Abstract
Background
Neck circumference (NC) is a relatively unused index of upper body adiposity. The present study aims to analyze the associations of NC with anthropometric measures of obesity, as well as cardiovascular and metabolic risks in Arab women.
Methods
This cross-sectional study included 623 women (aged 18–70 years) recruited from different primary care centers in Riyadh, Saudi Arabia. NC, waist circumference (WC), body mass index (BMI), blood pressure, and metabolic and serological markers were measured in all participants. Covariance and regression analyses were used to evaluate the associations between NC and cardiometabolic risk factors.
Results
The correlation coefficients of NC and WC with the clinical indices were highly significant (p < 0.01). Overall, the NC was positively correlated with all cardiometabolic markers except total cholesterol and LDLc (p < 0.001). Interestingly, NC was associated with cardiometabolic risk factors independent of other anthropometric indices.
Conclusion
NC is significantly and independently associated with cardiometabolic risk factors in Arab women.
Level of evidence
V, cross-sectional descriptive study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity in the Arabian Gulf region is among the highest in the world [1], with an overweight and obesity prevalence among Saudis of 55% [2]. Determining the epidemiology of obesity is important for the development of appropriate interventions and resource allocations for its control [3]. Considering the great economic and human costs associated with obesity, prevention is an urgent need. Management of obesity can aid in preventing cardiometabolic diseases and must be a priority [4]. There are several methods that can be used to diagnose health risks while taking into account increased body fat, such as bioelectrical impedance, dual-energy X-ray absorptiometry (DEXA), total body water [5], and hepatic left lobe volume (HLLV) [6, 7]. However, anthropometry is a simple, fast, and inexpensive way to estimate body fat and fat distribution, making it more practical for large epidemiological studies and primary clinic settings. The most widely used whole body adiposity assessment is body mass index (BMI), calculated as weight (kg)/height (m2). BMI, though, is not a sensitive indicator of either the amount or distribution of body fat [8]. Therefore, other indicators, such as waist circumference (WC), waist/hip ratio (WHR), and neck circumference (NC), have been recommended. WC corresponds to abdominal visceral fat (VF), which is shown to have a major role in cardiometabolic risk [9, 10], yet upper body subcutaneous fat (SF) shown to be related to cardiometabolic risk as much as abdominal VF [11]. In addition, free fatty acid release from upper body SF was found to be greater than lower body [12], further strengthening the significance of measuring upper body subcutaneous adipose tissue depots. NC is an index of upper body SF that correlates with whole body adiposity (BMI) [13], abdominal adiposity (WC and WHR) [14], abdominal VF [11], and the metabolic syndrome (MetS) components, such as systolic blood pressure (SBP) and diastolic blood pressure (DBP), triglycerides (TG), total cholesterol, fasting glucose, and insulin resistance (IR) [15, 16].
The aim of this study was to examine the associations between overall obesity (as measured by BMI) and upper body adiposity (as measured by NC or WC) in Saudi women and to specify the cardiometabolic risk factors that correlated with NC.
Methods
Study population
A cross-sectional survey was conducted at King Khalid University Hospital (KKUH) and primary health care centers in Riyadh, KSA. On the basis of the primary outcome measure of differences in cardiometabolic risks on NC, a sample size of 600 was determined to have 80% power, with a two-tailed significance level of 5% to detect a small effect size. This study was conducted in cooperation with the Biomarkers Research Program (BRP) at King Saud University (KSU), KSA. Data collection was carried out over a period of 18 months, from September 2014 to April 2016, using a total of 623 Saudi women aged 18–70 years. Exclusion criteria were as follows: organ failure, organ transplant, cancer, thyroid disorders, pregnancy, and breastfeeding. The subjects were selected based on systematic random sampling from eligible patients who attended KKUH primary health care centers on the sampling days. The sampling frame was constructed from the daily booking logs of each center. Names and file numbers of Saudi women aged 18–70 years were obtained first thing in the morning. We used the following formula for the systematic sampling: K ≤ N/n, where the population size (N) was the total number of the eligible population (N = total number of Saudi women aged 18–70 years attending the center, N = 4167), and the required sample size (n) was chosen based on the power calculation (n = 600). In order for the systematic sampling to be valid, the first participant was randomly selected, then every K (k = 6) participant in the daily booking logs was selected until the target sample size was achieved. In the case of rejection or if the participant did not meet the study criteria, the immediately adjacent participant was selected.
