Abstract
Eating disorders (ED) are prevalent mental illnesses composed mainly of anorexia nervosa, bulimia nervosa and binge eating disorders. Anxiety disorders are another set of mental illnesses, with phobic disorder (PD) being the most prevalent disorder. ED and PD are highly comorbid. The aim of this study is to assess, in 131 individuals attending an outpatient clinic for different health issues, the level of fear related to situations generating avoidance such as in social anxiety and specific phobias according to the fear questionnaire (FQ), the level of disgust according to the disgust scale (DS-R) and the vulnerability towards ED according to the SCOFF scale to demonstrate that high levels of both fear and disgust increase the vulnerability towards ED. The study demonstrated that the level of disgust increased when fear increases (r = 0.377, p < 0.001 for the first part of the FQ; r = 0.225, p = 0.01 for the second part of the FQ). Moreover, individuals with vulnerability towards having an ED presented a higher level of disgust than individuals without this vulnerability (p = 0.009). Furthermore, individuals with vulnerability towards ED have a higher level of anxiety related to PD subtypes (p = 0.008 for agoraphobia; p = 0.001 for injection/blood phobia) as well as to social anxiety (p = 0.01), independently from having a depressive or another anxiety disorder. In the multivariate analysis, a history of psychiatric consultation has been the only significantly different parameter between individuals with or without vulnerability towards ED (p = 0.0439). Accordingly, fear and disgust are negative emotions that seem to be clinically associated which better explains the comorbidity of ED with PD.
Level of evidence
Level III. Evidence obtained from well-designed cohort or case–control analytic studies, preferably from more than one center or research group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eating disorders (ED) are chronic psychiatric illnesses composed mainly of anorexia nervosa (AN), bulimia nervosa (BN) and binge eating disorders (BED), with a worldwide point prevalence ranging from 0.01 to 4.45% [22]. Among anxiety disorders, phobic disorders (PD) are the most common with a lifetime prevalence as high as 13.8% [4]. One of the challenges encountered in the treatment of eating and anxiety disorders are their frequent co-occurrence. The comorbidity between ED and anxiety disorders is around 65% [32]. Of these anxiety disorders, social anxiety disorder and specific phobias are the most frequently diagnosed disorders (44%) [32].
Disgust is a basic emotion that is evoked by stimuli which possess particular features that connote disease. In this sense, typical disgust elicitors are spoiled food, poor hygiene, and contact with ill or dead organisms. With the human evolution, more abstract solicitors of the disgust feeling have become identified such as “moral disgust” [37]. Elevated externally directed disgust has been identified as a contributing factor to the development of several mental disorders including anxiety disorders and obsessive–compulsive disorder [7, 28].
In their critical review, Cisler et al. suggested that fear and disgust are involved in the emotional response in some phobic disorders (PD) including blood-injection-injury phobia and spider phobia, and in contamination-related obsessive–compulsive disorder [11]. In specific phobias such as blood/injection and spider phobias, disgust seems to contribute to the etiology and maintenance of the disorder along with fear and anxiety [10].
Previous studies have tried to elicit the relation between ED and disgust and have suggested the role of disgust in the development and maintenance of AN [16, 20]. In a larger group of 124 patients, (32 patients with AN and 62 controls), Aharoni and Hertz showed that there is an elevated overall disgust sensitivity and an elevated sensitivity in most disgust domains in patients with AN compared to controls [1]. A recent study including 591 women also showed that patients with AN or BN experience higher levels of self-disgust compared to controls. Experience of self-disgust was itself associated with disgust sensitivity and anxiety [6]. Furthermore, ED are characterized by the presence of several phobic behaviors that are motivated by disgust and fear. Swallowing phobia is characterized by fear of choking on having consumed food, liquids or tablets [34]. “Emetophobia” or specific phobia of vomiting has also been described as one of the reasons behind reducing alimentary intake in patients that manifest clinical signs and symptoms of AN [36]. Finally, the concept of “fat phobia” or fear of gaining weight, which is an essential component in the diagnosis of AN according to all classifications, has been a subject of many controversies. In a meta-analysis evaluating literature about non-fat-phobic (NFP) AN, authors found that NFP-AN can be differentiated from conventional AN by milder levels of eating pathology [5]. However, data are still insufficient to clarify the relation between these two groups of patients and that further studies are necessary to find an evidence for the diagnostic validity for NFP-AN [5]. In sum, AN can be seen as a disorder that manifests with an increased need of control and perfectionism as well as a high level of emotional distress and self-dissatisfaction [9]. In the actual classification, whether the ED is accompanied with “fat phobia” will only change the ED subcategory from AN to an unspecified ED (American Psychiatric Association 2013).
