Abstract
Purpose
Age, gender and body mass index (BMI) are commonly described risk factors for the development of eating disorders. However, the magnitude of these factors (individually and together) is still not well-defined in some populations.
Methods
A systematic search was performed for studies that reported the prevalence of eating disorder risk among medical students using the Eating Attitudes Test-26 (EAT-26) and age, gender and BMI as risk factors. We included studies published in English peer-reviewed journals between 1982 and 2017. A total of 14 studies were included in the analyses, and the meta-regression analyses were performed using mean age (years), gender (proportion of female subjects), and mean BMI (kg/m2) as moderators with the risk of eating disorders measured using EAT-26 as an outcome variable. Four interaction terms were created (1) age × gender (2) age × BMI (3) gender × BMI and (4) age × gender × BMI to assess if two or more independent variables simultaneously influence the outcome variable.
Results
Utilizing the EAT-26, the pooled prevalence of at risk for eating disorders among medical students (k = 14, N = 3520) was 10.5% (95% CI 7.3–13.7%). Meta-regression model of age, gender and BMI alone revealed poor predictive capabilities. Meta-regression model of age × gender × BMI interaction revealed statistically significant results with a covariate coefficient of 0.001 and p value of 0.044.
Conclusion
Results from this sample of medical students provided evidence for the role of interactions between risk factors (e.g., age × gender × BMI) in predicting individuals at risk for eating disorders, whereas these variables individually failed to predict eating disorders.
Level of evidence
Level I, systematic review and meta-analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eating disorders are complex and very serious psychiatric illnesses that emerge from the interaction of a number of biological (e.g., physical maturation, genetic vulnerabilities, temperament, status such as overweight or obese), psychological (e.g., overvaluation of weight and shape), and environmental factors (e.g., developmental stressors, sexual assault, sexual objectification) [1,2,3]. Prevention and treatment programs designed to reduce the incidence and impact of eating disorders would certainly benefit from increased knowledge about these risk factors [3,4,5]. The working definition of a ‘risk factor’ in this review refers to a quantifiable property that is significantly correlated with and precedes the onset of a disorder [6]. ‘Modifiable’ risk factors (e.g., stress, glorification of the thin ideal) are those that can change spontaneously or be modified by an intervention, and are therefore the most relevant for prevention or early intervention [3, 7]. On the other hand, ‘non-modifiable’ risk factors (e.g., age) cannot be changed, although variables associated with them (e.g., stressors within developmental transitions; see below) might as well be malleable. If a preventive intervention significantly reduces or eliminates a risk factor and thus obviates or delays the onset of an eating disorder, then that variable (e.g., internalization of the thin beauty ideal) can be designated as a ‘causal risk factor’ [7, 8].
This review highlights current knowledge of some of the factors that likely put medical students in particular “at risk” for eating disorders. The main focus will be on age, gender, and body mass index (BMI) = [weight in kilograms/(height in meters)2]. The documented range for age of onset is quite large, perhaps from 8 until 70 years [9, 10]. However, the best available knowledge suggests that eating disorders typically manifest during adolescence or early adulthood, with a reported range of modal ages of onset between 12 and 22 years [11, 12]. It is therefore very likely that the transition in and out of adolescence is associated with a greater risk for eating disorders. Epidemiological studies have shown that gender differences exist between males and females, and the extent of the difference depends on the specific eating disorder symptomatology under discussion. For example, anorexia nervosa and bulimia nervosa are significantly more common in women than men, while binge eating disorder is generally comparable in women and men [13].
Overweight is also one of the risk factors for development and maintenance of eating disorders [14, 15]. A possible explanation is that overweight or obese persons internalize weight-based stigma originating from multiple sources and thus may have greater concerns about body image and a greater investment in weight loss, both of which lead them to exhibit more unhealthy weight and shape control efforts compared to their normal weight peers [14, 16]. Several studies have highlighted the association between both body dissatisfaction and elevated weight and shape concern and the risk of eating disorders, particularly in adolescents and young adults [3, 14, 17].
The literature has identified medical students as a high-risk group for several mental health problems, including eating disorders. Point prevalence estimates of the risk of eating disorders vary between studies, ranging from 2% (below the general population prevalence) to 30% [18, 19]. A recent systematic review and meta-analysis showed that in general one out of ten medical students is at risk for developing eating disorders [20], which is consistent with the estimate of approximately 10% for the population of people of the same age [21,22,23]. The same review also showed women medical students are at greater risk than their male counterparts. However, the exact association between risk of eating disorders, as determined by a valid screening instrument, and known risk factors for the development of these disorders remains unclear, particularly for university students. Accordingly, this meta-regression analysis aimed at studying the association between the risk of eating disorders in medical students and the risk factors of age, gender and body mass index. Based on previous research with other groups, we hypothesized that in medical students the status of at risk for eating disorders would be associated with female gender, younger age and higher BMI.