Data collection
All participants were interviewed using a pre-coded questionnaire, which comprised of five major parts: socio-demographic data, medical history, dietary habits and practices, physical activity, and lifestyle. Participants’ anthropometric measurements and blood test results were also obtained.
Adiposity measurements
The anthropometric measurements were recorded by well-trained healthcare providers according to the Anthropometry Procedures Manual of the National Health and Nutrition Examination Survey [17]. Height was recorded to the nearest 0.5 cm, weight was recorded to the nearest 0.1 kg, and BMI was calculated as weight (kg) divided by height (m) squared. All circumferences were taken using a non-stretch measuring tape, to the nearest 0.5 cm. Waist and hip circumferences were measured over light clothing. WC (cm) was measured at mid-point between the bottom of the rib cage and above the top of the iliac crest. Hip circumference (cm) was measured at the widest point of the buttocks. NC (cm) was measured at the level of the cricoid cartilage, mid-neck height, between the mid-cervical spine and mid-anterior neck, while subject standing with head in Frankfort horizontal plane, and shoulders relaxed, but not hunched [11, 13]. Total body fat percentage (%) was assessed using a DEXA device (model: Prodigy Advance, GE healthcare, Madison, WI, USA).
Clinical and biochemical parameters
Blood pressure was obtained from each participant’s right arm, while she was sitting down, after a minimum rest period of 5 min. The measurements were taken using standardized mercury sphygmomanometers (Diplomat Presameter 660/360; Rudolf Riester GmbH, Jungingen, Germany). The subjects who agreed to participate were scheduled for a second visit to the laboratory at the same clinic within 1 week. They were asked to fast for 10–12 h before blood samples were taken. Samples were analyzed and stored in BRP, College of Science, KSU. For the analysis, all blood and serum samples were placed in plain polystyrene tubes, which were delivered to BRP on the same day and stored at − 20 °C. Fasting blood glucose and lipids [total cholesterol, TG, and high-density lipoprotein cholesterol (HDLc)] were measured using the hexokinase and colorimetric methods, respectively, with a standard chemical analyzer (Konelab, Thermo Fisher Scientific, Vantaa, Finland). The analyzer was recalibrated frequently according to the manufacturer’s instructions. Low-density lipoprotein cholesterol (LDLc) was estimated using the Friedewald equation: total cholesterol−HDLc−(TG/2.2) [18]. Insulin concentrations were determined by the electro-chemiluminescence method (COBAS-E-411; Roche Diagnostics, Mannheim, Germany). Insulin resistance was assessed using a homeostasis model assessment (HOMA-IR): fasting insulin (µU/mL) × fasting plasma glucose (mmol/L)/22.5 [19].
Cardiometabolic risk factors
Cardiometabolic disease biomarkers were defined as follows according to the International Diabetes Federation (IDF) guidelines [20]: central obesity (≥ 80 cm), hypertriglyceridemia (TG ≥ 1·7 mmol/L), low HDLc (< 1.29 mmol/L or specific treatment for this lipid abnormality), hyperglycemia [fasting plasma glucose ≥ 5.6 mmol/L, or previously diagnosed type 2 diabetes mellitus (T2DM)], and hypertension (SBP ≥ 130 mmHg, DBP ≥ 85 mmHg, or treatment for previously diagnosed hypertension). MetS was assessed by the IDF/AHA/NHLBI 2009 consensus criteria [21], as the presence of any three or more of the previously defined risk factors: (1) raised TG; (2) reduced HDLc; (3) raised fasting plasma glucose; (4) raised blood pressure; and (5) central obesity.
