Abstract
Purpose
Impulsivity might contribute to the development and maintenance of obesity and eating disorders. Patients suffering from binge eating disorder (BED) show an impulsive eating pattern characterized by regular binge eating episodes. Novel behavioral interventions increasing inhibitory control could improve eating behavior in BED. We piloted a novel food-specific inhibition training in individuals with BED.
Methods
N = 22 BED patients according to SCID-I were randomly assigned to three sessions of a training or control condition. In both conditions, pictures of high-caloric food items were presented in peripheral vision on a computer screen while assessing gaze behavior. The training group had to suppress the urge to turn their gaze towards these pictures (i.e., to perform antisaccades). The control group was allowed to freely explore the pictures. We assessed self-reported food craving, food addiction, and wanting/liking of food pictures pre- and post-intervention.
Results
Twenty participants completed the study. The training proved to be feasible and acceptable. Patients of the training group significantly improved inhibitory control towards high-caloric food stimuli. Both groups reported a significantly lower number of binge eating episodes in the last four weeks after termination of the study. No changes were found in food craving, food addiction, liking, and wanting ratings.
Conclusions
A food-specific inhibition training could be a useful element in the treatment of BED and other eating disorders; however, larger efficacy studies in patient samples are needed to investigate the efficacy of this and similar training approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current theoretical frameworks and empirical evidence highlight the role of impulsivity in the development and maintenance of binge eating disorder (BED) [1–3]. Impulsivity is considered to be composed of several sub-domains [4, 5], including a hyper-valuation of rewarding stimuli and difficulties in inhibitory control. Patients suffering from BED show an impulsive eating pattern: they have regular binge eating episodes characterized by subjective loss of control over eating and ingestion of large amounts of food in a brief period of time [6]. Within this binge eating pattern, the two sub-domains of impulsivity might interact [3, 5]: BED patients might perceive food as highly rewarding and hence experience food cravings and find it hard to resist palatable food (i.e., higher reward sensitivity). In a further step, this might lead to spontaneous food intake which becomes disinhibited and is accompanied by a perceived loss of control over eating (i.e., diminished inhibitory control).
Based upon this evidence, novel behavioral interventions targeting impulsive action tendencies have recently been proposed for the treatment of eating disorders [7, 8], including anorexia and bulimia nervosa as well as BED. Besides approaches to optimize planning and goal setting or to modify attentional biases, these interventions also include training approaches to enhance inhibitory control [7–9]. Several inhibitory control tasks have been established, including the stop-signal task, the go/no-go task, and the antisaccade paradigm [9]. These inhibition tasks aim to increase the ability to stop, change, or delay a behavioral response, mainly to an appetitive cue such as food, by exercising the inhibition of a pre-potent behavior [9]. As a putative mechanism of these trainings, it is assumed that repeated response inhibition also affects the motivational component of impulsivity by leading to a devaluation of the appetitive cue [9]. Devaluation entails that the appetitive cue becomes less rewarding. In their recent review and meta-analysis, Jones et al. [9] report on six studies which have investigated stimulus devaluation after an inhibitory control training for appetitive behavior. The meta-analytic comparison did not reveal a significant effect of the inhibition trainings on devaluation of appetitive stimuli. It is important to note that different training approaches and different methods of stimulus evaluation have been used by these studies which could also influence results.
While the stop-signal task and the go/no-go task require a manual response, the antisaccade paradigm is based on oculomotor responses and requires the participant to look as quickly as possible at the opposite direction of a stimulus appearing in peripheral vision [10, 11]. If a novel stimulus appears in peripheral vision, our automatic reaction is to direct our gaze towards this stimulus. Hence, the antisaccade task requires suppressing an undesirable but highly dominant approach behavior and to execute an alternative behavior. In a recent cross-sectional study using an antisaccade task, patients with BED had increased difficulties suppressing gaze shifts towards food stimuli and antisaccade performance was significantly correlated with trait impulsivity [12].
Inhibition tasks led to reduced consumption or choice of food in single-session designs in healthy populations [8, 9]. Eating behavior assessed by these previous studies mainly comprised post-training ad-libitum consumption of food that has previously been integrated in the inhibition training, such as chocolate, crisps, or other snacks, or a choice of different healthy versus unhealthy food. One of these studies investigated a sample of females with frequent chocolate cravings. A chocolate-specific inhibition training facilitated inhibitory control over unwanted chocolate-related urges in this sample [13]. These findings might also encourage the use of a food-specific inhibition training in BED, as affected patients also suffer from recurrent food cravings and loss of control over their eating behavior. However, importantly, no studies using an inhibition training in clinical populations with an eating disorder have been identified by two recent reviews [8, 9]. In a randomized controlled proof-of-concept study, we conducted a pilot evaluation of a food-specific inhibition training based on the antisaccade task in individuals with BED with a main focus on (a) feasibility and acceptability, (b) effects on eating behavior, and (c) effects on devaluation of food stimuli.
