Abstract
Introduction
There may be shared neuropsychological dysfunctions in ADHD and obesity. This study tested a neuropsychological model of ADHD (reward/executive dysfunctioning) in individuals with obesity. Furthermore, the association between co-morbid binge eating and reward/executive dysfunction was explored.
Methods
Reward/executive dysfunctioning was assessed using both neuropsychological measures and questionnaires in individuals (aged 17–68) with obesity (N = 39; mean BMI = 39.70) and normal weight (N = 25; mean BMI = 22.94).
Results
No significant differences emerged between individuals with and without obesity on the outcome measures. However, individuals with obesity and binge eating showed significantly more self-reported delay discounting and inattention than those individuals with obesity but without binge eating. When controlling for inattention, this difference in delay discounting was no longer significant.
Discussion
Not obesity alone but obesity with binge eating was specifically associated with a mechanism often reported in ADHD, namely delay discounting. However, this effect may be more driven by inattention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Increasing evidence shows a significant association between attention-deficit/hyperactivity disorder (ADHD) and obesity [1], suggesting that potential shared psychopathological mechanisms underlying both. Knowledge of common neuropsychological deficits may give clues towards more effective treatments, as treatment can be tailored to the specific psychopathological needs [2]. ADHD is a heterogeneous disorder, with multiple neuropsychological pathways proposed towards ADHD behavior [3]. A classical neuropsychological model of ADHD is the dual pathway model; it proposes two intertwined but separable neuropsychological pathways towards ADHD behavior; i.e., a failing cognitive functioning and an altered motivational/reward-related pathway [4]. The dysfunctional cognitive functioning pathway is mainly characterized by deficits in inhibition and working memory [4]. The motivational pathway is characterized by an altered reward sensitivity, leading to high preferences for small immediate reward over later larger reward (temporal reward or delay discounting) and an aversion of delay-related situations (delay aversion) [4]. In ADHD samples, extensive research has shown deficits in both pathways both on performance-based neuropsychological measures and questionnaires [5, 6].
Far less research is conducted within samples of individuals with obesity, although evidence is reported for both reward-related deficits (most consistent evidence for delay discounting [7]) and executive functioning deficits [8] in individuals with obesity as compared to individuals without obesity. However, to our knowledge, both types of deficits underlying ADHD behavior have not been measured within one study in an adult sample of individuals with obesity using a multi-method assessment with both performance-based and self-report measures.
In addition, binge eating, defined as recurring episodes of eating significantly more food in a short period of time than most people would eat under similar circumstances, with episodes marked by feelings of lack of control [9], may play a role in the link between obesity and ADHD. A subsample of individuals with obesity is characterized by binge eating, with those with binge eating often having more internalizing and externalizing co-morbidity [10]. Because characteristics of binge eating are similar to the impulsive self-control deficits implicated in ADHD, the assumed common neuropsychological deficits may be more pronounced in this subgroup than in those with obesity without binge eating [11]. However, evidence is still inconsistent. Binge eating has been associated with inhibitory and working memory deficits [12] and deficits on the reward-related pathway in delay discounting [13], but although some find differences between those with binge-eating disorder as compared to the broader obese sample [13], others did not find the assumed differences between binge eaters and non-binge eaters [14]. This highlights the potential importance of taking into account co-morbid binge eating when conducting studies on obesity.
In sum, this study explored differences between individuals with and without obesity on reward and executive functioning pathways and differences within the individuals with obesity between those with and without binge eating. We expected differences on both pathways between individuals with and without obesity, with more pronounced differences in the individuals with obesity and binge eating as compared to those without binge eating. In addition, we checked whether these differences remained after controlling for ADHD symptomatology.
Methods
Participants
Our original sample consisted of 43 patients with obesity and 30 age/gender-matched healthy controls. The individuals with obesity consulted a local hospital for bariatric surgery. Five healthy controls were eliminated from the sample because of self-reported presence of binge eating on the Eating Disorder Examination Questionnaire (EDEQ) binge-eating item and four individuals with obesity were removed due to missing data on the EDEQ [15] binge-eating item (see instruments). Thus, the final sample consisted of 25 healthy controls (72% females) and 39 individuals with obesity (82.1% females) with no significant gender differences [Χ 2 (1) = 0.90, ns]. The mean age of the healthy controls and individuals with obesity was, respectively, 44.92 years (SD = 15.32) and 42.82 (SD = 13.23) (group difference not significant [F(1, 62) = 0.34, ns]). The mean BMI of the healthy controls (M = 22.94, SD = 1.43) was significantly lower [F(1,62) = 236.59, p < .001] than the BMI of the individuals with obesity (M = 39.70; SD = 5.31).