Statistical analysis
Statistical analyses were performed using SPSS 22 (IBM Corp., Armonk, NY, USA). Descriptive statistics were applied for all variables. Continuous data were presented as mean ± standard deviation (SD) and median (25–75th) percentiles for variable, following Gaussian and non-Gaussian variables. Categorical variables were presented as frequencies (n) and percentages (%). All continuous variables were checked for normality using the Kolmogorov–Smirnov test, as well as Skewness and Kurtoses (≤ 0.8). If not normal, continuous variables were transformed to log or SQRT transformation, where appropriate. All analyses involving insulin measures (insulin and HOMA-IR) were restricted to participants without diabetes. Correlations were conducted to determine significant associations between variables of interest. The findings were expressed as correlation coefficients and controlled for age, menopausal status, and current estrogen use. NC, WC, WHR, BMI, and Fat% were standardized to a mean of zero and an SD of one to facilitate comparisons of regression coefficients. Linear regression analysis was performed, considering the cardiometabolic risk factors (log fasting glucose, SQRT insulin, SQRT HOMA-IR, SQRT TG, HDLc, LDLc, SBP, and DBP) as dependent variables, as well as considering NC, BMI, WC, WHR, and Fat% as independent variables. All tests were two-sided, and levels of statistical significance were set at p values of < 0.05.
Results
Participants’ characteristics are shown in Table 1. The mean age was 47.3 ± 10.6 years, the mean BMI was 32.5 ± 6.2 kg/m2, and mean NC was 36.3 ± 2.6 cm. At least one cardiometabolic risk factor was present in 94% of the participants. The most prevalent risk factor was abdominal obesity, followed by hyperglycemia and low HDLc levels. Around 70% (69.3%) of the study population had MetS. Nearly one-half of the study population (42.7%) had hypertension, while only 15.7% reported that they had been previously diagnosed with hypertension. Only 0.5% of the subjects had good dietary habits and practices. The total physical activity score showed that 55.5% had poor physical activity and lifestyle, while only 9.8% of the participants reported good physical activity and lifestyle (data not presented, supplemental material).
NC and the other obesity indices
Partial correlations were used to examine associations between NC and Fat%, BMI, WC, and WHR after controlling for the effects of age. BMI showed the highest correlation with WC when compared to other clinical indices (r = 0.70, n = 514, p < 0.001). All NC and WC coefficients were highly significant (p < 0.01) (Table 2).
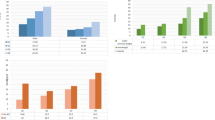
Each BMI subgroup was further divided into three subgroups based on 25th, 25–75th, and 75th percentiles of WC. NC significantly increased from the lower to higher WC subgroups within each BMI subgroup (Fig. 1). Interestingly, none in the normal weight subgroup had a WC above the 75th percentile.
NC and cardiometabolic risk indicators
Table 3 presents the adjusted correlation coefficients for all of the anthropometric indices and the cardiometabolic risk factors. NC and WC were significantly correlated with SBP, DBP, HDLc, TG, insulin, and HOMA-IR (p < 0.001). Compared to fat%, BMI, WC, and WHR, NC had the highest correlation with all cardiometabolic risk factors in all participants, as well as in the overweight and obese groups, but not in the normal group, after stratification (Table 3).
Multivariate regression analyses were used to examine the independent associations between NC and cardiometabolic risk factors. Table 4 illustrates the results of the multivariate regression analyses using each cardiometabolic risk factor as a dependent variable. All covariates listed were entered into the first model. In the second block, the independent variable (NC) was added. NC was associated with all risk factors except LDLc (Model 1). After further adjustment for BMI (Model 2), R2 changes were attenuated for SBP, DBP, HDLc, insulin, and HOMA-IR, but remained significantly associated with all risk factors. An increase in NC of 1 standard deviation (SD) was associated with a 4.87 mmHg increase (p < 0.001) in SBP in the primary model. After adjusting further for BMI (Model 2), the increase in SBP was 4.33 mmHg (p < 0.001) per 1 SD increase in NC. In Model 5, predictive powers (as adjusted R2) were the highest except for insulin and HOMA-IR. However, the R2 change only increased for fasting glucose (R2 change = 0.05, p < 0.001) (Table 4).
