Abstract
Purpose
We aimed to compare the predictive ability of the anthropometric indices reflecting general, central and visceral obesity for identification of metabolic syndrome (MetS) in maintenance hemodialysis (MHD) patients.
Methods
A multicenter, cross-sectional study that consisted of 1603 adult MHD patients (54.6 ± 16 years) was conducted in Guizhou Province, Southwest China. Eight anthropometric obesity indexes including body mass index (BMI), waist circumference (WC), waist-height ratio (WHtR), conicity index (Ci) and visceral adiposity index (VAI), lipid accumulation product (LAP), a body shape index (ABSI) and body roundness index (BRI) were recorded. MetS was defined based on the criteria of the International Diabetes Federation. Participants were categorized into four groups according to quartiles of different obesity indices. Binary logistic regression analyses were used to evaluate the associations between the eight obesity parameters and MetS. Receiver operator curve (ROC) analyses were used to identify the best predictor of MetS.
Results
The eight anthropometric obesity indexes were independently associated with MetS risk, even after adjustment for age, sex, educational status and history of smoking. The ROC analysis revealed that all the eight obesity indices included in the study were able to discriminate MetS [all area under the ROC curves (AUCs) > 0.6, P < 0.05]. LAP showed the highest AUC and according to the maximum Youden indexes, the cut off values for men and women were 27.29 and 36.45, respectively. The AUCs of LAP, VAI, ABSI, BRI, WC, WHtR, Ci and BMI were 0.88, 0.87, 0.60, 0.78, 0.79, 0.78, 0.69 and 0.76 for men, and 0.87, 0.85, 0.65, 0.79, 0.81, 0.79, 0.73 and 0.76 for women, respectively. There was no significant difference in the AUC value between LAP and VAI, BRI/WHtR and BMI in men and between BRI/WHtR and BMI in women. The AUC value for WHtR was equal to that for BRI in identifying MetS.
Conclusions
Visceral obesity marker LAP followed by VAI was the most effective predictor of MetS while ABSI followed by CI was the weakest indicator for the screening of MetS in MHD patients. BRI could be an alternative obesity measure to WHtR in assessment of MetS. LAP may be a simple and useful screening tool to identify individuals at high risk of MetS particularly in middle-aged and elderly Chinese MHD patients.
Level of evidence
Level V, descriptive study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Metabolic syndrome (MetS), characterized as a cluster of metabolic abnormalities, including hypertension, dysglycemia, central obesity, elevated triglyceride (TG) levels, and low high-density lipoprotein cholesterol (HDL-C) levels [1], has gradually risen as a major medical problem with an increasing prevalence in China in recent decades. The prevalence of MetS in mainland china has increased to 24.5% according to a study published in 2016 [2]. It seems that MetS is more common in maintenance hemodialysis (MHD) patients. The prevalence of MetS ranged from 61.0 to 75.3% among patients receiving hemodialysis in Taiwan [3]. MetS is associated with an increased risk of all-cause mortality in dialysis patients [4] and dialysis subjects with MetS had a nearly 6.42-fold greater risk of developing cardiovascular disease (CVD) events than those without MetS. Early identification and intervention of subjects with MetS are, therefore, indispensable to reduce mortality and CVD risk in MHD patients.
Obesity is a known risk factor of MetS. Obesity could be generally divided into general obesity which is commonly assessed with body mass index (BMI) and central adiposity with waist circumference (WC) as the most common measure. Other anthropometric measurements such as waist-to-height ratio (WHtR), waist–hip ratio and conicity index (Ci) are also widely used to evaluate central adiposity [5, 6]. None of these indexes, however, have the ability to distinguish subcutaneous fat from the visceral fat. Several studies have pointed out that it is visceral obesity but not subcutaneous adiposity that correlates with the metabolic abnormalities [7] and visceral fat is more strongly associated with incident MetS than subcutaneous fat [8]. Imaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI) are gold standards for assessing visceral fat [9], but their unfavorable characteristics such as time-consuming, relatively expensive, and expose the patient to contrast and radiation disenabled them to be used in clinical routine and epidemiological studies. Thus, the appearance of cheap and convenient surrogate markers of visceral adiposity which are feasible in general practice is of great importance. Visceral adiposity index (VAI) and lipid accumulation product (LAP) are validated reliable markers of visceral obesity [10, 11]. Recent years, a body shape index (ABSI) and body roundness index (BRI) have been proposed as alternative assessment parameters of visceral obesity [12, 13].There are only scarce data evaluating the predictive power of ABSI and BRI for the presence of MetS [14]. To the best of our knowledge, no study has investigated and compared the association between anthropometric indices reflecting general, central, visceral obesity and MetS in MHD patients.
