Abstract
Background
Exercise addiction is associated with multiple adverse outcomes and can be classified as co-occurring with an eating disorder, or a primary condition with no indication of eating disorders. We conducted a meta-analysis exploring the prevalence of exercise addiction in adults with and without indicated eating disorders.
Methods
A systematic review of major databases and grey literature was undertaken from inception to 30/04/2019. Studies reporting prevalence of exercise addiction with and without indicated eating disorders in adults were identified. A random effect meta-analysis was undertaken, calculating odds ratios for exercise addiction with versus without indicated eating disorders.
Results
Nine studies with a total sample of 2140 participants (mean age = 25.06; 70.6% female) were included. Within these, 1732 participants did not show indicated eating disorders (mean age = 26.4; 63.0% female) and 408 had indicated eating disorders (mean age = 23.46; 79.2% female). The odds ratio for exercise addiction in populations with versus without indicated eating disorders was 3.71 (95% CI 2.00–6.89; I2 = 81; p ≤ 0.001). Exercise addiction prevalence in both populations differed according to the measurement instrument used.
Discussion
Exercise addiction occurs more than three and a half times as often as a comorbidity to an eating disorder than in people without an indicated eating disorder. The creation of a measurement tool able to identify exercise addiction risk in both populations would benefit researchers and practitioners by easily classifying samples.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Regular and sustained participation in physical activity and exercise (one domain of physical activity) has been shown to yield several positive health outcomes, including improvements in mental health conditions [1], cardio-vascular disease [2] and well-being [3]. There is evidence, however, suggesting that for a sub-set of people, exercise can become obsessive, or compulsive (or both), to a point where negative health outcomes are experienced, with physical outcomes including bone fractures, psychological outcomes including increased anxiety, and social outcomes including the detriment of social relationships and financial debt [4]. Several terms have been used to describe the phenomenon, including ‘exercise dependence’ and ‘compulsive exercise’ [5, 6]. Unfortunately, several authors have failed to provide definitions for these terms, making the interpretation of findings in the related literature challenging [7]. In this paper, the term exercise addiction (EA) will be used, as it has been suggested as the most appropriate as it includes aspects of dependence and compulsion [8, 9], and can be defined as ‘a morbid pattern of behaviour in which the habitually exercising individual loses control over his or her exercise habits and acts compulsively, exhibits dependence, and experiences negative consequences to health as well as in his or her social and professional life’ [7].
Early conceptualization in this area suggested a distinction between being highly committed to exercise and EA, with committed, non-EA, subjects exercising mainly for extrinsic rewards, not seeing exercise as central to their life, and suffering fewer and/or less severe symptoms of withdrawal upon cessation [10]. Concurrently, EA subjects exercise for intrinsic rewards, seeing exercise as central to their life, and suffer severe psychological and physiological withdrawal upon cessation [11]. Many theoretical models have been proposed to explain EA, including the Sympathetic Arousal Hypothesis [12], the Cognitive Appraisal Hypothesis [13], the IL-6 model [14], Four Phase model [15], Biopsychosocial model [16]. Furthermore, Egorov and Szabo [17] updated the Cognitive Appraisal Hypothesis with their Interactional Model of EA. Disparities between these models indicate a lack of etiologic consensus amongst researchers, which could be one reason why the phenomenon has not been officially classified as a behavioural disorder in The Diagnostic and Statistical Manual of Mental Disorders 5 [18] or the International Classification of Diseases 11th Revision [19].
Several screening measures have been developed for assessing the risk of EA, with earlier ones lacking underlying theoretical frameworks, including the Obligatory Exercise Questionnaire (OEQ) [20] and the Exercise Dependence Questionnaire (EDQ) [21]. More recent screening measures have used underlying theoretical models, such as the Exercise Dependence Scale (EDS) [22], which uses Diagnostic and Statistical Manual of Mental Disorders 4 [23] criteria for substance abuse, and the Exercise Addiction Inventory (EAI) [24], based on Brown’s [25, 26] components of behavioural addictions. Currently, there is no consensus as to which questionnaire is the most appropriate; however, the most commonly used in recent studies are the EAI and the EDS [7].