One of the suggested mechanisms implicated in the pathophysiology of ED is a dysfunction in the insular lobe, a central component of the brain emotional circuitry. In several studies, a disturbed activity in the anterior insular lobe, known to be involved in appetite dysregulation, disturbance of body image and feeling of disgust, was found in patients with AN [29, 31]. Furthermore, AN and BN tend to have premorbid traits, such as perfectionism and anxiety that are related with dysregulation within and/or between limbic and executive cortico-striatal circuits [23]. At least in AN, an active HPA axis may contribute in maintaining the neuroendocrine, emotional and behavioral effects observed. More specifically, it is suggested that the HPA axis interacts with limbic structures, including the insular and prefrontal cortices, to uphold the changes in interoceptive and emotional awareness seen in AN [8]. Studies have shown that perception of facial disgust expressions activates the anterior insula [17]. Furthermore, some studies show that the anterior insula is involved in the coupling between disgust sensation and some negative emotions generated by the amygdala such as anger [2], increasing the level of disgust after anger emotion. On the other hand, insular lobe seems also to be activated after exposure to a threat and plays a role in determining the emotional response of individuals in stressful situations [15].
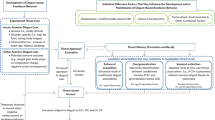
Accordingly, it can be hypothesized that individuals who express a heightened level of both disgust and fear feelings are at a higher risk to develop an ED. Studies evaluating the relationship of disgust and eating disorders in non-clinical populations exist [12, 25]. According to these studies, it seems that disgust, as a negative emotion, influences eating disorders symptoms through a heightened level of anxiety. The importance of the selection of a non-clinical population resides in the fact that individuals with vulnerability towards ED may show better coupling of their emotions than individuals suffering from clinical ED. No studies assessing specifically fear as a negative emotion generating by avoided situations such as in social anxiety and specific phobias exist. The aim of the current study is to assess the level of disgust and fear feelings in such situations in individuals who are at high risk of developing an ED.
Materials and methods
Study design and setting
This is a descriptive, cross-sectional study evaluating the relationship between the vulnerability towards ED, fear and disgust emotions in an outpatient setting. The study was carried out at the outpatient clinics of Hotel Dieu de France hospital in Lebanon during the month of June 2017. Approval of the ethical committee of the hospital was obtained (file registered under the Reference Number CEHDF 968). Informed verbal consent was obtained from the participants after a detailed explanation of the study protocol and objectives prior to their recruitment.
Sampling
A convenience sample was formed during the study period. The sample consisted of patients or their accompanist visiting the outpatient clinic of the hospital and who were waiting for their appointment (dermatology, infectious diseases, ophthalmology, orthopedics, etc.). The physical illnesses from which suffered the participants were so heterogeneous and the setting for recruitment of patients and their accompanist was sufficiently neutral as per the presence or absence of traits of fear and/or disgust. All individuals who accepted to participate in the study during the study period were included. Patients who could not understand and read English or French were assisted. All participants were given the assessment tools described below and were asked to answer all the included questions. The third author of this manuscript was waiting to assist the participants by answering any question they had regarding the content of the assessment tool.
Assessment tools and procedure
For every participant included in the study, socio-demographic parameters were collected (age, gender, marital status, education and employment). Clinical parameters were also collected (the presence of a mental illness, past or present history of psychotropic treatment, history of a psychologist or a psychiatrist visit). We controlled for the presence of a mental disorder by asking the patients directly to self-report whether they have been prescribed a psychotropic drug or whether they have consulted a psychiatrist or a psychologist in the past. Fear was evaluated using the Marks and Mathews scale or the fear questionnaire (FQ) [24]. It is a 24-item questionnaire that consists of simple and brief questions evaluating the degree of avoidance of specific situations (first part—17 items: “Fear I”), the suffering of the patient (second part—6 items: “Fear II”), and the level of discomfort with the phobic behavior (third part—1 item: “Fear III”), all rated on an eight-point Likert scale. Disgust was evaluated using the DS-R scale (disgust scale-revised) [18]. This is a 32-item scale measuring disgust sensitivity across eight domains (i.e., animals, body products, death, body envelope violations, food, hygiene, deviant sexual practices and sympathetic magic). A total score higher than 16 is considered positive. SCOFF questionnaire was used to assess the risk of developing an ED [26]. The SCOFF questionnaire is a brief and simple screening instrument comprising five dichotomous questions regarding binge eating, purging, and body dissatisfaction. The participant is considered at risk of developing an eating disorder when two or more of the answers are positive.
