Abstract
Purpose
The current study aimed to observe potential seasonal fluctuations in weight and self-weighing behavior among a diverse sample of adults engaged in a behavioral weight loss intervention.
Methods
Active duty personnel (N = 248) were randomized to either a counselor-initiated or self-paced 12-month behavioral weight loss intervention promoting daily self-weighing. Body weight and self-weighing frequency were collected from electronic scales (e-scales) provided at baseline.
Results
Overall, participants lost weight from winter to spring (p = 0.02) and gained weight from fall to winter (p < 0.001). No demographic differences in weight changes were observed. Participants self-weighed less frequently during summer compared to spring (p < 0.0001), less in fall compared to summer (p < 0.0001), and less in winter compared to fall (p < 0.0001). In multivariate models, weight change and self-weighing frequency during the previous season, as well as days since randomization and intervention intensity were associated with seasonal weight changes.
Conclusions
This study is the first to observe seasonal fluctuations of weight and self-weighing behavior among adults actively engaged in a weight loss intervention, consistent with research in the general population. Findings highlight the importance of acknowledging seasonal influence within weight loss programs and trials.
Level of evidence
Level I, randomized controlled trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 70.7% of adults are affected by overweight [body mass index (BMI ≥ 25)] and 37.9% by obesity (BMI ≥ 30), with rates rising annually [1]. A hypothesis for this increasing prevalence is that most adults experience consistent weight fluctuations throughout the year. Across the calendar year, these weight variations are typically modest [i.e., about 0.5 kilograms (kg)] [2, 3]. However, it appears that weight peaks during certain times and is then maintained [3,4,5,6].
Specifically, the literature indicates that weight increases more during the fall and winter than in the summer months [2, 4, 7,8,9,10]. Coinciding with these seasons in the United States (US), adults, not surprisingly, tend to gain the most weight during the holiday period (mid-November–January) [3, 6, 11,12,13,14,15]. Studies have found that US adults gain between 0.4 and 0.9 kg between November and January [3, 11, 13, 15,16,17]. However, despite the warmer climate, weight gains during this period were also found in individuals living in the southern hemisphere [6].
Research on seasonal weight patterns in adults actively trying to manage weight are inconsistent [16, 18, 19]. Some previous research found that adults engaged in weight maintenance programs did not significantly gain weight during the holiday period [16, 19]. However, Baker et al. [20] found that only adults who adhered most consistently to self-monitoring protocol in a weight management intervention did not gain weight during this time. In addition to these inconsistent findings, previous studies on weight loss seeking adults measured weight change only during the holiday period, rather than measuring weight fluctuations across all four seasons. Further, seasonal weight changes have been observed with relatively infrequent anthropometric and self-report measures [2,3,4, 6, 7, 9,10,11, 13].
Fortunately, electronic scales (i.e., e-scales) (e.g., Withings™, BodyTrace™, Aria™) provide researchers the opportunity to collect weight more frequently without additional participant burden. The one study, of which we are aware, that utilized smart scales to explore long-term weight changes in the general population found similar weight patterns observed in previous literature [8, 12]. Specifically, across multiple countries with differing religious practices and in both the northern and southern hemispheres, adults lost weight in the summer months. Weight peaked in the winter for those in the northern hemisphere; however, those in the southern hemisphere gained more weight in the spring [8, 12].
Seasonal changes can also influence lifestyle factors of adults actively trying to lose weight. Increased temperature and day length have been associated with physical activity; specifically, summer-like temperatures (75°F vs. 27.1°F) and an additional hour of sunlight facilitated a greater increase in physical activity among adults engaged in an intervention focused on exercise and diet in the US Mid-West region [21]. Phelan et al. [22] found that individuals who had successfully lost weight engaged in increased self-monitoring behaviors (i.e., self-weighing, diet recording) between November and February compared to those with no history of overweight or obesity. Yet these individuals were still comparatively more vulnerable to weight gain during this period [22]. Conversely, Pellegrini et al. [23] found no seasonal differences in dietary self-monitoring of weight-loss seeking adults. However, potential seasonal fluctuations specifically in regard to self-weighing behavior are unknown.