Methods
The methodology of this meta-regression analysis was guided by the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement [24].
Databases searches
An electronic database search was performed independently by three researchers using EMBASE, MEDLINE, ProQuest and Google Scholar for published literature. The research team developed a list of search strategies, including the following combination of keywords: medical students AND eating disorder(s) OR feeding disorder(s) OR eating problem(s) OR eating attitude(s) OR eating behavior(s). The reference sections of the identified papers were then individually screened by the researchers to identify more articles for potential inclusion in the review.
Inclusion criteria
Inclusion criteria were: (1) the full text is published in the English language, (2) published between January 1982 to December 2017, (3) assessed medical students as a target population, (4) reported disordered eating risk using the Eating Attitude Test-26 (EAT-26), and (5) described at least two of the independent variables (age, gender and BMI) that could be used in the regression analysis.
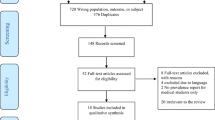
The review team independently screened titles and abstracts and assessed studies for eligibility criteria (see Fig. 1). Two members performed the initial data coding, which was later verified by third review member. Any conflicts in study appropriateness for inclusion in the review were resolved through dialogue with the senior reviewer/expert clinician and panel consensus. To standardize data extraction, the review team agreed to collect the following variables: study characteristic (e.g., name, year, sample size, country), participant characteristics (e.g., age, gender, BMI), and the main findings of the prevalence of eating disorders risk according to EAT-26.
Flow diagram of study inclusion. *See Jahrami et al. [20]
Data synthesis and statistical analyses
The prime purpose of this statistical review was to examine, across multiple studies, the strength of association between the presence or absence of eating disorders in medical students and the risk factors of age, gender, and body mass index. Meta-regression analysis [25], using a random effects model, was performed using mean age (years), gender (proportion of female subjects), and mean BMI (kg/m2) as moderators (i.e., independent or predictor variables), and the risk of eating disorders measured using continuous scores on the EAT-26 as the basis for a dichotomous outcome variable. Specifically, the prevalence of high risk for eating disorders was estimated for statistical modeling using the number of cases that screened positive using an EAT-26 score of ≥ 20 [26], adjusted for the total sample size. The EAT-26 at the cutoff point of 20 has a sensitivity value of 88.1% and a specificity value of 96.1% [27].
To examine whether two or more independent variables simultaneously predicted the outcome variable, four statistical interaction variables were created and each was tested in a separate model. These were (1) age × gender, (2) age × BMI, (3) gender × BMI, and (4) age × gender × BMI. It is common to include interaction terms in the model only if the corresponding main effects are also included, but reporting models with interaction terms only is justified in some instances [28]. To illustrate, here we reasoned that being female with a specific age and BMI profile may be important from research and clinical perspectives, whereas either fact alone is of little or no importance.
All meta-analyses were performed using OpenMetaAnalyst software provided by the Centre for Evidence Synthesis in Health/Center for Evidence-Based Medicine, The School of Public Health, Brown University [29]. Other descriptive statistical analyses were performed using STATA 14.0 [30].
Ethical considerations
Because this review assessed data from published articles that are indexed and available in the public domain, neither ethical approval nor informed consent was applicable or necessary.
Results
Study characteristics
Fourteen studies, involving a total of 3520 respondents from six countries, met the inclusion criteria for the current investigation [18, 19, 31,32,33,34,35,36,37,38,39,40,41]. A systematic summary of the selected characteristics of those studies is presented in Table 1. The median number of respondents per study was 223 (range 75–500). The median age (of the distribution of means across studies) of the respondents was 20 years (range 19–23 years), and the median BMI (of the distribution of mean BMI for each study) was 21 kg/m2 (range 20–23 kg/m2). Approximately, 75% of the respondents self-identified as female, and four studies included only females. Among these medical students, the pooled prevalence of those at risk for eating disorders was 10.5% (95% CI 7.3–13.7%), I2 = 94, τ2 = 0.003, Q = 0.001.