EA has been shown to be highly prevalent in populations that have either indicated or clinically diagnosed eating disorders (EDs), with prevalence rates in these populations ranging from 29 to 80% [27, 28]. This is supported by Berczik et al.’s [9] classification of EA being sandwiched between ‘body-dysmorphic disorder’ and ‘anorexia nervosa’ on Hollander and Wong’s [29] compulsive–obsessive spectrum. Of the different types of EDs, in-patients with clinically diagnosed restricting-type anorexia nervosa (AN) have been shown to have higher prevalence rates of EA (80%) when compared with binge/purging-type AN (43.3%), purging-type bulimia nervosa (BN; 39.3%), and EDs not otherwise specified (EDNOS; 31.9%) [30]. High prevalence of EA in patients with AN is of particular concern as these subjects have been shown to have the highest mortality rates of all EDs [31,32,33], as well as having an increased risk of osteopenia, osteoporosis, and related fractures [34]. It has been reported that subjects with indicated EDs and EA often present with stress fractures and engage in excessive exercising despite injury, with some subjects reporting exercising because it feels like a compulsion rather than for enjoyment [35, 36]. Considering that weight gain is one of the primary aims of treatment of patients with EDs (particularly AN) [37, 38], excessive exercise can result in longer periods to achieve the desired weight gain, which can be costly from a service provision prospective.
EA has also been shown to be prevalent in populations that show no evidence of indicated EDs (failing to reach published cut-off in ED testing questionnaires). For instance, a recent meta-analysis found 11.4% of health club users had EA in the absence of indicated EDs [39] Some primary studies have also shown significant differences between prevalence rates of EA with and without indicated EDs, with EA in the absence of EDs showing consistently lower prevalence rates than subjects with indicated EDs [27, 28]. Furthermore, a recent meta-analysis explored the prevalence of EA in different populations; however, offers no information on the ED status of the populations [40], making it unclear if the prevalence of EA differs by ED status.
Despite the potential differences in the underlying prevalence and potential adverse events of EA between those without and without indicated EDs, it is unknown whether EA risk differs substantially in subjects with and without indicated ED. Moreover, pooled prevalence rates and differences between pooled prevalence rates are unknown. Therefore, the primary aim of this study was, using meta-analytic techniques, to calculate ORs for EA in subjects with and without ED symptomology, and systematically compare the prevalence of EA according to EA measurement tools. Understanding this is essential to understanding more about these conditions, and could inform the creation of new measurement tools, as well as informing the development of targeted interventions. Considering that primary studies have reported that the prevalence of EA with indicated EDs is higher than those without indicated EDs [27, 28], we hypothesised that when comparing studies systematically we would find that EA is more prevalent in subjects with indicated EDs than without.
Methods
This systematic review was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria and the recommendations in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [41, 42].
Search strategy
Two investigators (MT, LS) searched PsycINFO, Medline, SportDiscuss and Open Grey from inception to 30/04/19 for articles written in English. The search terms (title of article) used were (exercise OR physical activity OR fitness OR sport OR sports) and (addition OR dependence OR dependency OR compulsion OR addict) or (maladaptive OR excessive OR compulsive OR obligatory OR obsessive) and (exercise OR physical activity OR fitness OR exerciser OR exercisers OR sport OR sports). The reference lists of the articles included in the analysis were hand-searched to identify additional literature, and conference abstracts were also considered.
Study selection
Titles and abstracts were independently assessed by two authors (MT, LS) for eligibility against the inclusion and exclusion criteria.
Inclusion criteria
Articles were included that met the following criteria:
-
1.
Studies that reported an EA with and without indicated EDs OR or statistics sufficient to calculate such an OR.
-
2.
Written in English.
-
3.
In adults (≥ 18 years).
-
4.
That measured the prevalence of EA in any population using any validated measuring tool of EA with established cut-offs (as per original authors’ guidelines) that define subjects as at risk of EA.
-
5.
Tested for indicated EDs using a validated measure.
-
6.
That used the same study population to determine EA prevalence rates in indicated and non-indicated ED populations (to eliminate population bias).
Exclusion criteria
-
1.
Non-adults (< 18 years).
