Abstract
Purpose
To investigate the presence of mood spectrum signs and symptoms in patients with anorexia nervosa, restricting subtype (AN-R) or bulimia nervosa (BN).
Method
55 consecutive female patients meeting DSM-IV criteria for eating disorders (EDs) not satisfying DSM-IV criteria for Axis I mood disorders were evaluated with the Lifetime Mood Spectrum Self-Report (MOODS-SR) and the Mini-International Neuropsychiatric Interview (MINI). The MOODS-SR explored the subthreshold comorbidity for mood spectrum symptoms in patients not reaching the threshold for a mood disorder Axis I diagnosis. MOODS-SR included 161 items. Separate factor analyses of MOODS-SR identified 6 ‘depressive factors’ and 9 ‘manic-hypomanic factors’.
Results
The mean total score of MOODS-SR was significantly higher in BN than in AN-R patients (97.5 ± 25.4 vs 61.1 ± 38.5, respectively; p = 0.0001). 63.6 % of the sample (n = 35) endorsed the threshold of ≥61 items, with a statistically significant difference between AN-R and BN (39.3 % vs 88.9 %; χ 2 = 14.6; df = 1; p = 0.0001). Patients with BN scored significantly higher than AN-R patients on several MOODS-SR factors: (a) MOODS-SR depressive component: ‘depressive mood’ (11.2 ± 7.4 vs 16.0 ± 5.8; p < 0.05), ‘psychomotor retardation’ (5.4 ± 5.6 vs 8.9 ± 3.8; p = 0.003), ‘psychotic features’ (2.0 ± 1.8 vs 4.1 ± 1.6; p = 0.001), ‘neurovegetative symptoms’ (5.0 ± 2.6 vs 7.7 ± 1.7; p = 0.001); (b) MOODS-SR manic/hypomanic component: ‘psychomotor activation’ (4.3 ± 3.6 vs 7.4 ± 3.1; p = 0.002), ‘mixed instability’ (1.0 ± 1.5 vs 2.0 ± 1.6; p < 0.05), ‘mixed irritability’ (2.5 ± 1.8 vs 3.7 ± 1.6; p < 0.05), ‘inflated self-esteem’ (1.1 ± 1.4 vs 2.1 ± 1.6; p < 0.05), and ‘wastefulness/recklessness’ (1.0 ± 1.4 vs 2.0 ± 1.2; p = 0.009).
Conclusions
MOODS-SR identifies subthreshold mood signs/symptoms among patients with AN-R, and BN and with no Axis I comorbidity for mood disorders, and provides a better definition of clinical phenotypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A number of clinical studies document how the comorbidity between mood disorders and anorexia (AN) and bulimia nervosa (BN) are a frequent phenomenon. However, the variability of comorbidity percentages across studies is impressive. The lifetime comorbidity for mood disorders ranges from 24 to 90 % in BN, and from 31 to 88 % in AN [1, 2]. Traditionally, the highest rates of lifetime comorbidity for the ‘unipolar side’ of mood disorders mainly refer to the AN ‘restricter’ subtype (AN-R). The comorbidity for the ‘bipolar side’ (Bipolar I–II Disorders, cyclothymia) is more frequently described in BN [1].
Mood disorder comorbidity complicates course and treatment response of AN, and BN [3, 4], and it is associated with a high risk of suicide attempts [5–7]. Similarly, a negative impact of AN, and BN on the course and treatment response of depressive episodes has been extensively described and recently reaffirmed in a prospective study [8].
The wide range of comorbidity percentages between the two psychopathological areas (from 20 to 90 %) can be only partially explained with the heterogeneity of clinical assessment adopted across the different studies, raising questions about the usefulness of the categorical approach. A dimensional approach, overcoming the unipolar/bipolar dichotomy, has been proposed to improve the phenotypic definition of mood disorders, and to enhance the validity and reliability of comorbidity assessment [9, 10].
