Abstract
Purpose
Obesity is a major public health burden. Outpatient clinics are an essential resource for individuals with obesity to access advice for weight loss management. The aim of this study was to compare anthropometric and weight loss outcomes between participants receiving general dietary (GD) advice, and those on a very low energy diet (VLED) under non-trial conditions.
Methods
Data from 276 adults with obesity attending a multidisciplinary weight management clinic were analysed. Changes in anthropometry, body composition, and blood pressure (BP) over 12 months were analysed using linear mixed-effects models.
Results
Males on the GD demonstrated statistically greater reductions in body weight (BW), BMI, percent fat mass (FM), systolic BP, waist and hip circumference (p < 0.01). Changes in males on a VLED did not reach significance. Females showed statistically significant reductions in BW, BMI, waist and hip circumference regardless of dietary intervention (p < 0.01); those on the GD significantly reduced percent FM (p < 0.001). Females on a VLED had statistically greater reductions in BW, BMI and systolic BP compared to those on the GD. No effect of exercise physiologist was observed in this study. Participants prescribed a GD attended for significantly longer than those on a VLED (p < 0.05), irrespective of gender. At 12 months, 14.3 and 4.5% of males and females on a VLED were still attending, compared to 10.6 and 4.5% on the GD.
Conclusions
In this retrospective study, females in both dietary intervention groups achieved significant changes across multiple measures. Only men receiving GD advice demonstrated significant changes.
Level of evidence
Level II-2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Global rates of overweight and obesity have risen to epidemic proportions, with more than 1.9 billion people estimated to be overweight, and 600 million people obese [1]. Data from the 2014–2015 National Health Survey conducted by the Australian Bureau of Statistics reports 63.4% of Australian adults were overweight, and 27.9% obese [2]. Prevalence of overweight and obesity was higher in men (70.8%) than women (56.3%). In clinical settings, obese patients require specialised care and equipment, have longer lengths of stay, and higher costs and rates of re-admission than normal weight patients (BMI 18.5–24.9 kg/m2) [3]. Individuals with obesity also have higher rates of comorbidities affecting quality of life and complicating medical treatment [4, 5], costing in excess of $58.2 billion per annum in reduced workplace productivity, government assistance, and costs to the Australian health sector [6]. Non-surgical weight management programs promote a multidisciplinary approach, focusing on intensive dietary and exercise interventions, with adjunctive behavioural modification [4, 7,8,9,10,11,12,13,14,15]. Studies evaluating non-surgical weight management in the clinical setting are scarce, often lack substantial follow-up [7, 12, 16] or demonstrate long-term weight re-gain [4, 8]. While surgical interventions achieve high rates of long-term weight loss [20–32% of initial body weight (BW)] [8] and high rates of co-morbidity resolution, surgery is subject to strict inclusion criteria including BMI cut-offs (BMI ≥ 40 kg/m2, or BMI ≥ 35 kg/m2 with significant co-morbidities), and exclusion of patients with psychiatric disorders and limited financial resources [8, 17]. In New South Wales (NSW), Australia, bariatric surgery remains unaffordable to most patients within the public health system [18]. Therefore, there is a need for effective non-surgical treatment for adults with obesity.
Changes in BW, anthropometry, and body composition are frequently reported outcomes in weight management studies [4, 7,8,9,10,11,12,13,14,15, 19, 20]. A loss of ≥ 5–10% of starting BW [clinically significant weight loss (CSWL)] improves cardiovascular risk factors and reduces mortality, and is frequently reported in studies [7, 9, 11, 13,14,15]. Published literature shows variable proportions of patients achieve CSWL of between 20% [7] and 81% [4]. Furthermore, fat mass (FM) reduction from intentional weight loss, particularly following a very low energy diet (VLED) [20], is associated with improvement in overall health and comorbidities, and is also frequently reported [19].
Relatively few studies assess the effectiveness of outpatient clinics under non-trial conditions, reducing the generalisability of results to real clinical settings. Based on current literature, we hypothesise that patients on an intensive VLED will achieve greater weight loss compared to general dietary (GD) advice, and that patients who consult with an exercise physiologist will demonstrate greater weight loss than those who do not. The aim of this study was to compare weight loss outcomes between dietary intervention patient groups in an outpatient obesity clinic.