Data extraction
The following information was extracted by the lead author including demographic [age, sex, body mass index (BMI)] and prevalence (total EA with and without indicated EDs n, EA with and without indicated EDs events n, measuring instrument of EA, measuring instrument of ED) data, and missing information was obtained where possible by contacting lead authors (see Acknowledgments). If prevalence data were missing and the authors did not respond/have access to the data (two attempted contacts to authors over a 1-month period), these studies were excluded. Prevalence data were then converted into ORs. Studies with missing demographic data, but full EA with and without indicated ED prevalence data, were included. Subjects were then categorised into two groups: subjects that failed to meet published cut-offs (as defined by the original author article) for EDs in the non-indicated ED group, and subjects that scored over the published cut-offs for EDs in the indicated ED group. In both ED status sub-groups, subjects that met the published cut-offs for EA were, respectively, categorised as EA.
Meta-analysis
A random-effects model was conducted, weighting studies based on the inverse variance, and calculating odds ratios (ORs) and prevalence rates with 95% confidence intervals (CIs) using Comprehensive Meta-Analysis version 3 [43]. The primary aim was to calculate ORs of EA in populations with and without indicated EDs. The meta-analysis was conducted in the following steps: 1. ORs of EA comparing those with and without indicated EDs were calculated with 95% CIs using a mixed effects analysis. 2. Heterogeneity was assessed with the Cochrane Q [44] and I2 [45] statistics for all analyses. 3. Sub-group analysis comparing ORs of EA in populations with and without indicated ED by EA measurement tool. Publication bias was assessed with a visual inspection of funnel plots and with the Begg–Mazumdar–Kendall’s tau [46] and Egger bias test [47]. As per recommendations from Fu et al. and Sterne et al. [48, 49], these tests were only conducted if the number of studies exceeded ten. If the Egger bias test was significant, to adjust for potential publication bias, the trim-and-fill adjusted analysis was used to remove the most extreme small studies from the positive side of the funnel plot and effect sizes re-calculated, until the funnel plot was symmetrical with the new effect size [50]. A sensitivity analyses was calculated around the primary analyses, using a one-study removed method. This was to detect whether the observed effect was overly influenced by any one study.
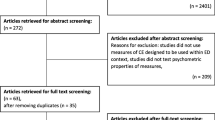
Results
The literature search yielded 1375 results, of which 369 were removed as duplicates, leaving 1006 studies screened using title and abstract. From the 1006 titles and abstracts screened, 223 studies were selected for full-text review. Of the 223 studies reviewed, 9 studies were eligible for inclusion. Reasons for exclusion are shown in Fig. 1 and descriptive statistics for included studies are shown in Table 1. From the 9 included studies, there were a total of 2140. 1732 subjects scored below published ED cut-offs and were categorised as the non-indicated ED group, of which 342 scored above EA cut-offs and were defined as exercise addicted. 408 subjects scored above the published ED cut-offs and were categorised as the indicated ED group, of which 225 scored above EA cut-off and were defined as EA. The methods of measuring EA were the Exercise Dependence Questionnaire [21], the Exercise Dependence Scale [22], the Obligatory Exercise Questionnaire [20], and the Exercise Addiction Inventory [24]. The methods of measuring for indicated EDs were the Eating Attitudes Test 40 [51], the Eating Attitudes Test 26 [52], the Eating Disorder Examination Questionnaire [53], the Eating Disorder Inventory-2 [54], and the SCOFF Questionnaire [55].
Meta-analysis results
ORs of EA in populations with and without indicated EDs
The pooled OR of EA in populations with indicated EDs compared to those without indicated EDs was 3.71 (95% CI 2.00-6.89; I2 = 81.159; p ≤ 0.001; Egger bias = 2.054 p = 0.480; trim-and-fill adjustment not required). The meta-analysis forest plot is shown in Fig. 2.
Sensitivity analysis
The direction or significance of the ORs was not changed by the sensitivity analysis, with point estimates ranging from 3.019 to 4.755. One study [56] had a large effect of the magnitude of the result, with the removal of this study yielding an estimate of 4.755 (95% CI 2.875–7.863; p ≤ 0.001)
Sub-group analysis of EA prevalence in populations with and without indicated ED by EA measurement type
As shown in Table 2, the OR of EA among subjects with indicated vs no-indicated EDs was highest when measured with the OEQ (6.9; 95% CI 2.2–21.8), followed by the EAI (4.2; 95% CI = 1.4–12.2), the EDS (3.9; 95% CI = 1.2–12.5), with the EDQ yielding the lowest OR (2.4; 95% CI 1.0–5.7).
