Abstract
Purpose
The aim of this study was to investigate the possible correlation between epicardial adipose tissue (EAT) thickness and predictive parameters for metabolic syndrome (MS) in overweight/obese prepubertal children.
Methods
73 prepubertal children, average age of 8.22 years, with no endocrine or syndromic causes of obesity or under drug therapy for chronic disease were enrolled. Weight, height, body circumferences and skinfolds’ thickness were measured. BMI, BMI z score (z-BMI) and waist-to-height ratio (WtHR) were calculated. Standard MS-related laboratory parameters were assessed. Finally, all children underwent echocardiographic measurement of EAT.
Results
A positive correlation between EAT and z-BMI was found only among overweight/obese children (r = 0.43, p = 0.001). In particular, data showed that 89 % of our sample had a waist (W) >90th percentile. Statistical differences in diastolic blood pressure (DBP; p < 0.01) and EAT (p = 0.02) were observed on comparing W <90th percentile vs W >90th percentile patients. Besides, in patients with W >90th percentile and family history of risk factors for MS, the value of EAT correlated positively with z-BMI, W, WtHR, triglycerides (Tg), insulin and homeostatic model assessment of insulin resistance and negatively with HDL.
Conclusions
The EAT and the markers of MS probably share the same pathogenetic factors. Further studies might elucidate whether EAT deserves to be included among the diagnostic factors of MS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Being overweight since childhood is considered a risk factor for the persistence of obesity in adulthood. Moreover, pediatric obesity results in a number of complications such as psychosocial disorders (low self-esteem, depression), lung diseases (obstructive sleep apnea and exercise intolerance), musculoskeletal disorders (scoliosis, valgus knee, flat foot), endocrine disorders (precocious puberty, insulin resistance, polycystic ovary syndrome), liver disease [non-alcoholic fatty liver disease (NAFLD), non-alcoholic steato-hepatitis (NASH), cirrhosis], metabolic problems [non-insulin-dependent diabetes mellitus (NIDDM), dyslipidemia], and cardiovascular diseases (hypertension, dyslipidemia, ventricular hypertrophy). Metabolic syndrome (MS) is more and more frequently diagnosed in obese adolescents.
While in adult patients the MS diagnosis is based on standard criteria (for shared definition, see [1, 2]), there are still major differences regarding its definition in children. These differences reflect the uncertainty about the primary cause of the syndrome, as well as the diagnostic criteria. It is difficult to make the classification of MS in children, because of the complexity of the evolving characteristics specific to this age group. The lack of agreement on a shared definition of MS in childhood causes confusion, discrepancies, and difficulties in comparing the results of different studies.
The assorted classifications of MS in childhood [3, 4], which are applicable only for children over 10 years of age, are mainly based on the modification of diagnostic criteria used for adulthood [2]. In an attempt to make the diagnostic criteria more congruent with the unique characteristics of childhood, many scientific societies have developed modifications of the International Diabetes Federation (IDF) proposal. For example, the consensus of the Italian Paediatric Society (Società Italiana di Pediatria—SIP) in 2006 (“Obesità nel bambino e nell’adolescente: Consensus su Prevenzione, Diagnosi e Terapia”) indicates the possibility of a diagnosis of MS in children based on the presence of three or more abnormalities [5]. According to the most recent advances in infant anthropometry [6], these abnormalities can be identified with:
-
waist circumferences (W) >90th percentile for age and sex, or the waist/height ratio (WtHR) >0.5;
-
triglycerides (Tg) >95th percentile for age and sex;
-
HDL cholesterol <5th percentile for age and sex;
-
systolic (SBP) and diastolic blood pressure (DBP) >95th percentile for age and sex;
-
fasting glucose >100 mg/dl.
With regard to the cardiac function, the epicardial adipose tissue (EAT) is part of the adipose organ. EAT is metabolically active and is a source of a number of bioactive molecules. In addition to an endocrine and paracrine activity, EAT also has a biomechanical interaction with the myocardium and is, therefore, able to impact the morphology and the dynamics of the heart muscle [7–14].
The echocardiographic measurement of EAT that corresponds to the echo-free space between the outer wall of the myocardium and the layer of visceral pericardium has been proposed as an easy and reliable index of visceral adiposity. EAT can be seen as a potential diagnostic tool and biomarker of both prediction of coronary artery disease [15] and therapy efficacy in subjects with MS and high cardiometabolic risk, as exhaustively explained by Iacobellis and co. [16–20].
At present, studies on children are scarce and mostly concern patients of “peripubertal age”. Few data can be found in literature and do not seem to be comparable with adults. One reason for these discrepancies is the difficulty, yet, to define a cutoff value able to differentiate patients at risk from subjects not at risk [4, 21–23]. Another issue is whether this cutoff value may be valid for the entire pediatric age [24–29]. Finally, it is crucial to evaluate which criteria for class weight should be considered [24–26].
