Abstract
Objective
Nutrition restoration in inpatients with anorexia nervosa (AN) is a core element in treatment, enabling recovery of cognitive functions essential for psychological care. This study aims to identify factors associated with inpatient weight gain.
Methods
Medical records from 107 inpatients aged 13–55 years with AN, hospitalized for more than 7 days at a specialized unit, were examined in a retrospective study. Weight evolution graphs were created for each patient and graded independently as optimal, moderate, and inadequate weight gain after 2 weeks and increasing, flat or decreasing weight in the first 2 weeks by expert clinicians. Driven by explicit hypotheses, bivariable analyses were carried out to detect relevant factors associated with weight gain during and after the first 2 weeks of admission.
Results
Initial weight gain in the first 2 weeks of hospitalization and the introduction of a protocol harmonizing treatment procedures around rapid refeeding were strong factors associated with optimal weight gain after 2 weeks of hospitalization, whereas prior hospitalization in a psychiatric unit, diagnosis with binge-eating/purging subtype and age over 18 years were significantly associated with inadequate weight gain (p < 0.001–0.05).
Conclusion
To promote weight gain during hospitalization, clinicians should consider the following therapeutic measures: rapid refeeding strategies, renutrition protocols, and controlling purging behaviors.
Level of evidence
Level III, retrospective cohort study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anorexia nervosa (AN) is a serious illness leading to major risk of malnutrition with devastating health consequences. In Switzerland, the lifetime prevalence for AN is 1.2 and 0.2% for women and men, respectively [1]. AN is characterised by aberrant feeding behaviors, body image distortions and an extreme pursuit of thinness and emaciation. Various treatment strategies have been developed, and the determination of treatment setting depends on patient safety, preferences and access to health care system [2].
Hospitalization is required when weight loss seriously threatens the health and life of the person. Recent NICE [3] and The Royal Australian and New Zealand College of Psychiatrists Guidelines [4] have formulated criteria to help assess acute situations where hospitalization becomes necessary. A recent systematic review [5] highlighted the lack of consensus on treatment protocols regarding refeeding practices. Also, there is no clear evidence on the best treatment setting (inpatient, outpatient vs partial hospitalization care) for weight gain in anorexia nervosa patients [2].
Restoring optimal weight is the key to avoiding severe physical complications and to improving cognitive function which then in turn make psychological interventions more useful and effective [6, 17]. Studies have shown that rapid initial refeeding increases weight gain [7]. Moreover, approaching or achieving normal weight during treatment is a predictor of a better outcome compared to lack of weight gain [8]. Low weight at time of discharge is associated with higher risk of readmission [9,10,11]. Therefore, weight gain and medical stabilisation constitute the primary treatment goals for patients with AN [12]. Weight gain trajectories may vary among inpatients [13] and need to be taken into consideration to assess patients’ progress or prognosis [14]. The study of weight curve dynamics is critical to better understand the process of weight restoration in anorexia nervosa inpatients [13, 14].
Given the variability of weight trajectories and the importance of weight gain during hospitalization of patients with AN, it is crucial to know the factors promoting or hindering weight gain. Most studies actually describe predictive factors for weight gain in terms of long-term effects or predictors of drop-out from inpatient treatment. It appears that late age at onset [7], long duration of illness [7, 15], low BMI at admission [16, 17], long initial hospital stay [17], previous admissions in psychiatric hospitals, vomiting and purgative behaviors [16, 18], as well as psychiatric co-morbidities [16] all constitute negative prognostic factors; whereas early weight gain in treatment is a positive prognostic factor for long-term response [19, 20]. Predictive factors of drop-out from inpatient treatment include binge-eating/purging behaviors [21,22,23,24,25,26,27], low BMI at admission [23, 28], age at admission [28, 29], impulsive behaviors [26, 30], personality disorders [31], severity of the disease [22, 29] and low educational status [29, 30].
The current study aims to supplement current knowledge by focusing on factors associated with actual weight gain during hospitalization. Based on prior findings and clinical experience, we formulated various hypotheses regarding factors associated with inpatient weight evolution curves. We hypothesized that inadequate weight gain would be associated with older age, psychiatric co-morbidities, nutrition stage, eating disorder (ED) phenotype, chronicity of the disease and digestive disorders. Medical follow-up and intensive refeeding strategies were hypothesized to be positively associated with weight gain.