Risk factors of individuals identified ‘at risk’ for eating disorders
Meta-regression analysis revealed that, individually, the potential risk factor variables of age, gender and BMI do not appear to account for individual differences in the development of an eating disorder (see Table 2, see Figs. 2, 3, 4).
When interaction variables were examined (see Table 2), there was a significant finding for age × gender × BMI interaction, with a covariate coefficient 0.001 (95% CI 0.0001–0.001), omnibus p value = 0.044 (Fig. 5). For female subjects, the combination of either (or both) higher age and high BMI predicted a higher risk of an eating disorder, whereas for males of age- and BMI- matched the risk remains lower. There was a statistical trend toward an age × gender interaction, with a covariate coefficient of 0.008 (95% CI − 0.001 to 0.016), omnibus p value = 0.068 (Fig. 6). There was another statistical trend toward gender × BMI interaction, with a covariate coefficient of 0.011 (95% CI − 0.001 to 0.022), omnibus p value = 0.051 (Fig. 7). Then, age × BMI interaction failed to predict the risk of eating disorders, omnibus p value = 0.275 (Fig. 8).
Although the small beta coefficients appear negligible in absolute terms, their effects retain their true value. That is, the size of these coefficients can be explained by the fact that they are largely scale dependent. This is seen in the model involving the age × gender × BMI interaction. The computed beta coefficient for the interaction term is 0.001. Therefore, a population of medical students that is 50% female and has a mean age of 20 years and a mean BMI of 20 kg/m2 will yield a 14% of risk of eating disorders after correcting for intercept, because 0.001 × (20 × 0.5 × 20) − 0.06 = 0.14.
Discussion
In the present study, the risk of eating disorders among medical students in the six countries for which data were available was similar to those previously reported by other university students in the same or similar countries [21,22,23]. The primary outcome of this investigation was that individual differences in age or gender or BMI alone do not appear to be significant predictors of high risk for eating disorders. However, the age × gender × BMI interaction, the gender × BMI interaction, and the age × gender interaction were successful predictors of high risk for development of eating disorders.
The association between the risk of eating disorders (particularly binge eating-related disorders) and BMI has been previously reported by numerous studies [42, 43]. Based on the literature, we initially thought that BMI is among a group of risk factors that appear to be specific for the development of eating disorders, such as body shape, weight concerns, dietary restraint, and positive family history of eating disorders [3, 8]. Thus, in our analysis the failure of BMI in predicting eating disorders was unexpected. Our results suggest that the relationship between BMI and eating disorders is mediated by other factors, perhaps internalized weight stigma and fear of fat, that motivate unhealthy weight control behaviors. This finding needs replication, because the range of mean BMIs in the studies reviewed here was extremely truncated.
The interaction between age × gender × BMI also points to the importance of looking at developmental paths to eating disorders. Furthermore, these risk factors seem to be correlated and have a cumulative effect [1, 3, 44, 45]. For example, it is likely that, as women go through puberty, have babies, grow older, go through menopause, etc., their actual BMI and perceived (over)weight status increase. Smolak and Levine’s model of the developmental psychopathology of eating disorders states that, in the context of (a) cultural obsessions with slenderness, sexiness, and youth, (b) weight-based stigma, and (c) striving for success in a competitive, demanding occupation that is androcentric and that allows precious little time for self-care, increases in BMI and perceived overweight cause women in medical school to have higher levels of body dissatisfaction and to feel more pressure, than age-matched men (male gender) to lose weight [46]. Future studies should examine the proposition that, in the presence of these multiple and normative stressors, medical students’ investment in increased weight control measures might include use of harmful and unhealthy weight control behaviors, thereby increasing the risk for eating disorders.
The key issue here for future prevention and intervention programs is to identify the general and specific risk factors for eating disorders, for eating disorders with comorbid conditions (e.g., depression), and for those comorbid conditions (e.g., depression) in the absence of eating disorders, and then to subdivide both the general risk factors for psychopathology and the specific risk categories into modifiable vs non-modifiable risk factors. Ideally, prevention and intervention programs should focus on specific and modifiable risk factors. The findings of this meta-regression clearly highlight that different risk factors interact with each other to produce an effect. It is noteworthy that, although gender and age are basically fixed and BMI is very difficult to modify in a sustained manner, gender roles and standards of attractiveness are modifiable, are expectations for and support for developmental tasks [46]. Similarly, the cultural, social, and personal meanings of weight need to change, as they have been shown to be key facets of eating disorders and obesity as public health problems [47]. In this regard, the nature and management of contextual stressors presented by medical school have recently received a great deal of attention [48, 49].