Instruments
Eating disorder psychopathology was assessed using the Eating Disorder Inventory-2 (EDI-2 [16]) subscales [Drive for Thinness (α = 0.85), Bulimia (α = 0.89), and Body Dissatisfaction (α = 0.95)] and the Eating Disorder Evaluation Questionnaire (EDEQ [12]) [Eating (α = 0.70), Weight (α = 0.85), Shape (α = 0.93), and Restraint (α = 0.66)]. To assess binge-eating behavior, we used the binge-eating item of the EDEQ.
Motivational reward sensitivity was assessed by means of the Reward Responsiveness Scale of the Behavioral Inhibition and Behavioral Activation (BISBAS) scales [17] (α = 0.57, n = 5) (sample item “When I see an opportunity for something, I get excited right away”) and a performance-based measure, the IOWA Gambling Task [18], with as outcome the total net score. The higher the score on both tasks, the more reward sensitivity. The Quick Delay Questionnaire (QDQ [19]), measured delay aversion (α = 0.69, n = 5) (sample item “Having to wait for things makes me feel stressed and tense”) and delay discounting (α = 0.64, n = 5) (sample item “I try to avoid tasks that will only benefit me in the long term and do not have any immediate benefits”).
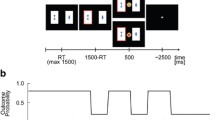
To assess cognitive functioning, we administered the Stop-Signal Paradigm of Logan [20], a performance-based measure of inhibitory control, and used the Stop-Signal Reaction Time (SSRT) as outcome. The higher the SSRT, the more problems in prepotent response inhibition. The Chessboard Working Memory Task [21] is a performance-based measure of visuospatial working memory capacity. The higher the score, the better the working memory capacity.
Finally, ADHD symptomatology was assessed by the Dutch version of the adult ADHD rating scale [22], total score (α = 0.80, n = 23), and its subscales Inattention (α = 0.76, n = 11) (sample item “I am easily distracted”) and Hyperactivity/Impulsivity (α = 0.69, n = 12) (sample item “I answer before questions are finished”). The majority of subscales reach satisfactory internal consistency; two subscales have, potentially due to a small number of items, more questionable internal consistency.
Analyses
Mean differences in self-report and performance-based measures were compared using MANOVAs (p value 0.05/SPSS) with (a) healthy controls vs. individuals with obesity, and (b) obesity with and without self-reported binge eating on the EDEQ as independent variables and measures of reward and cognitive functioning as dependent variables. Two series of MANOVAs were performed: (1) without controlling and (2) while controlling for the impact of ADHD symptomatology.
Results
Group characteristics
Compared to controls, the individuals with obesity scored significantly higher on the three EDI-2 [16] subscales [Drive for Thinness, Bulimia, Body Dissatisfaction] [Wilks’Lambda = 0.36, F(3,58) = 34.42, p < .001] and on three of the EDEQ [15] subscales [Eating, Weight, Shape concerns, except Restraint] [Wilks’Lambda = 0.40, F(4,59) = 22.19, p < .001].
Within the individuals with obesity, 30.8% (n = 12) of the individuals reported binge eating, whereas 69.2% (n = 27) did not. No significant gender [Χ 2 (1) = 1.09, ns], age [F(1,37) = 0.02, ns], nor BMI differences [F(1,37) = 0.56, ns] were detected between individuals with obesity and binge eating and those with obesity but without binge eating. Only on the Bulimia subscale of the EDI-2 [16], those with binge eating scored significantly higher and the other EDEQ/EDI subscales did not differ.
Outcome
No significant differences between healthy controls and individuals with obesity on any of the outcomes (behavioral inhibition, visual spatial working memory, reward sensitivity, delay aversion, delay discounting, ADHD inattention, ADHD hyperactivity, and ADHD total) were found (Table 1).
However, the comparison between individuals with obesity and binge eating and those with obesity but without binge eating showed significant differences (Table 2); those with binge eating as determined by their score on the EDEQ binge eating item scored significantly higher on Delay Discounting and the ADHD inattention scale compared to those without (Cohen’s ds >0.80: large effect sizes). However, this significant difference between individuals with obesity and binge eating and those with obesity but without binge eating on Delay Discounting disappeared after controlling for Inattention symptoms (this result is not presented in Table 2).
