Abstract
Purpose
Some features of eating disorders (EDs) are often present in childhood before the onset of the ED. We developed a novel questionnaire to retrospectively capture such childhood traits.
Methods
Focus groups were conducted at the University of California–San Diego, USA, and at the University of Turin, Italy. Three focus groups were conducted at each site, interviewing patients and parents to identify those traits that most commonly characterize childhood of patients with EDs. A preliminary version of the Premorbid Childhood Traits Questionnaire (PCT-Q) derived from these focus groups was then administered to 94 consecutive inpatients with an ED and to 286 healthy controls (HCs) at the Turin site. Also, 208 participants’ parents were enrolled as well; in fact, the PCT-Q was developed with both a proband and an informant version.
Results
A 37-item final version of the PCT-Q was generated. Reliability analyses suggested acceptability for harm avoidance (HA), social phobia, alexithymia, interoceptive awareness (IA), and food obsessions. Inter-rater reliability ranged from fair to moderate. ED sufferers scored significantly higher than HCs on HA, social phobia, alexithymia, IA, and food obsessions.
Conclusions
These findings support the possibility that premorbid traits contribute to a risk to develop an ED in some individuals.
Level of evidence
III: case–control analytic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The onset of eating disorders (EDs) typically occurs in adolescence; however, some common features of these illnesses are often already present before the ED onset [1, 2]. The available knowledge on risk factors has been broadened by a number of studies [3,4,5], and several lines of research showed that also certain personality traits are involved in EDs [6] and can represent vulnerability factors for EDs [7,8,9] as well as for other psychiatric illnesses [10].
It may be best accepted that perfectionism is a risk factor for EDs [9, 11] on the basis of evidence showing a relationship between this personality trait and both anorexia (AN) [3] and bulimia nervosa (BN) [12]. Still, childhood obsessive–compulsive personality traits (OCPTs) have been demonstrated to represent medium potency risk factors for the development of a full-blown ED [3, 4]. In addition, a premorbid diagnosis of obsessive–compulsive disorder has been found to negatively impact on AN prognosis [2]. Similarly, harm avoidance (HA) [13] has been proposed as potential risk factor for EDs [8]; it is characterized by cautiousness, anxiety, and inhibition, and represents a hallmark of the ED spectrum [7, 14]. Moreover, this temperament trait is heritable and detectable in non-affected family members [9].
Other traits which may predate the onset of an ED include interoceptive alterations [15, 16], and an imbalanced sensitivity to reward and punishment [17,18,19]. Poor interoceptive awareness (IA) is represented by an impaired recognition of both emotional states and hunger and satiety, and it is often a core psychopathological element of the EDs [20]. Literature on reward sensitivity in EDs is rapidly growing and studies reveal that those with an ED have high punishment sensitivity also after recovery [17, 18]. Therefore, reward alterations [21, 22] may be a trait already present in patients’ childhood, but, similarly to IA, no specific assessments are currently available about childhood alterations in patients with EDs.
Clinical experience suggests that some other characteristics predate the ED onset. For example, sleep problems are commonly found in both AN and BN [23], but as yet, there is no information available for patients’ sleep patterns in childhood. Furthermore, those with EDs in childhood tend to endeavor to do particularly well at school and report much commitment in hobbies and leisure activities. In spite of every-day clinical experience on the aforementioned features, no reliable instruments are to date available to evaluate them. As a result, a gap between clinical consensus and research needs emerges.
Longitudinal research in the field of EDs is challenging, also because these illnesses are relatively rare conditions [24]. Therefore, to maximize research feasibility and cost-effectiveness, premorbid traits can be assessed in a retrospective fashion for research purposes. In this light, Southgate and collaborators in 2008 [25] published a retrospective self-report assessment of OCPTs named Childhood Retrospective Perfectionism Questionnaire (CHIRP) to assess perfectionism, inflexibility, and drive for order and symmetry [25]. This line of research derived from Anderluh and collaborators’ work [3] that showed, using a semi-structured interviewed called EATATE Lifetime Diagnostic Interview, that OCPTs are stable traits with a high predictive value for development of EDs. According to the CHIRP results [25], those with an ED reported in childhood more behaviors indicating OCPTs than the control group, mirroring earlier results obtained with the EATATE interview [3]. To the best of our knowledge, no other validated self-report instruments are currently available to detect other premorbid alterations in the ED field.