Statistical analysis
All analyses were performed using SPSS version 21 and STATA 13. Descriptive statistics were reported using means and standard deviations for continuous variables, and proportions for categorical variables. T test was used for the comparison of age between the subgroups of participants according to the result of SCOFF score (positive or negative). Mann–Whitney U test was used for the comparison of scores between subgroups of participants according to the result of SCOFF score (positive or negative). Χ-square and Fisher’s exact tests were used for the association between categorical variables. Spearman correlation was used for the measurement of correlation between the sub-scales of fear in the whole sample as well as in the subgroups of participants according to the result of SCOFF scores (positive or negative). A p value lower than 0.05 was considered as statistically significant. Statistically significant associations were included in a multivariate logistic regression model. Adjusted odds-ratios (ORadj) and 95% confidence intervals (95% CI) were reported. Only those with an ORadj not including the value 1 were considered as significant.
Results
Participants’ characteristics
The sample consisted of 131 participants: 94 females (71.8%) and 37 males (28.2%). The age range was 13–68 years with an average age of 31.8 years (SD 12.0). The majority of respondents were single (68.7%), had university degree (82.7%) and were employed (60.4%). Eight participants (6.1%) have been treated with psychotropic medications. Thirty-three participants (25.2%) have already visited a psychologist and 15 (11.5%) have visited a psychiatrist.
Scores and correlations
The mean score on the first part of the Marks and Mathews scale (Fear I) in our sample was 25.2 (SD 17.2) and the mean score on the second part (Fear II) was 12.8 (SD 8.6). The mean score on the DS-R scale was 20.0 (SD 6.6). 45% of participants had a positive score on the SCOFF scale (had two or more out of five positive responses).
We found a statistically significant correlation between the level of disgust on DS-R and the score of the Fear I questionnaire (r = 0.377; p < 0.001). In addition, we found a statistically significant correlation between the level of disgust on DS-R and the severity of anxiety as represented by the Fear II questionnaire (r = 0.225; p = 0.01).
Comparison of subgroups
We have divided our participants into two subgroups: (1) Group A with no vulnerability towards ED as manifested by a negative score on the SCOFF scale; (2) Group B with a vulnerability towards ED as manifested by a positive score on the SCOFF scale. The comparison between both subgroups showed no difference for all parameters except for a higher probability of having consulted a psychiatrist for group B (p = 0.039), a higher score on DS-R for group B (p = 0.009) (Fig. 1), a higher total score on the fear questionnaire for group B (p = 0.001), a higher score on agoraphobia subscale for group B (p = 0.008), a higher score on the injection/blood subscale for group B (p = 0.001) and a higher score on social anxiety subscale for group B (p = 0.01) (Table 1; Fig. 2). Of note, the depression/anxiety subscale scores of the FQ were not statistically different between group A and B (p = 0.061). In the multivariate analysis, previous consultation with a psychiatrist has been the only significantly different parameter between group A and B [ORadj = 3.62; 95% CI (1.01–13.16); p = 0.039] (Table 2).
Discussion
The current study has demonstrated that, in individuals selected in our sample, the level of disgust is increased whenever the feeling of fear is high. In addition, this study demonstrates that individuals with vulnerability towards having an ED present a higher level of disgust than individuals without this vulnerability. Moreover, individuals with vulnerability towards ED have a higher level of fear related to PD subtypes as well as to social anxiety, independently from having a depressive or another anxiety disorder. Accordingly, fear in situations generating avoidance from one part and disgust from another part are two negative emotions that seem to be implicated in the psychopathology of ED. This is in concordance with the high comorbidity of ED and PD that is described in epidemiologic studies.
In the multivariate analysis, the only significantly different factor between individuals with or without vulnerability towards ED is having a history of psychiatric consultation. This finding may be explained by the fact that having a history of psychiatric consultation has a significant effect on vulnerability towards ED as well as on fear and anxiety symptoms. Having a past psychiatric history seems to be the precursor for heightened levels of fear and disgust in the group of individuals who are vulnerable to ED. Accordingly, it can be deduced that in the population of patients consulting a psychiatrist, those with vulnerability towards ED are those who manifest the highest levels of fear and disgust. This finding might show the importance of fear and disgust emotions as prognostic factors, predicting a more severe form of ED if one may speculate that patients who previously consulted a psychiatrist are those who have the most severe mental health issues. However, the cross-sectional aspect of this study design precludes us from confirming this causal relationship.