The aim of this 1-year-long longitudinal pilot study is the evaluation of the thickness of EAT observed in overweight/obese children of prepubertal age and its possible correlation with the parameters predictive of MS. This population study is important to verify whether EAT itself should be included among the predictors of MS.
Materials and methods
Subjects were 73 children (M = 39; F = 34), average age of 8.22 years (SD ± 1.35), free from previous treatments and seen at the Centre of Child Dietetics and Nutrition of the Department of Paediatrics and Paediatric Neuro-Psychiatry of the Policlinico Umberto I in Rome for obesity or other nutritional problems. Children with endocrine or syndromic causes of obesity and those under drug therapy for chronic diseases were excluded from the study. All patients were prepubertal (stage I of pubertal development according to Tanner).
The study was conducted in accordance with the guidelines proposed in the Declaration of Helsinki and approved by the local ethics committee. After obtaining written informed consent from one parent, the enrolled children were subjected to the following diagnostic procedures:
-
recording of family and personal history, with special attention to diseases such as hypertension, stroke/acute myocardial infarction, dyslipidemia, type II diabetes mellitus (NIDDM), hyperhomocysteinemia and hepatic steatosis;
-
gathering of information about habits and lifestyle, such as hours of sedentary lifestyle and sport;
-
gathering of food habits (through 24-h recall, food history and self-administered food frequency questionnaire);
-
assessment of the main anthropometric measurements (weight, height, circumferences and skinfolds) and calculation of body mass index (BMI), z score of BMI (z-BMI) and the ratio waist/height (WtHR) [6];
-
comorbidities, through physical examination and measurement of blood pressure (BP).
The weight was evaluated using a scale with steelyard, with the patient in underwear; the height was measured with a stadiometer. After BMI was calculated by the standard formula (kg/m2), patients were classified according to the z-BMI cutoffs determined by WHO [30], assigning the patients as obese if z-BMI was >2 and as overweight if z-BMI was >1.02. Waist (W), expressed in centimeters, was measured at the point located midway between the bottom of the last rib and the iliac crest [31].
Each child then underwent transthoracic ultrasound, using the MB-mode echocardiography, with probes 2–4 MHz, for the definition of the thickness of the epicardial adipose tissue at the level of the free surface of the right ventricle, from both parasternal long- and short-axis views, with the patient in the left lateral decubitus position. The measurement of EAT in this region provides the measure (in millimeters) of the maximum thickness of EAT. The maximum values at any site were measured, and the average value was considered.
The study was conducted in a single-blind manner (the sonographer operator was unaware of the metabolic parameters of the patient).
According to IDF guidelines [3, 4], only in children where we found a value of W >90th percentile by sex and age, blood test biomarkers of MS were checked. Prescribed laboratory tests were: glycemic profile [blood glucose and fasting insulin, homeostatic model assessment of insulin resistance (HOMA-IR)], lipid profile (total cholesterol, HDL cholesterol, LDL cholesterol, Tg) and liver function (transaminases).
Statistical analysis
Collected data were analyzed using Statistical Software Package for Social Sciences (SPSS Inc, Chicago, Illinois, USA) version 9.0 for Windows. All data were expressed as mean ± SD. The unpaired Student’s t test and the ANOVA analysis were used for the comparison of means and variances calculated in the different groups. Contingency tables (Chi-square test) were used for the comparison of proportions. The Pearson’s “r” correlation was used to evaluate the relation between EAT and the variables studied to investigate the MS. Multiple linear regression analysis (stepwise method) was performed with the values of EAT as the dependent variable and potential explanatory variables (independent) selected on the basis of a significant correlation with EAT. For all statistical methods, the value of p < 0.05 was considered statistically significant.
Results
The average values of the anthropometric and chemistry data are shown in Table 1. There were no statistically significant differences between males and females (data not shown).
Based on the values of the z-BMI [30, 32], patients could be grouped into three categories: obese (z-BMI >2) (48.0 % of the population considered); overweight (z-BMI >1.02) (31.5 % of the population considered); normal weight (z-BMI <1.02) (20.5 % of the population considered). None of the patients included in the study was underweight.
There were statistically significant differences among the three groups with respect to anthropometric parameters and thickness of EAT (ANOVA) (Table 2).
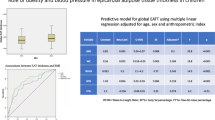
As for the relation between EAT and z-BMI in the two groups of normal weight children and overweight/obese ones, there was a positive correlation between EAT and z-BMI only in overweight/obese children (r = 0.43, p = 0.001) (see Fig. 1). There was no correlation between EAT and z-BMI in the group of normal weight children.