Subjects and methods
Study design and setting
This retrospective observational study was conducted at a tertiary hospital outpatient obesity clinic. Ethics approval was obtained from the Western Sydney Local Health District (WSLHD) Human Research Ethics Committee and designed in line with the Declaration of Helsinki [21]. Participants were outpatients at Westmead Hospital (Western Sydney, Australia), which services a large culturally and linguistically diverse population, estimated at 876,000 in 2013, making it the second-largest local health district in NSW by population served [22], and the fastest growing. WSLHD reports a lower Socio-Economic Indexes for Areas (SEIFA) of 994 compared to the national and Sydney averages of 1000 and 1011 respectively, reflecting lower socioeconomic status (SES) and higher disadvantage. In 2013, 49.7% of the population of WSLHD were estimated to be overweight or obese, and 19.5% were obese [22].
Participant eligibility
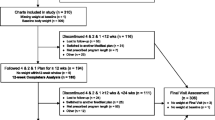
Participants were eligible if they attended an initial appointment at the Westmead Hospital Multidisciplinary Obesity Clinic between January 2011 and December 2012 inclusive, were aged ≥ 18 years at baseline, and had a starting BMI ≥ 30 kg/m2. Clinic admission was based upon referral from a health professional and subject to self-directed attendance. A total of 276 of 522 screened patients were eligible for analysis (Fig. 1).
Weight loss interventions
Participants were prescribed an energy-restricted diet plan that required following a VLED or GD advice based upon advice by an endocrinologist and dietitians, and personal preference. Participants prescribed VLED were educated on the ketogenic Optifast® meal replacement program (Optifast; Nestle Nutrition, Frankfurt, Germany). The VLED was intended to be at least two, preferably three meals per day, however some participants would not accept this starting rate due to concerns with hunger, cost or side effects; therefore, participants consuming at least one meal replacement per day were included in the VLED group. Efforts were made to increase daily frequency of VLED meals to take benefit of the ketogenic effect. Participants having one or two meal replacements per day were required to keep carbohydrate intake < 50–70 g per day and were provided with a proscriptive low carbohydrate, 800 calorie (1744 kJ) meal plan. Participants not prescribed a VLED were allocated to the GD group, and prescribed an energy-restricted diet based on the Australian Dietary Guidelines [23], consisting of 20–35% total energy from fat, 45–65% energy from carbohydrate and 15–25% energy from protein. Exercise was recommended, if medically safe, to augment caloric deficit. An exercise physiologist prescribed tailored moderate intensity physical activity, an endocrinologist assessed comorbidities, and dietitians monitored dietary adherence at each visit using self-completed food diaries, or failing that, a 24-h recall. It was estimated that 3–5% of patients attending the clinic were taking phentermine (Duromine®) at any time.
Data collection and management
Data were obtained from clinical databases and medical records, deidentified, and given a study code to blind researchers. Comorbidities and dietary and exercise intervention modality were recorded. Participants who attended only one appointment over 12 months were defined as non-attenders, and participants who attended ≥ 2 appointments were defined as attenders.
Data-collection instruments
Anthropometric and body composition data were taken as single measurements recorded by nursing staff at each visit according to standard protocol [24]. Height was measured to the nearest 0.5 cm using a stadiometer. Waist and hip circumference was measured to the nearest 0.5 cm using a measuring tape. Body composition data [BW (kg), FM (kg, %), and lean mass (LM) (kg, %)] were measured using a two-compartment bioimpedance scale (Tanita Body Composition Analyzer model BC-420MA), with participants wearing light clothing and no shoes. Body mass was measured to an accuracy of 0.1 kg, and composition percentages to an accuracy of 0.1%. Blood pressure (BP) was taken in a seated position using an automatic sphygmomanometer adjusted for obese patients. BMI was calculated as body mass (kg) divided by height (m2). Waist-to-height ratio (WHtR) was taken as waist circumference (cm) divided by height (cm) to obtain a ratio.
Outcomes and assessment
Primary outcomes were rate of change in BW per month up to 12 months of intervention, and achievement of CSWL (loss of ≥ 5% of starting BW over 12 months). Secondary outcomes were rates of change per month of BMI, hip and waist circumference, WHtR, BP, percentage and absolute FM and LM. Rates of change per month were chosen as times between consults were not always regular. Rates of change for each outcome were compared by dietary (GD vs VLED) and exercise physiologist intervention. Clinic retention (the proportion of patients from baseline who were still attending clinic visits up to 12 months) was also recorded.