Methods
The present research is a retrospective study based on the medical records of patients hospitalized before and after the introduction of a refeeding protocol in an inpatient ED unit in Lausanne, Switzerland. The impact of the protocol has been written up elsewhere [Gjoertz et al., submitted], and this paper focuses on examining factors associated with weight gain. The entire study was reviewed and approved by the Vaud Cantonal Ethics Committee.
Refeeding protocol
A refeeding protocol (Online Resource 1) was introduced at the Lausanne University Hospital in June 2014. Criteria for hospitalization include low BMI at admission, increased and rapid weight loss, minimal food intake for several days, electrolytes perturbation and alcohol/drug abuse which are consistent with NICE recommendations. Upon hospitalization, the aim of the protocol is first and foremost adequate renutrition to restore optimal weight. Nevertheless, it also enables detection and prevention of early refeeding-related complications as well as encouraging oral feeding whilst clearly establishing indications about when to introduce enteral nutrition via nasogastric tube.
The protocol details a stepwise approach. In the first week, the patients receive 50% of individual basic caloric needs at day 1, 75% at day 3 and 100% at day 6. During the second week, the basic caloric needs are reached, and 300 kcal, 600 kcal and 1000 kcal are added, respectively, every 3 days until the third week, when an extra 1000 kcal are added per day on top of the basic needs. If the goals are not reached for more than 2 days in a row or if the speed of weight gain is insufficient, enteral nutrition is introduced.
Calories are increased independently of the weight curve during the first 2 weeks of admission as this weight curve is difficult to interpret due to body water changes in the context of purging or somatic complications (e.g., pseudo-Bartter, impaired osmoregulation) that tend to produce a yoyo-like curve. In addition to the refeeding protocol, psychotherapeutic, physiotherapeutic and dietician support are also provided by the multidisciplinary team depending on patient characteristics and disease severity.
Participants
Patients admitted between October 1, 2013 and March 31, 2014, as well as from June 1, 2014, to June 1, 2016, were eligible for the study. Patients admitted during the months of April and May 2014 were intentionally left out to create a buffer period before implementation of the protocol in June 2014.
We obtained a list of patients admitted during the study period from the hospital (n = 125) and selected patients that met the following inclusion criteria: diagnosis of AN (restrictive, purgative or atypical) according to ICD-10 and 13 years of age and older. Eighteen subjects were excluded for the following reasons: diagnosis of bulimia (n = 10), hospitalization shorter than 7 days (n = 3) and a “respite” or “observation” type hospitalization (n = 5).
Data collection
For each patient, we attributed a study ID number. Data were extracted from paper and electronic medical records at the unit which were then entered into an Excel spreadsheet. Due to the lack of centralized health care data in Switzerland, we had access only to data pertaining to a patient’s hospitalization in this particular institution. Each patient was followed for the duration of their hospitalization at the unit. At discharge, the kind of follow-up care prescribed by clinicians was noted in the medical records; however, since the patients would be transferred to providers elsewhere, we did not have access to any extramural records for this study.
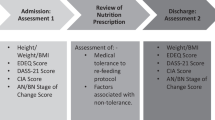
We documented socio-demographic characteristics, relevant medical history pertaining to ED according to data based on the first medical interview with the patient and information from medical records (duration of illness, family history, prior follow-up and admissions, psychiatric co-morbidities assessed at psychiatric examination), clinical symptoms at admission and data involving hospital course (length of admission, weight and BMI variation, electrolyte complications, nasogastric tube, discharge against medical advice) as well as type of follow-up prescribed after discharge and the number of rehospitalizations. These variables were chosen according to our review of the literature and the expertise of clinicians working at the ED unit.
The main dependent variable in this paper is weight gain. To define this clinical outcome, weight evolution graphs were created for each patient using all available data points from admission to discharge (Fig. 1), and two expert clinicians (AEA and FL) assessed each patient’s graph independently for two time periods. Two weeks after admission—i.e., after day 14 (D14)—weight gain below 500 g per week was considered inadequate, between 500 and 750 g per week as moderate, and over 750 g per week as optimal. These thresholds were defined based on guidelines in the literature [12, 32,33,34,35,36] as well as the clinical experience of several co-authors. Due to body water changes creating erratic ups and downs in the first 2 weeks, these initial data points are usually excluded from assessments. However, we wanted to explore whether it would be possible to characterize weight evolution simply during this time, and whether this initial phase has any impact on weight gain during the main period. For the first 2 weeks of hospitalization from day 1 (D1) of admission through D14, the experts noted whether there was weight gain, no weight gain/loss, or weight loss (including a U curve of initial weight loss followed by weight gain).