Given the relevance of identifying premorbid conditions in both research and clinical settings, we aimed to develop a novel questionnaire that expanded the CHIRP questions [25]. Doing so, we aimed to broaden the self-report measurement of premorbid traits, avoiding the time-consuming and costly methodology of clinical interviews, to focus on other individual (i.e., parenting style, biological, and environmental not included) premorbid traits that might predate the onset of an ED potentially constituting a risk factor for the development of the ED itself. On one hand, we followed the need to deepen the investigation of premorbid traits, but, on the other hand, we had a focus on their correlations with other premorbid conditions and current personality and eating psychopathology features. Therefore, the overarching goal of this study was to verify the presence of premorbid risk factors, expanding current knowledge on this topic, to better inform treatments and to pave the way to screening assessments to improve prevention. Grounded on literature data, clinical experience, and patients and their families’ contributions, we expected to develop an instrument able to capture childhood traits.
Materials and methods
Procedure
Three focus groups were first conducted at the University of California–San Diego (UCSD), USA, and then replicated at the University of Turin, Italy, by two experienced clinicians and researchers. Procedures were consistent at both sites. Groups were scheduled once a week. Patients and patients’ parents were interviewed together in an open-ended fashion and with simultaneous transcriptions to identify those traits that most commonly characterize childhood of patients with EDs. Groups were started and conducted asking open-ended questions like “Please, describe what were your (or your daughter’s) characteristics at school when she was just a kid”; “Would you mind telling us how you (or your daughter) used to play with others when she was just a kid?”; “Did you (or your daughter) tried to achieve the best marks at school putting a lot of effort in school activities even when very young (e.g., 8 years old)?”. Simultaneous transcriptions were then read, analyzed, and pooled together to identify different groups of childhood traits. The following traits emerged: (1) HA; (2) reward sensitivity; (3) social phobic aspects; (4) alexithymia; (5) achievement drive; (6) IA; (7) food obsessions; (8) worry about the future; (9) sleep problems, i.e., insomnia, sleep terror-like symptoms. Perfectionism and inflexibility have been mentioned and considered, but are already assessed by the CHIRP questionnaire [25].
As a second step, a 62-item questionnaire asking respondents for a yes/no response was developed targeting all the aforementioned constructs. Following Southgate et al.’s [25] methodology, the questionnaire has been formulated in both a proband and an informant version to minimize patients’ recall bias. Items were added after checking them for face and content validity. The original questionnaire was devised in English and then translated into Italian. The first version was then polished following senior clinicians’ comments and tested for semantic comprehension on a pilot sample (n = 25) at both sites. According to respondents’ feedback, four items were discarded so a 58-item version of the questionnaire, the Premorbid Childhood Traits Questionnaire (PCT-Q), which was finally generated (fully available in the Tables S1–S4). As a final step, to validate the questionnaire, it was administered to a larger sample in addition to a battery of other assessments.
Participants
Focus groups
Concerning the focus groups, 35 and 33 patients were recruited at UCSD and at the University of Turin, respectively. For all participants, at least one parent was present during the groups as well (both parents were co-present during the 75% of sessions at UCSD and 95% at the University of Turin). At both sites, only females were included. At UCSD, the vast majority of participants were Caucasian (98%), while all participants were Caucasian (100%) at the University of Turin site. Participants’ mean age was 22.3 ± 3.4 years and 23.4 ± 2.8 years at UCSD and at the University of Turin, respectively, with no statistically significant differences between sites (data not shown).
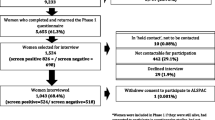
Validation study sample
The initial clinical sample was composed of 112 eligible candidates consecutively recruited at the University of Turin, Italy, between March 2015 and March 2017. However, 18 patients were excluded, because they refused to sign the informed consent or failed to complete the assessment battery, so 94 inpatients were finally involved in this study. Inclusion criteria were: (a) meeting DSM-5 [26] criteria for AN, both subtypes, and BN as assessed by an experienced psychiatrist using the Structured Clinical Interview for DSM-5 [27]; and (b) hospital admission for ED-related conditions. Fifty-two individuals (55.3%) were affected by AN restricting subtype (R-AN) while forty-two (44.7%) by bulimic variants (either AN binge-purging subtype [BN-AN; n = 26] or BN [n = 16]).
