Abstract
Purpose
To estimate the treated prevalence of eating disorders (ED) in Emilia-Romagna, Italy, and to compare health services utilization among age groups and geographical areas.
Methods
The study cohort consists of patients aged 12–64 years with a primary or secondary ED diagnosis, treated in regional healthcare facilities in 2012. Patients were followed up for 1 year from the first contact. Data were extracted from regional administrative databases.
Results
The study cohort included 1550 cases, 36.8 % with anorexia nervosa, 21.9 % with bulimia nervosa and 41.3 % with ED not otherwise specified. Adolescents (12–17 years) were 18.6 %, young adults (18–30) 32.7 % and older adults (31–64) 48.7 %. The annual treated prevalence rate was 5.2/10,000 (13.3 for adolescents, 9.3 for young adults and 3.4 for older adults) and was highest among adolescent (24.6/10,000) and young adult females (17.1/10,000). Cases without a record for ED in the previous year were 46.8 %. Older adults displayed higher comorbidity and used more services including hospital-based care. Outpatient care greatly exceeded inpatient care across age groups. Variations in care patterns across regional areas were found.
Conclusions
Our results indicate that the care pathway for ED varies among age groups and geographical areas, but is consistent with the regional care model that favors the use of outpatient services. Future perspectives include evaluating the integration among mental health services, specialty outpatient units and primary care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eating disorders (ED) tend to have early onset and long-term development, often with serious health consequences, psychosocial impairment and high costs for patients, families and society. Care of these complex, multi-faceted and high-comorbidity disorders usually involves multiple services. Clinical guidelines and recommendations are available [1–3], but various approaches and models are still competing without conclusive evidence [4–6]. Therefore, it is of public health concern to collect epidemiological data on prevalence and incidence, as well as to trace different care pathways and evaluate their impact on outcomes.
In Italy, studies reporting prevalence and incidence rates are sparse, and only occasional and short-term research on treatment outcomes is available [3, 4, 7–10].
Since 2004, Emilia-Romagna Region has implemented a health care programme for patients with ED [11], mainly addressed to young people aged 12–30. This programme adopts a multidisciplinary and multiprofessional treatment model, based on an integrated network of services. Training initiatives as well as careful annual monitoring of resources and activities have been implemented to promote health in childhood and continuity of care across services for different age groups. Five levels of care were identified, beyond primary care access and referral: (I) outpatient assessment and treatment in mental health services for adults and adolescents; (II) specialist outpatient assessment and treatment by expert multidisciplinary teams; (III) specialist day-hospital; (IV) residential treatment for psycho-nutritional rehabilitation; (V) medical or psychiatric inpatient treatment. Within the regional programme, outpatient treatment is delivered by the public sector, while residential and inpatient care can also involve private-licensed facilities, under the supervision of Local Health Authorities (LHA).
Given this framework, information on treatment provision across the full range of services is needed to evaluate the programme outputs and the ongoing regional planning.
The aims of this study are to estimate the treated prevalence of ED and to describe health services utilization over 1 year in a regional cohort of patients, subdivided into the age groups 12–17 and 18–30 (targeted by the ED programme) and 31–64 years. Comparisons between three major regional areas are also presented to identify possible heterogeneities in ED care provision.
Materials and methods
Setting, health services and treatments
Emilia-Romagna is a Northern Italy region with 4.4 million inhabitants residing in eleven LHA catchment areas. Within each LHA, a Mental Health Department (MHD) is responsible for community and residential mental health care for adults (Community Mental Health Centers CMHC) and children and adolescents (Childhood–Adolescence Mental Health Services CAMHS), as well as for inpatient care provided by general hospital psychiatric wards and drug addiction services. MHD services are connected with general practitioners, pediatricians and specialist services for outpatient care [12, 13]. The Regional Health Service also includes six large Hospital Trusts (HT), four of which are University-led. LHAs and HTs offer universal coverage for prevention and care. For planning, organizational and allocation reasons, health care services are grouped together into three major areas: Emilia Nord-AVEN (1,975,763 pop.), Emilia Centro-AVEC (1,358,617 pop.) and Romagna-AVR (1,124,866 pop.).