In this perspective, we aimed to show the clinical utility of a dimensional mood spectrum assessment in patients with AN, and BN, in the absence of full-blown Axis I comorbidity for unipolar or bipolar disorders. A dimensional approach should allow us to discriminate clinical phenotypes of patients with AN, and BN and comorbid mood spectrum signs and symptoms, with a greater level of specificity than that provided by the stereotypic descriptions of Axis I categories. According to the ‘mood spectrum model’ as originally conceived by Cassano and Colleagues, threshold-level manifestations of unipolar and bipolar mood psychopathology, atypical symptoms and behavioral traits are parts of the same continuum [9]. The ‘mood spectrum’ considers as clinically meaningful both manic/hypomanic and depressive features that may occur throughout the lifetime.
The Mood Spectrum Lifetime Questionnaire (MOODS-SR-Lifetime Version) has been constructed and validated to assess mood spectrum phenomenology, as described in detail elsewhere [11].
To the best of our knowledge, only two studies have documented lifetime mood spectrum symptoms in patients with EDs: the first one on patients with AN assessed with the MOODS-SR [12, 13]; the second on patients with AN, BN, and eating disorders not otherwise specified (EDNOS), evaluated with a previous version of the MOODS-SR, the SCI-MOODS [10]. The aim of the study was to investigate whether signs and symptoms belonging to the realm of the proposed mood spectrum model were present with different psychopathological profiles in patients with AN-R and BN.
Materials and methods
Participants
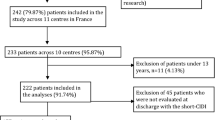
The sample consisted of 55 female patients meeting DSM-IV eating disorders (EDs) criteria, consecutively recruited at the University of Pisa within the framework of a larger Italian Multicenter Study, as described in detail elsewhere [14].
Patients were assessed with the DSM-IV criteria, as data were collected before the publication of DSM-5.
Exclusion criteria were: a primary diagnosis of schizophrenia, schizoaffective disorder, bipolar I or II disorder, unipolar depression; meeting criteria for current alcohol or substance abuse during the last 3 months, severe uncontrolled medical illnesses.
The Ethics Committee of the University of Pisa approved study procedures, as reported elsewhere [14]. All patients signed a written informed consent after receiving a complete description of the study evaluations and procedures.
Instruments
Study participants were administered with the Lifetime Mood Spectrum Self-Report (MOODS-SR) [11], and the Mini-International Neuropsychiatric Interview 5.0.0 (MINI) for DSM-IV diagnoses [15]. Raters who attended a formal training and who were blind to the research questions conducted the MINI interviews.
Interviewer training
All interviewers went through a course of training at the University of Pisa before the start of the study. Raters received instruction on the mood spectrum concept were given an extensive description of the MOODS-SR and the MINI, and were provided with detailed directions for the administration of the interviews. A consulting telephone service was available at the University of Pisa, to answer raters’ questions throughout the study.
MOODS-SR
The MOODS-SR is the lifetime self-report version of the Structured Clinical Interview for Mood Disorders (SCI-MOODS) that demonstrated excellent internal consistency, discriminant validity, inter-rater and test–retest reliability, as described in detail elsewhere [16]. The Kuder–Richardson coefficient, a special form of Cronbach’s alpha for dichotomous items, was used to assess the internal consistency of the SCI-MOODS. Values above 0.70 were assumed to denote good internal consistency. The internal consistency of the domains of the interview, expressed in terms of the Kuder–Richardson coefficient, was high, ranging from 0.79 to 0.92. Correlations of each of the domains with the others ranged from 0.63 to 0.85, indicating a strong inter-relationship among the domains. Agreement between the self-report (MOODS-SR) and the interview formats (SCI-MOODS) was substantial. Intra-class correlation coefficients (ICC) ranged from 0.88 to 0.97, providing a strong support for the reliability of the MOODS-SR questionnaire [11].
The MOODS-SR included 161 items coded as present/absent for one or more periods of at least 3–5 days in the lifetime. For questions exploring temperamental features or the occurrence of specific events, duration was not specified, because it would not be applicable. Separate factor analyses of the depressive and manic components of MOODS-SR identified 6 depressive factors [17] and 9 manic-hypomanic factors [18] ‘Depressive Mood,’ ‘Psychomotor Retardation,’ ‘Suicidality,’ ‘Drug/Illness-Related Depression,’ ‘Psychotic Features,’ and ‘Neurovegetative Symptoms’ were the depressive factors. The factors of mania/hypomania were: ‘Psychomotor Activation,’ ‘Creativity,’ ‘Mixed Instability,’ ‘Sociability/Extraversion,’ ‘Spirituality/Mysticism, ‘Psychotic Features,’ ‘Mixed Irritability,’ ‘Inflated Self-esteem,’ ‘Euphoria,’ and ‘Wastefulness/Recklessness.’