Discussion
This meta-analysis of 9 studies demonstrated that the OR of EA in populations with vs without indicated EDs was 3.7. The sensitivity analysis showed that the direction and significance of the findings were unchanged when one study was removed. ORs also differed largely in both populations depending on the EA measurement tool being used.
Subjects who score above published cut-offs for EDs are over three times more likely to be at risk of EA, with observed prevalence rates in subjects with indicated EDs comparing well with EA studies conducted on clinical ED populations [35, 57]. One possible reason is that excessive exercise has been consistently shown to be an inherent part of several types of EDs, with patients demonstrating aversions to weight gain and showing obsessions towards not gaining weight [58]. Furthermore, ED subjects have been shown to score higher on addictive personality measures and obsessive–compulsive behaviours [59]. Considering this, future studies that use clinically diagnosed ED patients (of all types of EDs) would be useful. Given that EA can be secondary to an ED and with the results of this study suggesting that subjects who show ED symptomology have significantly higher prevalence of EA, this adds to the evidence suggesting that practitioners working with ED patients should consider monitoring exercise levels a priority, as ED patients have been shown to suffer from serious medical conditions as a result of excessive exercise, such as fractures, increased rates of cardiovascular disease in younger patients and increased overall mortality [34].
The large difference in EA prevalence observed between indicated and non-indicated ED groups adds to evidence suggesting that ED symptomology should be screened for in all studies that measure EA. The current meta-analysis excluded 93 studies that failed to measure ED symptomology, which agrees with recent reviews suggested that the EA literature has not readily distinguished between ED status as standard practice [60]. Currently, to measure EA and screen for EDs, two questionnaires are needed. Future work to create a new tool that screens for EDs and EA in one single tool would be beneficial. Not only would this benefit researchers by only having to use one tool to categorise EA with and without indicated EDs, it could also be beneficial in both clinical and public health settings by highlighting at-risk subjects earlier, which could inform (in ED subjects) specialised nursing observation and bathroom supervision to regulate EA behaviours be implemented earlier in treatment. Moreover, earlier categorisation of EA with an indicated ED has the potential to allow practitioners such as general practitioners, physiotherapists and health practitioners to therapeutically explore EA at an earlier point.
The large differences in prevalence rates by EA measurement tool are a further indication that differing EA measurement tools are measuring different aspects of the same phenomenon, with the two tools with no underlying theories (OEQ and EDQ) yielding higher ORs than the two tools that use underlying addiction theories (EAI and EDS). To date, no studies have been conducted comparing subjects who score above the published thresholds for different EA measurement tools and clinical interviews to determine the sensitivity of these tools. It is, therefore, difficult to recommend a specific measurement tool. It is the authors’ view that the EAI and EDS be used until such studies are conducted, as they both are based on underlying theories of addiction and have been described as comparable by several authors [8, 9].
Limited research has been conducted exploring possible treatments for EA. Much of the focus of treatment has been focussed around cognitive behaviour therapies, yet their effectiveness has been shown to be limited [61]. Adams, Miller and Kraus [62] suggested specific therapeutic guidelines for subjects with EA, although Lichtenstein et al. [63] comment that studies to test these guidelines are sparse. Although one individual pharmacological case study has been conducted with an EA patient showing lower EAI scores post-4 weeks of taking an anti-psychotic drug (Quetiapine) [64], no other pharmacological treatments have been explored. Due to the higher rates of serious injury and mortality amongst ED patients, treatment for ED should be prioritised over treatment specifically for EA, although further research is required to explore the relationships between the two so that effective treatments can be refined and/or developed.
While this meta-analysis is the first to measure EA prevalence rates in populations with and without indicated EDs, the findings should be considered within the limitations of this study. First, the heterogeneity of population groups and measurement tools (for EA and ED) and very small sample sizes means that this should only be considered a broad overview; further studies are needed to determine more accurate prevalence rates, using homogeneous tools. Second, the use of questionnaires for testing for EDs has limited applications to clinical diagnoses. Third, the use of the questionnaires in this study precluded the sub-categorisation of different types of EDs, which is relevant as previous research has shown prevalence rates to differ depending on the type of ED [30]. Moreover, athletic subjects who use ED testing questionnaires have been shown to under-report due to possible stigmatisation, with false-positives a possibility [53, 65]. Lastly, there was high heterogeneity which we could not fully explain.