Guidelines about ED care pathways have been delivered and published by the regional programme taskforce since 2004 [11]. Each LHA catchment area has created outpatient expert multidisciplinary teams (psychologists, psychiatrists, clinical nutritionists, dieticians, internists) working either in MHD or in medical departments. Expert teams are entrusted with supervising integrated care through the network of local services and supporting other colleagues in MHD or hospital units for the appropriate treatment of ED. Each catchment area usually provides day-hospital (DH) treatments in public hospitals. In addition, DH treatment is delivered in a specialist private hospital in AVEN. This private facility is the main provider of residential care for ED in the region. Residential admissions in 2012 were focused on intensive treatment, often following hospitalization for medical or psychiatric emergencies, rather than on psycho-nutritional rehabilitation. Inpatient care is carried out by psychiatric as well as medical wards, with different organization across the various areas. Even if some large hospitals have considerable expertise, none of the three major geographical areas has attained a well-defined inpatient care pathway or has definitively implemented a “hub and spoke” model (except for AVEC, where the hub for adolescents is the Child Neuropsychiatric Unit in the University-led HT in Bologna).
Study population and data source
The study cohort consists of patients with a primary or secondary diagnosis of ED being treated in regional health care facilities in 2012.
Data were extracted from the regional administrative databases: hospital discharge records, residential discharge records, community mental health information system and child–adolescent mental health information system.
Inclusion criteria were: age 12–64 years, both genders, being resident in Emilia-Romagna, being admitted to a hospital or a residential facility or receiving at least one intervention in CMHCs or in CAMHSs in 2012, being diagnosed with anorexia nervosa (AN), bulimia nervosa (BN), or other eating disorders, identified by ICD-9-CM codes 3071, 30751, 30750, 30754, 30759, 3075, or ICD-10 codes F500, F501, F502, F503, F508, F509 that are used in the childhood and adolescence services’ databases. In the present study, we used the label eating disorders not otherwise specified (EDNOS) to denote eating disorders other than AN and BN.
Physical comorbidity was determined using information from hospital discharge records and coded as present if any of the 19 diagnoses comprising the Charlson index [14] was found among primary or secondary ICD-9-CM diagnoses. Psychiatric comorbidity was searched in hospital discharge records and in the CMHCs and CAMHSs databases.
Patients were followed up for 1 year starting from the day of their first clinical visit/admission in 2012 (or from January 1st, if at least one contact with inpatient or outpatient services was found in the previous year). Admissions and treatments during follow-up were retrieved from the aforementioned databases, and also from specialist outpatient clinic records and emergency room records. Mortality was retrieved from the regional mortality registry.
Population data used for prevalence calculation refer to 1st January 2012 (http://dati.istat.it/).
Statistical analyses
χ 2 and Kruskal–Wallis tests as appropriate were used to compare percentages and count variables among age groups. Care provision was compared among geographical areas using multiple regression analyses. Logistic, linear or Poisson regression models were used according to the type of intervention examined as dependent variable. To take into account differences in case mix among geographical areas, all models were adjusted for age, gender, ED diagnosis, physical comorbidity, psychiatric comorbidity and new cases (those without records for an eating disorder in the previous year), coded as yes/no. The significance level was set to p < 0.05. Analyses were carried out using SPSS 20.0 and Stata v13.1.
Results
Characteristics of the study cohort and prevalence
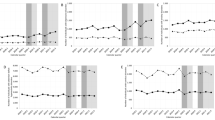
Of the 1550 patients identified, 570 (36.8 %) had a diagnosis of AN, 340 (21.9 %) of BN, and 640 (41.3 %) of EDNOS. Females were the large majority, adolescents 12–17 years old were 18.6 %, and young adults aged 18–30 were 32.7 %; Italians were 96.7 % (Table 1). Twenty-three percent had psychiatric comorbidity and 14 % had physical comorbidity. The percentage of patients with psychiatric and physical comorbidity increased significantly with age. Overall, the treated prevalence per 10,000 inhabitants in 2012 was 5.2 (13.3 for adolescents, 9.3 for young adults and 3.4 for the 31–64 years patients). Figure 1 shows the treated prevalence by age groups and gender. It was highest among females aged <18 years (24.59) and 18–30 (17.06) and declined to 6.07 in older adult females. In males, the prevalence in the corresponding age groups was 2.76, 1.81 and 0.75. The treated prevalence was 1.92/10,000 for AN, 1.15/10,000 for BN and 2.16/10,000 for EDNOS.