Moreover, a mood spectrum symptom threshold has been defined to lie somewhere below the threshold for diagnosable Axis I bipolar or unipolar disorder. A reliable estimate of the optimal threshold for mood spectrum was obtained by maximizing the sensitivity while keeping at an acceptable level, and the optimal was proposed at the score 61 [11]. However, this cutoff has not yet been validated.
MINI 5.0.0 [15]
The MINI 5.0.0 is a short structured diagnostic interview, developed jointly by psychiatrists and clinicians in the United States and Europe, for DSM-IV and ICD-10 psychiatric disorders. With an administration time of approximately 15 min, it was designed to meet the need for a short but accurate structured psychiatric interview for multicenter clinical trials and epidemiology studies, and to be used as a first step in outcome tracking in non-research clinical settings. The MINI contains 120 questions and screens 17 Axis I DSM-IV disorders for 24 current and lifetime diagnoses. It is organized in diagnostic sections. Using branching tree logic, the interview has two to four screening questions per disorder. Additional symptom questions within each disorder section are asked only if the screen questions are positively endorsed. The MINI has a good correlation with SCID-I and CIDI [15].
Statistical analyses
Demographic and clinical characteristics were compared in patients with AN-R and BN using Chi-square test or T test, as appropriate. Chi-square test was utilized to compare the percentages of subjects who endorsed the proposed items cutoff, in AN-R and BN groups. Student’s T test was utilized to compare the mean age, the depressive, and the manic/hypomanic MOODS spectrum mean scores, in the two diagnostic groups (AN-R vs BN). Pearson’s correlation coefficient was utilized to explore the potential correlations between the manic/hypomanic and the depressive component scores in the overall sample, in the AN-R group and in the BN group.
Two biomedical statisticians (G. M. and S. C.) performed the statistical analyses, using the Statistical Package for Social Sciences (SPSS, version 20.0).
Results
Demographic and clinical characteristics
Study participants included 55 female patients with mean age of 25.2 ± 4.7 years. Twenty-eight patients (50.9 %) met criteria for AN-R (mean age = 25.1 ± 5.3 years, mean BMI = 15.3 ± 1.3 kg/m2), and 27 for BN (mean age = 25.4 ± 4.0 years, mean BMI = 20.7 ± 3.3 kg/m2). Forty-nine patients fulfilled the criteria for a current major depressive episode (MDE) (49/104; 46.6 %), and were excluded from the analyses.
Demographic characteristics of the sample, collected with the MOODS-SR, are described in Table 1. Age at baseline was not significantly different in the two groups. Majority of the patients were not married (74.5 %; 41/55), completed college (63.6; 35/55 %), and were student, unemployed or engaged in home duties (76.3 %; 42/55).
Relationship between depressive and manic/hypomanic symptoms
There was a significant correlation between the depressive and the manic/hypomanic spectrum component scores in the overall sample (r = 0.57; p < 0.05), and in patients with AN-R (r = 0.67; p < 0.05), but not in BN patients (r = 0.21, p = ns).
Mood spectrum assessment and MOODS-SR Lifetime factors
The mean total score of MOODS-SR Lifetime in the overall sample was 79.0 ± 37.3 (range 5–146). The mean total score of MOODS-SR Lifetime was significantly higher in BN than in AN-R patients (97.5 ± 25.4 vs 61.1 ± 38.5, respectively; p = 0.0001). 63.6 % of the sample (n = 35) endorsed the proposed cutoff of 61 items, with a statistically significant difference between AN-R and BN (39.3 % vs 88.9 %; χ 2 = 14.6; df = 1; p = 0.0001).
Patients with BN had significantly higher scores than patients with AN-R on several MOODS-SR factors (Tables 2, 3), namely:
-
1.