Discussion
In our study, despite the use of well-validated multi-method assessment of multiple concepts and the selection of a sample with obesity and a matched control group, individuals with obesity showed no differences on the assumed neuropsychological deficits as compared to individuals without obesity.
In contrast, individuals with obesity and self-reported binge eating (on the EDEQ item) showed more self-reported delay discounting than those without binge eating, suggesting some evidence that there are shared mechanisms towards both ADHD and obesity with binge eating. This possible common mechanism is further qualified by the differences on the ADHD measure ‘inattention’ with higher scores for individuals with obesity and binge eating. However, when controlling for inattention, symptom differences in delay discounting disappeared, suggesting that the differences in delay discounting, observed between the two groups, may be more related to inattention symptomatology than the self-reported binge eating in itself.
Several explanations can be put forward for these findings. As with neuropsychological deficits of ADHD [21], neuropsychological deficits of obesity and binge eating may be heterogeneous with some, but not all individuals displaying executive and others displaying mainly reward-related deficits. As such, the sample size of our study may be too small to detect group differences on both domains.
This lack of differences may also be related to our assessments. In contrast to the more primary deficits in cognition and motivation in ADHD, for obesity and binge eating, these deficits may be more secondary and only become triggered and dysfunctional when food-related cues are used [12]. Nevertheless, despite the usage of non-food-related questions, individuals with obesity and binge eating did report worse on delay discounting, suggesting that for these individuals, targeting delay discounting and related inattention may be useful, for example, by exploring the utility of interventions that have proven effectiveness for ADHD [1].
Somewhat surprising, in this study sample, individuals with obesity and binge eating score significantly higher on inattention symptoms compared to individuals without binge eating; whereas they do not differ on the impulsivity/hyperactivity symptoms. However, other studies also found binge eating to be correlated with inattention and not with impulsivity [10, 24]. One explanation is that in contrast to inattention, impulsivity is not a homogeneous phenomenon, so the scales that measure impulsivity in ADHD do not measure the same in eating disorders, and vice versa [24].
Results should be interpreted within the context of our sample and assessments, the sample size was limited and especially males were underrepresented in the sample of individuals with obesity and binge eating, and thus, potential gender differences could not be explored. Therefore, our pilot study needs replication in a larger sample.
Furthermore, we determined our subgroup of individuals with binge eating by their score on an item of the EDEQ and not a broader assessment of binge eating, as such we cannot determine if they met full criteria of binge-eating disorder. In future research, it would be good to include a broader assessment of binge eating symptomatology (e.g., clinical interview). In addition, ADHD symptomatology was based on self-report and not officially diagnosed. Furthermore, without a subgroup with only binge-eating but not obesity, we cannot make any firm conclusions about the effects of binge eating on delay discounting on its own. Future studies should include such a subgroup to clarify the role of binge eating in obesity.
In sum, delay discounting, one aspect of the dual pathway model of ADHD was deficient in individuals with obesity and binge eating, but not in those with obesity without binge eating. However, this effect may be more driven by the associated ADHD symptomatology than by binge eating alone.
