Abstract
Background
Exposure therapy is the most effective treatment for anxiety and related disorders and its efficacy in the eating disorders is rapidly gaining support. Despite the strong evidence behind exposure therapy, many anxiety disorder providers do not endorse the usage of exposure therapy. Limited research has explored the use of exposure therapy in eating disorder providers, as well as the impact of framing on likelihood to use exposure therapy.
Objective
The current study (N = 125 eating disorder providers) manipulated the framing of exposure to feared foods (pizza).
Methods
We framed the treatment as an exposure, behavioral experiment, or acceptance/mindfulness-based intervention. We also tested attitudes towards exposure therapy in eating disorder providers.
Results
Participants were more likely to endorse willingness to use a treatment framed as a behavioral experiment over exposure and acceptance-based framing. This effect did not vary by degree type, type of provider, years in practice, experience, or training. We also found that providers with more training, specifically in eating disorder exposure, were more likely to use exposure over acceptance-based framed intervention (and vice versa). Finally, we found that eating disorder providers had a somewhat positive view of exposure therapy.
Conclusion
Framing of the intervention impacts likelihood that providers will endorse using specific interventions. Therefore, intervention development and dissemination efforts should consider the language around the description of evidence-based treatments. Furthermore, enhanced training and education specifically with eating disorder exposure therapy may enhance the likelihood of providers utilizing exposure therapy.
Level I: experimental study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Exposure is at the core of most effective treatments for anxiety disorders [1] and its application in the treatment of eating disorders is growing. For example, exposure and response prevention (ERP) has been used to expose individuals with bulimia nervosa (BN), binge eating disorder (BED), and anorexia nervosa (AN) binge-purge type to binge eating (i.e. craved food) and purging (i.e. restroom) cues to prevent subsequent behaviors [2,3,4]. In exposure and response prevention for AN (AN-EXRP), individuals are exposed to feared foods according to individual hierarchies (list of the least to the most anxiety provoking foods) and prevented from engaging in ritualistic behaviors (i.e. body checking [5, 6]). AN-EXRP was found to lead to increased caloric intake and outperformed cognitive remediation therapy [7,8,9]. Mirror exposure has also been successfully used to reduce body dissatisfaction, body checking and avoidance [10, 11]. Additional novel applications of exposure therapy for eating disorders aim to target fears of weight gain, intolerance of uncertainty, and other feared outcomes [6, 12].
Despite decades of research on the benefits of exposure therapy for anxiety and related disorders, exposure is underutilized in the treatment of anxiety disorders, post-traumatic stress disorder, obsessive–compulsive disorders, as well as eating disorders [6, 12]. Previous studies suggest that access to training and supervision, quality of training, client characteristics (i.e., severity of presentation), and therapist characteristics (i.e., level of education, theoretical orientation, anxiety sensitivity) and therapist attitudes (i.e., fear of upsetting the client) play a role in adoption and use of exposure therapy [13]. For example, some therapists believe that exposure therapy may be too distressing for their clients and may lead to worsening of symptoms or treatment dropout [14]. Therapists with higher levels of education and higher self-efficacy in being able to administer exposure treatment are associated with greater use of exposure [13]. Similar barriers have been identified in the utilization of exposure in the treatment of eating disorders. Therapists who are older and more experienced and those with high levels of anxiety are less likely to employ this intervention [15, 16].
Given the evidence supporting the benefits of exposure therapy and the growing literature supporting exposure therapy (i.e., specifically formal exposure therapy with a feared stimuli present and the target of increasing anxiety during the exposure) for eating disorders specifically, more research is needed to test how to improve utilization of exposure and why providers may (or may not) use exposure therapy with their patients. As has been noted by several established clinical researchers and treatment developers, many interventions used in clinical psychology contain similar aspects, but may be presented to patients or providers using different language [17,18,19]. This opinion has been purported by different theorists, with some suggesting that many of our established treatments (i.e., CBT, acceptance and commitment therapy) are different names for the same thing. Therefore, it seems highly plausible that the way in which the therapy is described (or framed) may impact the likelihood that providers will utilize the treatment.
In technical terms, framing refers to how a message is presented can impact how providers and clients respond to treatments, so much so that framing can be used to promote health behaviors [20, 21]. For example, gain-framed messages (i.e., emphasizing benefits of a particular behavior vs. consequences of failing to engage in it) were found effective in increasing physical activity, smoking cessation, and skin cancer prevention [22]. It seems plausible that how exposure therapy is framed to providers may impact providers’ attitudes and increase treatment motivation and adherence. For example, Arch and Craske proposed that framing exposure in value-based terms, rather than as anxiety symptom reduction may be helpful [17]. An experimental study found that framing of exposure therapy did not affect the client’s perceived credibility of the intervention [23]; however, framing has not yet been tested with regards to providers’ (rather than clients) likelihood to use the treatment.