Healthy controls (HCs) were recruited at the same Institution through flyers and a total of 286 HC (including medical students, psychology students, residents, individuals who were interested in giving their moral contribution to research) were finally enrolled. HCs were excluded if using psychotropic medications or meeting criteria for a current or lifetime diagnosis of EDs or other psychiatric disorders, as assessed by an experienced psychiatrist.
Also 208 parents (patients: 32 mothers and 13 fathers; HCs: 148 mothers and 15 fathers) were enrolled in this study and completed the informant version of the PCT-Q independently of their participant family member.
All participants’ height and weight were measured by a trained nurse; these measures were then used to calculate their body mass index (BMI, expressed as kg/m2).
This study was approved by the Ethics Committee of the Department of Neuroscience of the University of Turin, Italy. Written informed consent was obtained by all participants. The focus groups conducted at the University of California, San Diego were part of a clinical program, so did not require IRB approval.
Materials
Several assessments have been consistently used in the field of EDs’ garnering evidence on general and eating psychopathology of patients with EDs. Therefore, to compare the preliminary findings of the PCT-Q with validated and widely used assessments of the ED field, all participants were asked to complete the following two batteries of assessments.
-
1.
Childhood traits: participants assessed childhood traits (i.e., thinking back to the time when they were 10–12 years old) with the following measures:
-
(a)
Premorbid Childhood Traits Questionnaire (PCT-Q, see Tables S1–S4): a self-report questionnaire investigating childhood HA, reward sensitivity, social phobic aspects, alexithymia, achievement drive, IA, food obsessions, worry about the future, and sleep problems. Self-report and informant versions of the questionnaire were administered to study participants with binary responses. Kuder–Richardson’s coefficients of the scales ranged from .06 (reward sensitivity–then discarded from the final version of the PCT-Q) to .76 (alexithymia). See Table 1 for reliability details.
-
(b)
Childhood Retrospective Perfectionism Questionnaire (CHIRP) [25]: the CHIRP is a self-report questionnaire with sound psychometric properties [25] which measures the presence of OCPTs in childhood. Responses are binary (i.e., yes/no) and three subscales (perfectionism, inflexibility, and drive for order and symmetry) are provided. Examples of questions include the following: “At school, did you put more effort into your schoolwork because of attention to detail or perfectionism, than your friends/classmates?” (proband version); “At school, did your child put more effort into their schoolwork because of their attention to detail or perfectionism, than their friends/classmates?” (informant version).
-
(a)
Current symptoms: participants were asked to rate current behaviors and thoughts with the following:
-
(a)
Temperament and Character Inventory (TCI) [13].
The TCI is a 240-item self-administered questionnaire divided into seven dimensions. Four of these dimensions assess temperament: novelty seeking (NS), harm avoidance (HA), reward dependence (RD), and persistence (P). The other three dimensions assess character: self-directedness (SD), cooperativeness (C), and self-transcendence (ST). Responses are binary (i.e., true/false). The TCI showed good properties as regards both internal consistency and test–retest reliability [13]. Examples of questions include: “I often feel tense and worried in unfamiliar situations, even when others feel there is little to worry about”; “I have less energy and get tired more quickly than most people”.
-
(b)
Frost Multidimensional Perfectionism Scale (FMPS) [28].
The FMPS is a 35-item self-report scale with solid psychometric properties [28] evaluating perfectionism as a multidimensional concept. Six subscales are assessed on a five-point Likert scale: Concern over Mistakes, Personal Standards, Parental Expectations, Parental Criticism, Doubts about actions, and Organization. Higher scores reflect a greater level of perfectionism. Examples of questions include: “My parents set very high standards for me”; “I should be upset if I make a mistake”.
-
(c)
Eating Disorders Inventory-2 (EDI-2) [29].
The EDI-2 is a self-report inventory that measures disordered eating attitudes, behaviors, and personality traits common to individuals affected by an eating disorder. Eleven subscales assess symptoms and psychological correlates of the eating disorders; answers are rated on a Likert scale with high scores reflecting pathology. It is characterized by high internal consistency, indicated by Cronbach’s alpha values between .82 and .93 [30]. Examples of questions include: “I feel bloated after eating a small meal”; “When I am upset, I worry that I will start eating”.