Figure 2 shows the interactions between the tertiles of the NC and BMI subgroups (normal, overweight, and obese) on cardiometabolic risk factor levels. Within each BMI subgroup, there was a stepwise increase in the risk factor levels by tertiles of NC. There was no significant interaction between NC and BMI for cardiometabolic risk factors found except for insulin (p = 0.015) and HOMAIR (p = 0.041) (Fig. 2).
Discussion
Our study revealed that NC is significantly associated with BMI (total body adiposity), as well as WHR and WC, which are common surrogate markers of abdominal and upper body fat mass (VF and SF, respectively) [22]. These results were similar to several studies that examined the associations between the conventional anthropometric measures of adiposity and NC [23, 24]. Stabe et al. [25] reported that NC was associated with intra-abdominal fat. Similar to Joshipura et al. [26], our findings revealed that WC has a greater correlation with BMI and Fat% when compared to NC. This may imply that incremental increases in the NC would be highly independent of BMI when compared to WC [26].
Anthropometrics are the most basic tools for assessing the well-established relationship between body fat distribution and metabolic complications. In addition, they are inexpensive and more readily available than computed tomography (CT) and magnetic resonance imaging (MRI) in clinical practice. NC measurements require less effort on the part of the examiner and the subject than other anthropometric methods. NC requires a single measurement site with lesser anatomical and observer variation biases [25]. In addition, NC measurement may be more socially acceptable, convenient and tolerable, especially for overweight and obese women [23]. NC is measured directly on the body surface, which is more stable than the surfaces used to measure WC and HC, as Arab women prefer to be measured on light clothing instead of direct measurement on exposed abdominal area. The use of WC and HC may increase the chances of getting inaccurate measurements. By contrast, NC provides good inter and intra-observer reliability [27]. Moreover, WC risk prediction is influenced by the measurement’s anatomical location, and WC value comparisons are complicated by the absence of generally accepted anatomical landmarks for measuring WC, which can vary, according to the clinical study as follows: the mid-point between the last intercostal arch and iliac crest; the upper border of the iliac crest; the narrowest circumference abdomen; and distance above the umbilicus. Each specific site used to measure WC influences the WC value obtained, which can limit the evaluation of body fat distribution and the corresponding metabolic risks, especially in women [10, 25, 28]. The WC cut-off values for overweight and obesity vary widely throughout the world. WC may also be biased by the absence of specific, standardized cut-off points for certain populations, including those of the Arabian Gulf region. Measuring NC is a straightforward process with minimal cost and time requirements [23]. As a result, NC measurement provides a better and potentially more accurate clinical screening tool for predicting obesity and MetS.
Our study revealed that NC is associated with elevated SBP, DBP, TG, fasting glucose, insulin, and IR, as well as a reduced HDLc levels. These findings are in line with those of Zhou et al. [29]. In contrast, they found that the associations between BMI and WC and cardiometabolic risks were higher than NC and cardiometabolic risks. Moreover, their study included only normal weight (mean BMI = 22.67 ± 3.1 kg/m2) Chinese adults who were not taking any prescribed hypertension, diabetes, or dyslipidemia medications [29]. The data from the San Juan Overweight Adults Longitudinal Study (SOALS), which recruited overweight and obese adults free from previously diagnosed diabetes, showed results consistent with our study [26]; NC revealed higher positive associations with prediabetes and lipid abnormalities than did BMI, WC, and Fat%. Furthermore, the INTERHEART data, a standardized case–control study of 27,098 participants from 52 countries with many ethnic groups, indicated that BMI has a modest relation with the risk of cardiovascular disease and appears to be of no value in Arabs and southern Asian populations; WHR showed the strongest relation in most ethnic groups [30]. The results from a large European cohort study (519,978 participants) showed that WC and WHR were more associated with the risk of death than BMI. However, these associations tend to be stronger in subjects with a lower BMI, compared to those with a higher BMI [31]. In children and adolescents, these anthropometric measures, including NC, showed similar strengths in its associations with continuous MetS [32].