Certain variables were excluded both prior to and during statistical analysis. First, we excluded height and vital parameters because they were taken only at admission and not at discharge, so there was no way of detailing their evolution during hospitalization. Second, we decided to exclude the following variables because of too many missing values: childhood abuse (90 missing values), target BMI and target BMI reached/not reached (39 missing values), percentage of weight loss according to a BMI of 18 (42 missing values), and weight stability after discharge (62 missing values because no access to data outside the institution post-discharge). Other variables were excluded because, in retrospect, we considered them clinically irrelevant to our research question: civil status and number of siblings.
Statistical analysis
First, weight gain after 2 weeks of hospitalization was the main dependent variable with three categories—optimal (OWG), moderate (MWG) or inadequate weight gain (IWG)—as determined by clinical assessment of actual weight curves. According to hypotheses generated at the beginning of the study, we analyzed potential differences along selected socio-demographic and clinical characteristics at admission and at discharge using ANOVA for continuous independent variables (with Tukey correction for multiple comparisons) and the Pearson’s Chi-squared test for categorical independent variables.
Since, in the course of analyses, weight gain during the first 2 weeks of admission emerged as an important factor associated with weight gain after 2 weeks, we decided to perform similar hypotheses-generated bivariable analyses to identify factors associated with weight change in the first 2 weeks of admission as a minor dependent variable with three categories.
For both dependent variables—weight gain after 2 weeks and weight gain during the first 2 weeks—we assessed the pattern of findings using the original three categories as defined by clinicians to determine whether it would make sense to collapse them into two categories. Since the three categories proved to be sufficiently distinct in both instances, these descriptive analyses were maintained. In the text, we note factors which are significantly by different weight gain at p < 0.05 as well as tendentially suggestive at p < 0.20. All statistical analyses were performed with IBM SPSS Statistics 23 for PC.
Results
Overall sample description
As can be seen in Table 1, a large majority of the 107 patients with AN were female Swiss adults with a mean age of 26.9 years (SD 11.2, range 13.6–55.8). Three quarters of the patients were single, and 21.8% lived alone. One-third were either unemployed (10.5%) or on disability (22.9%).
Table 2 presents the patients’ clinical characteristics collected at admission to the hospital. Over half of the patients (57.9%) presented a restricting form of AN and were admitted to the hospital for refeeding purposes. 69.9% of the patients presented moderate or severe malnutrition stage at admission (BMI < 16 kg/m2). The average BMI was 14.8 (SD 1.85), 56.3% reported excessive exercise and 42.9% vomiting habits. Furthermore, 8.3% reported recent suicidal ideation. 30.8% of the patients were hospitalized before the implementation of the refeeding protocol.
As for their medical history, around half of the patients (52.8%) had previously been hospitalized for ED, and a third (32.9%) in a psychiatric unit. Over 85% of the patients had been treated by health care providers either in a day care unit or in psychiatric therapy. The average age of onset was 17.8 years (SD 6.2) with an average duration of 9 years (SD 9.8). Moreover, 20% had mood or personality disorders. 15% reported a family history of ED.
In Table 3, data concerning patients’ hospital stay and clinical characteristics at discharge are shown. On average, the total length of hospitalization was 72.9 days (SD 48.8). The average weight gain and BMI at discharge were 6.2 (SD 4.6) and 17.1 (SD 1.5), respectively. The difference between average BMI at admission and discharge was 2.3. During their stay, 76.2% developed an electrolytic disorder (including 72.4% hypocalcemia). The day care centre received 42.9% of the outpatients, and 44.9% were rehospitalized at a later date. Moreover, based on the same data and refeeding protocol [Gjoertz et al., submitted], the rehospitalization rate remained comparable before and after the introduction of the refeeding protocol (48.5% before protocol vs 43.2% post protocol).
Half of the inpatients (56.1%) increased their weight in the first 2 weeks of admission, whereas 22.4% showed a decrease or U-curved weight gain. Two weeks after admission, 30.4% of the patients demonstrated OWG at over 750 g/week, 43.6% MWG at between 500 and 750 g/week, and 26.3% IWG at less than 500 g/week.
Factors associated with weight gain after 2 weeks of hospitalization
In Table 4, demographic and clinical variables previously hypothesized to be associated with weight gain after 2 weeks of hospitalization are shown. The proportion of adults was highest in the group of patients with IWG at 92.3% (p = 0.04). The average age at admission was tendentially lowest in the group of patients with MWG at 24.0 years (SD 9.3, p = 0.10), whereby average age at onset of ED was tendentially highest among patients with OWG at 20.0 years (SD 9.4, p = 0.07).