Statistical analysis
To evaluate internal consistency, the Kuder–Richardson’s coefficient and relative 95% confidence intervals have been calculated for all the subscales of the PCT-Q: harm avoidance, reward sensitivity, social phobic aspects, alexithymia, achievement drive, interoceptive awareness, food obsessions, worry about the future, and sleep problems. With respect to Kuder–Richardson’s coefficient, a level of .6 has been deemed acceptable also given the exploratory design of this study [31,32,33].
Inter-rater reliability has been evaluated using Cohen’s k method, considering 50th percentile of informants’ responses as the cut-off for each subscale to determine presence/absence of each trait. Results have presented with relative 95% confidence intervals (95% CI). According to Landis and Koch [34], values < 0 indicate no agreement, 0–.20 slight agreement, .21–.40 fair agreement, .41–.60 moderate agreement, .61–.80 substantial agreement, and .81–1 almost perfect agreement.
Student’s t test has been used to evaluate the differences between groups for continuous variables.
Cohen’s d effect sizes were calculated as well; differences are defined as negligible (≥ − .15 and < .15), small (≥ .15 and < .40), medium (≥ .40 and < .75), large (≥ .75 and < 1.10), very large (≥ 1.10 and < 1.45), and huge (> 1.45).
The Statistical Package for Social Sciences 24.0 (SPSS, SPSS Inc., Chicago, IL, USA) was used for all analyses. To not overestimate the beta error, the alpha levels (two-tailed alpha = .05) were not adjusted for multiple comparisons.
Results
Current clinical characteristics of the sample
Participants were all Caucasian and most participants were women (HCs: 90.2% and ED patients: 92.6%, p = .056). Patients and HCs had a mean age of 24.8 ± 8.5 years and 23.7 ± 2.5 years, respectively (t = − 1.88, p = .061). Participants’ BMI significantly differed between patients and HCs (ED patients’ BMI: 15.9 ± 3.7, HCs’ BMI: 21.2 ± 2; t = 17.33, p < .001). Patients’ duration of illness was 7.1 ± 7.34 years.
Concerning current traits, patients with ED and HCs differed significantly on all TCI dimensions with the exception of persistence and self-transcendence (data not shown). Concerning perfectionism, ED individuals and HCs differed significantly on all scales but parental expectations; eating psychopathology resulted significantly different on all dimensions (data not shown).
Reliability and inter-rater reliability of the PCT-Q
As regards the PCT-Q, Kuder–Richardson’s coefficients were considered to be acceptable for HA, social phobia, alexithymia, IA, and food obsessions (see Table 1). Therefore, reward sensitivity, achievement drive, worry about the future, and sleep problems were discarded from the final version of the PCT-Q. All scales reported a reliability measure, four scales had reliability < .60, two between .60 and .70, three between .70 and .80, and none over .80; so, the median stability was 2.
With respect to inter-rater reliability, 208 informants completed the PCT-Q as well, informant version (see Tables S2 and S4). They were all parents with participants’ mothers (n = 180) and fathers (n = 28) providing a complete assessment. With more detail, 45 were patients’ parents and 163 HCs’ parents. Cohen’s k scores ranged from fair to moderate (see Table 1).
Premorbid clinical characteristics of the sample
Concerning premorbid traits as measured by the PCT-Q, ED sufferers scored significantly higher than HCs on HA, social phobia, alexithymia, IA, and food obsessions (Table 2).
As shown in Table 3, HCs and patients with EDs significantly differed on all CHIRP scores.
Correlations of the PCT-Q and eating and general psychopathology
The PCT-Q showed significant correlations with all the CHIRP scales (see Table 4), and with the vast majority of the TCI (see Table 4), EDI-2 (the three “core” subscales have been considered; see Table 5), and FROST sub-dimensions (see Table 5).
Discussion
A growing body of evidence showed that certain personality and anxiety traits represent predisposing factors that precede the onset of an ED and usually appear already in childhood [3, 35]. Nonetheless, such aspects are understudied also because of the lack of instruments able to systematically investigate them. To bridge this gap in literature, we developed a novel self-report questionnaire, the Premorbid Childhood Traits Questionnaire (PCT-Q), (fully available in the Tables S1–S4) investigating premorbid traits in patients with EDs.