Though several studies have compared the predictive power of different anthropometric measurements in predicting MetS in general population, no consensus has been reached to date regarding which index is best [14, 15]. We aimed to investigate and compare the predictive strength of the eight obesity indices which reflect general (BMI), abdominal (WC, WHtR, CI) and visceral (VAI, LAP, ABSI, BRI) obesity in assessment of MetS among Chinese MHD patients.
Materials and methods
Participants
We conducted a multicenter, cross-sectional study in the hemodialysis centers of 11 hospitals in Guizhou Province, Southwest China. As described in our previous research [16], all adult MHD patients who received 4-h standard twice to thrice-weekly dialysis treatment from June 1, 2017 to September 30, 2017 were invited to take part in our study. Participants were eligible for inclusion if they were aged 18 years or older and on standard MHD at these 11 hemodialysis centers for at least 3 months or longer. Exclusion criteria included those with hearing disabilities, physical deformities, language barriers, obvious edema or ascites. Patients on any kind of nutritional support or receiving HD for less than 3 months were also excluded from our study. All subjects enrolled in the present study had submitted written informed consent. The study protocol was approved by the ethics committee of The People’s Hospital of Guizhou province and this study was performed fulfilling the principles of Helsinki Declaration.
Data collection
Demographic information, medical history of hypertension, diabetes and details about lifestyle such as current or past cigarette smoking, educational status were obtained through a pretested questionnaire. The questionnaire was completed through a face-to-face interview by well-trained physicians. Blood pressure (BP) was taken in the non-fistula arm in a standardized manner by the nurses in the 11 hemodialysis centers. Pre-dialysis BP was measured before hemodialysis in a sitting position after a 5-min rest period. Intradialytic BP and post-dialysis BP were measured with the participants in the supine position. The latest laboratory parameters such as triglyceride (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c), fasting glucose were extracted from medical records. Participants who did not have laboratory parameters in the past 3 months were excluded in the final analysis.
Anthropometric measures
Anthropometric measurements were performed following standardized procedures after a routine HD session by well-trained nurses and physicians. Body weight was measured with an electronic scale with participants barefoot and in light clothing. Height was measured with participants barefoot and standing erect and measured to the nearest 1 cm.
Waist circumference (WC) was measured at the shortest point below the lower rib margin and the iliac crest in standing positions with an inelastic tape and measured to the nearest 1 cm.
Calculation of anthropometric indices
BMI, WHtR, CI [17], LAP index [18], VAI [11], ABSI [13] and BRI [12] were calculated with the following formulas:
-
BMI = weight (kg)/ height2 (m2);
-
WHtR = WC (cm)/ height (cm);
-
CI = 0.109−1 WC (m)[Weight (kg)/Height (m)]−1/2;
-
LAPmen = (WC(cm)-65) × TG(mmol/l);
-
LAPwomen = (WC(cm)-58) × TG(mmol/l);
-
VAImen = WC∕[39.68 + (1.88 × BMI)] × TG∕1.03 × 1.31∕HDL;
-
VAIwomen = WC∕[36.58 + (1.89 × BMI)] × TG∕0.81 × 1.52∕HDL;
-
ABSI = WC(m)/ [BMI2/3 (kg/m2) × height1/2 (m)];
-
BRI = 364.2 − 365.5[1 − π−2WC2 (m) Height−2 (m)]1/2.
Definition of MetS
According to the International Diabetes Federation (IDF) criteria [19], participants are considered to have MetS if they have central obesity (waist circumference ≥ 90 cm for men or ≥ 80 cm for women) plus any two of the four factors: (1) fasting serum glucose ≥ 5.6 mmol/L or have a history of diabetes; (2) serum triglycerides ≥ 1.7 mmol/L; (3) HDL cholesterol level < 1.03 mmol/L in men or < 1.29 mmol/L in women; (4) blood pressure ≥ 130/85 mmHg or have a history of high blood pressure and current use of antihypertensive medication.