Half the patients with IWG reported prior hospitalization in a psychiatric unit, compared to a third of patients with OWG and only 16.3% of patients with MWG (p = 0.004), mirrored by the findings on the average number of prior hospitalizations in specialized ED unit (p = 0.19). Patients with OWG were tendentially least likely to report a history of outpatient medical support prior to hospitalization at 78.6% (p = 0.18). Schizophrenia and personality disorders were the two psychiatric co-morbidities linked tendentially with IWG with prevalences of 11.5% (p = 0.06) and 34.6% (p = 0.10), respectively.
The average BMI for adults at admission was tendentially highest in the IWG group at 15.5 (p = 0.07), and there was also a tendency for this group to have the lowest prevalence of moderate to severe malnutrition stage (BMI < 16 kg/m2) at 61.5% (p = 0.20). Patients with OWG or MWG were most likely to present a restricting form of AN, whereas patients with IWG were most likely diagnosed with binge-eating/purging subtype (p = 0.02). At the time of admission, patients with IWG were most likely to report self-induced vomiting habits at 62.5% (p = 0.05), whereas patients with MWG were tendentially least likely to report laxative abuse at 5.3% (p = 0.07).
Among inpatients with OWG, 83.3% demonstrated increasing weight during the first 2 weeks of hospitalization. Moreover, 45.5% of patients who initially increased their weight continued on to OWG. On the flip side, half the subjects with IWG demonstrated weight decrease during the first 2 weeks of hospitalization. Accordingly, 56.6% of patients with initial weight decrease continued on to IWG after 2 weeks (p < 0.001). After implementation of the refeeding protocol, the percentage of OWG increased from 6.3 to 41.8%, and the proportion of patients with IWG dropped from 37.5 to 20.9% (p = 0.001).
Factors associated with weight change during the first 2 weeks of hospitalization
Since weight gain in the first 2 weeks of hospitalization appears to be strongly correlated with weight gain after 2 weeks, we also explored potential factors associated with weight change in the first 2 weeks of hospitalization (Table 5). Although only the association between weight gain and the introduction of the protocol remained significant, several variables demonstrated potential tendencies which may be worthy of consideration.
The three categories can be characterized as follows: patients with initial weight gain were tendentially more likely to present restrictive form of AN (66.7%, p = 0.17), to be adolescent (31.7%, p = 0.22), and to have a family history of ED (20%, p = 0.26). This group was tendentially least likely to report prior hospitalization in a psychiatric unit (p = 0.24). On average, the BMI at admission for adults was lowest in this group at 14.4 (p = 0.11). Among patients with no initial weight gain or loss, they occupied an intermediate position along several indicators; however, they were tendentially most likely to report previous hospitalization in an ED unit (69.6%, p = 0.19) and any history of outpatient follow-up (95.5%, p = 0.30) yet least likely to report concentration disorders at admission (20%, p = 0.17). Finally, half the patients with initial weight loss presented binge-eating/purging subtype of AN at admission (50.0%, p = 0.17) and a history of outpatient psychiatric support (54.5%, p = 0.30). This group was also tendentially most likely to present substance abuse (12.5%, p = 0.28) and suicidal ideation (17.6%, p = 0.23).
Discussion
The present research attempted to identify factors associated with different weight gain patterns surrounding the introduction of a new refeeding protocol [Gjoertz et al., submitted; Online Resource 1]. Five factors were significantly associated with weight evolution after the first 2 weeks: initial weight gain during the first 2 weeks of hospitalization, implementation of the refeeding protocol, prior hospitalization in a psychiatric unit, AN subtype, and age at admission.
Factors associated with weight gain after 2 weeks of hospitalization
In this study, we find that weight gain in the first 2 weeks of hospitalization appears to have a strong influence on the course of weight gain thereafter. Weight gain in the first 2 weeks of admission was strongly associated with OWG after 2 weeks of admission. Similarly, weight loss in the first 2 weeks of admission was strongly associated with IWG after 2 weeks of admission. Therefore, enabling initial weight gain is essential for OWG. The benefits of weight gain in the treatment of AN are now well known and help prevent long-term sequelae among these patients. These results also support recent literature promoting rapid and aggressive refeeding [6, 21, 36] and the recommendations from the Society for Adolescent Health and Medicine (SAHM) [32]. Jennings et al. [13] noticed similarly an initial rapid weight gain among the group of patients displaying constant weight increase followed by flat curves. Unlike our results, the treatment-resistant group in their study showed weight increase at the beginning of hospitalization, possibly because of low resting energy expenditure at admission.