The 37-item final version of the PCT-Q was found to capture premorbid harm avoidance, social phobia, alexithymia, interoceptive awareness, and food obsessions. Importantly, inter-rater reliability was found to be good, corroborating patients’ recall of their childhood symptoms. Moreover, the PCT-Q was highly correlated with measures of premorbid and current dimensions. Also in this light, the psychometric properties of this novel questionnaire appeared to be satisfactory. It is noteworthy that Cohen’s k values indicate a fair agreement between probands and informants’ versions. This is an expected finding, since some items of the PCT-Q refer to internal states and feelings that are difficult to fully identify from an observer standpoint. Furthermore, part of the sample could be confounded by alexithymic individuals who tend to poorly identify and express emotions [36] in turn further hampering statistical agreement.
Our findings are consistent with those provided by the CHIRP [25] not only because both measures found patients as more prone than HCs to report the presence of ED-related traits in patients’ early childhood, but also because inter-rater reliability scores were similar and the two questionnaires were found as highly correlated to each other. In fact, the inter-rater reliability values ranged from .28 to .43 and from .22 to .41 for CHIRP [25] and PCT-Q, respectively.
Some interesting traits have been identified by the PCT-Q. HA has strong neurobiological underpinnings [37, 38], and it has been clinically observed and reported to be heightened after recovery from EDs thus providing indirect support to its possible premorbid alteration [35]. The questionnaire appears to effectively capture premorbid HA and preliminary data showed that this trait effectively differs between ED individuals and HCs. With respect to anxiety elements in EDs, the questionnaire also identified childhood social phobia. Anxiety disorders are highly comorbid with EDs [39] and tend to predate the onset of EDs in a substantial proportion of cases [40, 41]. Social phobia is one of the most common anxiety disorders diagnosed before the onset of the ED [35], and several lines of research suggest anxiety to persist after recovery [35, 42], so our data seem to be in line with the current literature.
IA is known to be altered in those affected by an ED [20, 37]. Although such alteration is known to be a relevant factor [37] it remains unclear as to whether it could occur premorbidly or not. The questionnaire was found to capture this construct and pilot data showed interesting childhood differences between those with an ED and HCs. In addition, in the ongoing debate on shared risk factors between EDs and other major psychiatric diagnoses (e.g., depressive disorders) [43], IA might have a role as a specific childhood alteration of those who will develop eating disturbances. However, only longitudinal data and larger samples could confirm this research hypothesis.
Broadly speaking, disturbances of IA may facilitate the lack of integration of basic bodily signals and alexithymia, namely the difficulty at recognizing and labeling emotions, hallmark of full-blown EDs [20, 37]. From this standpoint, it is of interest that the PCT-Q captured alexithymia as present already in childhood. Difficulties in recognizing and managing emotions are common in EDs [36]; however, it is an every-day clinical experience to see that these elements often characterize patients with ED even before the onset of the illness. Notwithstanding, data on childhood alexithymia are lacking, so this questionnaire could be of help in gathering data in this regard.
The questionnaire identified also childhood food obsessions, i.e., persistent and intrusive thoughts about food with relevant treatment implications in case of AN [44]. Obsessive compulsive disorder in childhood has been found to negatively impact on AN [2]; however, the relationship between specific food obsessions and ED onset is currently understudied. Only longitudinal study conducted on large samples could answer this research question; however, the PCT-Q was found to be a reliable measure of such aspects thus potentially informing future research on this issue.
Reward sensitivity, achievement drive, worry about the future, and sleep problems were each below the reliability threshold set at 0.6 and hence discarded from the final version of the PCT-Q. Also, they resulted as not correlated with other premorbid and/or current traits as much as other PCT-Q dimensions did. It is possible that these items were not worded accurately enough or that the construct that emerged from the focus groups did not generalizable to all affected individuals. In contrast to our a priori hypothesis, the questionnaire failed to effectively capture reward sensitivity. Perhaps, reward sensitivity, as well as achievement drive (i.e., the attempt to excel in all activities)—although the latter is a more debated aspect [45]—could benefit from a more homogeneous sample; in fact, restricting and binge-purging variants may lead to mixed results given their well-known differences with respect to persistence, reward, and impulse regulation [17, 21, 22]. Concerning worry about the future, potentially related to the fear of uncertainty found in both AN and BN [36, 46], it resulted as weakly distinguishing HC and patients; in fact, the former group described greater anxiety than patients during childhood. On one hand, the items of this scale may benefit from being reworded, but, on the other hand, this dimension could be too broad to be fully predictive by asking relatively few questions. Finally, sleep problems were not deeply investigated (i.e., four items) and could be shared by a variety of mental and neurological disorders [47, 48], although their predictive value has not been investigated. Also, some features (e.g., sleep terror) could be frequently found also in healthy individuals without any relevant repercussions on their mental health; in fact, HCs scored high on this scale as well.