Limitations
The limitations of this meta-analytic review are very important to consider when interpreting the results. First, the findings need to be replicated with larger and more diverse samples of medical students. Second, because this review focused on medical students as a population, in the absence of other meta-analyses the results may not be generalize to other populations, (including university graduate students in general or people in similar competitive, high stress circumstances), such as students in elite dance schools. Larger meta-analyses (e.g., including multiple populations that vary in age, culture, context, etc.) are needed to produce results that are more generalizable and more clinically useful in a broad sense. Inclusion in future studies of non-English language research papers and unpublished work will give further insight into the topic. Third, the risk factors in this review were minimal due to the limited availability of adequate information in the original articles. Researchers conducting future cross-sectional and prospective studies are encouraged to include more demographic information and to give more attention to risk factors that are specific to eating disorders, such as overinvestment in weight and shape, thin ideal internalization, dieting, and body dissatisfaction.
Fourth, it is well-known that meta-analyses are an attractive form of review, because the increased statistical power of aggregate level data provides a closer estimate of the ‘true’ population effect size. In this regard, meta-regression can identify trends in the available data not revealed in the original studies. However, confidence in the outcomes of a meta-analysis is completely dependent on the quality of the data in the studies being reviewed. Some experts have pointed out that the overdependence on cross-sectional data from ‘patient’ samples in epidemiological studies investigating the risk factors of eating disorders has played a significant role in limiting our ability to distinguish risk factors from correlates or consequences of illness. Development of multivariate models based on longitudinal data from community-based samples, age-specific samples (e.g., high school or university age students), or context-specific groups (e.g., medical students, elite athletes, dancers) offers more insight than even data obtained from well-designed, case–control studies of specialty clinic-based samples [44, 50].
Conclusion
In conclusion, results from this sample of studies of medical students provided evidence for the role of interactions between risk factors (i.e., age × gender × BMI) in predicting medical students at risk for eating disorders. Future prospective studies are needed to uncover the interactive nature of these risk factors and to use the findings to construct prevention and treatment programs to improve the outcomes of individuals at risk for or with eating disorders.
References
Mazzeo SE, Bulik CM (2009) Environmental and genetic risk factors for eating disorders: what the clinician needs to know. Child Adolesc Psychiatr Clin N Am 18:67–82. https://doi.org/10.1016/j.chc.2008.07.003
Hilbert A, Pike K, Goldschmidt A et al (2014) Risk factors across the eating disorders. Psychiatry Res 220:500–506. https://doi.org/10.1016/j.psychres.2014.05.054
Jacobi C, Hayward C, de Zwaan M et al (2004) Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull 130:19–65. https://doi.org/10.1037/0033-2909.130.1.19
Bratland-Sanda S, Sundgot-Borgen J (2013) Eating disorders in athletes: overview of prevalence, risk factors and recommendations for prevention and treatment. Eur J Sport Sci 13:499–508. https://doi.org/10.1080/17461391.2012.740504
Levine MP (2017) Universal prevention of eating disorders: a concept analysis. Eat Behav 25:4–8. https://doi.org/10.1016/j.eatbeh.2016.10.011
Herzog DB, Eddy KT (2009) Eating disorders: what are the risks? J Am Acad Child Adolesc Psychiatry 48:782–783. https://doi.org/10.1097/CHI.0b013e3181aa03d7
Stice E (2002) Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull 128:825–848
Stice E, Marti CN, Rohde P (2013) Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J Abnorm Psychol 122:445–457. https://doi.org/10.1037/a0030679
Peebles R, Wilson JL, Lock JD (2006) How do children with eating disorders differ from adolescents with eating disorders at initial evaluation? J Adolesc Health Off Publ Soc Adolesc Med 39:800–805. https://doi.org/10.1016/j.jadohealth.2006.05.013