To our knowledge, no study has examined if framing of exposure therapy affects clinician’s attitudes about utilizing this intervention, specifically within the field of eating disorders. Framing may help alleviate some of the clinician barriers such as believing that the intervention will cause the client too much distress [14] and clinician’s levels of anxiety [15], as well as appeal to various theoretical orientations. One way to frame exposure therapy is to present it as a behavioral experiment. Another way to frame exposure is as mindfulness/acceptance-based treatment (i.e., accepting or being mindful of emotions). Several researchers have pointed out the similarities between these interventions [18, 24, 25]. Additionally, mindfulness/acceptance-based interventions are conceptualized as consistent with the behavioral tradition [26].
The current study had two primary goals. First, to examine attitudes toward exposure therapy in eating disorder providers. Second, to test if manipulating the framing of a similar intervention impacted the likelihood that providers would endorse likelihood to use the intervention. We hypothesized that providers would have a somewhat negative view toward exposure therapy, given the literature from the anxiety disorder field. We also hypothesized that providers would be more likely to endorse using an intervention when it was framed as a behavioral experiment or mindfulness/acceptance-based treatment versus as exposure therapy, given prior reports on the negative views of providers towards exposure therapy. Finally, we hypothesized that less training and experience with exposure therapy would magnify the likelihood that providers would not report likelihood to use exposure therapy.
Methods
Participants
Participants were 125 eating disorder treatment providers (therapists, psychologists, dietitians, and physicians) across the United States. See Table 1 for demographic, educational, and training characteristics.
Procedures
All methods were approved by the University of Louisville Institutional Review Board and all participants provided informed consent. Eating disorder treatment providers were recruited via email and direct message from online therapist listing sites, including psychologytoday.com and the Academy for Eating Disorders forum. Treatment providers were asked to fill out online questionnaires about their credentials, clinical training, clinical experience, and theoretical orientation. Then participants were provided with a brief description of an intervention for fear of eating pizza and asked how likely they were to use each type of therapy. Pizza was chosen as the feared food given high endorsement of pizza as a feared food in pilot data. All three vignettes described exposure therapy but differed in how the therapy was framed. The first vignette called exposure, the second behavioral experiment, and the third was referred to as mindfulness/acceptance-based intervention. All three vignettes are included in Table 2 (see for exact wording). The order of these vignettes were counterbalanced across six conditions (e.g. Condition 1: 1—exposure, 2—behavioral experiment, 3—mindfulness; Condition 2: 1—exposure, 2—mindfulness, 3—behavioral experiment; etc.) to account for possible ordering effects. The vignette order that providers received was determined by a random number generator. There were no other differences across the conditions other than the order of these questions. After the manipulation therapists were asked questions about their perceptions of exposure therapy. These questions were adapted from the Therapist Beliefs about Exposure Scale.
Measure
Therapist Beliefs About Exposure Scale (TBES; [27]). The TBES is a 21-item scale designed to measure therapist’s perceptions of exposure therapy as an acceptable treatment for anxiety. Respondents are asked to rate statements about exposure therapy on a scale from 0 (strongly disagree) to 5 (strongly agree). This measure has been shown to have good reliability and validity [27]. In this study, we used a 12-item short version of the TBES rated on a scale from 1 (strongly disagree) to 7 (strongly agree) and added additional questions about exposure therapy training and experience, as well as specific questions related to eating disorder treatment and training. We adapted this measure to fit with an eating disorder provider sample. The full list of questions asked is available via request from the first author, as well as are listed in Table 3.
Statistical analyses
We examined means and standard deviations of provider demographics and attitudes toward exposure therapy. We also used repeated measure ANOVAs to test if there was a significant effect of framing type, as well as to test interactions between framing type and demographic information.
Results
Provider demographics
Please see Table 1 that provides demographic information (e.g., degree, type of work setting, years in practice) on the providers in this study. We had a wide range of providers both in terms of degree type, work setting, theoretical orientations, as well as experiences with exposure therapy and types of treatments provided.
Provider attitudes toward exposure therapy
Please see Table 2 for wording of the vignette and Table 3 that lists each question asked about exposure therapy and providers’ responses. In general providers had a somewhat positive view of exposure therapy.