MOODS-SR depressive component: ‘depressive mood’ (11.2 ± 7.4 vs 16.0 ± 5.8; p < 0.05), ‘psychomotor retardation’ (5.4 ± 5.6 vs 8.9 ± 3.8; p = 0.003), ‘psychotic features’ (2.0 ± 1.8 vs 4.1 ± 1.6; p = 0.001), ‘neurovegetative symptoms’ (5.0 ± 2.6 vs 7.7 ± 1.7; p = 0.001).
-
2.
MOODS-SR manic/hypomanic component: ‘psychomotor activation’ (4.3 ± 3.6 vs 7.4 ± 3.1; p = 0.002), ‘mixed instability’ (1.0 ± 1.5 vs 2.0 ± 1.6; p < 0.05), ‘mixed irritability’ (2.5 ± 1.8 vs 3.7 ± 1.6; p < 0.05), ‘inflated self-esteem’ (1.1 ± 1.4 vs 2.1 ± 1.6; p = 0.012), and ‘wastefulness/recklessness’ (1.0 ± 1.4 vs 2.0 ± 1.2; p = 0.009).
Discussion
Axis I comorbidity for mood disorders is the rule and not the exception in patients with EDs. Mood disorder comorbidity might contribute to ED complications, such as suicide, substance abuse or chronic course [1, 2, 19].
MOODS-SR was able to detect in a sample of patients with EDs a broader range of comorbid mood signs belonging to both subthreshold forms of mania and depression compared to the commonly used scales for mood disorders and temperaments. This result could be explained neither with the well-documented Axis I high rates of comorbidity between eating and mood disorders, nor with the occurrence of ‘hyperthymic/cyclothymic temperaments’. Thus, the Axis I comorbidity for mood disorders (unipolar and bipolar) was the main exclusion criterion of our study. At the same time, affective temperaments, with their limited number of features, did not cover the wide range of signs and symptoms detected by MOODS-SR.
More interestingly, we highlighted several differences in MOODS-SR factor scores between patients with BN and AN-R. We found that patients with BN scored higher than patients with AN-R on a number of factors belonging both to the depressive and to the manic/hypomanic component of MOODS-SR. Moreover, the higher scores on the manic factors of BN patients were not correlated with the higher scores of the depressive factors, thus excluding a potential relationship with a generic ‘severity effect.’ A significant correlation between depressive and manic/hypomanic spectrum scores was found in the overall sample and in patients with AN-R, not in BN patients. This result is similar to the correlations we previously observed in a study on mood disorder patients [20].
More in detail, patients with BN showed higher scores than patients with AN-R on the ‘psychomotor activation,’ ‘mixed instability,’ ‘mixed irritability,’ and ‘wastefulness/recklessness’ MOODS-SR factors of the manic component. Taken together, these factors might delineate a soft mixed state in patients with BN. Depression in patients with AN-R is usually characterized by depressed mood with a few mixed traits, excluding the need for ‘physical activity to burn fat and calories,’ a typical symptoms of AN-R that should be differentiated from psychomotor activation or recklessness. Mixed features in patients with BN could interfere with the course of the disorder and with treatment compliance. In the choice of treatment strategies, the presence of mixed feature specifiers should be considered as mixed traits could lead to a higher suicidal risk in BN patients [21, 22].
Surprisingly, patients with BN reported more subthreshold psychotic-like thoughts than patients with AN-R. This finding should be interpreted with caution, given that a number of studies have highlighted the role of the dopaminergic system in AN rather than in BN. This provided a rationale for the use of neuroleptics in severe AN, especially restricting subtype [23–25]. In the literature, patients with AN-R have been considered as more prone than patients with BN to delusional thoughts, at least with regard to body perception [23–25]. A number of studies reported that the overall group of EDs could span a spectrum from delusional to non-delusional thinking, with ‘unlimited shades of gray in between’ [26, 27]. Psychotic symptoms could be better explained within the inner psychopathology of the EDs rather than by assuming there is a link with psychotic disorders [28]. Moreover, in a previous study, we conducted on a sample of patients with bipolar disorders, psychotic spectrum symptoms positively correlated with the severity of mood dysregulations and the total number of mood spectrum signs and symptoms [29].