Mayer et al. [25] considered that covariation bias, which is the phenomenon of overestimating the contingency between certain stimuli and negative outcomes, may be a cognitive bias involved in the maintenance of ED. The study was based on the fact that fear is generally considered to be linked to a style of confirmatory processing of certain particular fear-relevant stimuli with certain specific affectively linked outcomes, which makes that it serves the maintenance or enhancement of fear. Fearful individuals are generally found to already expect beforehand that fear-relevant stimuli will be more often followed by negative outcomes [33]. However, in certain anxiety disorders, certain fear-related stimuli such as animal phobia are found to be more frequently associated with disgust-related outcomes such as the exposure to low-predatory animals [13]. In a sample of 61 women assessed for covariation bias, ED pathology was positively associated with a covariation bias referring to the associations between obese bodies and fear-relevant outcomes, and between slim bodies and disgust-relevant outcomes [25]. This demonstrates that these two negative emotions are closely experienced by patients with ED and play a role in the prognosis of the disease.
Several dimensional aspects of the comorbidity between ED and PD through fear and disgust have also been extensively studied. Worry, which is a mental process accompanying anxiety disorders and characterized by the predominance of a negative-type and preoccupied thought about possible threatening future events, has been assessed in patients with ED. Worry has been found to be associated with all the symptoms of ED [30]. In line with the results of the current study, Davey and Chapman showed in a non-clinical population that the experience of disgust may be heightened in individuals with ED symptomatology [12]. However, the results became non-significant when trait anxiety levels and anxiety sensitivity were considered as confounding factors which suggest that disgust is not an independent predictor of ED symptoms and may be linked to anxiety traits and sensitivity [12]. In contrast with the methodology of this paper, the relationship between fear and disgust was directly evaluated in our study, with increased disgust when fear increases. Further studies are needed to confirm this association. Health anxiety has been linked with symptoms of ED. In a study that sought to determine the incremental specificity of disgust propensity and sensitivity in the prediction of symptoms of health anxiety in a large non-clinical sample, it has been suggested that disgust may be a unique vulnerability for the vigilance for bodily sensations/changes aspect of health anxiety [27]. This finding broadens the spectrum of anxiety feelings of individuals with vulnerability towards ED and demonstrates that they do not only fear situations or objects in their environment but they also fear changes and sensations that might normally occur in their bodies. A better understanding of this correlation between anxiety, body image and eating behavior comes from an interesting study explaining the development of body image dissatisfaction in a clinical sample of patients suffering from ED. According to the cross-sectional findings of this study, insecure attachment with heightened anxiety appears to be a consistent correlate of negative body image evaluations in women with either AN or BN [35]. As a matter of fact, Hart et al. [19] defined the anxiety and/or fear associated with one’s physique being evaluated as Social Physique Anxiety (SPA). It has been later demonstrated that SPA is correlated with the presence of ED symptoms [14]. However, whether it is named SPA or social anxiety with body dissatisfaction, it seems that one of the most important factors that determine the attachment style and the level of anxiety related to it is the role of parenting experience. Hinrichsen et al. [21] demonstrated that, in 70 women suffering from an ED, social anxiety is associated with emotionally inhibited parenting by fathers (i.e., parenting that reflects a lack of ability to share feelings with the child), while agoraphobia is associated with anxious/fearful parenting by mothers (i.e., parenting that reflects anxious, fearful traits in the parent and a pessimistic outlook on life). Accordingly, phobic fear and anxiety in individuals with vulnerability towards ED may be understood in a more global concept that emanates from an unhealthy parenting experience leading to an anxious attachment style that evolves to an anxiety towards one’s body shape and/or health and a fear from ordinary environmental cues.
This study has some limitations. First, it is a cross-sectional study showing an association rather than a causal relationship. Second, the number of individuals belonging to the subgroups is low which might lower the strength of the statistical analysis. Third, individuals were only interrogated about their symptoms without having any other objective assessment tool. Fourth, the selected sample presented some heterogeneity since a subset of interviewed participants had physical problems while others were healthy in addition to the fact that participants’ age range was wide. Fifth, participants should have given a written consent on the study protocol before filling the questionnaires.