Framing manipulation
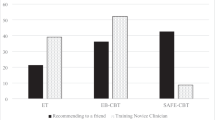
There was a significant multivariate effect for framing type in a repeated measures ANOVA Wilks Λ =0.92, F(2, 79) = 3.25, p = 0.044, η2p = 0.08 (medium effect). Bonferroni comparison tests indicated that there were significant differences between Condition 1 (behavioral experiments) and Condition 2 (exposure), such that providers preferred behavioral experiments (M = 5.49, SE = 0.21) over exposure (M = 5.02, SE = 0.22), p = 0.042. There were no significant differences between mindfulness and exposure or between behavioral experiments and mindfulness (ps > 0.353). There were no order effects. Please see Fig. 1 for a comparison between means.
Does framing vary for degree type, type of provider, years in practice, years in ED practice, experience with exposure (general and ED), and training in exposure therapy?
There was a significant interaction between degree type (PhD/PsyD vs MA) Wilks Λ = 0.81, F(2, 58) = 6.72, p = 0.002, η2p = 0.19 (large effect), such that PhD/PsyD were more likely to implement exposure over mindfulness interventions, whereas MA were more likely to implement mindfulness over exposure interventions. Please see Fig. 2 for a depiction. There was no significant interaction between provider type (psychologist, social worker, nurse/psychiatrist, dietitian) and framing (p = 0.647). There was no significant interaction between years in practice and framing (p = 0.985). There was no significant interaction between years in ED practice and framing (p = 0.802). There was no significant interaction between general experience with exposure therapy and framing, though it approached significance (p = 0.078). There was a significant interaction between prior experience with exposure therapy for eating disorders and framing Wilks Λ = 0.85, F(2, 75) = 6.66, p = 0.002, η2p = 0.18 (large effect), such that those with less experience with exposure were less likely to use exposure therapy framing, whereas training with exposure therapy increased the likelihood of using both behavioral experiments and exposure equally. Those with less exposure training were more likely to use mindfulness framing, whereas those with more exposure training reported willingness to use mindfulness slightly less than behavioral experiments or exposure. Please see Fig. 3 for a depiction. There was no significant interaction between receiving training in exposure therapy (general) and framing (p = 0.183).
Interaction between level of experience with exposure therapy and likelihood to use it in treatment. Participants indicated how likely they are to use each treatment on a scale from 1 (not likely at all) to 7 (very likely). Experience with exposure is measured using the item: Have you had any prior experience with delivering exposure therapy for eating disorders?
Discussion
We manipulated framing of the same intervention in terms of a behavioral experiment, exposure, or mindfulness/acceptance-based language. We found that despite describing the same intervention (facing fear foods, specifically pizza), providers were most likely to endorse wanting to use the intervention when it was framed as a behavioral experiment. This preference for language framed as a behavioral experiment did not vary by type of provider, years in practice, experience, or general training. We also found that there was a somewhat positive view of exposure therapy in general and exposure therapy for eating disorders specifically. Overall, these findings suggest that providers may be most likely to implement evidence-based exposure treatments if they are framed as behavioral experiments, possibly because this framing may seem less threatening. These findings also point to the fact that the way in which we frame our interventions matters for the likelihood of their acceptance and use in clinical practice.
Though overall we found that behavioral experiments were endorsed as the most likely usable intervention, there were also specific important variations in the endorsement of likelihood to use treatments. For example, we found that likelihood to use exposure versus mindfulness-based treatment varied based on degree type and specific experience with exposure for eating disorders. Specifically, providers with a masters degree were significantly more likely to use mindfulness (versus exposure), whereas providers with a doctorate were more likely to use exposure therapy (versus mindfulness). We also found that individuals with more experience with eating disorder specific exposure therapy (but not with general exposure therapy) were more likely to endorse likelihood to use treatment framed as exposure therapy. These findings are consistent with previous literature on amount of training and level of education being positively associated with the use of exposure therapy [13]. As evidence for the treatment of eating disorders with exposure is growing [6, 8, 9, 12], these data suggest that more education and specific eating disorder exposure experience is needed to enhance the likelihood that providers will use exposure therapy. This fact may be especially relevant for training within masters’ programs. As our workforce moves towards a greater emphasis on masters professionals as primary direct care providers [28, 29], it will be especially important to ensure inclusion of training and real-world practice with exposure therapy within these programs.