Statistical analysis
The characteristics of the participants were presented as medians (interquartile range) for highly skewed variables or as mean ± standard deviation (SD) for normally distributed continuous variables. Frequency and proportion were used for qualitative data. Comparisons between patients with and without MetS were performed using one-way analysis of variance (ANOVA) tests for normally distributed continuous variables. Mann–Whitney U tests were used for highly skewed variables. Categorical variables were analyzed with the Chi-square test. Quartiles of BMI, WC, WHtR, CI, BRI, ABSI, LAP and VAI were calculated and binary logistic regression analyses were used to estimate the odds ratio for risk of MetS per quartile. The lowest quartiles of the obesity indices were set as the reference. Receiver operating characteristic (ROC) analyses were applied to determine predictive power of the eight obesity indices in assessment of MetS. The areas under the ROC curves (AUCs) with 95% confidence interval (CI) were calculated. The optimal cut off was calculated from the Youden index. Significance tests for comparison of AUCs from different obesity indices were analyzed using the method of DeLong et al. [20].
Statistical analyses were performed using SPSS software (version 13.0 for windows; SPSS, Chicago, IL, USA). The ROC analysis was performed using MedCalc version 13.0 for Windows (MedCalc Software, Mariakerke, Belgium). P values less than 0.05 were considered statistically significant.
Results
Baseline characteristics of the study population
2561 participants were included in our initial study. 884 patients were excluded from our final analysis due to missing data for anthropometric measurements and laboratory parameters. The final analysis included data obtained form 1603 adult MHD patients (54.6 ± 16 years). 40.7% (651/1603) participants in our study were female. Baseline characteristics of the participants stratified by gender were presented in Table 1. Participants with MetS were older than those without MetS both in men and women. Notably, for anthropometric indices, the medians of BMI, WC, WHtR, ABSI, BRI, CI, VAI and LAP in patients with MetS were higher than those without MetS (all P < 0.05). Hemodialysis patients who had MetS had higher levels of TG, TC, LDL-c, fasting glucose and lower HDL-c compared to those without MetS (all P < 0.05). No differences were observed for systolic and diastolic blood pressure levels between participants with and without MetS (all P > 0.05) both in men and women. Participants with MetS were more likely to have a history of hypertension and diabetes, compared with those without MetS (P < 0.05). Females with MetS had relatively low levels of education when compared to those without MetS.
Odds ratios and 95% confidence intervals of various obesity indices across their quartiles for MetS
As shown in Table 2, the binary logistic regression analysis showed that the eight anthropometric measurements included in the study were independently associated with MetS risk, even after adjustment for age, sex, educational status and history of smoking. Participants in the highest quartile of obesity indices had the highest risk to develop MetS compared to those in the lowest quartile. The adjusted relative risk of MetS increased with increasing quartiles of the eight obesity indices.
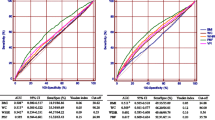
ROC curve analysis of different adiposity indices to predict MetS
The performance of the eight adiposity indices as predictors of MetS is showed in Table 3 and Fig. 1. The ROC analysis revealed that all the eight obesity indices included in the study were able to discriminate MetS [all area under the ROC curves (AUCs) > 0.6, P < 0.05]. LAP showed the highest AUC and according to the maximum Youden indexes, the cut off values for men and women were 27.29 and 36.45, respectively. There was no significant difference in the AUC value between LAP and VAI, BRI/WHtR and BMI in men and between BRI/WHtR and BMI in women. The AUC value for WHtR was equal to that for BRI in identifying MetS. As shown in Table 4, significance tests for comparison of AUCs of WC, BMI, BRI, CI and WHtR were further conducted as their 95% CI were overlapped. Statistical significances were obtained between WC and BMI, BRI, WHtR and CI (all P < 0.001). The differences between CI and BRI, WHtR, WC were also significant in both genders (all P < 0.001). WC showed higher predictive power in assessment of MetS than BRI, WHtR and BMI in both genders (P < 0.05).