Taken as a whole, data emerging from our lifetime MOODS-SR evaluation in patients with AN-R and BN suggested the existence of a continuum from manic to depressive side, without a clear cutoff between the two dimensions. The experience with the MOODS-SR in such patients enforced past and recent claims toward the need for a dimensional approach to comorbidity between mood and eating disorders. Thus, our study confirmed previous reports that suggested patients with EDs might manifest a broad halo of psychopathologic features belonging both to the depressive and the manic/hypomanic components of the mood spectrum. The use of instruments such as the MOODS-SR could help clinicians to identify these aspects and to highlight their importance. However, subthreshold comorbidity for mood spectrum signs and symptoms assessed with MOODS-SR showed a main limitation: MOODS-SR did not allow us to clarify whether the scores reflected mood instability across time, or the presence of stable ‘cyclothymic/hyperthymic personality traits,’ especially in BN patients. In the same way, it was impossible to ascertain whether the maintenance of normal weight, typical in BN patients, played a role in the modulation of the mood spectrum phenomenology, or whether mood dysregulations interfered with the eating/feeding disorder presentation, diminishing the ability to reduce weight.
However, through the MOODS-SR lifetime and the systematic assessment of the mood spectrum dimensions, we could confirm that mood spectrum phenomenology is a relevant component in EDs, regardless of full-blown illness episodes (manic, depressive and mixed states). In the BN patients, such dimensions were much higher than in the AN-R patients, suggesting that in BN mood spectrum, comorbidity was an important psychopathological dimension that could underpin specific clinical characteristics and illness course, with specific neurobiological mechanisms. Soft, subthreshold mood features should be influenced by lifetime energy and mood fluctuations, especially by subthreshold manic phases, with a key role during depressive phases.
Nevertheless, these data have limited generalizability until they have been substantiated in larger studies conducted with DSM-5 criteria. As already specified, the choice of utilizing DSM-IV instead of DSM-5 criteria was due to the data collection of the original study that took place before DSM-5 publication. Moreover, the limited sample size was partially due to the choice not to recruit patients with EDNOS. EDNOS can be a more frequent diagnosis, but its clinical characteristics are too variable and non-homogeneous. Assessment with a new model of mood spectrum comorbidity could be more reliable in patients with a full-blown diagnosis of AN-R or BN, instead of a sample characterized by many of the symptoms of other EDs, but which do not meet the full-blown criteria for the ‘more classic’ diagnoses.
Despite these limitations, we believe that the proposed mood spectrum model could become relevant for a better comprehension of EDs, focusing on its importance in the identification of different phenotypes of patients who might present and respond differently to available treatments.
References
McElroy SL, Kotwal R, Keck PE Jr, Akiskal HS (2005) Comorbidity of bipolar and eating disorders: distinct or related disorders with shared dysregulations? J Affect Disord. 86(2–3):107–127. doi:10.1016/j.jad.2004.11.008 (Review. PubMed PMID: 15935230)
Godart NT, Perdereau F, Rein Z, Berthoz S, Wallier J, Jeammet P, Flament MF (2007) Comorbidity studies of eating disorders and mood disorders. Critical review of the literature. J Affect Disord 97(1–3):37–49. doi:10.1016/j.jad.2006.06.023 (Epub 2006 Aug 22. Review. PubMed PMID: 16926052)