Statistical analysis
Values are presented as mean (standard deviation), unless stated otherwise. Median values with upper and lower quartiles are used to summarise skewed data. Comorbidities are reported in absolute numbers and proportions (%). Categorical variables were compared between intervention groups using Pearson’s Chi-squared or Fisher’s exact test, and two-sample t tests used to compare continuous variables between intervention groups at baseline. Linear mixed-effects models were used to investigate the effects of dietary intervention and gender on rates of change of continuous outcomes in the first 12 months. In these models, participant identifier was the group variable, month was considered as both a continuous random and fixed effect, and gender and dietary intervention considered as categorical fixed effects. Since there were statistically significant two-way interactions between the effects of gender and dietary intervention on the rates of change of the continuous outcomes, all dietary intervention effects have been reported separately by gender. Normal Q–Q plots were used to check that residuals from fitted models showed no obvious departure from the underlying assumption of normality. Statistical significance was taken at the 5% level (p < 0.05). Analyses were performed using SPSS version 21.0 (IBM, SPSS, Chicago, IL, USA) and S-PLUS, version 8.0 (TIBCO, Software Inc., Palo Alto, CA, USA).
Results
Sample characteristics
Two-hundred and seventy-six adult outpatients with obesity, with an age range of 18–78 years, were included in this study, 177 (64.1%) of which were female (Table 1). Thirty-six participants (13.1%) followed a VLED; 22 were women (8.0%) and 14 were men (5.1%). VLED participants had significantly higher baseline BW, BMI, WC, HC, WHtR and FM (%, kg) than those on the GD. Male VLED participants had higher baseline LM (kg) and female GD participants had significantly higher baseline %LM than female VLED participants. Of the 276 participants, 185 (67.0%) attended more than one appointment (attenders). Female attenders were significantly older than non-attenders, and had a lower median baseline weight; however, differences did not reach significance and no other differences were observed. Obstructive sleep apnoea was the most frequent comorbidity, followed by hypertension, asthma, and diabetes. Significant differences were found in prevalence of osteoarthritis and hypothyroidism (p < 0.05). Psychiatric conditions, including anxiety, depression, bipolar disorder, schizophrenia and intellectual/developmental delays were observed in 26.3% of males and 23.3% of females. There were no significant differences in any variables at baseline between those who saw the exercise physiologist and those who did not.
Clinic attendance and retention
Median (IQR) length of attendance did not differ by gender [1.8 months (0, 9.2) and 1.4 months (0, 6.2) for males and females, respectively (p = 0.132) over 12 months]. However, median length of attendance was influenced by dietary intervention; participants prescribed the VLED intervention attended for significantly less time [males 1.8 months (0, 9.0); females 1.1 months (0, 6.0)] than those who were prescribed the GD [males 4.5 months (0.5, 10.3); females 4.4 months (1.1, 7.8)], irrespective of gender (p < 0.05). Retention (the proportion of participants from baseline still attending clinic visits at 12 months) was higher in males in both dietary interventions. Twelve-month retention rates in the VLED group were 14.3 and 4.5% for males and females respectively, and GD participants had 10.6 and 4.5% retention for males and females, respectively (Fig. 2).
Effectiveness of dietary interventions
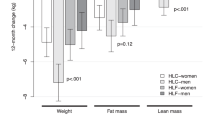
Males
Males on the GD had statistically significant reductions in anthropometric measurements of BW (− 0.93 kg/month), BMI (− 0.30 kg/m2/month), WC (− 0.53 cm/month) and HC (− 0.63 cm/month), as well as SBP and DBP (Table 2). While males on the VLED showed decreases in these measurements, none reached statistical significance. Males on the GD also had statistically significant reductions in %FM and total FM of − 0.51%/month and − 1.1 kg/month, respectively (p < 0.05), though those on a VLED has non-significant increases in %FM and total FM, and concomitant reductions in %LM and total LM. Maximum weight loss among males on the VLED was − 8.0% at 11 months after initial visit, and − 28.6% among males on the GD, achieved at 16 months after initial visit (Fig. 2).