Against hypothesis, we found that providers had a more positive view of exposure therapy than we had expected. In general providers reported exposure therapy as an acceptable treatment for eating disorders. They also reported that clients are able to benefit from exposure therapy. Interestingly, though positive attitudes were reported, there were lower reports of having prior experience with exposure and providers reported less than a third of their time was spent using exposure therapy. These results are promising because they suggest, overall, eating disorder providers may have a more positive view of exposure therapy than has previously been expected. Literature in the anxiety disorder field shows that access to training and supervision, therapists’ belief in treatment efficacy, and self-efficacy in being able to administer exposure therapy are associated with higher utilization of exposure therapy [13]. These findings suggest that, especially if there is increased training and experiences available, providers may be likely to report willingness to implement exposure therapy for eating disorders.
Limitations
The current study is not without limitations. We had a relatively small sample of providers, though we did have a diverse range of occupations, degrees, and theoretical orientations. We also did not assess behaviorally if clinicians used these interventions, rather we relied on their self-report of how likely a provider would be to use the intervention. Future research should test if manipulating framing of interventions, possibly in a psychoeducational format, increases the actual practice of these therapies. For example, Waller et al. [15] found a brief 90 min training on exposure therapy increased the reported acceptability of exposure therapy. Additionally, our vignette focused on facing fear foods and it is possible that facing other feared stimuli might change our findings. Finally, we sought to use a previously implemented measure of therapist beliefs [27], however, our analyses our limited by reliance on self-report of therapist experiences and beliefs.
Conclusions
Overall, we found that framing the same intervention as a behavioral experiment increased the reported likelihood that providers would use this treatment for facing fear foods in the eating disorders. This finding did not differ based on degree type, type of provider, years in practice, experience, or training. However, we did find that more training was associated with a higher likelihood to use exposure vs acceptance-based treatments. These data show how language around behavioral interventions impacts the likelihood that providers will use these treatments, which has implications for how we train eating disorder providers in exposure-based treatments.
References
Kaczkurkin AN, Foa EB (2015) Cognitive-behavioral therapy for anxiety disorders: an update on the empirical evidence. Dialogues Clin Neurosci 17(3):337–346
Bulik CM, Sullivan PF, Carter FA, McIntosh VV, Joyce PR (1998) The role of exposure with response prevention in the cognitive-behavioral therapy for bulimia nervosa. Psychol Med 28(3):611–623. https://doi.org/10.1002/eat.10126
McIntosh VVW, Carter FA, Bulik CM, Frampton CMA, Joyce PR (2011) Five-year outcome of cognitive behavioral therapy and exposure with response prevention for bulimia nervosa. Psychol Med 41(5):1061–1071. https://doi.org/10.1017/S0033291710001583
Schyns G, van den Akker K, Roefs A, Hilberath R, Jansen A (2018) What works better? Food cue exposure aiming at the habituation of eating desires or food cue exposure aiming at the violation of overeating expectancies? Behav Res Ther 102:1–7. https://doi.org/10.1016/J.BRAT.2017.12.001
Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT (2011) Rationale for the application of exposure and response prevention to the treatment of anorexia nervosa. Int J Eat Disord 44(2):134–141. https://doi.org/10.1002/eat.20784
Levinson CA, Rapp J, Riley EN (2014) Addressing the fear of fat: extending imaginal exposure therapy for anxiety disorders to anorexia nervosa. Eat Weight Disord 19(4):521–524. https://doi.org/10.1007/s40519-014-0115-6
Glasofer DR, Albano AM, Simpson HB, Steinglass JE (2016) Overcoming fear of eating: a case study of a novel use of exposure and response prevention. Psychotherapy 53:223–231. https://doi.org/10.1037/pst0000048
Steinglass J, Albano AM, Simpson HB, Carpenter K, Schebendach J, Attia E (2012) Fear of food as a treatment target: exposure and response prevention for anorexia nervosa in an open series. Int J Eat Disord 45(4):615–621. https://doi.org/10.1002/eat.20936
Steinglass JE, Albano AM, Simpson HB, Wang Y, Zou J, Attia E, Walsh BT (2014) Confronting fear using exposure and response prevention for anorexia nervosa: a randomized controlled pilot study. Int J Eat Disord 47(2):174–180. https://doi.org/10.1002/eat.22214