Methods
Participants
Participants were recruited via public advertisements and mailing lists. Eligible patients fulfilled a diagnosis of full-syndrome BED according to DSM-5. Exclusion criteria comprised a severe somatic disorder, current substance dependence, psychotic disorder, suicidal crisis, pregnancy or lactation, non-correctable impairments of vision, previous bariatric surgery, intake of psychoactive medication except SSRIs, current attendance of psychotherapy for BED or a structured weight-loss intervention, and insufficient language proficiency.
Food-specific inhibition training
We developed an inhibition training that is based on the antisaccade paradigm.
Each antisaccade trial started with a central fixation cross presented on the computer screen for 1250 ms. Participants were instructed to look at the fixation cross. The cross was followed by a brief blank screen for 200 ms. Subsequently, a food picture was presented either right or left of the screen in slight peripheral vision for 1000 ms. In the classical antisaccade paradigm, participants are instructed to look as quick as possible in the other direction or the exact mirror position of the stimulus as soon as it appears on the computer screen [14]. This means, they are instructed to perform the so-called antisaccade (to look in the opposite direction of a stimulus). The pre-potent reaction to a novel stimulus in peripheral vision is to look at this stimulus, that is, to perform the so-called prosaccade. However, in order to meet task requirements, the participant has to firstly suppress a reflexive prosaccade to the stimulus and to secondly initiate and execute the adequate motor response—the antisaccade [14]. This is why the antisaccade task is considered to address inhibitory control processes.
Food pictures depicted 40 different high-caloric food items that have been classified as preferred “binge food” (e.g., chocolate cake). They were presented in randomized order. The task consisted of 240 trials divided into three blocks. Gaze behavior was assessed using the iView X Hi-Speed Eye Tracking System (SensoMotoric Instruments, Berlin, Germany) with a sampling rate of 500 Hz.
This task was used for both, the training and the control condition, but with different instructions.
Training condition (FIT)
As within the original antisaccade paradigm [10], patients were requested to look as quickly as possible on the other side of the screen upon stimulus onset, that is, to perform an antisaccade. Main outcome in this training condition was the percentage of errors, that is, the percentage of trials with erroneous prosaccades. Patients received a feedback on their error rate after each training session.
Control condition (CC)
Patients of the control condition were requested to let one’s eyes wander across the screen. Main outcome in the control condition was the percentage of prosaccades versus percentage of antisaccades. Patients received a feedback on how often they had looked on the picture and how often they looked away from the picture.
We conducted three sessions of the training/control condition on three different days within 2 weeks. In a fourth session, patients of the control condition received the instructions of the training condition in order to evaluate plasticity of the antisaccade performance and required training dosage.
Assessment and outcomes
Diagnostic assessment
Diagnostic assessments were conducted pre- and post-training by a trained rater and comprised assessment of body weight and height, the SCID-I interview to assess BED diagnosis, and other DSM-IV axis-I disorders as well as the following German versions of validated self-report instruments:
The Eating Disorder Examination (EDE-Q) [15] assesses attitudes and behaviors associated with eating disorders. The EDE-Q comprises 22 items which assess frequency and intensity of the respective variable in the last 28 days. Calculation of a total score and scores of for subscales (restraint, eating concern, weight concern, shape concern) is possible. Internal consistency of the subscales and the global score was acceptable to excellent in a representative German population sample [16].
The Food Craving Questionnaire state-reduced (FCQ-S-r) assesses state properties of food cravings. It comprises 15 items which are answered on a five-point Likert scale (do not agree at all—fully agree). The three subscales reflect lack of control, reinforcement, and hunger. The validation study showed high internal consistency of the FCQ and confirmed construct validity [17].
The Yale Food Addiction Scale (YFAS) [18] assesses addiction-like eating of palatable foods based on the seven diagnostic criteria for substance dependence in DSM-IV. It comprises 27 items which are predominantly answered on a five-point Likert scale assessing frequencies, and some items require yes/no answers. The YFAS has a single-factor structure. A total score reflecting symptom severity can be calculated, and there is a cut-off score for the classification of food addiction. The YFAS has shown satisfactory internal consistency and good construct validity.