Females
Both GD and VLED groups had statistically significant reductions in BW, BMI, WC, HC and WHtR from baseline. Reductions in BW and BMI were significantly greater in females on the VLED (p < 0.01), however, differences in rate of change of WC and HC between dietary interventions did not reach significance (Table 2). Females on the GD showed statistically significant reductions from baseline in %FM (− 0.23%/month), total FM (− 0.60 kg/month) and concomitant increases in %LM (0.23%/month), however, the absolute decrease in LM did not reach significance. Females on the VLED had statistically significant reductions in both FM and LM (− 1.2 and − 0.35 kg/month), however, changes in %FM and %LM were not significant. None of the observed decreases in BP were significant for females in either dietary intervention, with the exception of the reduction of SBP in VLED participants (− 1.5 mmHg/month), a significantly greater reduction than that observed in the GD group (p < 0.05). The highest weight loss among women on the VLED was − 21.4% (11 months after initial visit), and maximum weight loss among women on the GD was − 39.8%, at 12 months after initial visit (Fig. 2).
Effectiveness of exercise physiology intervention
Independent sample t tests were performed to determine if anthropometric, body composition, or BP changes differed significantly between those who saw the exercise physiologist and those who did not. No significant differences were noted in the primary outcome of percent weight loss between those who saw the exercise physiologist after three and six visits [mean (sd) of − 3.4% (3.7%) and − 6.0% (6.6%)] and those who did not [− 3.4% (4.6%) and − 7.4% (6.2%)]; p > 0.05. No significant between-group differences were detected in any secondary outcomes (p > 0.05).
Clinically significant weight loss
The number of participants who achieved CSWL within a 12-month period was assessed. Ninety-one (33.0%) participants did not attend a second appointment, and were excluded from this analysis. Of the 185 attenders, 145 (78.4%) demonstrated a loss of weight from their first to final clinic visit. Fifty-seven participants achieved CSWL, accounting for 30.8% of attenders and 39.8% of participants who lost weight.
Discussion
This study demonstrates barriers faced by patients and clinicians in outpatient weight management, particularly low attendance and retention rates. Regular attenders were older, a finding observed in similar studies [25], attributed to greater motivation and compliance [26]. At baseline, VLED participants were significantly larger in a number of anthropometric and body composition measures than their GD counterparts, consistent with guidelines for prescription of VLEDs to class III obese patients [BMI ≥ 40 kg/m2, as per National Institute for Health and Care Excellent (NICE) guidelines [27]], or those with a clinically assessed need to rapidly lose weight. This necessitated the division of groups by gender and dietary intervention, resulting in uneven distribution of dietary intervention within both genders that had implications for statistical analysis. Results showed that men had greater weight loss success on the GD than on the VLED, contradicting our initial hypothesis. Interestingly, males on the VLED gained %FM, in contrast to previous research performed under controlled conditions [19, 20]. These differences may be explained by poorer compliance on the VLED, or by uneven groups and larger baseline values preventing changes from reaching statistical significance. In women, both dietary interventions demonstrated statistically significant reductions in weight loss indices; those on the VLED demonstrated significantly greater reductions in BW, BMI and SBP than those on the GD, in line with previous research [28] and in agreement with the hypothesis of this study. Compliance may have been better in female VLED participants, as weight loss was greater compared to males; however, a larger study population would be needed to determine causes of this effect. The hypothesis that patients who consulted with an exercise physiologist would exhibit greater weight loss than those who did not was not confirmed in this study, necessitating further investigation. No significant differences with respect to exercise were observed between groups for any anthropometric or body composition parameters, however, due to the small study population, the range of statistical analyses that could be performed was limited.
Higher rates of weight loss were observed in this study compared to the previous literature [25, 26], likely attributable to larger baseline values of study participants, as those with higher baseline weights typically lose weight at a faster rate than those with lower starting weights [29]. In the current study, CSWL observed in attenders was 30.8%, a rate higher than initially expected and consistent with controlled trials [11, 15]. CSWL has been shown to produce significant improvements in clinical parameters and comorbidities in a growing body of the literature [13, 16], supporting recommendations to encourage assessment of successful weight loss interventions by such measures, in addition to traditional anthropometric and body composition changes. The only clinical parameter measured in our study was BP; SBP was significantly reduced in males on the GD and in females on the VLED, a finding well documented in the weight loss literature [30].