The population was then divided according to WtHR (<0.5 = 19.2 %, ≥0.5 = 80.8 %). We observed statistically significant differences in z-BMI (p = 0.002) and DBP (p = 0.05) (Table 3). For EAT thickness, the differences did not reach statistical significance.
The data show that 89 % of our sample had a W >90th percentile. Moreover, statistically significant differences with regard to DBP (p < 0.01) and EAT (p = 0.02) were observed when comparing patients W <90th percentile vs W >90th percentile.
According to the IDF proposal [3, 4] we checked into patients aged <10 years with W >90th percentile, paying special attention to those with a family history of risk factors for MS, who in our series represent 31 % of the whole sample vs patients with negative family antecedents. The anthropometric and laboratory characteristics as well as the value of EAT of these two subsets are shown in Table 4. There were statistically significant differences between the two groups with respect to z-BMI, W and EAT.
After comparing the correlations of the results found in these two subsets and in children with W <90th percentile (Table 5), we observed that:
-
(1)
in patients with W >90th percentile and family history of risk factors for MS (+), the value of EAT correlates positively with z-BMI, W, WtHR, Tg, insulin and HOMA-IR and negatively with HDL. The multiple regression analysis (stepwise method) shows a weak dependence of EAT on W (R2 = 0.36; p = 0.001) and an increase of its dependence when considering at the same time W and blood glucose (R2 = 0.50; p = 0.000);
-
(2)
in patients with W >90th percentile and no family history of risk factors for MS (−), the value of EAT correlates positively with z-BMI, W, WtHR and Tg. The multiple regression analysis shows a strong dependence of EAT only on WtHR (R2 = 0.84, p = 0.000);
-
(3)
in patients with W <90th percentile, the value of EAT does not correlate with any considered parameters; hence the regression analysis was not performed.
Discussion
EAT thickness in the adult population has been studied and evaluated by different groups as an index of visceral adiposity [7, 9–12, 14, 16–20], also in correlation with the MS [1–4].
Measurements of EAT in the pediatric population are more recent [24–29]. The lack of standard criteria to define the cutoffs of overweight and obesity in the pediatric population [30, 32] makes it difficult to give precise values of the normal thickness and to establish a correlation as accurate as possible between EAT and clinical status. To make matters worse, (1) even the definition of MS is still controversial in children and we refer mainly to an increased risk [3, 4]; (2) the threshold of 10 years of age established by the IDF for the diagnosis of MS is a criterion which is entirely arbitrary; (3) the changes induced by puberty, and that can affect many metabolic and anthropometric parameters (even EAT?), are neither easily relatable to a precise age, nor in a precise way to a clinical stage of development.
In our study, we chose to use z-BMI as identified by the WHO [30, 32] to define overweight/obesity. Without a shared opinion on what system of classification to use, we found the use of this standard useful, since z scores and percentiles have a 1:1 equivalence in a normal distribution. Thus, for a given age, a specified difference in z score represents the same difference in normalized BMI units at any z score level, unlike percentiles [21–23]. Based on this benchmark, 79.4 % of our sample is overweight/obese (47.9 % obese, 31.5 % overweight).
Although important for a first distinction between normal weight, overweight and obese, neither BMI nor any of its derivatives are markers of cardiometabolic risk. For this reason, studying EAT in relation to weight or weight classes is not the most useful way to proceed. Nonetheless, the behavior of EAT in different weight classes is also interesting, since in normal weight patients z-BMI does not correlate at all with EAT, while in overweight/obese patients there is a strong positive correlation between the two parameters.
When studying the relations to cardiometabolic risk, two main parameters are currently considered [6]: WtHR and W (or the percentile of W for children). Both are pathological in our population, even sometimes in subjects not classified as overweight/obese based on z-BMI. WtHR is pathological in 80.8 % of the sample, while W is >90th percentile in 89 % of the subjects.
So, we decided to use WtHR and W to compare the results of EAT. Patients with pathological WtHR had an EAT average thickness higher than subjects with normal WtHR. This difference, although of considerable size and with average values not overlapping, does not reach statistical significance, perhaps because of both the small size of the sample and the gap between classes.
The IDF suggests, however, that special attention should be given to children who, while bearing a high percentile of W, also have a family history of early cardiometabolic events. In our study, this relates to 57.5 % of the population.
While patients with W <90th percentile, regardless of their family history, do not show any significant difference between the parameters evaluated, in the subgroup of patients with W >90th percentile, after sub-dividing them into two subsets according to positive or negative family history for MS risk factors, there are statistically significant differences both for z-BMI and EAT, with both parameters showing higher values in patients with positive family history for cardiometabolic risk.
