medical Center ethics committee. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all study participants.
Data available
Data will be made available upon reasonable request from the corresponding author.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stahi, T., Kaminer, K., Gur, E. et al. T-wave morphology descriptors in patients with bulimia nervosa. Eat Weight Disord 26, 661–666 (2021). https://doi.org/10.1007/s40519-020-00905-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-020-00905-8