Patients were asked to fill in a questionnaire assessing acceptability and feasibility of the training, using response categories on a 5-point Likert scale (not at all—very much). This questionnaire was custom-made and adapted from a psychotherapy evaluation questionnaire previously used [19]. Items comprised topics such as subjective need/interest in such a training, expectations associated with training participation, detailed questions about effects of the training on eating behavior, overall satisfaction with the training, and with specific aspects of the training sessions.
Training outcomes
We chose the number of binge eating episodes in the last 4 weeks as main outcome of the proof-of-concept study, as this characterizes the core psychopathology of BED. This was assessed using item 22 of the EDE-Q in a telephone follow-up assessment four weeks after termination of study participation. Secondary outcomes comprised food craving using the FCQ-S-r and aspects of food addiction using the YFAS.
Assessment of wanting and liking of food pictures
In order to investigate the effects of the training on devaluation of food stimuli, patients rated wanting and liking of food picture pre- and post-training according to Berridge [20].
Procedure
After screening for eligibility, patients were invited for a first appointment that included receipt of written consent, diagnostic assessment, and the assessment of wanting and liking of food pictures. Patients were randomly assigned to either receive the training or the control condition. Patients were blind with respect to the condition they received. Within the following two weeks, each patient completed the three training/control sessions and the fourth session assessing antisaccade performance in both patient groups. Patients were instructed to abstain from eating and smoking three h ahead of each session and reported on hunger and mood directly before and after each session. In the last session, patients filled in the FCQ-S-r and the YFAS, and performed again the rating of wanting and liking of food pictures. Four weeks after termination of the study, number of binge eating episodes in the last four weeks was assessed via telephone.
Ethical standards
This study was approved by the Ethics Committee of the Medical Faculty Tübingen. All participants gave written informed consent.
Trial registration
This trial is registered at the German Clinical Trials Register (DRKS00006566).
Statistical analyses
Potential group differences in baseline sample characteristics were analyzed using t tests for independent groups. Potential training effects were analyzed using repeated measures analyses of variance with group as between-subject factor and time as within-subject factor. Potential training effects in antisaccade performance within groups were analyzed using paired sample t tests. Statistical significance was defined as α = 0.05.
Results
Sample characteristics
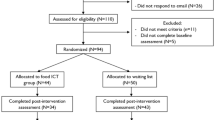
Twenty-six patients were enrolled into the study. Four patients dropped out after the diagnostic session. Twenty-two patients were randomized and in each parallel arm, one patient dropped out before terminating the training. Patients dropping out did not differ from the patients completing the study regarding BMI and number of binge eating episodes; however, they were significantly younger than those terminating the study (23.3 ± 3.3 vs. 36.6 ± 11.9 years). Twenty patients completed the study. The group had an average age of 36.6 ± 11.9 years, an average BMI of 29.6 ± 6.3 kg/m², and an average EDE-Q total score of 3.4 ± 10. There were no significant group differences at baseline for demographic or clinical variables.
Training performance
Patients of the control condition looked significantly more often on food pictures than patients of the training condition at all three sessions (Fig. 1; F(1,18) = 23.15; p < 0.01). Patients of the training group showed a markedly larger intra-group variance in performance as indicated by a larger standard deviation (Fig. 1). Patients of the training group reduced their error rates significantly from session 1 to session 2 (t(9) = 2.36; p < 0.05) and remained stable to session 3, while patients of the control condition remained stable from session 1 to session 2 and significantly reduced their gaze shifts to food pictures from session 2 to session 3 (t(9) = 2.5; p < 0.05).
Feasibility and acceptability of the training
Four patients dropped out before the training started and two patients did not complete the three training sessions. Patients completing the training condition (n = 10) reported high satisfaction with the training (4.1 ± 1.2), and were rather willing to recommend the training (3.7 ± 1.2) and to participate again (3.6 ± 1.3). Patients of the control group rated their experience in a similar way with respect to satisfaction (4.5 ± 0.5), willingness to recommend study participation (3.7 ± 1.1), and to participate again (3.6 ± 1.2). Acceptance ratings did not significantly differ between groups (p > 0.05).
Training outcomes
Patients of both groups reported a significantly lower number of binge eating episodes in the last four weeks after termination of the training (Table 1). No changes were found with respect to secondary outcomes (food craving and food addiction) (Table 1).
Wanting and liking of food pictures
No changes were found regarding ratings of wanting and liking of food pictures (Table 1).