Löwe B, Zipfel S, Buchholz C, Dupont Y, Reas DL, Herzog W (2001) Long-term out come of anorexia nervosa in a prospective 21-year follow-up study. Psychol Med 31(5):881–890. doi:10.1007/s00787-012-0328-z (PubMed PMID: 11459385)
Berkman ND, Lohr KN, Bulik CM (2007) Outcomes of eating disorders: a systematic review of the literature. Int J Eat Disord. 40(4):293–309. doi:10.1002/eat.20369 (Review. PubMed PMID: 17370291)
Franko DL, Keel PK, Dorer DJ, Blais MA, Delinsky SS, Eddy KT, Charat V, Renn R, Herzog DB (2004) What predicts suicide attempts in women with eating disorders? Psychol Med. 34(5):843–853. doi:10.1017/s0033291703001545 (PubMed PMID: 15500305)
Bulik CM, Thornton L, Pinheiro AP, Plotnicov K, Klump KL, Brandt H, Crawford S, Fichter MM, Halmi KA, Johnson C, Kaplan AS, Mitchell J, Nutzinger D, Strober M, Treasure J, Woodside DB, Berrettini WH, Kaye WH (2008) Suicide attempts in anorexia nervosa. Psychosom Med 70(3):378–383. doi:10.1097/PSY.0b013e3181646765 (Epub Feb 6 PubMed PMID: 18256339)
Forcano L, Fernández-Aranda F, Alvarez-Moya E, Bulik C, Granero R, Gratacòs M, Jiménez-Murcia S, Krug I, Mercader JM, Riesco N, Saus E, Santamaría JJ, Estivill X (2009) Suicide attempts in bulimia nervosa: personality and psychopathological correlates. Eur Psychiatry. 24(2):91–97. doi:10.1016/j.eurpsy.2008.10.002 (Epub 2008 Dec 19. PubMed PMID: 19101125)
Mischoulon D, Eddy KT, Keshaviah A, Dinescu D, Ross SL, Kass AE, Franko DL, Herzog DB (2011) Depression and eating disorders: treatment and course. J Affect Disord. 130(3):470–477. doi:10.1016/j.jad.2010.10.043 (Epub 2010 Nov 24. PubMed PMID: 21109307; PubMed Central PMCID: PMC3085695)
Cassano GB, Dell’Osso L, Frank E, Miniati M, Fagiolini A, Shear K, Pini S, Maser J (1999) The bipolar spectrum: a clinical reality in search of diagnostic criteria and an assessment methodology. J Affect Disord. 54(3):319–328. doi:10.1016/S0165-0327(98)00158-X (Review. PubMed PMID: 10467978)
Campos RN, Angst J, Cordas TA, Moreno RA (2011) ESPECTRA: searching the bipolar spectrum in eating disorder patients. BMC Psychiatry. 11:59. doi:10.1186/1471-244X-11-59 (PubMed PMID: 21489298; PubMed Central PMCID: PMC3094285)
Dell’Osso L, Armani A, Rucci P, Frank E, Fagiolini A, Corretti G, Shear MK, Grochocinski VJ, Maser JD, Endicott J, Cassano GB (2002) Measuring mood spectrum: comparison of interview (SCI-MOODS) and self-report (MOODS-SR) instruments. Compr Psychiatry. 43(1):69–73. doi:10.1053/comp.2002.29852 (PubMed PMID: 11788923)
Wildes JE, Marcus MD, Fagiolini A (2007) Eating disorders and illness burden in patients with bipolar spectrum disorders. Compr Psychiatry. 48(6):516–521. doi:10.1016/j.comppsych.2007.05.012 (Epub 2007 Aug 20. PubMed PMID: 17954136; PubMed Central PMCID: PMC2077842)
Wildes JE, Marcus MD, Gaskill JA, Ringham R (2007) Depressive and manic-hypomanic spectrum psychopathology in patients with anorexia nervosa. Compr Psychiatry. 48(5):413–418. doi:10.1016/j.comppsych.2007.05.009 (PubMed PMID: 17707248)
Mauri M, Borri C, Banti S, Baldassari S, Rucci P, Cassano GB (2002) The anorexic-bulimic spectrum in patients with eating disorders, mood disorders and controls. Ital J Psychopathol 8:2
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59(Suppl 20):22–33 (quiz 34–57. Review. PubMed PMID: 9881538)
Fagiolini A, Dell’Osso L, Pini S, Armani A, Bouanani S, Rucci P, Cassano GB, Endicott J, Maser J, Shear MK, Grochocinski VJ, Frank E (1999) Validity and reliability of a new instrument for assessing mood symptomatology: the structured clinical interview for mood spectrum (SCI-MOODS). Int J Methods Psychiatr Res 8:71–81