To our knowledge, no study utilized smart scales to observe longitudinal weight and self-monitoring patterns in adults enrolled in a behavioral weight loss intervention promoting regular self-weighing on an e-scale. Importantly, although previous research suggests those with higher BMI might experience increased weight fluctuations [2, 3, 14, 24], there is conflicting and limited research on gender, racial, ethnic, and age group differences in seasonal weight change [2, 6, 11, 14, 25]. Some studies found that males were more vulnerable to these weight changes than females [2, 6, 11], while other studies reported no gender differences [13, 25]. The one study of which we are aware that measured racial and age group differences found that non-White and middle-aged individuals were the most likely to experience long-term seasonal weight variation [2]. By observing longitudinal weight patterns in a diverse population of weight-loss seeking adults, the current study aims to identify potentially critical seasons of weight gain. Additionally, exploratory analyses aim to observe if gender, race, ethnicity, age, and BMI contribute to seasonal weight fluctuations.
Methods
Participants
Participants were recruited (January 2014–March 2016) from Joint Base San Antonio, TX, using posters, electronic bulletins, presentations on the base, emails, newspaper advertisements, and word of mouth. The sample consisted of active duty personnel, who had at least 1 year left on station, were 18 years of age or older, had a BMI greater than or equal to 25.0 kg/m2, and had access to a computer and phone. Potential participants were required to self-monitor diet and physical activity for a week and obtain a letter from a healthcare provider clearing the individual for participation in the study. Participants were excluded if they failed more than one military fitness-test in the past 12 months, since military discharge would then be likely and thus make follow-up assessments challenging. Other exclusion criteria included having a medical condition that would limit one’s ability to make dietary changes or engage in physical activity or taking medication that would affect weight. The entire sample (N = 248) was approximately equally distributed by gender and BMI category, as well as racially and ethnically diverse (Table 1). Specifically, 66% identified as Caucasian, 20% as African American and 15% were classified as “Other”. The “Other” category included American Indian/Alaska Native, Asian, Native Hawaiian/Pacific Islander, multiple races, and unknown race combined given the infrequency of these responses. Further, 23% identified as Hispanic/Latino.
Procedure
Informed consent was obtained at the screening visit. Participants were randomized at the individual level using a computerized block design to either receive a counselor-initiated (CI) weight loss intervention or a self-paced (SP) intervention. Weight loss goals (10%) and personalized calorie goals based on baseline weight, as well as exercise goals (i.e., gradually increase moderate to vigorous exercise to 225–250 min per week) were the same across conditions. While each condition received a 12-month manualized behavioral weight loss program based on the Look AHEAD intensive lifestyle intervention, the two weight loss conditions varied in the level of intervention and the amount of self-initiation required. Participants received data collection incentives worth a total of $20 (i.e., a pedometer and a stainless-steel water bottle) for participating in the two follow-up data collection visits. The study protocol was approved by the Institutional Review Board (IRB) of the 59th Medical Wing in San Antonio, TX and acknowledged by the IRB at the University of Tennessee Health Science Center. Further details on the sample, the study CONSORT diagram, study procedures, and main outcomes can be found elsewhere [26, 27].
Measures
Sociodemographic characteristics
At the baseline visit, self-reported sociodemographic characteristics (i.e., gender, age, race, ethnicity) were collected. Analyses were evaluated based on the categories of gender (male, female), BMI (overweight: 25.0–29.9 kg/m2 and obese: ≥ 30 kg/m2), age group (< 30 years old, 30–40 years, > 40 years), ethnicity (non-Hispanic/Latino, Hispanic/Latino) and race (Caucasian, African American, and Other).