Discussion
In the present randomized controlled proof-of-concept study, we conducted a pilot evaluation of three sessions of a food-specific inhibition training based on the antisaccade task in individuals with BED. Twenty participants completed the study. They represented a clinical group as indicated by an average high binge eating frequency and a BED diagnosis recognized via the SCID-I. Low drop-out rate and a positive patient feedback indicate that the training is both feasible and acceptable. Patients of the training group initially showed significant inhibitory control impairments with error rates similar to those previously reported in BED patients [12]; however, they were able to significantly reduce error rates and increase food-related inhibitory control over three training sessions. Surprisingly, the control group reduced prosaccades towards food as well. Four weeks after termination of the study, patients of both groups reported a significantly lower number of binge eating episodes in the last four weeks, indicating that study participation irrespective of group affiliation might have had a positive effect on eating behavior. Our finding is in line with previous evidence from healthy participants: in most of these previous studies, already a single session of a food-specific inhibition training that was based on stop-signal or go/no go procedures resulted in reduced food intake or healthier choices immediately after the training session [8]. However, only one study has assessed longer-term effects of such a training, looking at weight loss four weeks after the training, but found no significant effects [21].
We found no effects with respect to food craving and food addiction. None of the previous studies in healthy populations has assessed food addiction and only few have assessed food craving, and they report baseline data only [22, 23]. However, this might be due to limited expected change in these variables over a single training session, and likewise in our study, three sessions might not be sufficient to influence these aspects, especially in a clinical population.
Patients reported no devaluation of food pictures in wanting and liking ratings, which is in line with most previous studies in healthy individuals [9]. Jones et al. in their recent review point out that the approach by which food cues are evaluated (i.e., implicit association tests, Likert scales) might lead to different results regarding stimulus devaluation and that the devaluation hypothesis needs further investigation.
The reduction of prosaccades in the inhibition training and of binge eating episodes in both groups could be due to different methodological or clinical issues, e.g., it might suggest that the chosen control condition was not suitable, i.e., the mere confrontation with high-caloric food stimuli might have activated inhibitory control processes leading to changes in eating behavior or food cue exposure might have led to habituation and extinction. An alternative control condition would have been training of antisaccades towards neutral control stimuli instead of food pictures. Other potential explanations for the observed improvements in both groups might be unspecific effects of any intervention, including expectation effects or effects of heightened self-monitoring of symptoms.
Negative emotions and emotion regulation difficulties closely interact with impulsive eating, especially in BED [24]. An adjacent concept is experiential avoidance which describes the unwillingness to remain in contact with internal events and may lead to a range of avoidant coping strategies. Recently, experiential avoidance has been shown to moderate the relationship between negative emotions and emotional eating in healthy women [25]. These relationships are also of relevance for food-specific inhibition trainings, e.g., patients high in experiential avoidance might refrain from participating in such treatment approaches as they avoid confrontation with disorder-relevant stimuli and negative emotions that might emerge during training sessions.
Limitations
The sample of the present study was small. Only female patients took part in the study, but BED also affects men. Investigating the efficacy of inhibitory control trainings in both sexes is warranted. We have used a range of different food pictures for the inhibition training which represented high-caloric food items that have been classified as preferred “binge food”; however, the training was not adapted to individual (binge) food preferences which might even enhance training outcome. There are different alternative possibilities to design a control condition for inhibition trainings, and the one we have chosen might not have been sufficiently discriminative from the training condition as both groups showed comparable changes in eating behavior.
Conclusion
In a small randomized controlled proof-of-concept study, patients with BED were able to significantly improve inhibitory control towards high-caloric food stimuli over three sessions of an inhibition training based on the antisaccade task. The training proved to be feasible and acceptable. The training and the control group reported a significantly lower number of binge eating episodes in the last four weeks after termination of the study, which might suggest that the control condition had also beneficial effects. Larger efficacy studies in patient samples are needed to investigate the efficacy of this and similar training approaches to influence eating behavior. Potential advancements of the inhibition training include selecting the patient’s individually preferred binge food for training, combination with an impulsivity-focused psychotherapy [26], or non-invasive brain stimulation which could enhance inhibitory control [11].
References
Smith DG, Robbins TW (2013) The neurobiological underpinnings of obesity and binge eating: a rationale for adopting the food addiction model. Biol Psychiatry 73:804–810
Gerlach G, Herpertz S, Loeber S (2015) Personality traits and obesity: a systematic review. Obes Rev 16:32–63
Schag K, Schönleber J, Teufel M, Zipfel S, Giel KE (2013) Food-related impulsivity in obesity and binge eating disorder—a systematic review. Obes Rev 14: 477–495.