What is already known?
It is known that exercise addiction exists both as a primary condition without indicated eating disorders, and as a secondary condition to an eating disorder. What is unknown is the magnitude of risk for EA with an indicated eating disorder vs no-indicated eating disorders.
What does this study add?
Subjects with indicated eating disorders are over 3.5 times more likely to suffer from addiction to exercise than their non-indicated eating disorder counterparts. Due to the higher risk of mortality in subjects with eating disorders, this study adds to the evidence that exercise levels should be closely monitored in these populations. Furthermore, the absence of eating disorders does not preclude the risk of being addicted to exercise. Further study in this area to explore treatments and the effect on quality of life is warranted.
Conclusion
The OR for EA in populations with vs without indicated EDs is 3.7, with EA being significantly more prevalent in subjects with indicated EDs than in subjects without indicated EDs, adding to the evidence that practitioners working with ED subjects should closely monitor exercise levels. However, even in those showing no indicated EDs, EA is of notable prevalence—EA should not be discounted entirely on the basis of no indicated ED behaviours. It is also recommended that all future research exploring the prevalence of EA test for EDs to determine accurate prevalence rates.
References
Mikkelsen K, Stojanovska L, Polenakovic M, Bosevski M, Apostolopoulos V (2017) Exercise and mental health. Maturitas. Elsevier 106:48–56. https://doi.org/10.1016/j.maturitas.2017.09.003
Wilson MG, Ellison GM, Cable NT (2016) Basic science behind the cardiovascular benefits of exercise. Br J Sport Med. BMJ 50:93–99. https://doi.org/10.1136/bjsports-2014-306596rep
Mandolesi L, Polverino A, Montuori S, Foti F, Ferraioli G, Sorrentino P et al (2018) Effects of physical exercise on cognitive functioning and wellbeing: biological and psychological benefits. Front Psychol Front 9:509. https://doi.org/10.3389/fpsyg.2018.00509
Landolfi E (2013) Exercise addiction. Sport Med 43:111–119. https://doi.org/10.1007/s40279-012-0013-x
Leuenberger A (2006) Endorphins, exercise, and addictions: a review of exercise dependence. Prem J Undergrad Publ Neurosci 3:1–9. Available from https://impulse.appstate.edu/sites/impulse.appstate.edu/files/2006_06_05_Leuenberger.pdf
Adams J (2009) Understanding exercise dependence. J Contemp Psychother 39:231–240. https://doi.org/10.1007/s10879-009-9117-5
Szabo A, Griffiths MD, de La Vega Marcos R, Mervó B, Demetrovics Z (2015) Methodological and conceptual limitations in exercise addiction research. Yale J Biol Med 88:303–308. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=26339214&site=ehost-live
Goodman A (1990) Addiction: definition and implications. Br J Addict 85:1403–1408. https://doi.org/10.1111/j.1360-0443.1990.tb01620.x
Berczik K, Szab A, Griffiths MD, Kurimay T, Kun B, Urbán R et al (2012) Exercise addiction: symptoms, diagnosis, epidemiology, and etiology. Subst Use Misuse 47:403–417. https://doi.org/10.3109/10826084.2011.639120
de Coverley Veale DM (1987) Exercise dependence. Br J Addict 82:735–740. https://doi.org/10.1111/j.1360-0443.1987.tb01539.x
Sachs ML (1981) Running Addiction. In: Sachs M, Sachs M (eds) Psychol run. Human Kinetics, Champaign, pp 116–126
Thompson JK, Blanton P (1987) Energy conservation and exercise dependence: a sympathetic arousal hypothesis. Med Sci Sports Exerc. https://doi.org/10.1249/00005768-198704000-00005
Szabo A (1995) The impact of exercise deprivation on well-being of habitual exercisers. Aust J Sci Med Sport 27:68–75. Available from: http://articles.sirc.ca/search.cfm?id=390518
Hamer M, Karageorghis CI (2007) Psychobiological mechanisms of exercise dependence. Sports Med 37:477–484. https://doi.org/10.2165/00007256-200737060-00002