In closing, the PCT-Q was found to identify premorbid traits of HA, social phobia, alexithymia, IA, and food obsessions. This questionnaire could entail several advantages in both research and clinical settings. In fact, the self-report format makes it quick and easy to administer, and premorbid data may be used to not only individualize treatments but also plan prevention strategies. However, some limitations should be acknowledged: reliability levels were not high as well as the informant rate, test–retest data were lacking, the sample size was not very large, and the back-translation from English to Italian could have slightly modified some items of the questionnaire. Furthermore, recall bias could not be ruled out given the retrospective design of this study. That said, future research may want to deepen the psychometrics of the PCT-Q (e.g., exploratory factor analysis) and check the prognostic value of these data also comparing different mental illnesses; finally, it would be of interest to compare adolescent and adult samples to minimize completers’ memory bias and verify these findings.
Data availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Klump KL, Strober M, Bulik CM, Thornton L, Johnson C, Devlin B et al (2004) Personality characteristics of women before and after recovery from an eating disorder. Psychol Med 34(8):1407–1418
Carrot B, Radon L, Hubert T, Vibert S, Duclos J, Curt F, Godart N (2017) Are lifetime affective disorders predictive of long-term outcome in severe adolescent anorexia nervosa? Eur Child Adolesc Psychiatry 26:969–978. https://doi.org/10.1007/s00787-017-0963-5
Anderluh MB, Tchanturia K, Rabe-Hesketh S, Treasure J (2003) Childhood obsessive-compulsive personality traits in adult women with eating disorders: defining a broader eating disorder phenotype. Am J Psychiatry 160(2):242–247. https://doi.org/10.1176/appi.ajp.160.2.242
Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS (2004) Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull 130(1):19–65. https://doi.org/10.1037/0033-2909.130.1.19
Himmerich H, Bentley J, Kan C, Treasure J (2019) Genetic risk factors for eating disorders: an update and insights into pathophysiology. Ther Adv Psychopharmacol 9:2045125318814734. https://doi.org/10.1177/2045125318814734
Marzola E, Fassino S, Amianto F, Abbate-Daga G (2017) Affective temperaments in anorexia nervosa: the relevance of depressive and anxious traits. J Affect Disord 218:23–29. https://doi.org/10.1016/j.jad.2017.04.054
Fassino S, Abbate-Daga G, Amianto F, Leombruni P, Boggio S, Rovera GG (2002) Temperament and character profile of eating disorders: a controlled study with the Temperament and Character Inventory. Int J Eat Disord 32(4):412–425. https://doi.org/10.1002/eat.10099
Lilenfeld LR (2011) Personality and temperament. Curr Top Behav Neurosci 6:3–16. https://doi.org/10.1007/7854_2010_86
Thornton LM, Trace SE, Brownley KA, Ålgars M, Mazzeo SE, Bergin JE, Maxwell M, Lichtenstein P, Pedersen NL, Bulik CM (2017) A comparison of personality, life events, comorbidity, and health in monozygotic twins discordant for anorexia nervosa. Twin Res Hum Genet 20:310–318. https://doi.org/10.1017/thg.2017.27
Stanfield AC, McKechanie AG, Lawrie SM, Johnstone EC (2019) Owens D.G.C.: predictors of psychotic symptoms among young people with special educational needs. Br J Psychiatry 5:1–6. https://doi.org/10.1192/bjp.2018.296
Culbert KM, Racine SE, Klump KL (2015) Research review: what we have learned about the causes of eating disorders—a synthesis of sociocultural, psychological, and biological research. J Child Psychol Psychiatry 56(11):1141–1164. https://doi.org/10.1111/jcpp.12441
Boone L, Soenens B, Luyten P (2014) When or why does perfectionism translate into eating disorder pathology? A longitudinal examination of the moderating and mediating role of body dissatisfaction. J Abnorm Psychol 123(2):412–418. https://doi.org/10.1037/a0036254