Sharma L, Markon KE, Clark LA (2014) Toward a theory of distinct types of “impulsive” behaviors: a meta-analysis of self-report and behavioral measures. Psychol Bull 140:374–408
Dawe S, Loxton NJ (2004) The role of impulsivity in the development of substance use and eating disorders. Neurosci Biobehav Rev 28:343–351
American Psychiatric Association (Ed.) (2013) Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association, Washington, DC
Treasure J, Cardi V, Leppanen J, Turton R (2015) New treatment approaches for severe and enduring eating disorders. Physiol Behav 152:456–465
Turton R, Bruidegom K, Cardi V, Hirsch CR, Treasure J (2016) Novel methods to help develop healthier eating habits for eating and weight disorders: a systematic review and meta-analysis. Neurosci Biobehav Rev 61:132–155
Jones A, Di Lemma LC, Robinson E, Christiansen P, Nolan S, Tudur-Smith C, Field M (2016) Inhibitory control training for appetitive behaviour change: a meta-analytic investigation of mechanisms of action and moderators of effectiveness. Appetite 97:16–28
Antoniades C, Ettinger U, Gaymard B, Gilchrist I, Kristjansson A, Kennard C, John Leigh R, Noorani I, Pouget P, Smyrnis N, Tarnowski A, Zee DS, Carpenter RH (2013) An internationally standardised antisaccade protocol. Vision Res 84:1–5
Giel KE, Schag K, Plewnia C, Zipfel S (2013) Antisaccadic training to improve impulsivity in binge eating disorder. Eur Eat Disord Rev 21:488–492
Schag K, Teufel M, Junne F, Preissl H, Hautzinger M, Zipfel S, Giel KE (2013) Impulsivity in binge eating disorder: food cues elicit increased reward responses and disinhibition. PLoS ONE 8:e76542
Houben K, Jansen A (2015) Chocolate equals stop. Chocolate-specific inhibition training reduces chocolate intake and go associations with chocolate. Appetite 87:318–323
Munoz DP, Everling S (2004) Look away: the anti-saccade task and the voluntary control of eye movement. Nat Rev Neurosci 5:218–228
Hilbert A, Tuschen-Caffier B (2006) Eating disorder examination: deutschsprachige Übersetzung. Verlag für Psychotherapie, Münster
Hilbert A, de Zwaan M, Braehler E (2012) How frequent are eating disturbances in the population? Norms of the eating disorder examination-questionnaire. PLoS ONE 7:e29125
Meule A, Lutz A, Vogele C, Kubler A (2012) Food cravings discriminate differentially between successful and unsuccessful dieters and non-dieters. Validation of the food cravings questionnaires in German. Appetite 58:88–97
Meule A, Vögele C, Kübler A (2012) Deutsche Übersetzung und Validierung der Yale Food Addiction Scale. Diagnostica 58:115–126
Giel KE, Leehr EJ, Becker S, Herzog W, Junne F, Schmidt U, Zipfel S (2015) Relapse prevention via videoconference for anorexia nervosa—findings from the RESTART pilot study. Psychother Psychosom 84:381–383
Berridge KC (2009) ‘Liking’ and ‘wanting’ food rewards: brain substrates and roles in eating disorders. Physiol Behav 97:537–550
Veling H, van Koningsbruggen GM, Aarts H, Stroebe W (2014) Targeting impulsive processes of eating behavior via the internet. Effects on body weight. Appetite 78:102–109
Houben K, Jansen A (2001) Training inhibitory control. A recipe for resisting sweet temptations. Appetite 56:345–349
Lawrence NS, Verbruggen F, Morrison S, Adams RC, Chambers CD (2015) Stopping to food can reduce intake. Effects of stimulus-specificity and individual differences in dietary restraint. Appetite 85:91–103
Leehr EJ, Krohmer K, Schag K, Dresler T, Zipfel S, Giel KE (2015) Emotion regulation model in binge eating disorder and obesity—a systematic review. Neurosci Biobehav Rev 49:125–134
Litwin R, Goldbacher EM, Cardaciotto L, Gambrel LE (2016) Negative emotions and emotional eating: the mediating role of experiential avoidance. Eat Weight Disord. doi:10.1007/s40519-016-0301-9
Schag K, Leehr EJ, Martus P, Bethge W, Becker S, Zipfel S, Giel KE (2015) Impulsivity-focused group intervention to reduce binge eating episodes in patients with binge eating disorder: study protocol of the randomised controlled IMPULS trial. BMJ Open 5:e009445
Acknowledgements
We thank all patients for their participation in the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Giel, K.E., Speer, E., Schag, K. et al. Effects of a food-specific inhibition training in individuals with binge eating disorder—findings from a randomized controlled proof-of-concept study. Eat Weight Disord 22, 345–351 (2017). https://doi.org/10.1007/s40519-017-0371-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-017-0371-3