The results of the present study demonstrated clear and consistent positive associations of NC with SBP, DBP, TG, fasting glucose, insulin, and IR. These associations were present in both univariate and multivariate analyses and remained highly significant after adjusting for covariates, similar to other studies [11, 15, 33, 34]. Among Brazilian women, NC was associated with hypertension, insulin insensitivity, hypertriglyceridemia, lower HDLc, and higher fasting glucose level. NC also significantly correlated with intima–media thickness of common or internal carotid arteries, a direct measure of subclinical atherosclerosis, independent of BMI and WC [35].
Our data and results from other studies suggested that NC contributes to the cardiometabolic consequences as an upper body fat marker [33, 34]. Upper body SF, as measured by NC, may confer risk beyond visceral adiposity [11, 29]. Changes in regional fat distribution, including SF of the neck, are associated with adipose tissue dysfunction and abnormal adipokine secretion leading to metabolic diseases [14, 15]. Upper body fat is more lipolytically active than lower body adipose tissue, which is mechanism to explain the associations of NC with cardiometabolic risk. Upper body SF is responsible for a larger proportion of systemic free fatty acid release than is VF, specifically in obese individuals [12, 36]. This lipolytic activity of upper body fat and high levels of plasma free fatty acids could result in IR [36], increased VLDL-triglyceride production [37], oxidative stress [38], and the development of hypertension. Therefore, NC, as representative of upper body fat, should be able to predict metabolic and cardiovascular risks [25, 34, 36]. NC’s predictive value in identifying cardiometabolic risk has also been confirmed in a recent meta-analysis of Ataie-Jafari and colleagues [39].
Our study has some limitations. The cross-sectional nature of this study prevents causal conclusions. Second, we used DEXA scan to quantify fat%; other methods, such as CT scan, may quantify upper body fat better. Despite these limitations, our study does have the advantage of being the first study to examine the association between NC and cardiometabolic risk factors in the Arabian Gulf region.
In summary, NC is a very efficient marker of obesity and cardiometabolic risk among Arab women independent of other conventional anthropometric indices. Community-based, prospective cohort studies at a national level are needed to determine whether NC is an important risk factor for the development of cardiometabolic conditions.
References
Hnoosh A, Vega-Hernández G, Jugrin A, Todorova L (2012) Direct medical costs of diabetes-related complications in Saudi Arabia. Value Health 15:A178. https://doi.org/10.1016/j.jval.2012.03.966
Memish ZA, El Bcheraoui C, Tuffaha M et al (2014) Obesity and associated factors—Kingdom of Saudi Arabia, 2013. Prev Chronic Dis 11:E174. https://doi.org/10.5888/pcd11.140236
Alnuaim A (2014) Rising prevalence of diabetes mellitus in Saudi Arabia: cause for concern and call for urgent control program. Ann Saudi Med 34(6):463–464. https://doi.org/10.5144/0256-4947.2014.463
Fast facts: obesity—a global problem (2016) http://www.fastfacts.com/_files/ff%20obesity%20a%20global%20problem.pdf. Accessed 14 Feb 2016
Loan MV (1998) Skinfolds, circumferences, and bioimpedance. In: St. Jeor ST (ed) Obesity assessment tools, methods, interpretations. International Thomson Publishing, New York, pp 68–82
Busetto L, Tregnaghi A, De Marchi F, Segato G, Foletto M, Serqi G et al (2002) Liver volume and visceral obesity in women with hepatic steatosis undergoing gastric banding. Obes Res 10(5):408–411. https://doi.org/10.1038/oby.2002.56