Cloninger CR, Svrakic DM, Przybeck TR (1993) A psychobiological model of temperament and character. Arch Gen Psychiatry 50(12):975–990
Atiye M, Miettunen J, Raevuori-Helkamaa A (2015) A meta-analysis of temperament in eating disorders. Eur Eat Disord Rev 23:89–99. https://doi.org/10.1002/erv.2342
Lilenfeld L, Wonderlich S, Riso L, Crosby R, Mitchell J (2006) Eating disorders and personality: a methodological and empirical review. Clin Psychol Rev 26(3):299–320
Duffy ME, Rogers ML, Joiner TE, Bergen AW, Berrettini W, Bulik CM, Brandt H, Crawford S, Crow S, Fichter M, Halmi K, Kaplan AS, Klump KL, Lilenfeld L, Magistretti PJ, Mitchell J, Schork NJ, Strober M, Thornton LM, Treasure J, Woodside B, Kaye WH, Keel PK (2019) An investigation of indirect effects of personality features on anorexia nervosa severity through interoceptive dysfunction in individuals with lifetime anorexia nervosa diagnoses. Int J Eat Disord 52:200–205. https://doi.org/10.1002/eat.23008
Harrison A, O’Brien N, Lopez C, Treasure J (2010) Sensitivity to reward and punishment in eating disorders. Psychiatry Res 177(1–2):1–11. https://doi.org/10.1016/j.psychres.2009.06.010
Jappe LM, Frank GK, Shott ME, Rollin MD, Pryor T, Hagman JO et al (2011) Heightened sensitivity to reward and punishment in anorexia nervosa. Int J Eat Disord 44(4):317–324. https://doi.org/10.1002/eat.20815
Bischoff-Grethe A, McCurdy D, Grenesko-Stevens E, Irvine LE, Wagner A, Yau WY, Fennema-Notestine C, Wierenga CE, Fudge JL, Delgado MR, Kaye WH (2013) Altered brain response to reward and punishment in adolescents with Anorexia nervosa. Psychiatry Res 214:331–340. https://doi.org/10.1016/j.pscychresns.2013.07.004
Fassino S, Pierò A, Gramaglia C, Abbate-Daga G (2004) Clinical, psychopathological and personality correlates of interoceptive awareness in anorexia nervosa, bulimia nervosa and obesity. Psychopathology 37(4):168–174. https://doi.org/10.1159/000079420
Wierenga CE, Ely A, Bischoff-Grethe A, Bailer UF, Simmons AN, Kaye WH (2014) Are extremes of consumption in eating disorders related to an altered balance between reward and inhibition? Front Behav Neurosci 8:410. https://doi.org/10.3389/fnbeh.2014.00410
Bailer UF, Price JC, Meltzer CC, Wagner A, Mathis CA, Gamst A et al (2017) Dopaminergic activity and altered reward modulation in anorexia nervosa-insight from multimodal imaging. Int J Eat Disord 50(5):593–596. https://doi.org/10.1002/eat.22638
Asaad Abdou T, Esawy HI, Abdel Razek Mohamed G, Hussein Ahmed H, Elhabiby MM, Khalil SA, El-Hawary YA (2018) Sleep profile in anorexia and bulimia nervosa female patients. Sleep Med 48:113–116. https://doi.org/10.1016/j.sleep.2018.03.032
Smink FR, van Hoeken D, Hoek HW (2012) Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 14(4):406–414. https://doi.org/10.1007/s11920-012-0282-y
Southgate L, Tchanturia K, Collier D, Treasure J (2008) The development of the childhood retrospective perfectionism questionnaire (CHIRP) in an eating disorder sample. Eur Eat Disord Rev 16(6):451–462. https://doi.org/10.1002/erv.870
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5, 5th edn. American Psychiatric Association, Arlington
First MB, Williams JB, Karg RS, Spitzer RL (2015) SCID-5-CV: structured clinical interview for DSM-5 disorders; clinician version. American Psychiatric Association Publishing, Arlington
Frost RO, Marten P, Lahart C, Rosenblate R (1990) The dimensions of perfectionism. Cogn Ther Res 14:449
Garner DM (1991) Eating Disorder Inventory-2. Professional manual. Psychological Assessment Resources Inc, Odessa
Thiel A, Paul T (2006) Test–retest reliability of the Eating Disorder Inventory 2. J Psychosom Res 61(4):567–569
Nunnally JC, Bernstein IH (1994) Psychometric theory, 3rd edn. Mc Graw Hill, New York
Cho E, Kim S (2015) Cronbach’s coefficient alpha: well known but poorly understood. Organ Res Methods 8(2):207–230