Conclusion
ED and PD share several clinical features. Among those, disgust and fear seem to be two negative emotions that manifest more importantly in individuals who are at risk of having an ED. Moreover, in the population of patients consulting a psychiatrist, those with vulnerability towards ED seem to manifest high levels of fear and disgust. Future longitudinal studies in the field of phobic fear and anxiety in individuals with vulnerability towards ED are needed. These studies might be interested in assessing, altogether, the impact of unhealthy parenting experiences, attachment styles, anxiety towards one’s body shape and/or health and fear from ordinary environmental cues.
References
Aharoni R, Hertz MM (2012) Disgust sensitivity and anorexia nervosa. Eur Eat Disord 20(2):106–110. https://doi.org/10.1002/erv.1124
Anderson AK, Christoff K, Panitz D, De Rosa E, Gabrieli JDE (2003) Neural correlates of the automatic processing of threat facial signals. J Neurosci 23(13):5627–5633
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, fifth edition: DSM-5. American Psychiatric Publishing, Arlington, USA
Bandelow B, Michaelis S (2015) Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci 17(3):327–335
Becker AE, Thomas JJ, Pike KM (2009) Should non-fat-phobic anorexia nervosa be included in DSM-V? Int J Eat Disord 42(7):620–635. https://doi.org/10.1002/eat.20727
Bell K, Coulthard H, Wildbur D (2017) Self-disgust within eating disordered groups: associations with anxiety, disgust sensitivity and sensory processing. Eur Eat Disord Rev 25(5):373–380. https://doi.org/10.1002/erv.2529
Berle D, Phillips ES (2006) Disgust and obsessive-compulsive disorder: an update. Psychiatry 69(3):228–238. https://doi.org/10.1521/psyc.2006.69.3.228
Bou Khalil R, Souaiby L, Farès N (2017) The importance of the hypothalamo-pituitary-adrenal axis as a therapeutic target in anorexia nervosa. Physiol Behav 171:13–20. https://doi.org/10.1016/j.physbeh.2016.12.035
Carter JC, Bewell-Weiss CV (2011) Nonfat phobic anorexia nervosa: clinical characteristics and response to inpatient treatment. Int J Eat Disord 44(3):220–224. https://doi.org/10.1002/eat.20820
Çavuşoğlu M, Dirik G (2011) Fear or disgust? The role of emotions in spider phobia and blood-injection-injury phobia. Turk J Psychiatry 22(2):115–122
Cisler JM, Olatunji BO, Lohr JM (2009) Disgust, fear, and the anxiety disorders: a critical review. Clin Psychol Rev 29(1):34–46. https://doi.org/10.1016/j.cpr.2008.09.007
Davey GCL, Chapman L (2009) Disgust and eating disorder symptomatology in a non-clinical population: the role of trait anxiety and anxiety sensitivity. Clin Psychol Psychother 16(4):268–275. https://doi.org/10.1002/cpp.623
De Jong PJ, Peters ML (2007) Contamination vs. harm-relevant outcome expectancies and covariation bias in spider phobia. Behav Res Ther 45:1271e1284
Diehl NS, Johnson CE, Rogers RL, Petrie TA (1998) Social physique anxiety and disordered eating: what’s the connection? Addict Behav 23(1):1–6
Etkin A, Wager TD (2007) Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry 164(10):1476–1488. https://doi.org/10.1176/appi.ajp.2007.07030504
Fox JRE, Harrison A (2008) The relation of anger to disgust: the potential role of coupled emotions within eating pathology. Clin Psychol Psychother 15(2):86–95. https://doi.org/10.1002/cpp.565
Fusar-Poli P, Placentino A, Carletti F, Landi P, Allen P, Surguladze S, Politi P et al (2009) Functional atlas of emotional faces processing: a voxel-based meta-analysis of 105 functional magnetic resonance imaging studies. J Psychiatry Neurosci JPN 34(6):418–432
Haidt J, McCauley C, Rozin P (1994) Individual differences in sensitivity to disgust: A scale sampling seven domains of disgust elicitors. Personal Individ Differ 16(5):701–713. https://doi.org/10.1016/0191-8869(94)90212-7
Hart EA, Leary MR, Rejeski WJ (1989) The measurement of social physique anxiety. J Sport Exerc Psychol 11:94–104