New cases were 46.8 %, without significant differences among age groups. AN was significantly more common in adolescents, while EDNOS was more common among older adults. Notably, the AVEC area was the one with the highest proportion of patients aged 12–17 (24.8 %), and AVR area was the one with the highest proportion of patients aged 31–64 (58.4 %). Mortality was uncommon: only two women, both aged 58 years, died during the follow-up, for cerebrovascular disease and polytraumatism.
Treatments and health services use
Table 2 summarizes the interventions provided over the follow-up year, sorted by increasing levels of care.
Overall, more than two-thirds of patients were seen in the CMHC (69.3 %). The majority of cases (86.8 %) received at least one specialist outpatient visit, but only in about one-fifth the visit was consultation in endocrinology, dietology or nutrition units. About one-third of patients were hospitalized at least once and 3.7 % were admitted to intensive psychiatric residential facilities. This small subgroup of severe patients received other treatments in the follow-up year: the large majority (86.2 %) had at least one CMHC intervention, 75.9 % were hospitalized and the same percentage had at least one specialist visit. Twelve patients (20.7 %) had at least one day-hospital admission, and 32 (55.2 %) had at least one emergency room visit.
Treatments and health services use by age groups
CAMHS interventions included diagnostic assessment in 21.8 % of adolescents and clinical treatment (including psychological, psychoterapeutic or rehabilitation treatments after the evaluation phase) in 46 % of adolescents and 2.8 % of young adults.
The percentage of patients treated in CMHC increased significantly with age. The most common type of care was clinical-psychiatric treatment (i.e., clinical interviews aimed at monitoring drug treatment and/or unstructured psychological interventions), while psychotherapy (i.e., a psychological treatment meeting the requirements for a structured psychotherapy model in terms of setting and technique) was provided to 22.1 % of adolescents, 32.2 % of young adults and 28.3 % of older adults. Only a limited percentage of patients (5.7 %, mainly adults) received socio-rehabilitative care, i.e., skills training in daily living activities or in social relationships or vocational rehabilitation.
While treatment in hospital or residential facilities increased with age, day-hospital treatment was more frequent among patients aged <31 years. However, adolescents had a longer stay in the psychiatric/neuropsychiatric units and general medical units compared with adults.
Lastly, more than one-third of patients in each age group had at least one emergency room visit. The median number of ER visits was 1 in the age groups <31 years and 2 in those aged 31–64, respectively. Only 0.5 % of patients had more than 10 ER visits, denoting the presence of few high emergency room users.
Overall, 83.7 % of patients were treated in more than one health care setting. The youngest age group was less likely to be treated in diverse care settings. In particular, compared with adults (21.1 and 31.8 %), a lower percentage of adolescents (9 %) had a pattern of care including hospital or day-hospital, outpatients specialized visits and community mental health care.
Comparisons among geographical areas
Crude and adjusted percentages of interventions provided over 1 year were compared among geographical areas (Table 3). The intensity and the profile of care provided exhibited several differences, after adjusting for the case mix. Adjusted percentages of CAMHS treatment were highest in AVEC, while CMHC treatment was significantly more frequent in AVEN and AVR. AVEN showed the highest referral to day-hospital for clinical treatment but a lower delivery of endocrinology/nutritionist outpatient visits. In addition, AVEC showed significantly higher percentages of hospitalization, compared with the other areas. Although the number of health services used was the same in each area, the pattern of care differed. In particular, considering only the most frequent patterns of care, the joint hospital-specialist outpatient clinics pathway was significantly more frequent in AVEC and a predominance of MHD with specialist outpatient treatment was observed in AVR.