None of the patients who gained weight during the first 2 weeks presented a refeeding syndrome—i.e., a potentially fatal medical complication due to fluids and electrolytes shifts while initiating renutrition [19]. This finding suggests that intensive renutrition may be safe and effective. Using a stepwise approach to promote intensive renutrition from the very beginning of hospitalization is a safe way to improve weight gain among patients with AN. Besides, early recognition of weight drop may prevent the progression of IWG often associated with higher risk of relapse [14].
Using the same data, Gjoertz et al. (submitted) showed that “patients admitted after the introduction of the protocol were over ten times more likely to achieve OWG than those who had been hospitalized before the protocol”. More patients demonstrated weight gain in the first 2 weeks of admission following the introduction of the protocol as well. Furthermore, proportionally fewer patients had MWG, IWG and initially flat weight curves. Therefore, treatment outcomes improved with the implementation of the protocol.
Most protocols are based on staged oral refeeding using enteral nutrition as an additional measure to allow rapid and safe weight gain [5]. In the literature, it has also been shown that higher regular weekly weight gain during hospitalization was associated with higher BMI at discharge [33]. Despite the variety of clinical profiles, following a strict refeeding protocol enables multidisciplinary medical teams to offer better follow-up based on the patients’ specific needs.
Moreover, our study revealed that the majority of inpatients with IWG had been hospitalized in a psychiatric unit before, whereas most inpatients with OWG or MWG had not. This finding suggests that prior hospitalization in a psychiatric unit may be a predictive factor for IWG. Patients with severe and chronic illness tend to be less responsive to any treatment [6], and prior hospitalization in psychiatric units has been identified as a predictor of unfavorable long-term outcomes [7]. Thus, noting a previous history of psychiatric hospitalization may help clinicians to detect treatment resistance. In the present study, we also found that patients with IWG had more severe psychiatric profiles. Therefore, clinicians should improve psychological follow-up during and after hospitalization.
The association between IWG and binging/purging disorder confirms our hypothesis and is in line with the literature showing purging behaviors as negative predictive factors particularly for long-term outcomes [16, 18]. In further agreement with the literature [21,22,23,24,25,26,27], patients who binged/purged were most likely to drop-out of treatment. In our study, the prevalence of self-induced vomiting habits among IWG was also higher than binging/purging behavior. The containment of binging/purging behavior remains difficult for logistic reasons at the ED unit, but also because of the inherently unfavorable prognosis of purging behaviors compared to other types of AN diagnosis [18]. This finding reinforces the idea that purging habits are a risk factor for inpatient weight gain. Therefore, such patients should be identified early on and followed up carefully.
In our sample, patients under the age of 18 were less likely to wind up with IWG than adults. This result corresponds with our hypothesis and previous studies, whereby patients over 18 had more difficulty in reaching the target weight [28]. Since the proportion of patients dropping out of treatment was smaller in the group of patients under 18 than among adults [29] and the response to initial hospitalization in terms of weight gain predicted better maintenance 12 months post-discharge among adolescents [17], age at admission is an important factor that should be taken into account.
Several factors tendentially associated with weight gain after 2 weeks may be worthy of consideration. Variables such as psychiatric co-morbidities and the number of prior hospitalizations for ED went in the expected direction; whereas the results for BMI at admission for adults, malnutrition stage, history of medical follow-up, laxative abuse and age at onset went in a direction contrary to our original hypotheses. Only two psychiatric co-morbidities turned out to be tendentially associated with weight gain in our study—i.e., schizophrenia and disorders of personality and behavior. Both personality disorders [31] and schizophrenia [37] have been found to contribute to drop-out among inpatients. These two psychiatric disorders, which are linked with various personality disturbances, make it difficult for inpatients to follow a strict protocol, accept medical support, or adapt to a hospital environment.
The number of prior hospitalizations in a specialized ED unit was tendentially highest among patients with IWG, which is consistent with prior findings whereby failure to reach the target weight was more common among patients with prior hospitalization for ED [28]. However, other findings have shown that previous hospitalization for ED tended to protect against dropping out from inpatient treatment [30]. Although we believed that patients benefiting from medical follow-up before hospitalization were more likely to gain weight during their stay, there was no significant difference between our three categories for this variable. If anything, patients with OWG were tendentially least likely to have received any medical support prior to admission.