Harvey T, Troop NA, Treasure JL, Murphy T (2002) Fear, disgust, and abnormal eating attitudes: a preliminary study. Int J Eat Disord 32(2):213–218. https://doi.org/10.1002/eat.10069
Hinrichsen H, Sheffield A, Waller G (2007) The role of parenting experiences in the development of social anxiety and agoraphobia in the eating disorders. Eat Behav 8(3):285–290
Hoek HW (2016) Review of the worldwide epidemiology of eating disorders. Curr Opin Psychiatry 29(6):336–339. https://doi.org/10.1097/YCO.0000000000000282
Kaye WH, Wierenga CE, Bailer UF, Simmons AN, Wagner A, Bischoff-Grethe A (2013) Does a shared neurobiology for foods and drugs of abuse contribute to extremes of food ingestion in anorexia and bulimia nervosa? Biol Psychiat 73(9):836–842. https://doi.org/10.1016/j.biopsych.2013.01.002
Marks IM, Mathews AM (1979) Brief standard self-rating for phobic patients. Behav Res Ther 17(3):263–267
Mayer B, Muris P, Wilschut M (2011) Fear- and disgust-related covariation bias and eating disorders symptoms in healthy young women. J Behav Ther Exp Psychiatry 42(1):19–25
Morgan JF, Reid F, Lacey JH (1999) The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ 319(7223):1467–1468
Olatunji BO (2009) Incremental specificity of disgust propensity and sensitivity in the prediction of health anxiety dimensions. J Behav Ther Exp Psychiatry 40(2):230–239
Olatunji BO, Cisler J, McKay D, Phillips ML (2010) Is disgust associated with psychopathology? Emerging research in the anxiety disorders. Psychiatry Res 175(1–2):1–10. https://doi.org/10.1016/j.psychres.2009.04.007
Royet J-P, Plailly J, Delon-Martin C, Kareken DA, Segebarth C (2003) fMRI of emotional responses to odors: influence of hedonic valence and judgment, handedness, and gender. NeuroImage 20(2):713–728. https://doi.org/10.1016/S1053-8119(03)00388-4
Sassaroli S, Bertelli S, Decoppi M, Crosina M, Milos G, Ruggiero GM (2005) Worry and eating disorders: a psychopathological association. Eat Behav 6(4):301–307
Stip E, Lungu OV (2015) Salience network and olanzapine in schizophrenia: implications for treatment in anorexia nervosa. Can J Psychiatry 60(3 Suppl 2):S35–S39
Swinbourne J, Hunt C, Abbott M, Russell J, St. Clare T, Touyz S (2012) The comorbidity between eating disorders and anxiety disorders: prevalence in an eating disorder sample and anxiety disorder sample. Austr N Z J Psychiatry 46(2):118–131. https://doi.org/10.1177/0004867411432071
Tomarken AJ, Sutton SK, Mineka S (1995) Fear-relevant illusory correlations: what types of associations promote judgmental bias? J Abnorm Psychol 104:312–e326
Torralbas-Ortega J, Puntí-Vidal J, Valls-Ibáñez MV, Arias-Núñez E, Naranjo-Díaz MC (2012) Choking phobia: care plan in children and adolescents. Enferm Clin 22(4):224–230. https://doi.org/10.1016/j.enfcli.2012.02.003
Troisi A, Di Lorenzo G, Alcini S, Nanni RC, Di Pasquale C, Siracusano A (2006) Body dissatisfaction in women with eating disorders: relationship to early separation anxiety and insecure attachment. Psychosom Med 68(3):449–453
Veale D, Costa A, Murphy P, Ellison N (2012) Abnormal eating behaviour in people with a specific phobia of vomiting (emetophobia). Eur Eat Disord Rev 20(5):414–418. https://doi.org/10.1002/erv.1159
Vicario CM, Rafal RD, Martino D, Avenanti A (2017) Core, social and moral disgust are bounded: a review on behavioral and neural bases of repugnance in clinical disorders. Neurosci Biobehav Rev 80:185–200. https://doi.org/10.1016/j.neubiorev.2017.05.008
Funding
This research did not receive any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study has received the approval of the ethical committee of Hotel dieu de France hospital (file registered under the Reference Number CEHDF 968).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Bou Khalil, R., Bou-Orm, I.R., Tabet, Y. et al. Disgust and fear: common emotions between eating and phobic disorders. Eat Weight Disord 25, 79–86 (2020). https://doi.org/10.1007/s40519-018-0512-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-018-0512-3