This study is not without limitations. The study was designed to evaluate an outpatient obesity clinic without restrictions of a controlled trial, and control and randomly allocated groups were not viable due to significant differences between gender and dietary intervention groups at baseline, resulting in an uneven yet representative distribution of patients across intervention groups. The non-trial nature of this study limited the statistical analyses that could be performed and high attrition rates, a result of self-directed attendance, prevented long-term follow-up. Though weight re-gain is common [4, 17], assessment of this was limited by the attrition rate (Fig. 2). Further, the use of BIA for body composition analysis, although previously validated in obese populations [31] has been shown to be less valid in certain ethnic populations, necessitating specific calibration equations [32] that were not able to be used in our clinic, which serves an ethnically diverse population; therefore, results of BIA should be interpreted with caution. Women were overrepresented in our population, an issue common in weight loss studies. Australian data from the National Health Survey 2014–2015 [2] reported that 70.8% of men were overweight or obese, compared with 56.3% of women, and attributed to lower referral rates of males, or reluctance to attend weight loss clinics [25]. Finally, VLEDs work by defined and marked limitation of energy intake, and have the benefit of anorectic effect of ketosis when energy restriction is significant [33]. Failure of participants on the VLED to maintain full meal replacements may be a reason for relatively poor response in men, and less so in women.
Behavioural modifications, in addition to diet and exercise changes, are essential in addressing weight management, producing an average weight loss between 4.8–5.1% [8, 10, 12] and achievement of CSWL in 20–61% of participants [7, 13, 15]. While our study did not specifically address behavioural modification, all clinicians included some aspect of behavioural modification within their discipline. In the future, multidisciplinary clinics should consider providing direct psychological support for patients that require more intensive behavioural intervention to support weight loss efforts. Considering the benefit of achieving CSWL, other clinics may consider this a measure of weight loss success, particularly in light of high rates of comorbidities seen in morbidly obese individuals. In our study, VLED participants had a shorter median length of attendance than GD participants, likely reflective of the difficulty of adjusting to a VLED and cost associated with meal replacements. However, participants on a VLED had higher retention (attendance at 12 months after initial visit). These patients were likely more motivated, perhaps after observing larger initial weight loss. While low retention rates likely impacted upon study findings, this issue highlights one of the greatest barriers to effective management of obesity in free clinics and should be monitored to ensure patients are receiving adequate and appropriate treatment. Figure 2 illustrates the variability of individual weight loss trajectories and patterns of weight re-gain over time. Failure to achieve or maintain weight loss likely plays a major role in participants’ decisions to maintain changes in their behaviour, reflected in the high attrition rates in our study. Results from our study support previous suggestions to consider screening patients prior to attending weight management clinics, to assess readiness to change and prioritise patients who may benefit more from intervention, potentially leading to improved cost-effectiveness [26]. Low SES and ethnicity have been shown to correlate with overweight and obesity in Australian adults [34]. Although information pertaining to SES and ethnicity were not collected in our study, WSLHD serves an ethnically diverse population with higher rates of socioeconomic disadvantage compared to national and state averages [22], placing this population at increased risk of obesity, reflected in high rates of overweight and obesity from recent statistical data [35]. A number of socioeconomic and behavioural factors act as barriers to successful weight loss and maintenance, particularly for those on a VLED. Costs of purchasing VLED meal replacements can be prohibitive and participants can miss out on the social aspects of eating, affecting adherence to VLEDs. Other factors that may influence adherence to weight loss programs include basic nutrition and cooking skills, lack of accountability [36], and time and cost of attending self-directed clinic visits, particularly for those with limited access to transport. Finally, this clinic imposes little exclusion for attendance, contrary to most controlled trials. Inclusion of non-English speaking individuals and those with comorbid conditions may also account for low retention and attendance rates and ultimately weight loss, although to what degree is unknown. Addressing obesity in these vulnerable populations is essential, as these populations face the greatest barriers to weight management and are at greatest risk of obesity [17]. Rather than excluding such patients, clinics should adapt interventions to be inclusive and specific for successful weight management, or refer such patients to programs where weight management can be addressed appropriately.