Discussion
The present study describes outpatient and inpatient care provided by the network of Emilia-Romagna health services to patients with eating disorders over 12 months.
The first findings concern the treated prevalence. In line with other research [15–18], the prevalence of EDNOS was higher than that of AN and BN. Our data show that AN typically affects the younger, while EDNOS is common in older patients. The high frequency of EDNOS is likely to depend on the stringent diagnostic criteria for AN and BN. Furthermore, our results might support the “transdiagnostic” hypothesis, according to which eating disorders are partially interchangeable over time [15, 16] and evolve with age and chronicity towards “not otherwise specified” clinical entities, not less serious or challenging than the other two. The female-to-male ratio of 10:1 confirms the well-known gender distribution in ED. Non-Italian citizens represent only 3.3 % of ED cases, a figure well below the proportion resident Emilia-Romagna in 2012 (12.1 %). Therefore, ED seem to be less frequent or undertreated among non-Italians, probably reflecting the inequality in access to health services by migrants in Italy [19]. Prevalence is lower than generally reported [3, 20, 21], though direct comparisons with other studies are hindered by methodological differences. Since we investigated only patients recruited in health services, a possible reason of this gap is the absence of patients treated by private specialists or untreated. Another reason is that cases only treated at the two outpatient specialist University centers in Bologna, around 300 patients according to previous estimates [22], could not be identified, due to the lack of diagnoses in the specialist outpatient clinics database. Nonetheless, as expected, the annual prevalence peaks in women aged 12–17. Besides, the adolescent and younger-adult groups, to which the regional ED programme is mainly addressed, display prevalence rates three times higher than the older age class. Consistent with another investigation in Bologna [23], new cases are about 50 %. A possible interpretation of this finding is the increased sensitization to ED among primary care physicians and pediatricians that may lead to early diagnosis and timely referrals. In addition, the implementation of a regional pathway to care may facilitate a better access to services. On the other hand, especially for young adults, episodes of care within the health services network appear to be shorter than expected, given the long-term course of these disorders. This suggests that many patients discontinue treatment or are treated in the private healthcare setting, as reported elsewhere [24–26].
The second relevant findings deal with chronicity. Older patients showed higher physical and psychiatric morbidity and used more services including hospital-based care. In CMHC, almost 30 % of cases received psychotherapy, regardless of age, while socio-rehabilitative and residential treatments were more often delivered to the older patients.
Inpatient care was more frequent among older patients; on the contrary, DH treatments often involved younger patients. Notably, this seems to be an appropriate pattern of care, since it entails providing the younger cases with intensive care and sparing them the experience of hospitalization and its possible negative impact in terms of chronicity and morbidity [27, 28]. On the other hand, a consistent body of research underscores that therapy outcomes seem more favorable in youths [29]. The large proportion of older and burdensome cases reported in our study highlights even more the importance of optimizing care for adolescents and young adults and upholds the implementation and reinforcement of the regional ED programme to prevent future chronicization.
The relatively low percentage of cases treated with psychotherapy in CMHC deserves an explanation. Although psychotherapy is recommended by treatment guidelines [1–3], to implement rigorous psychotherapeutic approaches targeted to eating disorders, highly trained personnel would be required for considerable amounts of time. Unfortunately, the current cuts to healthcare expenditure and the subsequent increased workload of therapists make more feasible less structured forms of psychological interventions, or referral to private psychotherapists.
The third finding is that outpatient care greatly exceeds inpatient care in all age groups. This is consistent with evidence from national and international research [3, 4, 8, 24, 25, 30]. During the 12-month observation, the majority of patients attended MHD community services and almost all had at least an outpatient specialist visit. Furthermore, the most frequent patterns of care consisted in the association of at least two services throughout the follow-up year. Highly integrated and multidisciplinary outpatient care is strongly recommended by current guidelines on ED [1–3] and represents the second level of care of Emilia-Romagna regional programme. Our data are not detailed enough to outline a well-defined care pathway, being limited to describing the use of various services. Nevertheless, integrated care across the services network is meant to be practiced, since patients usually refer to diverse settings and specialists. Besides, the relatively low rate of emergency rooms visits is encouraging and suggests that ED patients’ healthcare needs are at least partially met. It is worth mentioning that MHD services appear to be flexible with regard to adolescents care, since 25.6 % of adolescents were first recruited in CMHC rather than in CAMHS (see Table 1). This does not exclude treatment provision by CAMHS over the observation year, but hints at the capacity of the MHD services to cooperate in a highly integrated way, tailoring the transition from childhood/adolescence to adult services on adolescents’ needs and clinical symptoms. Notably, residential care involved a minority of cases, mostly aged >30. In 2012, this level of care was based on intensive care rather than long-term psycho-nutritional rehabilitation.