Body weight
At the baseline visit, participant weight was measured in kg on a calibrated scale. Height was measured in centimeters using a wall-mounted stadiometer and BMI was calculated using the standard formula. Participants were asked to monitor their weight daily using the BodyTrace™ e-scale provided to them at baseline. Their weight was uploaded daily from the e-scale to a secure website using automatic cellular transmission. Participants were able to view their weight trajectory on their personalized webpage and were provided counselor feedback about weight changes via email (if in the counselor-initiated condition or by request in the self-paced condition). Smart scales (e.g., BodyTrace™) are shown to be valid measurements of weight in comparison to weight measured at in-person visits [28].
Data analysis
In univariate analyses, mean percent of weight change from a given season to the subsequent season was compared across participant characteristics (i.e., gender, race, age, ethnicity, BMI category, intervention condition,) using Wilcoxon–Mann–Whitney and Kruskal–Wallis tests. In addition, mean number of times participants self-weighed during each given season compared to the subsequent season was compared using Wilcoxon–Mann–Whitney test. Spearman’s rank correlations measured the association between continuous variables of interest (i.e., weight change during given season, number of days since randomization, frequency of self-weighing during the given season, maximum and average weight during the given season, standard deviations of weights during the given season) and percent of weight change from the given to subsequent season. For seasonal comparisons, astronomical seasons were used [i.e., winter (December 22–March 21st), spring (March 22nd–June 21st), summer (June 22nd–September 22nd), fall (September 22nd–December 21st)] to facilitate comparisons with previous research of seasonal weight fluctuations [8]. Multiple regression step-wise modeling predicted the mean percent of weight change from each given season to the subsequent season controlling for significant covariates. Models comparing overall weight change (kg) and weekly rate of weight change between seasons found similar results (data not shown). To be included in each season comparison, participants had at least two BodyTrace™ weights that were ≥ 14 days apart within both the given and subsequent season.
Results
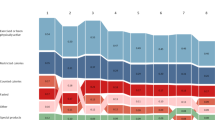
Winter to spring
The sample characteristics varied slightly depending on engagement with self-weighing during each season (Table 2). In univariate analyses, overall, there was a significant weight change (p = 0.004) from winter to spring (n = 193) (Table 2). On average, participants lost 0.61% of weight (0.53 kg) between these two seasons. Weight change did not differ by gender, ethnicity, race, age or BMI. A non-significant trend suggested that those in the CI intervention group lost more weight between winter and spring (p = 0.052); specifically, on average the CI group lost 1.00% of weight and those in the SP group lost 0.19% of weight. As detailed in Table 3, weight change between winter and spring was significantly positively correlated with the number of days since randomization (by the end of winter) (r = 0.28, p < 0.0001) and weight change during the winter season (r = 0.59, p < 0.0001). Specifically, fewer days since randomization and increased weight loss during the winter season was associated with increased weight loss from winter to spring. Weight change between winter and spring was significantly negatively correlated with standard deviation of weights during winter (r = – 0.27, p < 0.0001). Thus, increased variability of weight during winter was associated with increased weight loss between winter and spring. No other significant relationships were observed. The mean number of days participants self-weighed did not significantly differ between winter and spring [M 40.6, SD (standard deviation) 26.7 vs. M 39.7, SD 28.2, respectively].
In multivariate models, intervention group (p = 0.009) and weight change during winter (p < 0.0001) were significant predictors of increased weight loss between the two seasons (Table 4). Specifically, greater weight loss during winter and being part of the CI intervention group was associated with increased weight loss from winter to spring. After accounting for covariates, on average, the CI group lost 0.99% of their baseline weight (M = 0.86 kg) and the SP group lost 0.19% of baseline weight (0.18 kg) from winter to spring.