Zayed M, Garry JP (2017) Geriatric anorexia nervosa. J Am Board Fam Med 30:666–669. https://doi.org/10.3122/jabfm.2017.05.170182
Smink FRE, van Hoeken D, Hoek HW (2012) Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 14:406–414. https://doi.org/10.1007/s11920-012-0282-y
Micali N, Solmi F, Horton NJ et al (2015) Adolescent eating disorders predict psychiatric, high-risk behaviors and weight outcomes in young adulthood. J Am Acad Child Adolesc Psychiatry 54:652–659.e1. https://doi.org/10.1016/j.jaac.2015.05.009
Striegel-Moore RH, Rosselli F, Perrin N et al (2009) Gender difference in the prevalence of eating disorder symptoms. Int J Eat Disord 42:471–474. https://doi.org/10.1002/eat.20625
Fan Y, Li Y, Liu A et al (2010) Associations between body mass index, weight control concerns and behaviors, and eating disorder symptoms among non-clinical Chinese adolescents. BMC Public Health 10:314. https://doi.org/10.1186/1471-2458-10-314
Haines J, Neumark-Sztainer D (2006) Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res 21:770–782. https://doi.org/10.1093/her/cyl094
Burrows A, Cooper M (2002) Possible risk factors in the development of eating disorders in overweight pre-adolescent girls. Int J Obes 26:1268–1273. https://doi.org/10.1038/sj.ijo.0802033
Stice E, Shaw H, Marti CN (2007) A meta-analytic review of eating disorder prevention programs: encouraging findings. Annu Rev Clin Psychol 3:207–231. https://doi.org/10.1146/annurev.clinpsy.3.022806.091447
Liao Y, Knoesen NP, Castle DJ et al (2010) Symptoms of disordered eating, body shape, and mood concerns in male and female Chinese medical students. Compr Psychiatry 51:516–523. https://doi.org/10.1016/j.comppsych.2009.11.007
Shashank J, Praveen G, Chethan T (2016) A crosssectional study to asses the eating disorder among female medical students in a rural medical college of Karnataka state. Natl J Community Med 7:524–527
Jahrami H, Sater M, Abdulla A et al (2018) Eating disorders risk among medical students: a global systematic review and meta-analysis. Eat Weight Disord. https://doi.org/10.1007/s40519-018-0516-z
Naeimi AF, Haghighian HK, Gargari BP et al (2016) Eating disorders risk and its relation to self-esteem and body image in Iranian university students of medical sciences. Eat Weight Disord 21:597–605. https://doi.org/10.1007/s40519-016-0283-7
Pengpid S, Peltzer K (2018) Risk of disordered eating attitudes and its relation to mental health among university students in ASEAN. Eat Weight Disord. https://doi.org/10.1007/s40519-018-0507-0
Yu Z, Tan M (2016) Disordered eating behaviors and food addiction among nutrition major college students. Nutrients. https://doi.org/10.3390/nu8110673
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Med 6:e1000100. https://doi.org/10.1371/journal.pmed.1000100
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2011) Introduction to meta-analysis. Wiley, Oxford
Garner DM, Olmsted MP, Bohr Y, Garfinkel PE (1982) The eating attitudes test: psychometric features and clinical correlates. Psychol Med 12:871–878
Mann AH, Wakeling A, Wood K et al (1983) Screening for abnormal eating attitudes and psychiatric morbidity in an unselected population of 15-year-old schoolgirls. Psychol Med 13:573–580. https://doi.org/10.1017/S0033291700047991
Cleves M, Gould W, Gould WW et al (2008) An introduction to survival analysis using Stata, 2nd edn. Stata, College station
OpenMeta[Analyst]—CEBM @ Brown. http://www.cebm.brown.edu/openmeta/index.html. Accessed 26 Jan 2018
Stata MP (2015) 14.0. Coll Stn TX StataCorp
Szweda S, Thorne P (2002) The prevalence of eating disorders in female health care students. Occup Med Oxf Engl 52:113–119
Babar N, Alam M, Ali SS et al (2002) Anorexic behaviour and attitudes among female medical and nursing students at a private university hospital. JPMA 52:272–276
Memon AA, Adil SE-E-R, Siddiqui EU et al (2012) Eating disorders in medical students of Karachi, Pakistan—a cross-sectional study. BMC Res Notes 5:84. https://doi.org/10.1186/1756-0500-5-84
Liao Y, Liu T, Cheng Y et al (2013) Changes in eating attitudes, eating disorders and body weight in Chinese medical university students. Int J Soc Psychiatry 59:578–585. https://doi.org/10.1177/0020764012445862
Alberton VC, Dal-Bó MJ, Piovezan AP, Silva RM da (2013) Abnormal eating behaviors among medical students at a university in southern Santa Catarina, Brazil. Rev Bras Educ Médica 37:15–20. https://doi.org/10.1590/S0100-55022013000100003