Patients with IWG were tendentially less likely to be diagnosed with moderate to severe malnutrition stage (BMI < 16 kg/m2) and also more likely to have a higher average BMI at admission. These results do not match our expectations and are also contrary to previous findings [28], whereby patients with lower BMI at admission tended not to reach the target weight fixed at admission or have higher risk of drop-out [23]. Only one study showed higher body weight at admission in the patient group with the most weight fluctuations [13].
However, as seen in Gjoertz et al. (submitted), BMI at admission was actually independently related to the introduction of the protocol in multivariable analyses, suggesting that the proportion of patients with high or low BMI at admission changed after the introduction of the protocol. We think that the implementation of the protocol sensitized clinicians to the importance of early hospitalization resulting in more patients being hospitalized with higher BMI at admission. Older age at onset and laxative abuse were tendentially associated with OWG. Therefore, contrary to our assumption, older age at onset and laxative abuse may not actually prevent weight gain. All subsequent factors—i.e., BMI at admission for adolescents, mood disorders, disease of the digestive system, duration of ED, length of admission, secondary diagnosis of digestive disorder, and nurse support during hospitalization—were not associated with weight gain in our study.
Factors associated with weight change during the first 2 weeks of hospitalization
Since weight change in the first 2 weeks of hospitalization is the variable with the strongest association to subsequent weight gain, we tried to identify factors associated with initial weight change. Only the introduction of the refeeding protocol demonstrated a statistically significant impact on weight gain, diminishing the percentage of flat weight curves. Several factors were tendentially associated with weight evolution during the first 2 weeks. Patients presenting with binging/purging AN subtype, substance abuse, and suicidal ideation were tendentially more likely to lose weight in the first 2 weeks of admission. Patients with prior hospitalization in a specialized ED unit or any history of out-patient follow-up were tendentially more likely to demonstrate no weight gain/loss; and patients under 18, with less prior hospitalization in a psychiatric unit, presenting with restricting AN subtype and lower BMI were tendentially more likely to increase their weight in the first 2 weeks. These characteristics may be worthy of consideration in future studies and by treating clinicians.
Limitations
There are certain limitations to our study. First, as weight evolution graphs were graded using three categories and preliminary analyses did not support collapsing into two categories, the statistical analyses remain descriptive. As initial weight loss followed by weight gain (U curves) was defined as initial weight loss, there may be equivocal results involving this category.
Second, study data were extracted from medical records in paper and electronic formats, but as is typical for actual clinical data, missing values were an issue. Useful information such as the amount of caloric intake and adherence to treatment could not be extracted because those data had not been recorded in the computer system or on paper. Although numerous practices and controls are in place to increase adherence to therapy in an inpatient setting, binging and purging could not be entirely excluded in this setting. Moreover, due to decentralized health care data in Switzerland, actual study data are limited to hospitalization at the ED unit. This means that all follow-up indicators such as stability of weight gain after discharge could not be assessed in this study as patients were referred to other institutions for outpatient follow-up management. Third, the generalizability of the findings is limited as the study covered only one hospital. However, the ED unit is the reference unit for ED in the entire canton.
Fourth, the study was supposed to encompass the same number of patients hospitalized before and after the introduction of the protocol. Nevertheless, due to a miscommunication between clinicians working at the hospital and the researchers, the actual date of the introduction of the protocol was discovered after most of the data had already been collected. It was, therefore, necessary to extract information from patients hospitalized even earlier than had already been done. Because of time restrictions, we were not able to collect data from as many patients before the protocol as after, resulting in the two groups being of unequal size: 32 patients before and 74 patients after the introduction of the protocol.
Finally, as seen in the sister publication [Gjoertz et al., submitted], not only did the introduction of the protocol have a significant impact on the main outcome of this study—strongly significant increase in the proportion of OWG post protocol—but also the patient profile changed significantly—with relationship status and BMI at admission remaining significant in multivariable analyses.
Clinical implications
Our findings suggest that intensive initial renutrition should be started immediately at admission to promote weight gain. Following a strict refeeding protocol enables safe and efficient weight gain subsequently. Moreover, some characteristics such as purging behaviors and psychiatric disorders are associated with IWG and should be taken into consideration by implementing specific treatment strategies such as cognitive-behavioral therapy during hospitalization to contain binging/purging behaviors. Early detection and adequate treatment may prevent hospitalization at a later stage and thereby improve prognosis. Unfortunately, the factors associated with weight evolution during the first 2 weeks are not as clear cut, but given their strong association with weight gain after 2 weeks, they should be elucidated in future clinical work and research.