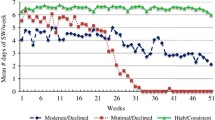
Spring to summer
In univariate analyses, overall, there was not a significant weight change between spring and summer (p = 0.095) (n = 170) (Table 2). Weight change did not significantly differ by gender, ethnicity, race, age or BMI category. As presented in Table 3, weight change between spring and summer was significantly positively correlated with number of days since randomization (by the end of spring) (r = 0.27, p = 0.0003) and weight change during the spring season (r = 0.49, p < 0.0001); such that, increased number of days since randomization and increased weight gain during spring was associated with increased weight gain from spring to summer. No other significant relationships were observed. On average, participants self-weighed significantly less frequently during summer compared to spring (M = 36.5, SD = 26.7 vs. M = 44.3, SD = 26.7, respectively, p < 0.0001).
In multivariate models, weight change between spring and summer was found to be a function of days on study since randomization (by the end of spring) (p = 0.0096) and weight change during the spring season (p < 0.0001) (Table 4). Specifically, each additional month from randomization (by the end of spring) was associated with increased weight gain by 0.30% on average. Additionally, each one kg of weight gain during spring was associated with increased weight gain from spring to summer by 0.20% on average.
Summer to fall
In univariate analyses, overall, weight did not significantly change between summer and fall (p = 0.27) and this did not significantly differ by gender, ethnicity, race, age or BMI category (n = 118) (Table 2). Weight change between summer and fall was positively correlated with summer weight change (r = 0.57, p < 0.0001); such that, increased weight gain during the summer season was associated with increased weight gain from summer to fall (Table 3). No other significant relationships were observed. On average, participants self-weighed significantly less frequently during fall than summer (M = 28.2, SD = 25.3 vs. M = 45.7, SD = 24.6, respectively, p < 0.0001).
In multivariate models, weight change during the summer season was the only significant predictor of weight change between summer and fall (p < 0.0001) (Table 4). Specifically, on average, no change in weight during summer was associated with a 0.5 kg increase in weight from summer to fall. Further, 2.0 kg of weight loss during summer, on average, was associated with 1.5 kg of weight loss between summer and fall.
Fall to winter
In univariate analyses, overall, there was a significant weight change between fall and winter (p < 0.001) (n = 68) (Table 2). On average, participants gained 1.21% of weight (1.01 kg) from fall to winter. Weight change did not significantly differ by gender, ethnicity, race, age or BMI. However, those in the CI intervention group gained more weight between fall and winter (p = 0.043); specifically, on average, the CI group gained 1.72% of baseline weight and those in the SP group gained 0.64% of baseline weight. Weight change between fall and winter was significantly positively correlated with weight change during the fall season (r = 0.49, p < 0.0001); such that, increased weight gain during the fall season was associated with increased weight gain from fall to winter (Table 3). Weight change between fall and winter was significantly negatively correlated with the number of days participants self-weighed during fall (r = – 0.37, p < 0.0001); such that, less frequent self-weighing during the fall season was associated with increased weight gain between fall and winter. Participants, on average, weighed significantly less frequently during winter than fall (M = 27.3, SD = 22.6 vs. M = 38.1, SD = 24.6, respectively, p < 0.0001).
In multivariate models, increased weight gain during the fall season (p < 0.0001), less frequent self-weighing during fall (p = 0.0011), and the CI condition (p = 0.04) were significant predictors of increased weight gain between fall and winter (Table 4). After accounting for covariates, on average, those in the CI group gained 1.72% of weight (M = 1.46 kg) and the SP group gained 0.65% of weight (M = 0.51 kg) between fall and winter. Further, accounting for other influencing factors, on average, each additional day of self-weighing was associated with a 0.03% weight loss between the two seasons and each additional kg of weight gain in fall was associated with a 0.25% weight increase from fall to winter.