The last finding concerns the level of implementation of the ED programme. Our results indicate some relevant variations in patterns of care provided. The main reason is a persisting heterogeneous organization across the regional areas, and even among LHAs and HTs, depending on local resources, managerial decisions and professional approaches.
Our study has several limitations. First, coding problems in the outpatient specialist database did not allow to trace the whole care delivered to ED. As a consequence, treated prevalence and service use in the follow-up period are likely to be underestimated, since ambulatory visits either at two University centres or at medical units treating ED could not be retrieved. Second, information on clinical severity and weight/BMI is not available from administrative databases. Third, the short follow-up carries limited information on health care process, appropriateness of treatment and outcome.
The main strength of the study is the large population investigated through the linkage of health services databases. This is an important achievement, since it is claimed that most studies fail to provide a full picture of the system of care for ED [23].
Conclusions
In summary, the results of this population-based study indicate that the care pathway for ED varies among age groups and geographical areas, but is consistent with the regional care model that favors the use of outpatient services. Some future perspectives can be envisaged. Outcome studies on a longer period, mainly on incident cases, should be carried out. With regard to the programme evolution, the priorities consist of strengthening expert teams at the specialist level of outpatient care, improving integration between MHD and nutritionist units, as well as favouring multiprofessional work through resource allocation. It is also important to reinforce training of GPs and pediatricians and the collaboration of MHD services with primary care [30–32] to enable early detection of ED. In addition, given the increasing migratory flows and the lack of epidemiological studies on ED in immigrants in Italy, a possible inequality in access to health services among migrants needs to be further ascertained and monitored over time. These steps can lead to define a clear organizational model and to increase homogeneity and continuity of care, in order to avoid chronic and comorbid consequences, and reduce individual, family and health care burden.
References
American Psychiatric Association (2006) Treatment of patients with eating disorders, third edition. Am J Psychiatry 163((7 Suppl)):4–54
Wilson GT, Shafran R (2005) Eating disorders guidelines from NICE. Lancet 365:79–81. doi:10.1016/S0140-6736(04)17669-1
Ministero della Salute (2013) Appropriatezza clinica, strutturale e operativa nella prevenzione, diagnosi e terapia dei disturbi dell’alimentazione. Quaderni del Ministero della Salute 17/22 Roma, p 1–89
De Virgilio G, Coclite D, Napoletano A, Barbina D, Dalla Ragione L, Spera, Di Fiandra T (2013) Conferenza di consenso sui disturbi del comportamento alimentare (DCA) negli adolescenti e nei giovani adulti. Roma (Rapporti ISTISAN 13/6), p 1–109
Treasure J, Claudino AM, Zucker N (2010) Eating disorders. Lancet 375:583–593. doi:10.1016/S0140-6736(09)61748-7
Zipfel S, Wild B, Groβ G, Friederich HC, Teufel M, Schellberg D, Giel KE, de Zwaan M, Dinkel A, Herpertz S, Burgmer M, Löwe B, Tagay S, von Wietersheim J, Zeeck A, Schade-Brittinger C, Schauenburg H, Herzog W, on behalf of the ANTOP study group (2014) Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatient with anorexia nervosa (ANTOP study): randomised controlled trial. Lancet 383:127–137. doi:10.1016/S0140-6736(13)61746-8