This study adds to the growing literature assessing the effectiveness of outpatient obesity clinics not under traditional study conditions, and findings from this study should help to direct future research and development for resources for this burgeoning area.
References
WHO (2016) Obesity and overweight fact sheet. Updated June 2016. http://www.who.int/features/factfiles/obesity/facts/en/index1.html
Australian Bureau of Statistics (2015) National health survey: first results, 2014-15. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.001~2014-15~Main%20Features~Overweight%20and%20obesity~22. Accessed 4 Sept 2017
Bertakis KD, Azari R (2005) Obesity and the use of health care services. Obes Res 13(2):372–379. doi:10.1038/oby.2005.49
Bischoff SC, Damms-Machado A, Betz C, Herpertz S, Legenbauer T, Low T et al (2012) Multicenter evaluation of an interdisciplinary 52-week weight loss program for obesity with regard to body weight, comorbidities and quality of life—a prospective study. Int J Obes 36(4):614–624. doi:10.1038/ijo.2011.107
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K et al (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292(14):1724–1737. doi:10.1001/jama.292.14.1724
Australian Institute of Health and Welfare (2011) Obesity and injury in Australia: a review of the literature. Australian Institute of Health and Welfare, Canberra, Australia
Gallagher R, Kirkness A, Zelestis E, Hollams D, Kneale C, Armari E et al (2012) A randomised trial of a weight loss intervention for overweight and obese people diagnosed with coronary heart disease and/or type 2 diabetes. Ann Behav Med 44(1):119–128. doi:10.1007/s12160-012-9369-2
Giel KE, Binkele M, Becker S, Stubler P, Zipfel S, Enck P (2008) Weight reduction and maintenance in a specialized outpatient health care center. Obes Res Clin Pract 2(3):I–II. doi:10.1016/j.orcp.2008.02.001
Lantz H, Peltonen M, Agren L, Torgerson JS (2003) A dietary and behavioural programme for the treatment of obesity. A 4-year clinical trial and a long-term posttreatment follow-up. J Intern Med 254(3):272–279
Malone M, Alger-Mayer SA, Anderson DA (2005) The lifestyle challenge program: a multidisciplinary approach to weight management. Ann Pharmacother 39(12):2015–2020. doi:10.1345/aph.1G287
Morrison DS, Boyle S, Morrison C, Allardice G, Greenlaw N, Forde L (2012) Evaluation of the first phase of a specialist weight management programme in the UK National Health Service: prospective cohort study. Public Health Nutr 15(1):28–38. doi:10.1017/s1368980011001625
Osland EJ, Powell EE, Banks M, Jonsson JR, Hickman IJ (2007) Obesity management in liver clinics: translation of research into clinical practice. J Gastroenterol Hepatol 22(4):504–509. doi:10.1111/j.1440-1746.2006.04830.x
Ryan DH, Johnson WD, Myers VH, Prather TL, McGlone MM, Rood J et al (2010) Nonsurgical weight loss for extreme obesity in primary care settings: results of the Louisiana obese subjects study. Arch Intern Med 170(2):146–154. doi:10.1001/archinternmed.2009.508
Spanos D, Hankey C, Boyle S, Melville C (2014) Comparing the effectiveness of a multi-component weight loss intervention in adults with and without intellectual disabilities. J Hum Nutr Diet 27(1):22 –29. doi:10.1111/jhn.12051
Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI et al (2011) A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med 365(21):1969–1979. doi:10.1056/NEJMoa1109220
St George A, Bauman A, Johnston A, Farrell G, Chey T, George J (2009) Effect of a lifestyle intervention in patients with abnormal liver enzymes and metabolic risk factors. J Gastroenterol Hepatol 24(3):399–407. doi:10.1111/j.1440-1746.2008.05694.x
Mauro M, Taylor V, Wharton S, Sharma AM (2008) Barriers to obesity treatment. Eur J Intern Med 19(3):173 –180. doi:10.1016/j.ejim.2007.09.011
Edye M, Talbot ML (2014) Inequalities of access to bariatric surgery in Australia. Med J Aust 201(9):502–503
Beavers KM, Beavers DP, Nesbit BA, Ambrosius WT, Marsh AP, Nicklas BJ et al (2014) Effect of an 18-month physical activity and weight loss intervention on body composition in overweight and obese older adults. Obesity 22(2):325–331. doi:10.1002/oby.20607