References
Mohler-Kuo M, Schnyder U, Dermota P et al (2016) The prevalence, correlates, and help-seeking of eating disorders in Switzerland. Psychol Med 46:2749–2758. https://doi.org/10.1017/S0033291716001136
Hay PJ, Touyz S, Claudino AM et al (2019) Inpatient versus outpatient care, partial hospitalisation and waiting list for people with eating disorders. Cochrane Database Syst Rev 1:CD070827. https://doi.org/10.1002/14651858.CD010827.pub2
Eating disorders: recognition and treatment| Guidance and guidelines| NICE. https://www.nice.org.uk/guidance/ng69. Accessed 12 Jan 2019
Hay P, Chinn D, Forbes D et al (2014) Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Aust N Z J Psychiatry 48:977–1008. https://doi.org/10.1177/0004867414555814
Hale MD, Logomarsino JV (2019) The use of enteral nutrition in the treatment of eating disorders: a systematic review. Eat Weight Disord 24:179–198. https://doi.org/10.1007/s40519-018-0572-4
(2006) Treatment of Patients With Eating Disorders, Third Edition. In: APA Practice Guidelines for the Treatment of Psychiatric Disorders: Comprehensive Guidelines and Guideline Watches, 1st ed. American Psychiatric Association, Arlington, VA
Morgan HG, Russell GFM (1975) Value of family background and clinical features as predictors of long-term outcome in anorexia nervosa: four-year follow-up study of 41 patients. Psychol Med 5:355–371. https://doi.org/10.1017/S0033291700056981
Karlsson GP, Clinton D, Nevonen L (2013) Prediction of weight increase in anorexia nervosa. Nord J Psychiatry 67:424–432. https://doi.org/10.3109/08039488.2012.754051
Garber AK, Michihata N, Hetnal K et al (2012) A Prospective examination of weight gain in hospitalized adolescents with anorexia nervosa on a recommended refeeding protocol. J Adolesc Health 50:24–29. https://doi.org/10.1016/j.jadohealth.2011.06.011
Baran SA, Weltzin TE, Kaye WH (1995) Low discharge weight and outcome in anorexia nervosa. Am J Psychiatry 152:1070–1072. https://doi.org/10.1176/ajp.152.7.1070
Lay B, Jennen-Steinmetz C, Reinhard I, Schmidt MH (2002) Characteristics of inpatient weight gain in adolescent anorexia nervosa: relation to speed of relapse and re-admission. Eur Eat Disorders Rev 10:22–40. https://doi.org/10.1002/erv.432
Lund BC, Hernandez ER, Yates WR et al (2009) Rate of inpatient weight restoration predicts outcome in anorexia nervosa. Int J Eat Disord 42:301–305. https://doi.org/10.1002/eat.20634
Jennings KM, Gregas M, Wolfe B (2018) Trajectories of change in body weight during inpatient treatment for anorexia nervosa. J Am Psychiatr Nurses Assoc 24:306–313. https://doi.org/10.1177/1078390317726142
Avnon A, Orkaby N, Hadas A et al (2018) Inpatient weight curve trajectory as a prognostic factor among adolescents with anorexia nervosa: a preliminary report. Eat Weight Disord 23:645–651. https://doi.org/10.1007/s40519-017-0415-8
Keel PK, Brown TA (2010) Update on course and outcome in eating disorders. Int J Eat Disord 43:195–204. https://doi.org/10.1002/eat.20810
Salbach-Andrae H, Schneider N, Seifert K et al (2009) Short-term outcome of anorexia nervosa in adolescents after inpatient treatment: a prospective study. Eur Child Adolesc Psychiatry 18:701. https://doi.org/10.1007/s00787-009-0024-9
Lock J, Litt I (2003) What predicts maintenance of weight for adolescents medically hospitalized for anorexia nervosa? Eating Disorders 11:1–7. https://doi.org/10.1002/erv.496
Steinhausen H-C (2002) The outcome of anorexia nervosa in the 20th century. AJP 159:1284–1293. https://doi.org/10.1176/appi.ajp.159.8.1284
Le Grange D, Accurso EC, Lock J et al (2014) Early weight gain predicts outcome in two treatments for adolescent anorexia nervosa. Int J Eat Disord 47:124–129. https://doi.org/10.1002/eat.22221
Nazar BP, Gregor LK, Albano G et al (2017) Early response to treatment in eating disorders: a systematic review and a diagnostic test accuracy meta-analysis. Eur Eat Disord Rev 25:67–79. https://doi.org/10.1002/erv.2495
Garber AK, Sawyer SM, Golden NH et al (2016) A systematic review of approaches to refeeding in patients with anorexia nervosa. Int J Eat Disord 49:293–310. https://doi.org/10.1002/eat.22482