Cassano GB, Benvenuti A, Miniati M, Calugi S, Mula M, Maggi L, Rucci P, Fagiolini A, Perris F, Frank E (2009) The factor structure of lifetime depressive spectrum in patients with unipolar depression. J Affect Disord 115(1–2):87–99
Cassano GB, Mula M, Rucci P, Miniati M, Frank E, Kupfer DJ, Oppo A, Calugi S, Maggi L, Gibbons R, Fagiolini A (2009) The structure of lifetime manic-hypomanic spectrum. J Affect Disord. 112(1–3):59–70
Miettunen J, Raevuori A (2011) A meta-analysis of temperament in axis I psychiatric disorders. Compr Psychiatry 53:152–166
Cassano GB, Rucci P, Frank E, Fagiolini A, Dell’Osso L, Shear MK, Kupfer DJ (2004) The mood spectrum in unipolar and bipolar disorder: arguments for a unitary approach. Am J Psychiatry. 161(7):1264–1269 (PMID 15229060)
Halfon N, Labelle R, Cohen D, Guilé JM, Breton JJ (2013) Juvenile bipolar disorder and suicidality: a review of the last 10 years of literature. Eur Child Adolesc Psychiatry 22(3):139–151. doi:10.1007/s00787-012-0328-z (Epub 2012 Oct 7)
Saunders KE, Hawton K (2013) Clinical assessment and crisis intervention for the suicidal bipolar disorder patient. Bipolar Disord 15(5):575–583. doi:10.1111/bdi.12065 (Epub 2013 Apr 9)
Cassano GB, Miniati M, Pini S, Rotondo A, Banti S, Borri C, Camilleri V, Mauri M (2003) Six-month open trial of haloperidol as an adjunctive treatment for anorexia nervosa: a preliminary report. Int J Eat Disord. 33(2):172–177. doi:10.1002/eat.10130 (PubMed PMID: 12616583)
Mauri M, Miniati M, Mariani MG, Ciberti A, Dell’Osso L (2013) Haloperidol for severe anorexia nervosa restricting type with delusional body image disturbance: a nine-case chart review. Eat Weight Disord. 18(3):329–332. doi:10.1007/s40519-013-0052-9 (Epub 2013 Aug 3. PubMed PMID: 23907761)
Miniati M, Mauri M, Ciberti A, Mariani MG, Marazziti D, Dell’Osso L (2015) Psychopharmacological options for adult patients with anorexia nervosa. CNS Spectr. 6:1–9. doi:10.10171/s1092852914000790 (PubMed PMID: 26145463)
Phillips KA, Kim JM, Hudson JI (1995) Body image disturbance in body dysmorphic disorder and eating disorders. Obsessions or delusions? Psychiatr Clin North Am. 18(2):317–334. doi:10.1080/714111355 (Review. PubMed PMID: 7659601)
Rojo-Moreno L, Plumed JJ, Fons MB, Gonzalez-Piqueras JC, Rojo-Bofill L, Livianos L (2011) Auditory hallucinations in anorexia nervosa. Eur Eat Disord Rev. 19(6):494–500. doi:10.1002/erv.1084 (Epub 2011 Mar 10. Review. PubMed PMID: 21394834)
Miotto P, Pollini B, Restaneo A, Favaretto G, Sisti D, Rocchi MB, Preti A (2010) Symptoms of psychosis in anorexia and bulimia nervosa. Psychiatry Res. 175(3):237–243. doi:10.1016/j.psychres.2009.03.011 (Epub 2009 Dec 21. PubMed PMID: 20022383)
Benvenuti A, Rucci P, Ravani L, Gonnelli C, Frank E, Balestrieri M, Sbrana A, Dell’Osso L, Cassano GB (2005) Psychotic features in borderline patients: is there a connection to mood dysregulation? Bipolar Disord. 7(4):338–343. doi:10.1111/j.1399-5618.2005.00217 (PubMed PMID: 16026486)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
The Ethics Committee of the University of Azienda Ospedaliero-Universitaria of Pisa approved all study procedures.
Informed consent
All patients signed a written informed consent after receiving a complete description of the study and having the opportunity to ask questions.
Conflict of interest
The authors declare that they have no conflict of interest.
Data sharing statement
No basic research and clinical research studies that require a data-sharing statement were performed for this paper.
Rights and permissions
About this article
Cite this article
Miniati, M., Benvenuti, A., Bologna, E. et al. Mood spectrum comorbidity in patients with anorexia and bulimia nervosa. Eat Weight Disord 23, 305–311 (2018). https://doi.org/10.1007/s40519-016-0333-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-016-0333-1