Giannetti M, Piaggi P, Ceccarini G, Mazzeo S, Querci G, Fierabracci P et al (2012) Hepatic left lobe volume is a sensitive index of metabolic improvement in obese women after gastric banding. Int J Obes (Lond) 36:336–341. https://doi.org/10.1038/ijo.2011.243
Seidell JC, Flegal KM (1997) Assessment and classification of overweight and obesity. Br Med Bull 53(2):238–252
Preis SR, Massaro JM, Robins SJ et al (2010) Abdominal subcutaneous and visceral adipose tissue and insulin resistance in the Framingham heart study. Obes (Silver Spring) 18:2191–2198. https://doi.org/10.1038/oby.2010.59
Klein S, Allison DB, Heymsfield SB et al (2007) Waist circumference and cardiometabolic risk: a consensus statement from Shaping America’s Health: Association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Obes (Silver Spring) 15:1061–1067. https://doi.org/10.1038/oby.2007.632
Preis SR, Massaro JM, Hoffmann U et al (2010) Neck circumference as a novel measure of cardiometabolic risk: the Framingham Heart study. J Clin Endocrinol Metab 95:3701–3710. https://doi.org/10.1210/jc.2009-1779
Jensen MD (1997) Lipolysis: contribution from regional fat. Annu Rev Nutr 17:127–139
Ben-Noun L, Sohar E, Laor A (2001) Neck circumference as a simple screening measure for identifying overweight and obese patients. Obes Res 9:470–477. https://doi.org/10.1542/peds.2010-0242
Onat A, Hergenc G, Yuksel H, Can G, Ayhan E, Kaya Z, Dursunoglu D (2009) Neck circumference as a measure of central obesity: associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin Nutr 28:46–51. https://doi.org/10.1016/j.clnu.2008.10.006
Ben-Noun L, Laor A (2003) Relationship of neck circumference to cardiovascular risk factors. Obes Res 11(2):226–231. https://doi.org/10.1038/oby.2003.35
Sjostrom CD, Håkangård AC, Lissner L, Sjostrom L (1995) Body compartment and subcutaneous adipose tissue distribution risk factor patterns in obese subjects. Obes Res 3:9–22
The National Health and Nutrition Examination Survey (2002) Anthropometry procedures manual. https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Bonora E, Formentini G, Calcaterra F et al (2002) HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects prospective data from the Verona Diabetes Complications Study. Diabetes Care 25:1135–1141. https://doi.org/10.2337/diacare.25.7.1135
Alberti KG, Zimmet P, Shaw J. IDF Epidemiology Task Force Consensus Group (2005) The metabolic syndrome: a new worldwide definition. Lancet 366:1059–1062. https://doi.org/10.1016/S0140-6736(05)67402-8
Alberti KGMM, Eckel RH, Grundy SM et al (2009) Harmonizing the Metabolic Syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society and International Association for the Study of Obesity. Circulation 120(16):1640–1645. https://doi.org/10.1161/CIRCULATIONAHA.109.192644
Ross R, Freeman J, Hudson R et al (2002) Abdominal obesity, muscle composition and insulin resistance in premenopausal women. J Clin Endocrinol Metab 87:5044–5051. https://doi.org/10.1210/jc.2002-020570
Aswathappa J, Garg S, Kutty K, Shankar V (2014) Utility of neck circumference, a simple and novel measure as anthropometric marker of obesity in adults. World J Pharm Pharm Sci 3(3):1618–1629
Hingorjo MR, Qureshi MA, Mehdi A (2012) Neck circumference as a useful marker of obesity: a comparison with body mass index and waist circumference. J Pak Med Assoc 62(1):36–40
Stabe C, Vasques ACJ, Lima MMO et al (2013) Neck circumference as a simple tool for identifying the metabolic syndrome and insulin resistance: results from the Brazilian Metabolic Syndrome Study. Clin Endocrinol (Oxf) 78(6):874–881. https://doi.org/10.1111/j.1365-2265.2012.04487.x