Freimuth M, Moniz S, Kim SR (2011) Clarifying exercise addiction: differential diagnosis, co-occurring disorders, and phases of addiction. Int J Environ Res Public Health 8:4069–4081. https://doi.org/10.3390/ijerph8104069
McNamara J, McCabe MP (2012) Striving for success or addiction? Exercise dependence among elite Australian athletes. J Sports Sci 30:755–766. https://doi.org/10.1080/02640414.2012.667879
Egorov AY, Szabo A (2013) The exercise paradox: an interactional model for a clearer conceptualization of exercise addiction. J Behav Addict 2:199–208. https://doi.org/10.1556/jba.2.2013.4.2
American Psychiatric Association. DSM-V. Am. J. Psychiatry. 2013
WHO (2019) WHO| international classification of diseases, 11th revision (ICD-11). WHO
Pasman L, Thompson JK (1988) Body image and eating disturbance in obligatory runners, obligatory weightlifters, and sedentary individuals. Int J Eat Disord 7:759–769. https://doi.org/10.1002/1098-108x(198811)7:6%3C759:aid-eat2260070605%3E3.0.co;2-g
Ogden J, Veale D, Summers Z (1997) The development and validation of the exercise dependence questionnaire. Addict Res 5:343–355. https://doi.org/10.3109/16066359709004348
Hausenblas HA, Downs DS (2002) How much is too much? The development and validation of the exercise dependence scale. Psychol Health 17:387–404. https://doi.org/10.1080/0887044022000004894
Diagnostic and Statistical Manual of Mental Disorders (2000) Fourth Edition, Text Revision (DSM-IV-TR)
Terry A, Szabo A, Griffiths M (2004) The exercise addiction inventory: a new brief screening tool. Addict Res Theory 12:489–499. https://doi.org/10.1080/16066350310001637363
Brown RIF (1993) Some contributions of the study of gambling to the study of other addictions. Gambl Behav Probl Gambl 1:241–272
Brown RIF (1997) A theoretical model of the behavioural addictions–applied to offending. Addict Crime 13–65
Dalle Grave R, Calugi S, Marchesini G (2008) Compulsive exercise to control shape or weight in eating disorders: prevalence, associated features, and treatment outcome. Compr Psychiatry 49:346–352. https://doi.org/10.1016/j.comppsych.2007.12.007
Bratland-Sanda S, Martinsen EW, Rosenvinge JH, Rø O, Hoffart A, Sundgot-Borgen J (2011) Exercise dependence score in patients with longstanding eating disorders and controls: the importance of affect regulation and physical activity intensity. Eur Eat Disord Rev J Eat Disord Assoc 19:249–255. https://doi.org/10.1002/erv.971
Hollander E, Kwon JH, Stein DJ, Broatch J, Rowland CT, Himelein CA (1996) Obsessive-compulsive and spectrum disorders: overview and quality of life issues. J Clin Psychiatry 57(SUPPL. 8):3–6
Dalle Grave R (2009) Features and management of compulsive exercising in eating disorders. Phys Sportsmed 37:20–28. https://doi.org/10.3810/psm.2009.10.1725
Smink FRE, van Hoeken D, Hoek HW (2012) Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 14:406–414. https://doi.org/10.1007/s11920-012-0282-y
Sauchelli S, Arcelus J, Granero R, Jiménez-Murcia S, Agüera Z, Del Pino-Gutiérrez A et al (2017) Dimensions of compulsive exercise across eating disorder diagnostic subtypes and the validation of the Spanish version of the compulsive exercise test. Front Psychol 7:1852. https://doi.org/10.3389/fpsyg.2016.01852
Arcelus J, Mitchell AJ, Wales J, Nielsen S (2011) Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. JAMA Psychiatry 68:724–731. https://doi.org/10.1001/archgenpsychiatry.2011.74
Solmi M, Veronese N, Correll CU, Favaro A, Santonastaso P, Caregaro L et al (2016) Bone mineral density, osteoporosis, and fractures among people with eating disorders: a systematic review and meta-analysis. Acta Psychiatr Scand 133:341–351. https://doi.org/10.1111/acps.12556
Klein DA, Bennett AS, Schebendach J, Foltin RW, Devlin MJ, Walsh BT (2004) Exercise “addiction” in anorexia nervosa: model development and pilot data. CNS Spectr 9:531–537. https://doi.org/10.1017/s1092852900009627