Discussion
Current findings are the first, to our knowledge, to observe seasonal weight fluctuations among weight-loss seeking adults. Results suggest that adults experienced seasonal weight gains and losses throughout the year despite active engagement in a behavioral weight loss intervention. Overall, participants weighed significantly more in winter (December 22nd–March 21st) than they did in the previous fall season. These results are consistent with previous research in the general population, which suggest that adults experience increased weight gain in the fall and winter compared to summer months [2, 4, 7,8,9,10]. However, inconsistent with findings that indicate adults maintain this weight gain the rest of the year [4,5,6], these individuals, on average, lost a significant amount of weight the following spring (March 22nd–June 21st). Perhaps, participation in a weight loss intervention helped to prevent the current sample from retaining their winter weight gains.
Seasonal fluctuations in self-weighing frequency were also observed. Despite an overall decrease in weight from winter to spring, there were no differences in self-weighing frequency between these two seasons. Additionally, although weight between spring and summer remained stable, individuals self-weighed less in summer than in spring. Less surprisingly, consistent with the average experience of weight gain during this seasonal change, adults self-weighed themselves less frequently in fall compared to summer, as well as less frequently in winter compared to fall. Although dissimilar from previous research suggesting no seasonal effects of dietary self-monitoring [23], the current study is the first, to our knowledge, to observe seasonal changes specifically in regard to self-weighing. Perhaps, adults self-weigh themselves less consistently near the end of the year, in anticipation of weight gain during fall and winter. Given that research suggests frequent self-weighing is effective for successful weight loss, avoidance of this behavior during this period could perhaps influence even greater weight gain [29, 30].
Surprisingly, although the CI intervention group lost more weight than the SP group from winter to spring, this group gained significantly more weight from fall to winter. The SP group gained weight (0.65%, M = 0.51 kg) at a modest rate similarly to that reported among the general population in previous studies [3, 11, 13, 15,16,17]. In comparison, the increased weight gain of the CI group (1.72%, M = 1.46 kg), suggests that individuals enrolled within a more intensive weight loss intervention might be more susceptible to weight gain during the winter season. Throughout the intervention, the CI group most likely engaged in more frequent weight loss behaviors (e.g., self-weighing, dietary self-monitoring, receiving counselor feedback). Thus, during winter (coinciding with the US holiday season), the CI group perhaps practiced less restrictive eating and self-weighing due to depletion of self-regulatory capacity [31, 32]. Further, after enrollment in a weight loss trial and experiencing successful weight loss, the CI group might have felt less vulnerable to winter weight gain and subsequently practiced less self-monitoring behavior. This finding is consistent with a previous study that found adults who had successfully lost weight were more vulnerable to weight gain between November and January [22]. Additionally, after experiencing less successful treatment outcome during the winter period, the CI group appeared to be even more motivated to lose weight (0.99%, M = 0.86 kg) in anticipation of spring in comparison to the SP group (0.19%, M = 0.18 kg).
Inconsistent with previous research suggesting differences in BMI, gender, race, and age [2, 3, 6, 11, 14, 24], the current study found no demographic differences in univariate and multivariate analyses of seasonal weight change. No differences were observed despite the fact that the current sample included a higher percentage of males (49%) and those identifying as ethnic (23%) and racial minorities (35%) compared to previous studies [2, 3, 14, 24]. These findings, consistent with some research suggesting no gender differences, indicate that, perhaps, adults are equally vulnerable to seasonal weight fluctuations regardless of a variety of demographic differences [13, 25]. Further, given that this sample consisted of active duty personnel enrolled in a weight loss intervention, fewer demographic differences might have been observed due to shared motivation for military enforced weight standards and intervention goals.