Gigantesco A, Masocco M, Picardi A, Lega I, Conti S, Vichi M (2010) Hospitalization for anorexia nervosa in Italy. Riv Psichiatria 45:154–162. doi:10.1708/497.5895
Sukkar SG, Foppiani L, Campostano A (2005) Management and treatment of eating disorders in an Italian Region. Eat Weight Disord 10(3):204–209. doi:10.1007/BF03327548
Dalle Grave R, Calugi S, El Ghoch M, Conti M, Fairburn CG (2014) Inpatient cognitive behavior therapy for adolescent with anorexia nervosa: immediate and longer-term effects. Front Psychiatry 5:14. doi:10.3389/fpsyt.2014.00014
De Virgilio G, Coclite D, Napoletano A, Barbina D, Di Fiandra T (2013) Convegno. Lo stato dell’arte e le prospettive nella gestione dei DCA a un anno dalla Conferenza nazionale di consenso. Istituto Superiore di Sanità. Roma, 30 Ottobre 2013. Atti. Roma (Rapporti ISTISAN 13/49)
Regione Emilia-Romagna (2004) DGR n 1016/2004. Linee guida per il potenziamento dell’assistenza ai disturbi del comportamento alimentare. Bologna
Lora A, Starace F, Di Munzio W, Fioritti A (2014) Italian Community Psychiatry in practice. Description and comparison of three regional systems. J Nerv Ment Dis 202:446–450. doi:10.1097/NMD.0000000000000143
Pedrini L, Colasurdo G, Costa S, Fabiani M, Ferraresi L, Franzoni E, Rocchi MBL, Sisti D, Squarcia A, Trebbi S, Turchetti D, Visconti P, Tullini A, de Girolamo G, The PREMIA Group (2012) The characteristics and activities of child and adolescent mental health services in Italy: a regional survey. BMC Psychiatry 30(12):7. doi:10.1186/1471-244X-12-7
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383. doi:10.1016/0021-9681/87
Fairburn CG, Bohn K (2005) Eating disorder NOS (EDNOS): an example of the troublesome “not otherwise specified” (NOS) category in DSM IV. Behav Res Ther 43(6):691–701. doi:10.1016/j.brat.2004.06.011
Fairburn CG, Harrison PJ (2003) Eating disorders. Lancet 361:407–416. doi:10.1016/S0140-6736(03)12378-1
Micali N, Hagberg KW, Petersen I, Treasure JL (2013) The incidence of eating disorders in the UK in 20002009: findings from the General Practice Research Database. BMJ Open. doi:10.1136/bmjopen-2013-002646
Ricca V, Mannucci E, Mezzani B, Di Bernardo M, Zucchi T, Paionni A, Placidi GPA, Rotella CM, Faravelli C (2001) Psychopathological and clinical features of outpatients with an eating disorder not otherwise specified. Eat Weight Disord 6(3):157–165. doi:10.1007/BF03339765
Tognetti M (2015) Health inequalities: access to services by immigrants in Italy. Open J Soc Sci. doi:10.4236/jss.2015.34002
Preti A, De Girolamo G, Vilagut G, Alonso J, Graaf RD, Bruffaerts R, Demyttenaere K, Pinto-Meza A, Haro JM, Morosini P, ESEMeD-WMH Investigators (2009) The epidemiology of eating disorders in six European countries: results of the ESEMeD Project. J Psychiatr Res 43:1125–1132. doi:10.1016/j.jpsychires.2009.04.003
Hoek HW, van Hoeken D (2003) Review of the prevalence and incidence of eating disorders. Int J Eat Disord 34(4):383–396. doi:10.1002/eat.10222
AVEC. Programma Disturbi del Comportamento Alimentare Area Vasta Emilia Centro (2013). http://salute.regione.emilia-romagna.it/salute-mentale-e-dipendenze/dca. Accessed 19 Sept 2016 (in Italian)
Calugi S, Avaldi VM, Dalle Grave R, Rucci P, Fantini MP (2014) Mental health services use and management of eating disorders in an Italian Department of Mental Health. Eat Weight Disord 19(2):191–197. doi:10.1007/s40519-014-0103-x
Striegel-Moore RH, DeBar L, Wilson GT, Dickerson J, Rosselli F, Perrin N, Lynch F, Kraemer HC (2008) Health service use in eating disorders. Psychol Med 38:1465–1474. doi:10.1017/S0033291707001833