Hildebrandt T, Loeb K, Troupe S, Delinsky S (2012) Adjunctive mirror exposure for eating disorders: a randomized controlled pilot study. Behav Res Ther 50(12):797–804. https://doi.org/10.1016/j.brat.2012.09.004
Trottier K, Carter JC, MacDonald DE, McFarlane T, Olmsted MP (2015) Adjunctive graded body image exposure for eating disorders: a randomized controlled initial trial in clinical practice. Int J Eat Disord 48(5):494–504. https://doi.org/10.1002/eat.22341
Reilly EE, Anderson LM, Gorrell S, Schaumberg K, Anderson DA (2017) Expanding exposure-based interventions for eating disorders. Int J Eat Disord 50(10):1137–1141. https://doi.org/10.1002/eat.22761
Harned MS, Dimeff LA, Woodcock EA, Contreras I (2013) Predicting adoption of exposure therapy in a randomized controlled dissemination trial. J Anxiety Disord 27(8):754–762. https://doi.org/10.1016/j.janxdis.2013.02.006
Olatunji BO, Deacon BJ, Abramowitz JS (2009) The Cruelest Cure? Ethical Issues in the Implementation of Exposure-Based Treatments. Cogn Behav Pract 16(2):172–180. https://doi.org/10.1016/J.CBPRA.2008.07.003
Waller G, D’Souza Walsh K, Wright C (2016) Impact of education on clinicians’ attitudes to exposure therapy for eating disorders. Behav Res Ther 76:76–80. https://doi.org/10.1016/j.brat.2015.11.014
Waller G, Stringer H, Meyer C (2012) What cognitive behavioral techniques do therapists report using when delivering cognitive behavioral therapy for the eating disorders? J Consult Clin Psychol 80(1):171–175. https://doi.org/10.1037/a0026559
Arch JJ, Craske MG (2008) Acceptance and commitment therapy and cognitive behavioral therapy for anxiety disorders: different treatments, similar mechanisms? Clin Psychol Sci Pract 15:263–279. https://doi.org/10.1111/j.1468-2850.2008.00137.x
Baer RA, Fischer S, Huss DB (2005) Mindfulness and acceptance in the treatment of disordered eating. J Ration Emot Cogn Behav Ther 23:281–300. https://doi.org/10.1007/s10942-005-0015-9
Hayes SC, Levin ME, Plumb-Vilardaga J, Villatte JL, Pistorello J (2013) Acceptance and commitment therapy and contextual behavioral science: examining the progress of a distinctive model of behavioral and cognitive therapy. Behav Ther 44(2):180–198. https://doi.org/10.1016/j.beth.2009.08.002
Collins LM, Murphy SA, Nair VN, Strecher VJ (2005) A strategy for optimizing and evaluating behavioral interventions. Ann Behav Med 30:65–73. https://doi.org/10.1207/s15324796abm3001_8
Mann T, Sherman D, Updegraff J (2004) Dispositional motivations and message framing: a test of the congruency hypothesis in college students. Health Psychol 23(3):330–334. https://doi.org/10.1037/0278-6133.23.3.330
Gallagher KM, Updegraff JA (2012) Health message framing effects on attitudes, intentions, and behavior: a meta-analytic review. Ann Behav Med 43:101–116. https://doi.org/10.1007/s12160-011-9308-7
Arch JJ, Twohig MP, Deacon BJ, Landy LN, Bluett EJ (2015) The credibility of exposure therapy: does the theoretical rationale matter? Behav Res Ther 72:81–92. https://doi.org/10.1016/j.brat.2015.05.008
Hayes SC (2004) Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behav Ther 35(4):639–665. https://doi.org/10.1016/S0005-7894(04)80013-3
Shapiro SL, Carlson LE, Astin JA, Freedman B (2006) Mechanisms of mindfulness. J Clin Psychol 62(3):373–386. https://doi.org/10.1002/jclp.20237
Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J (2006) Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther 44(1):1–25. https://doi.org/10.1016/J.BRAT.2005.06.006
Deacon BJ, Farrell NR, Kemp JJ, Dixon LJ, Sy JT, Zhang AR, McGrath PB (2013) Assessing therapist reservations about exposure therapy for anxiety disorders: the Therapist Beliefs about Exposure Scale. J Anxiety Disord 27:772–780. https://doi.org/10.1016/j.janxdis.2013.04.006
Kazdin AE, Fitzsimmons-Craft EE, Wilfley DE (2017) Addressing critical gaps in the treatment of eating disorders. Int J Eat Disord 50(3):170–189. https://doi.org/10.1002/eat.22670
Kazdin AE, Rabbitt SM (2013) Novel models for delivering mental health services and reducing the burdens of mental illness. Clin Psychol Sci 1(2):170–191. https://doi.org/10.1177/2167702612463566
Funding
We received no funding to complete this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to report.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All methods were approved by the University of Louisville Institutional Review Board and all participants provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Levinson, C.A., Christian, C. & Vanzhula, I.A. Manipulating the theoretical framing of exposure therapy for eating disorders impacts clinicians’ treatment preferences. Eat Weight Disord 25, 1205–1212 (2020). https://doi.org/10.1007/s40519-019-00751-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00751-3