ROC curves for different obesity indices as predictors of MetS in men and women. ROC receiver operating characteristic curve, BMI body mass index, WC waist circumference, WHtR waist-to-height ratio, CI conicity index, BRI body roundness index, ABSI a body shape index, LAP lipid accumulation product, VAI visceral adiposity index
Discussion
This is the first study, to the best of our knowledge, to investigate and compare the predictive strength of the eight obesity indices which reflect general (BMI), abdominal (WC, WHtR, CI) and visceral (VAI, LAP, ABSI, BRI) obesity in assessment of MetS among Chinese MHD patients. We found that the eight obesity indices were independently associated with MetS risk even after adjustment for age, sex, educational status and history of smoking. Visceral obesity marker LAP presented the highest discriminant value for MetS in both genders followed by VAI while ABSI followed by CI was the weakest predictor of MetS. WC performed better than WHtR, BRI and BMI for the screening of MetS. BRI could be an alternative obesity measure to WHtR in assessment of MetS.
The present study suggested that LAP was the best predictor of MetS among all the investigated indicators, this was compatible with previous studies [21,22,23]. Together with previous studies, our results further highlighted the usefulness of LAP in predicting MetS across different diseases and different ethnic groups. The AUC equivalent to VAI and LAP did not differ statistically in men. However, the AUC of LAP was higher than that of VAI in women (P < 0.05), which demonstrated that LAP presented better ability to discriminate MetS than VAI only in women. The exact mechanism underlying the gender disparity remains to be elucidated. Different sex hormones might affect the fat distribution. Studies have suggested that postmenopausal females tend to deposit more visceral fat [24], and median age of our female participants were 49–59 year, we could speculate that most of our female participants were menopausal and women in our study were more likely to have visceral obesity as BRI,VAI, LAP were much higher in women than that of men. A previous study from Northeast China had come to a similar conclusion [25].
VAI demonstrated better ability to discriminate MetS than general and central obesity indicators in our study. Consistent with our results, a previous study had confirmed the superiority of VAI compared to WC, WHtR and BMI in predicting MetS [26].
BRI and ABSI have been identified as novel markers of visceral obesity [12, 27]. BRI was found to be a superior measurement for determining the presence of left ventricular hypertrophy compared to BMI, WC and WHtR [28]. Our results demonstrated that though ABSI and BRI were able to identify MetS, ABSI was the weakest predictor of MetS among the eight obesity indices. Furthermore, BRI did not show superior predictive power than WC, WHtR and BMI in assessment of MetS. This finding is consistent with a previous study in Iran [29].
Exact mechanisms accounting for our findings were unknown but the following explanation might be responsible for our results. LAP and VAI are two mathematical models that developed based on the combination of WC and TG, while ABSI, BRI and other obesity indicators did not take TG into consideration. But raised plasma triglycerides are included in the MetS diagnosis criteria. Furthermore, increased visceral fat and serum levels of TG are associated with insulin resistance even in subjects with normal BMI and normal glucose tolerance [30]. Insulin resistance may result in dysglycemia and is associated with hypertension [31]. Thus, indexes considering TG might have a closer relationship with MetS. More studies are needed to determine whether ABSI and BRI could be ideal markers of visceral obesity.
There were several limitations in our study. First, the cross-sectional nature of our study disenabled us to make causal inferences. Second, hypertension in dialysis patients should be defined on the basis of home BP or 44-h ambulatory BP monitoring (ABPM) [32], but we considered the patients with high BP on the basis of intradialytic or pre- or post-dialysis BP. The prevalence of MetS, therefore, might be exaggerated. But most HD patients in our study were receiving antihypertensive therapy, they should be considered to have high BP. Further studies are needed to clarify whether the IDF criteria is suitable for MHD patients. Third, mean age of our subjects were 54.6 ± 16 years, our results and conclusions might be more suitable for middle-aged and elderly Chinese MHD patients and the applicability of these results may be limited for other populations.
Conclusions
Visceral obesity marker LAP followed by VAI presented the highest discriminant value for MetS, while ABSI followed by CI was the weakest predictor of MetS in MHD patients. Considering the simplicity and superiority of LAP in recognizing MetS, we suggest LAP as a useful screening tool to identify individuals at high risk of MetS particularly in middle-aged and elderly Chinese MHD patients.