Joshipura K, Muñoz-Torres F, Vergara J, Palacios C, Pérez C (2016) Neck circumference may be a better alternative to standard anthropometric measures. J Diabetes Res 2016:6058916. https://doi.org/10.1155/2016/6058916
LaBerge RC, Vaccani JP, Gow RM, Gaboury I, Hoey L, Katz SL (2009) Inter- and intra-rater reliability of neck circumference measurements in children. Pediatr Pulmonol 44:64–69. https://doi.org/10.1002/ppul.20944
Wang J, Thornton JC, Bari S et al (2003) Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutr 77:379–384. https://doi.org/10.1093/ajcn/77.2.379
Zhou JY, Ge H, Zhu MF et al (2013) Neck circumference as an independent predictive contributor to cardio-metabolic syndrome. Cardiovasc Diabetol 12:76. https://doi.org/10.1186/1475-2840-12-76
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P et al (2005) Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet 366:1640–1649. https://doi.org/10.1016/S0140-6736(05)67663-5
Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K et al (2008) General and abdominal adiposity and risk of death in Europe. N Engl J Med 359:2105–2120. https://doi.org/10.1056/NEJMoa0801891
Ejtahed HS, Qorbani M, Motlagh ME, Angoorani P, Hasani-Ranjbar S, Ziaodini H et al (2018) Association of anthropometric indices with continuous metabolic syndrome in children and adolescents: the CASPIAN-V study. Eat Weight Disord 23(5):597–604. https://doi.org/10.1007/s40519-017-0455-0
Kumar NV, Ismail MH, Mahesha P, Girish M, Tripathy M (2014) Neck circumference and cardio- metabolic syndrome. J Clin Diagn Res 8(7):MC23–MC25. https://doi.org/10.7860/JCDR/2014/8455.4641
Yan Q, Sun D, Li X et al (2014) Neck circumference is a valuable tool for identifying metabolic syndrome and obesity in Chinese elder subjects: a community-based study. Diabetes Metab Res Rev 30:69–76. https://doi.org/10.1002/dmrr.2464
Rosenquist KJ, Massaro JM, Pencina KM et al (2013) Neck circumference, carotid wall intima-media thickness, and incident stroke. Diabetes Care 36(9):e153–e154. https://doi.org/10.2337/dc13-0379
Ferrannini E, Haffner SM, Mitchell BD et al (1991) Hyperinsulinemia: the key feature of a cardiovascular and metabolic syndrome. Diabetologia 34:416–422
Martin ML, Jensen MD (1991) Effects of body fat distribution on regional lipolysis in obesity. J Clin Invest 88:609–613
Kissebah AH, Alfarsi S, Adams PW, Wynn V (1976) Role of insulin resistance in adipose tissue and liver in the pathogenesis of endogenous hypertriglyceridaemia in man. Diabetologia 12:563–571
Ataie-Jafari A, Namazi N, Djalalinia S, Chaghamirzayi P, Abdar ME, Zadehe SS et al (2018) Neck circumference and its association with cardiometabolic risk factors: a systematic review and meta-analysis. Diabetol Metab Syndr 10:72. https://doi.org/10.1186/s13098-018-0373-y
Acknowledgements
The authors are grateful to Malak Nawaz Khan Khattak for the statistical analysis.
Funding
The study was funded by the Deanship of Scientific Research, Chair for Biomarkers of Chronic Diseases, Biochemistry Department, College of Science, King Saud University, Riyadh, 11421, Saudi Arabia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The research protocol and the consent documents were approved by the Ethics Committee of KSU, in Riyadh, KSA (No. 429679/67/4) and the University of Maryland College Park Institutional Review Board (IRB) (No. 411873-4).
Informed consent
All subjects gave their informed consent after we provided a full explanation of the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Albassam, R.S., Lei, K.Y., Alnaami, A.M. et al. Correlations of neck circumference with body composition and cardiometabolic risk factors in Arab women. Eat Weight Disord 24, 1121–1130 (2019). https://doi.org/10.1007/s40519-018-0630-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-018-0630-y