Cortina JM (1993) What is coefficient alpha? An examination of theory and applications. J Appl Psychol 78(1):98–104
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K (2004) Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry 161(12):2215–2221. https://doi.org/10.1176/appi.ajp.161.12.2215
Abbate-Daga G, Quaranta M, Marzola E, Amianto F, Fassino S (2015) The relationship between alexithymia and intolerance of uncertainty in anorexia nervosa. Psychopathology 48(3):202–208. https://doi.org/10.1159/000381587
Kaye WH, Fudge JL, Paulus M (2009) New insights into symptoms and neurocircuit function of anorexia nervosa. Nat Rev Neurosci 10(8):573–584. https://doi.org/10.1038/nrn2682
Bailer UF, Frank GK, Price JC, Meltzer CC, Becker C, Mathis CA et al (2013) Interaction between serotonin transporter and dopamine D2/D3 receptor radioligand measures is associated with harm avoidant symptoms in anorexia and bulimia nervosa. Psychiatry Res 211(2):160–168. https://doi.org/10.1016/j.pscychresns.2012.06.010
Swinbourne J, Hunt C, Abbott M, Russell J, St Clare T, Touyz S (2012) The comorbidity between eating disorders and anxiety disorders: prevalence in an eating disorder sample and anxiety disorder sample. Aust N Z J Psychiatry 46(2):118–131. https://doi.org/10.1177/0004867411432071
Deep AL, Nagy LM, Weltzin TE, Rao R, Kaye WH (1995) Premorbid onset of psychopathology in long-term recovered anorexia nervosa. Int J Eat Disord 17(3):291–297
Salbach-Andrae H, Lenz K, Simmendinger N, Klinkowski N, Lehmkuhl U, Pfeiffer E (2008) Psychiatric comorbidities among female adolescents with anorexia nervosa. Child Psychiatry Hum Dev 39(3):261–272. https://doi.org/10.1007/s10578-007-0086-1
Pollice C, Kaye WH, Greeno CG, Weltzin TE (1997) Relationship of depression, anxiety, and obsessionality to state of illness in anorexia nervosa. Int J Eat Disord 21(4):367–376
Wade TD, Bulik CM, Neale M, Kendler KS (2000) Anorexia nervosa and major depression: shared genetic and environmental risk factors. Am J Psychiatry 157(3):469–471. https://doi.org/10.1176/appi.ajp.157.3.469
Steinglass J, Albano AM, Simpson HB, Carpenter K, Schebendach J, Attia E (2012) Fear of food as a treatment target: exposure and response prevention for anorexia nervosa in an open series. Int J Eat Disord 45(4):615–621. https://doi.org/10.1002/eat.20936
Waller G, Shaw T, Meyer C, Haslam M, Lawson R, Serpell L (2012) Persistence, perseveration and perfectionism in the eating disorders. Behav Cogn Psychother 40(4):462–473. https://doi.org/10.1017/S135246581200015X
Frank GK, Roblek T, Shott ME, Jappe LM, Rollin MD, Hagman JO et al (2012) Heightened fear of uncertainty in anorexia and bulimia nervosa. Int J Eat Disord 45(2):227–232. https://doi.org/10.1002/eat.20929
Hasler BP, Kirisci L, Clark DB (2016) Restless sleep and variable sleep timing during late childhood accelerate the onset of alcohol and other drug involvement. J Stud Alcohol Drugs 77(4):649–655
Jacoby A, Snape D, Lane S, Baker GA (2015) Self-reported anxiety and sleep problems in people with epilepsy and their association with quality of life. Epilepsy Behav 43:149–158. https://doi.org/10.1016/j.yebeh.2014.09.071
Funding
This is unfunded research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of topical collection on Personality and eating and weight disorders.
The study took place at two sites: at the University of California San Diego, Eating Disorders Research and Treatment Program, Chancellor Park, 4510 Executive Drive, Suite 315, San Diego CA 92121; and at the Eating Disorders Centre of the University of Turin, via Cherasco 11, 10126, Turin, Italy.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Marzola, E., Fassino, S., Migliaretti, G. et al. Development and validation of the Premorbid Childhood Traits Questionnaire (PCT-Q) in eating disorders. Eat Weight Disord 24, 815–823 (2019). https://doi.org/10.1007/s40519-019-00748-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00748-y