Kahn C, Pike KM (2001) In search of predictors of dropout from inpatient treatment for anorexia nervosa. Int J Eat Disord 30:237–244. https://doi.org/10.1002/eat.1080
Surgenor LJ, Maguire S, Beumont PJV (2004) Drop-out from inpatient treatment for anorexia nervosa: can risk factors be identified at point of admission? Eur Eat Disorders Rev 12:94–100. https://doi.org/10.1002/erv.539
Woodside DB, Carter JC, Blackmore E (2004) Predictors of premature termination of inpatient treatment for anorexia nervosa. AJP 161:2277–2281. https://doi.org/10.1176/appi.ajp.161.12.2277
Vall E, Wade TD (2015) Predictors of treatment outcome in individuals with eating disorders: a systematic review and meta-analysis. Int J Eat Disord 48:946–971. https://doi.org/10.1002/eat.22411
Fassino S, Pierò A, Tomba E, Abbate-Daga G (2009) Factors associated with dropout from treatment for eating disorders: a comprehensive literature review. BMC Psychiatry 9:67. https://doi.org/10.1186/1471-244X-9-67
Wallier J, Vibert S, Berthoz S et al (2009) Dropout from inpatient treatment for anorexia nervosa: critical review of the literature. Int J Eat Disord 42:636–647. https://doi.org/10.1002/eat.20609
Hubert T, Pioggiosi P, Huas C et al (2013) Drop-out from adolescent and young adult inpatient treatment for anorexia nervosa. Psychiatry Res 209:632–637. https://doi.org/10.1016/j.psychres.2013.03.034
Roux H, Ali A, Lambert S et al (2016) Predictive factors of dropout from inpatient treatment for anorexia nervosa. BMC Psychiatry 16:339. https://doi.org/10.1186/s12888-016-1010-7
Huas C, Godart N, Foulon C et al (2011) Predictors of dropout from inpatient treatment for anorexia nervosa: data from a large French sample. Psychiatry Res 185:421–426. https://doi.org/10.1016/j.psychres.2009.12.004
Pham-Scottez A, Huas C, Perez-Diaz F et al (2012) Why do people with eating disorders drop out from inpatient treatment? J Nerv Ment Dis 200(9):807–813. https://doi.org/10.1097/NMD.0b013e318266bbba
The Society for Adolescent Health and Medicine (2015) Position paper of the society for adolescent health and medicine: medical management of restrictive eating disorders in adolescents and young adults. J Adolesc Health 56:121–125. https://doi.org/10.1016/j.jadohealth.2014.10.259
Mewes R, Tagay S, Senf W (2008) Weight curves as predictors of short-term outcome in anorexia nervosa inpatients. Eur Eat Disorders Rev 16:37–43. https://doi.org/10.1002/erv.807
Hart S, Abraham S, Franklin R, Russell J (2011) Weight changes during inpatient refeeding of underweight eating disorder patients. Eur Eat Disorders Rev 19:390–397. https://doi.org/10.1002/erv.1052
Herzog T, Zeeck A, Hartmann A, Nickel T (2004) Lower targets for weekly weight gain lead to better results in inpatient treatment of anorexia nervosa: a pilot study. Eur Eat Disorders Rev 12:164–168. https://doi.org/10.1002/erv.424
Marzola E, Nasser JA, Hashim SA et al (2013) Nutritional rehabilitation in anorexia nervosa: review of the literature and implications for treatment. BMC Psychiatry 13:290. https://doi.org/10.1186/1471-244X-13-290
Nozaki T, Motoyama S, Arimura T et al (2007) Psychopathological features of anorectic patients who dropped out of inpatient treatment as assessed by the Minnesota Multiphasic Personality Inventory. Bio Psycho Soc Med 1:15. https://doi.org/10.1186/1751-0759-1-15
Acknowledgements
The authors would like to thank Dr. Andreas Niedegger and Dr. Pauline Coti Bertrand for their expertise and support.
Funding
This research did not receive any specific Grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study for this publication was approved by the Vaud Cantonal Ethics Committee.
Informed consent
The Vaud Cantonal Ethics Committee approved this retrospective medical records study without requiring patient informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chatelet, S., Wang, J., Gjoertz, M. et al. Factors associated with weight gain in anorexia nervosa inpatients. Eat Weight Disord 25, 939–950 (2020). https://doi.org/10.1007/s40519-019-00709-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00709-5