There are some limitations of the current study that are important to consider. More frequent counselor-initiated encouragement of self-weighing in the CI condition perhaps facilitated more frequent self-weighing in this group compared to the SP group. Although all participants included in these analyses self-weighed at least twice and more than 2 weeks apart within each season, individual differences in self-weighing frequency most likely occurred. In addition, because of this self-weighing criterion for inclusion in analyses, each seasonal comparison contained different sample sizes due to differences in self-weighing frequency across the seasons. For example, because participants self-weighed less frequently in fall and winter months, the smallest sample size (n = 68) was observed when comparing fall to winter seasons. Importantly, the current sample consisted of a military population, which might limit generalizability to the general population of weight loss seeking adults. Active duty military personnel have access to additional resources to assist in weight loss (e.g., free fitness centers, healthcare), and often individuals with severe health and mental health conditions are excluded from enlistment or are discharged. Further, annual fitness tests, a critical factor for employment, might have facilitated greater motivation for weight loss [33] than in the civilian population; thus, it is possible that seasonal differences might be smaller in this study than a similar study conducted in a civilian population. Despite these differences, the US Military is affected by similar rates of overweight and obesity (60.8%) compared to similar to the civilian population [34]. It is possible that these findings are most generalizable to populations who are interested in losing weight or preventing weight gain. Finally, multiple comparisons were not adjusted for given the exploratory nature of the analyses.
In the current study, the use of BodyTrace™ data provided a unique opportunity to observe more frequent, measured weight representations during each season. However, future studies should use e-scale measurements to observe seasonal weight patterns among other samples of weight loss seeking adults, as well as account for individual differences in self-weighing frequency. Additionally, the climate of the current study site, San Antonia, Texas, might have influenced these specific seasonal weight patterns. Thus, future studies should replicate findings in locations with differing climates. Further, given the inconsistencies in the literature among the general population, researchers should continue to explore potential demographic differences in seasonal weight fluctuations among adults actively trying to lose weight [2, 6, 11, 13, 14, 25].
Similar to a previous study examining seasonal differences in behavior of adults in a physical activity intervention [21], the current study highlights the importance of acknowledging the influence of season within behavioral weight loss interventions. Perhaps, weight loss programs might further increase support and motivation during the fall and winter seasons in anticipation of the less successful weight loss during these seasons as seen in this study. Adults might benefit from information about seasonal weight variations, to prepare for potentially modest weight gains during these seasons. Additionally, anticipation of spring and summer (e.g., swimsuit season, increased physical activity due to warmer climate) might help facilitate even more successful weight loss. Perhaps, enrollment in weight loss programs might be more beneficial in the spring, a period with the highest chance for weight loss, compared to fall. Additionally, seasonal effects of treatment outcomes in behavioral weight loss trials might be important to consider. Finally, despite actively engaging in weight loss behaviors consistent with those in a behavioral weight loss intervention, adults still might experience seasonal weight fluctuations similarly to the general population.
References