References
Oda E (2012) Metabolic syndrome: its history, mechanisms, and limitations. Acta Diabetol 49(2):89–95. https://doi.org/10.1007/s00592-011-0309-6
Li R, Li W, Lun Z, Zhang H, Sun Z et al (2016) Prevalence of metabolic syndrome in Mainland China: a meta-analysis of published studies. BMC Public Health 16:296. https://doi.org/10.1186/s12889-016-2870-y
Duong TV, Wong TC, Chen HH, Chen TW, Chen TH et al (2018) The cut-off values of dietary energy intake for determining metabolic syndrome in hemodialysis patients: a clinical cross-sectional study. PLoS One 13(3):e0193742. https://doi.org/10.1371/journal.pone.0193742
Sanguankeo A, Upala S (2018) Metabolic syndrome increases mortality risk in dialysis patients: a systematic review and meta-analysis. Int J Endocrinol Metab 16(2):e61201. https://doi.org/10.5812/ijem.61201
Nevill AM, Stewart AD, Olds T, Duncan MJ (2018) A new waist-to-height ratio predicts abdominal adiposity in adults. Res Sports Med. https://doi.org/10.1080/15438627.2018.1502183
Mamtani MR, Kulkarni HR (2005) Predictive performance of anthropometric indexes of central obesity for the risk of type 2 diabetes. Arch Med Res 36(5):581–589. https://doi.org/10.1016/j.arcmed.2005.03.049
Borel AL, Nazare JA, Smith J, Aschner P, Barter P et al (2015) Visceral, subcutaneous abdominal adiposity and liver fat content distribution in normal glucose tolerance, impaired fasting glucose and/or impaired glucose tolerance. Int J Obes (Lond) 39(3):495–501. https://doi.org/10.1038/ijo.2014.163
Shah RV, Murthy VL, Abbasi SA, Blankstein R, Kwong RY et al (2014) Visceral adiposity and the risk of metabolic syndrome across body mass index: the MESA Study. JACC Cardiovasc Imaging 7(12):1221–1235. https://doi.org/10.1016/j.jcmg.2014.07.017
Cornier MA, Despres JP, Davis N, Grossniklaus DA, Klein S et al (2011) Assessing adiposity: a scientific statement from the American Heart Association. Circulation 124(18):1996–2019. https://doi.org/10.1161/CIR.0b013e318233bc6a
Roriz AK, Passos LC, de Oliveira CC, Eickemberg M, Moreira Pde A et al (2014) Evaluation of the accuracy of anthropometric clinical indicators of visceral fat in adults and elderly. PLoS One 9(7):e103499. https://doi.org/10.1371/journal.pone.0103499
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S et al (2010) Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 33(4):920–922. https://doi.org/10.2337/dc09-1825
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W et al (2013) Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity (Silver Spring) 21(11):2264–2271. https://doi.org/10.1002/oby.20408
Krakauer NY, Krakauer JC (2012) A new body shape index predicts mortality hazard independently of body mass index. PLoS One 7(7):e39504. https://doi.org/10.1371/journal.pone.0039504
Wang H, Liu A, Zhao T, Gong X, Pang T et al (2017) Comparison of anthropometric indices for predicting the risk of metabolic syndrome and its components in Chinese adults: a prospective, longitudinal study. BMJ Open 7(9):e016062. https://doi.org/10.1136/bmjopen-2017-016062
Perona JS, Schmidt-RioValle J, Rueda-Medina B, Correa-Rodriguez M, Gonzalez-Jimenez E (2017) Waist circumference shows the highest predictive value for metabolic syndrome, and waist-to-hip ratio for its components, in Spanish adolescents. Nutr Res 45:38–45. https://doi.org/10.1016/j.nutres.2017.06.007
Zhou C, Peng H, Yuan J, Lin X, Zha Y et al (2018) Visceral, general, abdominal adiposity and atherogenic index of plasma in relatively lean hemodialysis patients. BMC Nephrol 19(1):206. https://doi.org/10.1186/s12882-018-0996-0
El Said HW, Mohamed OM, El Said TW, El Serwi AB (2017) Central obesity and risks of cardiovascular events and mortality in prevalent hemodialysis patients. Int Urol Nephrol 49(7):1251–1260. https://doi.org/10.1007/s11255-017-1568-0
Marcadenti A, Fuchs FD, Moreira LB, Gus M, Fuchs SC (2017) Adiposity phenotypes are associated with type-2 diabetes: LAP index, body adiposity index, and neck circumference. Atherosclerosis 266:145–150. https://doi.org/10.1016/j.atherosclerosis.2017.09.022
Alberti KG, Zimmet P, Shaw J (2006) Metabolic syndrome–a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 23(5):469–480. https://doi.org/10.1111/j.1464-5491.2006.01858.x