Wonderlich S, Mirchel JE, Crosby RD, Myers TC, Kadlec K, Lahaise K, Swan-Kremeier L, Dokken J, Lange M, Dinkel J, Jorgensen M, Schander L (2012) Minimizing and treating chronicity in the eating disorders: a clinical overview. Int J Eat Disord 45(4):467–475. doi:10.1002/eat.20978
Fassino S, Pierò A, Tomba E, Abbate-Daga G (2009) Factors associated with dropouts from treatment for eating disorders: a comprehensive literature review. BMC Psychiatry 9:67. doi:10.1186/1471-244X-9-67
Gowers SG, Weetman J, Shore A, Hossain F, Elvins R (2000) Impact of hospitalisation on the outcome of adolescent anorexia nervosa. Br J Psychiatry 176:138–141. doi:10.1192/bjp.176.2.138
Herpetz-Dahlmann B, Schwarte R, Krei M, Egberts K, Warnke A, Wewetzer C, Pfeiffer E, Fleischhaker C, Scherag A, Holtkamp K, Hagenah U, Bühren K, Konrad K, Schmidt U, Schade-Brittinger C, Timmesfeld N, Dempfle A (2014) Day-patient treatment after short inpatient care versus continued inpatient treatment in adolescents with anorexia nervosa (ANDI): a multicentre, randomised, open-label, non-inferiority trial. Lancet 383:1222–1229. doi:10.1016/S0140-6736(13)62411-3
Legenbauer TM, Meule A (2015) Challenges in the treatment of adolescent anorexia nervosa—is enhanced cognitive behavior therapy the answer? Front Psychiatry 6:148. doi:10.3389/fpsyt.2015.00148
Simon J, Schmidt U, Pilling S (2005) The health service use and cost of eating disorders. Psychol Med 35(11):1543–1551. doi:10.1017/S003329170500470
Fursland A, Watson HJ (2014) Eating disorders: a hidden phenomenon in outpatient mental health? Int J Eat Disord 47:422–425. doi:10.1002/eat.22205
Johnston O, Fornai G, Cabrini S, Kendrik T (2007) Feasibility and acceptability of screening for eating disorders in primary care. Fam Pract 24:511–517. doi:10.1093/fampra/cmm029
Acknowledgments
The authors thank Drs. Eleonora Verdini and Giuseppina Lanciotti (Information System Unit, Health Care and Social Authority, Emilia-Romagna Region) for providing data and precious advice on regional administrative databases.
The members of Regional Group on Eating Disorders are Giuliano Limonta, Massimo Rossetti (Department of Mental Health and Pathological Addictions, Piacenza Local Health Authority), Anna Maria Gibin (Department of Mental Health and Pathological Addictions, Parma Local Health Authority), Enrica Manicardi (Reggio Emilia Hospital Trust), Claudio Annovi (Department of Mental Health and Pathological Addictions, Modena Local Health Authority), Carlotta Gentili (Department of Mental Health and Pathological Addictions, Bologna Local Health Authority), Emilio Franzoni (Bologna Hospital-University Trust), Carlo Della Gala (Department of Mental Health and Pathological Addictions, Imola Local Health Authority), Stefano Caracciolo (Ferrara Hospital-University Trust), Ester Giaquinto (Department of Primary Care, Romagna Local Health Authority), Daniela Ghigi (Department of Mental Health and Pathological Addictions, Romagna Local Health Authority).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical and informed consent
Regional databases were linked using a unique patient identifier and data were analyzed in anonymous form. Therefore, approval from the Local Ethics Committee and patients’ informed consent was not sought, in line with Italian privacy regulations.
Additional information
The members of Regional Group on Eating Disorders are listed in Acknowledgments.
Rights and permissions
About this article
Cite this article
Piazza, A., Rucci, P., Clo, M. et al. Health services utilization in patients with eating disorders: evidence from a cohort study in Emilia-Romagna. Eat Weight Disord 21, 625–633 (2016). https://doi.org/10.1007/s40519-016-0323-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-016-0323-3