Ogden CL, Fryar CD, Carroll MD, Flegal KM (2004) Mean body weight, height, and body mass index, United States 1960–2002. Adv Data 347:1–17
Ma Y, Olendzki BC, Li W et al (2006) Seasonal variation in food intake, physical activity, and body weight in a predominantly overweight population. Eur J Clin Nutr 60(4):519–528. https://doi.org/10.1038/sj.ejcn.1602346
Yanovski JA, Yanovski SZ, Sovik KN, Nguyen TT, O'Neil PM, Sebring NG (2000) A prospective study of holiday weight gain. N Engl J Med 342(12):861–867. https://doi.org/10.1056/NEJM200003233421206
Sabbag C (2012) Seasonal BMI changes of rural women living in Anatolia. Int J Environ Res Public Health 9(4):1159–1170. https://doi.org/10.3390/ijerph9041159
Schoeller DA (2014) The effect of holiday weight gain on body weight. Physiol Behav 134:66–69. https://doi.org/10.1016/j.physbeh.2014.03.018
Sturm R, Patel D, Alexander E, Paramanund J (2016) Seasonal cycles in food purchases and changes in BMI among South Africans participating in a health promotion programme. Public Health Nutr 19(15):2838–2843. https://doi.org/10.1017/S1368980016000902
Lloyd L, Miller B (2013) The impact of seasonality on changes in body weight and physical activity in Mexican-American women. Women Health 53(3):262–281
Mehrang S, Helander E, Chieh A, Korhonen I (2016) Seasonal weight variation patterns in seven countries located in northern and southern hemispheres. Conf Proc IEEE Eng Med Biol Soc 2016:2475–2478. https://doi.org/10.1109/EMBC.2016.7591232
Shahar DR, Froom P, Harari G, Yerushalmi N, Lubin F, Kristal-Boneh E (1999) Changes in dietary intake account for seasonal changes in cardiovascular disease risk factors. Eur J Clin Nutr 53(5):395–400
Visscher TL, Seidell JC (2004) Time trends (1993–1997) and seasonal variation in body mass index and waist circumference in the Netherlands. Int J Obes Relat Metab Disord 28(10):1309–1316. https://doi.org/10.1038/sj.ijo.0802761
Cook CM, Subar AF, Troiano RP, Schoeller DA (2012) Relation between holiday weight gain and total energy expenditure among 40- to 69-y-old men and women (OPEN study). Am J Clin Nutr 95(3):726–731. https://doi.org/10.3945/ajcn.111.023036
Helander EE, Wansink B, Chieh A (2016) Weight gain over the holidays in three countries. N Engl J Med 375(12):1200–1202. https://doi.org/10.1056/NEJMc1602012
Stevenson JL, Krishnan S, Stoner MA, Goktas Z, Cooper JA (2013) Effects of exercise during the holiday season on changes in body weight, body composition and blood pressure. Eur J Clin Nutr 67(9):944–949. https://doi.org/10.1038/ejcn.2013.98
Hourdakis M, Papandreou D, Malindretos P, Vassilakou D, Papastergiou D, Tantsidis D, Kouvelas D (2010) Effect of Greek orthodox Easter holidays on body weight gain. Prev Nutr Food Sci 40(1):49–54. https://doi.org/10.1108/00346651011015917
Rees SG, Holman RR, Turner RC (1985) The Christmas feast. Br Med J (Clin Res Ed) 291(6511):1764–1765
Andersson I, Rossner S (1992) The Christmas factor in obesity therapy. Int J Obes Relat Metab Disord 16(12):1013–1015
Reid R, Hackett AF (1999) Changes in nutritional status in adults over Christmas 1998. J Hum Nutr Diet 12(6):513–516. https://doi.org/10.1046/j.1365-277x.1999.00205.x
Boutelle KN, Kirschenbaum DS, Baker RC, Mitchell ME (1999) How can obese weight controllers minimize weight gain during the high-risk holiday season? By self-monitoring very consistently. Health Psychol 18(4):364–368
Watras AC, Buchholz AC, Close RN, Zhang Z, Schoeller DA (2007) The role of conjugated linoleic acid in reducing body fat and preventing holiday weight gain. Int J Obes (Lond) 31(3):481–487. https://doi.org/10.1038/sj.ijo.0803437
Baker RC, Kirschenbaum DS (1998) Weight control during the holidays: highly consistent self-monitoring as a potentially useful coping mechanism. Health Psychol 17(4):367–370
Welch WA, Spring B, Phillips SM, Siddique J (2018) Moderating effects of weather-related factors on a physical activity intervention. Am J Prev Med 54(5):e83–e89. https://doi.org/10.1016/j.amepre.2018.01.025
Phelan S, Wing RR, Raynor HA, Dibello J, Nedeau K, Peng W (2008) Holiday weight management by successful weight losers and normal weight individuals. J Consult Clin Psychol 76(3):442–448. https://doi.org/10.1037/0022-006X.76.3.442