Bosi MLM, Nogueira JAD, Alencar CH, Moreira JA (2016) Body image and eating behavior among medical students: eating disorders among medical students. Epidemiol Open Access 6:1–4. https://doi.org/10.4172/2161-1165.1000256
Manaf NA, Saravanan C, Zuhrah B (2016) The prevalence and inter-relationship of negative body image perception, depression and susceptibility to eating disorders among female medical undergraduate students. JCDR 10:VC01–VC04. https://doi.org/10.7860/JCDR/2016/16678.7341
Haroon S, Usman M, Hafeez M (2016) Eating disorders in medical students of Islamabad Pakistan-a cross-sectional study. Ophthalmol Update 1993–2863:89–92
Gupta N, Bhargava R, Chavan BS, Sharan P (2017) Eating attitudes and body shape concerns among medical students in Chandigarh. Indian J Soc Psychiatry 33:219. https://doi.org/10.4103/0971-9962.214605
Vijayalakshmi P, Thimmaiah R, Reddy SSN et al (2017) Gender differences in body mass index, body weight perception, weight satisfaction, disordered eating and weight control strategies among indian medical and nursing undergraduates. Investig Educ En Enferm 35:276–284. https://doi.org/10.17533/udea.iee.v35n3a04
Ngan SW, Chern BCK, Rajarathnam DD et al (2017) The relationship between eating disorders and stress among medical undergraduate: a cross-sectional study. Open J Epidemiol 07:85. https://doi.org/10.4236/ojepi.2017.72008
Guss JL, Kissileff HR, Devlin MJ et al (2002) Binge size increases with body mass index in women with binge-eating disorder. Obes Res 10:1021–1029. https://doi.org/10.1038/oby.2002.139
Marzilli E, Cerniglia L, Cimino S (2018) A narrative review of binge eating disorder in adolescence: prevalence, impact, and psychological treatment strategies. Adolesc Health Med Ther 9:17–30. https://doi.org/10.2147/AHMT.S148050
Stice E, Desjardins CD (2018) Interactions between risk factors in the prediction of onset of eating disorders: exploratory hypothesis generating analyses. Behav Res Ther 105:52–62. https://doi.org/10.1016/j.brat.2018.03.005
Levine M, Murnen S (2009) “Everybody knows that mass media are/are not [pick one] a cause of eating disorders”: a critical review of evidence for a causal link between media, negative body image, and disordered eating in females. J Soc Clin Psychol 28:9–42. https://doi.org/10.1521/jscp.2009.28.1.9
Smolak L, Levine M (1996) Developmental transitions at middle school and college. In: Smolak L, Levine MP, Striegel-Moore R (eds) The developmental psychopathology of eating disorders: implications for research, prevention, and treatment. Lawrence Erlbaum Associates, Inc, Hillsdale, pp 207–233
Puhl RM, Neumark-Sztainer D, Austin SB et al (2014) Setting policy priorities to address eating disorders and weight stigma: views from the field of eating disorders and the US general public. BMC Public Health 14:524. https://doi.org/10.1186/1471-2458-14-524
Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH (2013) A systematic review of stress-management programs for medical students. Acad Psychiatry J Am Assoc Dir Psychiatr Resid Train Assoc Acad Psychiatry 37:158–164. https://doi.org/10.1176/appi.ap.12010003
Shehnaz SI, Arifulla M, Sreedharan J, Gomathi KG (2017) What do faculty feel about teaching in this school? assessment of medical education environment by teachers. Educ Health Abingdon Engl 30:68–74. https://doi.org/10.4103/1357-6283.210500
Stice E (2016) Interactive and mediational etiologic models of eating disorder onset: evidence from prospective studies. Annu Rev Clin Psychol 12:359–381. https://doi.org/10.1146/annurev-clinpsy-021815-093317
Panchami P, Samuel T (2016) A cross-sectional study of disturbed eating attitudes and behaviours in medical students. Int J Res Med Sci 4:2830–2833. https://doi.org/10.18203/2320-6012.ijrms20161959
Funding
No funds were received towards the study at any stage.
Author information
Authors and Affiliations
Contributions
HJ and ZS designed the study. HJ coordinated data search, data entry, data cleaning and performed statistical analyses. HJ and ML wrote the first draft, ZS and MF provided intellectual contributions to strengthening the manuscript and suggested additional data analyses. All authors provided critical revisions of manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Jahrami, H., Saif, Z., Faris, M.AI. et al. The relationship between risk of eating disorders, age, gender and body mass index in medical students: a meta-regression. Eat Weight Disord 24, 169–177 (2019). https://doi.org/10.1007/s40519-018-0618-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-018-0618-7