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44(3):837–845
Bhat MA, Laway BA, Shah ZA, Wani AI, Mubarik I (2015) Insulin resistance, metabolic syndrome and chronic low grade inflammation in Sheehan’s syndrome on standard replacement therapy: a case control study. Pituitary 18(3):312–318. https://doi.org/10.1007/s11102-014-0575-8
Guo SX, Zhang XH, Zhang JY, He J, Yan YZ et al (2016) Visceral adiposity and anthropometric indicators as screening tools of metabolic syndrome among low income rural adults in Xinjiang. Sci Rep 6:36091. https://doi.org/10.1038/srep36091
Nascimento-Ferreira MV, Rendo-Urteaga T, Vilanova-Campelo RC, Carvalho HB, da Paz Oliveira G et al (2017) The lipid accumulation product is a powerful tool to predict metabolic syndrome in undiagnosed Brazilian adults. Clin Nutr 36(6):1693–1700. https://doi.org/10.1016/j.clnu.2016.12.020
Blaak E (2001) Gender differences in fat metabolism. Curr Opin Clin Nutr Metab Care 4(6):499–502
Dai D, Chang Y, Chen Y, Chen S, Yu S et al (2016) Visceral adiposity index and lipid accumulation product index: two alternate body indices to identify chronic kidney disease among the rural population in Northeast China. Int J Environ Res Public Health 13(12)
Motamed N, Khonsari MR, Rabiee B, Ajdarkosh H, Hemasi GR et al (2017) Discriminatory ability of visceral adiposity index (VAI) in diagnosis of metabolic syndrome: a population based study. Exp Clin Endocrinol Diabetes 125(3):202–207. https://doi.org/10.1055/s-0042-119032
(2016) Indirect measure of visceral adiposity ‘A Body Shape Index’ (ABSI) is associated with arterial stiffness in patients with type 2 diabetes. 4(1):e000188. https://doi.org/10.1136/bmjdrc-2015-000188
Chang Y, Guo X, Li T, Li S, Guo J et al (2016) A body shape index and body roundness index: two new body indices to identify left ventricular hypertrophy among rural populations in Northeast China. Heart Lung Circ 25(4):358–364. https://doi.org/10.1016/j.hlc.2015.08.009
Haghighatdoost F, Sarrafzadegan N, Mohammadifard N, Asgary S, Boshtam M et al (2014) Assessing body shape index as a risk predictor for cardiovascular diseases and metabolic syndrome among Iranian adults. Nutrition 30(6):636–644. https://doi.org/10.1016/j.nut.2013.10.021
Katsuki A, Sumida Y, Urakawa H, Gabazza EC, Murashima S et al (2003) Increased visceral fat and serum levels of triglyceride are associated with insulin resistance in Japanese metabolically obese, normal weight subjects with normal glucose tolerance. Diabetes Care 26(8):2341–2344
Soleimani M (2015) Insulin resistance and hypertension: new insights. Kidney Int 87(3):497–499. https://doi.org/10.1038/ki.2014.392
Sarafidis PA, Persu A, Agarwal R, Burnier M, de Leeuw P et al (2017) Hypertension in dialysis patients: a consensus document by the European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association—European Dialysis and Transplant Association (ERA-EDTA) and the Hypertension and the Kidney working group of the European Society of Hypertension (ESH). J Hypertens 35(4):657–676. https://doi.org/10.1097/HJH.0000000000001283
Acknowledgements
This study was supported by the following Science Foundation: (1) Qian Ke Co LH characters [2016]7151 from Guizhou science and technology plan project; (2) GZSYQN (2016)11.
Author information
Authors and Affiliations
Contributions
CZ and LZ contributed to the design, analysis, and interpretation of the data and drafted the manuscript; YZ provided guidance in the writing of this paper; JY, XT and YP contributed to the acquisition of the data.
Corresponding author
Ethics declarations
Conflict of interest
We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Ethical statement
Ethics Committee of The People’ s Hospital of Guizhou province approved the study. This study was performed fulfilling the principles of Helsinki Declaration.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, C., Zhan, L., Yuan, J. et al. Comparison of visceral, general and central obesity indices in the prediction of metabolic syndrome in maintenance hemodialysis patients. Eat Weight Disord 25, 727–734 (2020). https://doi.org/10.1007/s40519-019-00678-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00678-9