Kulovitz MG, Kolkmeyer D, Conn CA, Cohen DA, Ferraro RT (2014) Medical weight loss versus bariatric surgery: does method affect body composition and weight maintenance after 15% reduction in body weight?. Nutrition 30(1):49–54. doi:10.1016/j.nut.2013.06.008
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Med Assoc 310(20):2191–2194
WSLHD (2014) Western Sydney local health district about us. http://www.wslhd.health.nsw.gov.au/About-Us. Accessed 28 May 2014
National Health and Medical Research Council (2003) The Australian dietary guidelines. National Health and Medical Research Council, Canberra
Stewart A, Marfell-Jones M, Olds T, de Ridder H (2011) International standards for anthropometric assessment. International Society for the Advancement of Kinanthropometry, Underdale, SA
Brook E, Cohen L, Hakendorf P, Wittert G, Thompson C (2014) Predictors of attendance at an obesity clinic and subsequent weight change. BMC Health Serv Res 14:78–78. doi:10.1186/1472-6963-14-78
Hickson M, Macqueen C, Frost G (2009) Evaluation of attendance and weight loss in an intensive weight management clinic compared to standard dietetic care. J Hum Nutr Diet 22(1):72–76. doi:10.1111/j.1365-277X.2008.00927.x
National Institute for Health and Care Excellence (2006) Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children CG43. National Institute for Health and Care Excellence, London
Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W et al (2007) Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 107(10):1755–1767. doi:10.1016/j.jada.2007.07.017
Finkler E, Heymsfield SB, St-Onge M-P (2012) Rate of weight loss can be predicted by patient characteristics and intervention strategies. J Acad Nutr Diet 112(1):75–80. doi:10.1016/j.jada.2011.08.034
Tuck ML, Sowers J, Dornfeld L, Kledzik G, Maxwell M (1981) The effect of weight reduction on blood pressure, plasma renin activity, and plasma aldosterone levels in obese patients. N Engl J Med 304(16):930–933. doi:10.1056/nejm198104163041602
Ling CH, de Craen AJ, Slagboom PE, Gunn DA, Stokkel MP, Westendorp RG et al (2011) Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin Nutr 30(5):610–615. doi:10.1016/j.clnu.2011.04.001
Dehghan M, Merchant AT (2008) Is bioelectrical impedance accurate for use in large epidemiological studies? Nutr J 7:26. doi:10.1186/1475-2891-7-26
Delbridge E, Proietto J (2006) State of the science: VLED (very low energy diet) for obesity. Asia Pac J Clin Nutr 15 Suppl:49–54
Brennan SL, Henry MJ, Nicholson GC, Kotowicz MA, Pasco JA (2010) Socioeconomic status, obesity and lifestyle in men: the Geelong osteoporosis study. J Men’s Health 7(1):31–41. doi:10.1016/j.jomh.2009.10.004
Health statistics New South Wales—overweight or obesity by LHD and year. NSW Ministry of Health, Sydney, New South Wales, Australia. http://www.healthstats.nsw.gov.au/Indicator/beh_bmi_age/beh_bmi_lhn?filter1ValueId=&filter2ValueId=. Accessed 30 May 2014
Metzgar CJ, Preston AG, Miller DL, Nickols-Richardson SM (2015) Facilitators and barriers to weight loss and weight loss maintenance: a qualitative exploration. J Hum Nutr Diet 28(6):593–603. doi:10.1111/jhn.12273
Acknowledgements
We thank the staff at the Westmead Hospital University Clinic and Medical Record Department for providing their assistance with data measurement and collection.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows: RV, CB, AC and JM conducted research; RV, CB and KB analysed data; RV wrote the paper; all authors edited the final manuscript; AC and CB designed the research and had primary responsibility for final content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Venchiarutti, R.L., Byth, K., Marks, J.L. et al. Comparing the effectiveness of general dietary advice versus a very low energy diet in an obese outpatient population in Australia. Eat Weight Disord 24, 739–747 (2019). https://doi.org/10.1007/s40519-017-0443-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-017-0443-4