References
Cortese S, Comencini E, Vincenzi B, Speranza M, Angriman M (2013) Attention-deficit/hyperactivity disorder and impairment in executive functions. A barrier to weight loss in individuals with obesity? BMC Psychiatry 13:286. doi:10.1186/1471-244X-13-286
Sonuga-Barke EJS, Halperin JM (2010) Developmental phenotypes and causal pathways in attention deficit/hyperactivity disorder: potential targets for early intervention? J Child Psychol Psychiatry 51:368–398. doi:10.1111/j.1469-7610.2009.02195.x
Coghill D, Seth S, Matthews K (2014) A comprehensive assessment of memory, delay aversion, timing, inhibition, decision making and variability in attention deficit hyperactivity disorder: advancing beyond the three-pathway models. Psychol Med 44:1889–2001. doi:10.1017/S0033291713002547
Sonuga-Barke EJS (2003) The dual pathway model of AD/HD: an elaboration of neuro-developmental characteristics. Neurosci Biobehav Rev 27:593–604. doi:10.1016/j.neubiorev.2003.08.005
Luman M, Oosterlaan J, Sergeant JA (2005) The impact of reinforcement contingencies on ADHD: A review and theoretical appraisal. Clin Psychol Rev 25:183–213. doi:10.1016/j.cpr.2004.11.001
Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF (2005) Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry 57:1336–1346. doi:10.1016/j.biopsych.2005.02.006
Caleza C, Yanez-Vico RM, Mendoza A, Iglesias-Linares A (2016) Childhood obesity and delayed gratification behavior: a systematic review of experimental studies. J Pediatr 169:201–207. doi:10.1016/j.jpeds.2015.10.008
Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Penalver C, Rohde LA, Faraone SV (2016) Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry 173:34–43. doi:10.1176/appi.ajp.2015.15020266
Fairburn CG, Wilson (1993) Cognitive treatments for eating disorders. J Consult Clin Psychol 61:261–269
Claes L, Vandereycken W, Vandeputte A, Braet C (2013) Personality prototypes in female pre-bariatric obese patients: do they differ in eating disorder symptoms, psychological complaints, and coping behavior? Eur Eat Disord Rev 21:72–77. doi:10.1002/erv.2188
Davis C, Levitan RD, Smith M, Tweed S, Curtis C (2006) Associations among overeating, overweight, and attention deficit/hyperactivity disorder. A structural equation modelling approach. Eat Behav 7:266–274. doi:10.1016/j.eatbeh.2005.09.006
Voon V (2016) Cognitive biases in binge eating disorder: the hijacking of decision making. CNS Spectr 20, 566–573. doi:10.1017/S1092852915000681
Manwaring JL, Green L, Myerson J, Strube MJ, Wilfley DE (2011) Discounting of various types of rewards by women with and without binge eating disorder. Evidence for general rather than specific differences. Psychol Record 61:561–582
Davis C, Patte K, Curtis C, Reid C (2010) Immediate pleasures and future consequences. A neuropsychological study of binge eating and obesity. Appetite 54:208–213. doi:10.1016/j.appet.2009.11.002
Fairburn CG, Beglin SJ (1994) Assessment of eating disorder psychopathology: interview or self-report questionnaire? Int J Eat Disord 16:363–370
Garner DM (1991) Eating disorder inventory-2: professional manual. Psychological Assessment Resources, Odessa, FL
Carver CS, White TL (1994) Behavioural inhibition, behavioural activation, and affective responses to impending reward and punishment: The BIS/BAS Scales. J Pers Soc Psychol 67:319–333
Bechara A, Damásio AR, Damásio H, Anderson SW (1994) Insensitivity to future consequences following damage to human prefrontal cortex. Cognition 50:7–15
Logan GD, Schachar RJ, Tannock R (1997) Impulsivity and inhibitory control. Psychol Sci 8:60–64
Clare, S., Helps S, Sonuga-Barke EJ (2010) The quick delay questionnaire: a measure of delay aversion and discounting in adults. Atten Deficit Hyperact Disord 2:43–48. doi:10.1007/s12402-010-0020-4
Dovis S, Van der Oord S, Huizenga H, Wiers R, Prins P (2015) Prevalence and diagnostic validity of motivational impairments and deficits in visuospatial short-term memory and working memory in ADHD subtypes. Eur Child Adolesc Psychiatry 24:575–590. doi:10.1007/s00787-014-0612-1
Kooij SJJ, Boonstra MA, Swinkels SH, Bekker EM, de Noord I, Buitelaar JK (2008) Reliability, validity and utility of instruments for self-report and informant report concerning symptoms of ADHD in adult patients. J Atten Disord 11:445–458. doi:10.1177/1087054707299367
De Velasco M, Barduro E, Perez-Templado J, Silveira B, Quintero J (2015) Review of the association between obesity and ADHD. Actas Esp Psiquiatr 43:16–23
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Erlbaum, Hillsdale
Acknowledgements
The authors like to thank An Strauven and Ward Proost of the Obesity Clinic of the General Hospital in Mol and students Eva Van Den Broeck, Charlotte Van Dorst, Fien De Vliegher, and Margaux Gijbels for their help with the data collection and data input.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Saskia van der Oord has received a consultant fee from Janssen Cilag and has received a speaker honorarium from MEDICE and Shire. Talks and consultancy were all on topics related to non-pharmacological treatments. Caroline Braet declares that she has no conflict of interest. Samuel Cortese declares that he has no conflict of interest. Laurence Claes declares that she has no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Van der Oord, S., Braet, C., Cortese, S. et al. Testing the dual pathway model of ADHD in obesity: a pilot study. Eat Weight Disord 23, 507–512 (2018). https://doi.org/10.1007/s40519-017-0375-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-017-0375-z