Pellegrini CA, Conroy DE, Phillips SM, Pfammatter AF, McFadden HG, Spring B (2018) Daily and seasonal influences on dietary self-monitoring using a smartphone application. J Nutr Educ Behav 50(1):56–61. https://doi.org/10.1016/j.jneb.2016.12.004
Hull HR, Hester CN, Fields DA (2006) The effect of the holiday season on body weight and composition in college students. Nutr Metab (Lond) 3:44. https://doi.org/10.1186/1743-7075-3-44
Wagner DR, Larson JN, Wengreen H (2012) Weight and body composition change over a six-week holiday period. Eat Weight Disord 17(1):e54–56
Krukowski RA, Hare ME, Talcott GW, Johnson KC, Richey PA, Kocak M et al (2015) Dissemination of the Look AHEAD intensive lifestyle intervention in the United States Air Force: study rationale, design, and methods. Contemp Clin Trials 40:232–239. https://doi.org/10.1016/j.cct.2014.12.014
Krukowski RA, Hare ME, Talcott GW, Gladney LA, Johnson KC, Richey PA, Klesges RC (2018) Dissemination of the look AHEAD intensive lifestyle intervention in the United States military: a randomized controlled trial. Obesity 26(10):1558–1565. https://doi.org/10.1002/oby.22293
Pebley K, Klesges RC, Talcott GW, Kocak M, Krukowski RA (in press) E-scale measurements in comparison to clinic weight measurements. Obesity
Shieh C, Knisley MR, Clark D, Carpenter JS (2016) Self-weighing in weight management interventions: a systematic review of literature. Obes Res Clin Pract 10(5):493–519. https://doi.org/10.1016/j.orcp.2016.01.004
Zheng Y, Klem ML, Sereika SM, Danford CA, Ewing LJ, Burke LE (2015) Self-weighing in weight management: a systematic literature review. Obesity (Silver Spring) 23(2):256–265. https://doi.org/10.1002/oby.20946
Vohs KD, Heatherton TF (2000) Self-regulatory failure: a resource-depletion approach. Psychol Sci 11(3):249–254. https://doi.org/10.1111/1467-9280.00250
Hofmann W, Rauch W, Gawronski B (2007) And deplete us not into temptation: automatic attitudes, dietary restraint, and self-regulatory resources as determinants of eating behavior. J Exp Soc Psychol 43:497–504. https://doi.org/10.1016/j.jesp.2006.05.004
Dall TM, Zhang Y, Chen YJ, Askarinam Wagner RC, Hogan PF, Fagan NK et al (2007) Cost associated with being overweight and with obesity, high alcohol consumption, and tobacco use within the military health system’s TRICARE prime-enrolled population. Am J Health Promot 22:120–139. https://doi.org/10.4278/0890-1171-22.2.120
Tanofsky-Kraff M, Sbrocco T, Theim KR, Cohen LA, Mackey ER, Stice E, Henderson JL, McCreight SJ, Bryant EJ, Stepehens MB (2013) Obesity and the US military family. Obesity 21:2205–2220. https://doi.org/10.1002/oby.20566
Acknowledgements
The research represents a Collaborative Research and Development Agreement with the United States Air Force (CRADA #13-168-SG-C13001). The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (RO1 DK097158) of the National Institutes of Health, with the title of “Dissemination of the Look Ahead Weight Management Treatment in the Military”, Robert Klesges and Rebecca Krukowski, Principal Investigators. The trial is registered on clinicaltrials.gov (NCT 02063178). The opinions expressed in this document are solely those of the authors and do not represent an endorsement by or the views of the United States Air Force, the Department of Defense, or the United States Government. Finally, we would like to thank the participants and the research team for their dedication to the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the Institutional Review Board of the 59th Medical Wing in San Antonio, Texas and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants in the currrent study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fahey, M.C., Klesges, R.C., Kocak, M. et al. Seasonal fluctuations in weight and self-weighing behavior among adults in a behavioral weight loss intervention. Eat Weight Disord 25, 921–928 (2020). https://doi.org/10.1007/s40519-019-00707-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00707-7