Laban MM, Wilkins JC, Sackeyfio AH, Taylor RS (1995) Osteoporotic stress fractures in anorexia nervosa: etiology, diagnosis, and review of four cases. Arch Phys Med Rehabil Elsevier 76:884–887. https://doi.org/10.1016/s0003-9993(95)80558-3
Misra M, Klibanski A (2011) Bone health in anorexia nervosa. Curr Opin Endocrinol Diabetes Obes. https://doi.org/10.1097/MED.0b013e32834b4bdc
Kaye WH, Gwirtsman HE, Obarzanek E, George DT (1988) Relative importance of calorie intake needed to gain weight and level of physical activity in anorexia nervosa. Am J Clin Nutr. https://doi.org/10.1093/ajcn/47.6.989
Trott M, Jackson S, Firth J, Stubbs B, Smith L (2019) Exercise addiction prevalence and correlates in the absence of eating disorder symptomology. J Sports Sci 37:1–93. https://doi.org/10.1080/02640414.2019.1671688
Di Lodovico L, Poulnais S, Gorwood P (2019) Which sports are more at risk of physical exercise addiction: a systematic review. Addict Behav 93:257–262. https://doi.org/10.1016/j.addbeh.2018.12.030
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100. https://doi.org/10.7326/0003-4819-151-4-200908180-00136
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4:e296. https://doi.org/10.7554/elife.08500.009
Borenstein M, Hedges L, Higgins J, Rothstein H (2013) Comprehensive meta analysis. Biostat, Englewood
Cochran WG (1954) The combination of estimates from different experiments. Biometr JSTOR 10:101–129. https://doi.org/10.2307/3001666
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med Wiley 21:1539–1558. https://doi.org/10.1002/sim.1186
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics. https://doi.org/10.2307/2533446
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta—analysis detected by a simple, graphical test. BMJ Br Med J. https://doi.org/10.1136/bmj.315.7109.629
Fu R, Gartlehner G, Grant M, Shamliyan T, Sedrakyan A, Wilt TJ et al (2011) Conducting quantitative synthesis when comparing medical interventions: aHRQ and the Effective Health Care Program. J Clin Epidemiol. https://doi.org/10.1016/j.jclinepi.2010.08.010
Sterne JA, Egger M, Moher D (2008) Addressing reporting biases. Cochrane Handb Syst Rev Interv Cochrane B Ser. https://doi.org/10.1002/9780470712184.ch10
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. https://doi.org/10.1111/j.0006-341x.2000.00455.x
Garner DM, Garfinkel PE (1979) The eating attitudes test: an index of the symptoms of anorexia nervosa. Psychol Med Camb Univ Press 9:273–279. https://doi.org/10.1017/s0033291700030762
Garner DM, Olmsted MP, Bohr Y, Garfinkel PE (1982) The eating attitudes test: psychometric features and clinical correlates. Psychol Med 12:871–878. https://doi.org/10.1017/s0033291700049163
Fairburn CG, Beglin SJ (1994) Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord 16:363–370. https://doi.org/10.1002/1098-108X(199412)16:4%3C363:AID-EAT2260160405%3E3.0.CO;2-%23
Garner DM (1991) Eating disorder inventory-2: professional manual. Psychological Assessment Resources. Inc, Florida
Morgan JF, Reid F, Lacey JH (1999) The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ 319:1467–1468. https://doi.org/10.1136/bmj.319.7223.1467
Grandi S, Clementi C, Guidi J, Benassi M, Tossani E (2011) Personality characteristics and psychological distress associated with primary exercise dependence: an exploratory study. Psychiatry Res 189:270–275. https://doi.org/10.1016/j.psychres.2011.02.025
Dalle Grave R (2008) Excessive and compulsive exercises in eating disorders: prevalence, associated features, and management. Dir Psychiatry 28:273–282. https://doi.org/10.1016/j.comppsych.2007.12.007
Davis C, Katzman DK, Kaptein S, Kirsh C, Brewer H, Kalmbach K et al (1997) The prevalence of high-level exercise in the eating disorders: etiological implications. Compr Psychiatry 38:321–326. https://doi.org/10.1016/s0010-440x(97)90927-5
Davis C, Claridge G (1998) The eating disorders as addiction: a psychobiological perspective. Addict Behav 23:463–475. https://doi.org/10.1016/S0306-4603(98)00009-4
Symons Downs D, MacIntyre RI, Heron KE (2019) Exercise addiction and dependence. In: Anshel MH, Petruzzello SJ, Labbé EE (eds), APA Handb Sport Exerc Psychol Vol 2 Exerc Psychol vol 2, p 589–604. https://doi.org/10.1037/0000124-030
Weinman A, Weinman Y (2014) Exercise addiction- diagnosis, bio-psychological mechanisms and treatment issues. Curr Pharm Des 20:4062–4069. https://doi.org/10.2174/13816128113199990614
Adams JM, Miller TW, Kraus RF (2003) Exercise dependence: diagnostic and therapeutic issues for patients in psychotherapy. J Contemp 33:93–107. https://doi.org/10.1023/A:1022883104269
Lichtenstein MB, Hinze CJ, Emborg B, Thomsen F, Hemmingsen SD (2017) Compulsive exercise: links, risks and challenges faced. Psychol Res Behav 10:85–95. https://doi.org/10.2147/prbm.s113093
Di Nicola M, Martinotti G, Mazza M, Tedeschi D, Pozzi G, Janiri L (2010) Quetiapine as add-on treatment for bipolar I disorder with comorbid compulsive buying and physical exercise addiction. Prog Neuropsychopharmacol Biol Psychiatry 34:713–714. https://doi.org/10.1016/j.pnpbp.2010.03.013
Sundgot-Borgen J, Torstveit MK (2004) Prevalence of eating disorders in elite athletes is higher than in the general population. Clin J Sport Med. https://doi.org/10.1097/00042752-200401000-00005
Bamber D, Cockerill IM, Carroll D (2000) The pathological status of exercise dependence. Br J Sports Med 34:125–132. https://doi.org/10.1136/bjsm.34.2.125
Blaydon MJ, Lindner KJ (2002) Eating disorders and exercise dependence in triathletes. Eat Disord. 10:49–60. https://doi.org/10.1080/106402602753573559
Blaydon MJ, Linder KJ, Kerr JH (2004) Metamotivational characteristics of exercise dependence and eating disorders in highly active amateur sport participants. Pers Individ Differ 36:1419–1432. https://doi.org/10.1016/s0191-8869(03)00238-1
De Young KP, Anderson DA (2010) The importance of the function of exercise in the relationship between obligatory exercise and eating and body image concerns. Eat Behav 11:62–64. https://doi.org/10.1016/j.eatbeh.2009.09.001
Di Lodovico L, Dubertret C, Ameller A (2018) Vulnerability to exercise addiction, socio-demographic, behavioral and psychological characteristics of runners at risk for eating disorders. Compr Psychiatry 81:48–52. https://doi.org/10.1016/j.comppsych.2017.11.006
Lease HJ, Bond MJ (2013) Correspondence between alternate measures of maladaptive exercise, and their associations with disordered eating symptomatology. J Behav Addict 2:153–159. https://doi.org/10.1556/jba.2.2013.012
Meulemans S, Pribis P, Grajales T, Krivak G (2014) Gender differences in exercise dependence and eating disorders in young adults: a path analysis of a conceptual model. Nutrients 6:4895–4905. https://doi.org/10.3390/nu6114895
Serier KN, Smith JE, Lash DN, Gianini LM, Harriger JA, Sarafin RE et al (2018) Obligatory exercise and coping in treatment-seeking women with poor body image. Eat Weight Disord 23:331–338. https://doi.org/10.1007/s40519-018-0504-3
Acknowledgements
The authors wish to express their gratitude to Malcolm Bond, Kyle De Young, Kelsey Serier and Laura Di Lodovico for their help and support in the collection of raw data for analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was granted ethical approval by Anglia Ruskin University.
Informed consent
Informed consent was not requried due to this being a systematic review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Trott, M., Jackson, S.E., Firth, J. et al. A comparative meta-analysis of the prevalence of exercise addiction in adults with and without indicated eating disorders. Eat Weight Disord 26, 37–46 (2021). https://doi.org/10.1007/s40519-019-00842-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00842-1