There is a high probability that EAT might relate to cardiometabolic risk already during pediatric age, and this is supported by the statistical relations linking EAT, anthropometric parameters and metabolic parameters. In patients with pathological percentiles of W and a family history positive for MS risk factors, EAT thickness correlates not only with the anthropometric parameters (z-BMI, W, WtHR), but also with the metabolic ones. In particular, EAT thickness correlates positively with Tg, insulin, and HOMA-IR, which is an important factor in the genesis of several obesity-related diseases; it correlates negatively with HDL, which is known as an important protective factor for cardiovascular disease [33, 34].
Moreover, some anthropometric (W) and metabolic (glucose) factors seem to have a synergic effect on EAT thickness, suggesting that EAT might be strongly influenced not only by weight gain, but also by the onset of endocrine abnormalities. In support, it must be stressed that, in patients with W >90th percentile but negative family history, EAT thickness correlates with the anthropometric parameters, yet, but not with the metabolic ones. A possible exception to this consideration is that also in this subset, the EAT thickness correlates positively with Tg; it is well known, however, that Tg levels are related to the abuse of carbohydrates in the diet [35–38], a typical feature of the vast majority of overweight/obese Italians even in the pediatric age.
EAT seems therefore to be subjected to the same pathogenetic factors (environmental? genetic? epigenetic?), that are the basis of the family involvement in the development of cardiometabolic disorders. All of this further supports the IDF suggestion to keep close tabs on children in whom central obesity and family risk factors for MS gather together.
Mazur [25] has recently demonstrated a close correlation between the EAT thickness and W, indicating EAT as a reliable index of rapid assessment for the definition of visceral adiposity and as a marker of MS in subjects of peripubertal age.
Our work, however, is the first to consider only prepubertal children, in whom the bias represented by the impact of sex hormones on the development and deposition of visceral adipose tissue can be completely ruled out. The exclusion of this important confounding factor, not left out by any other previous pediatric work in the literature [24–28], gives the results reported here a greater reliability.
Limitations
Although our study is in line with the literature, the major limitation of this work is the small sample and the unequal distribution between normal weight and overweight/obese.
A second limit, for other reasons a point of force (see above), is the use of patients under 10 years of age, with the relative impossibility of establishing a diagnosis of MS (according to IDF). Because of these limits, it was not possible to perform an analysis of the ROC curve to propose a cutoff value for normality thickness of EAT in relation to the diagnosis of MS. The small size of the sample has also restrained from detecting any significant differences in the thickness of EAT between males and females.
Finally, due to the stochastic recruitment of patients in this study, the subpopulations identified are numerically inhomogeneous and, as such, difficult to compare.
We intend to continue to expand the case study to better evaluate these correlations and to assess the progress of patients already recruited over time, to highlight potential improvements following the reorganization of the eating habits and lifestyles.
References
Eckel RH, Grundy SM, Zimmet PZ (2005) The metabolic syndrome. Lancet 365:1415–1428. doi:10.1016/S0140-6736(05)66378-7
Alberti KGMM, Zimmet PZ, Shaw JE (2005) The metabolic syndrome—a new world-wide definition. Lancet 366:1059–1062. doi:10.1016/S0140-6736(05)67402-8
Zimmet P, Alberti G, Kaufman F, Tajima N, Silink M, Arslanian S, Wong G, Bennett P, Shaw J, Caprio S. International Diabetes Federation Task Force on Epidemiology and Prevention of Diabetes. (2007) The metabolic syndrome in children and adolescents. Lancet 369(9579):2059–61. doi:10.1016/S0140-6736(07)60958-1
Alberti G, Zimmet P, Kaufman F, Tajima N, Silink M, Arslanian S, Wong G, Bennett P, Shaw J, Caprio S (2007) The IDF consensus definition of the metabolic syndrome in children and adolescents. International Diabetes Federation. http://www.idf.org/metabolic-syndrome/children
Maffeis C, et al (2006) Obesità del bambino e dell’adolescente: consensus su prevenzione, diagnosi e terapia. Argomenti di Pediatria 1(06). www.ecog-obesity.eu/papers/Consensus_Italia.pdf
Maffeis C, Banzato C, Talamini G (2008) Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr 152:207–213. doi:10.1016/j.jpeds.2007.09.021
Iacobellis G, Corradi D, Sharma AM (2005) Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med 2:536–543. doi:10.1038/ncpcardio0319
Iacobellis G, Pond CM, Sharma AM (2006) Different “weight” of cardiac and general adiposity in predicting left ventricle morphology. Obesity 14:1679–1684. doi:10.1038/oby.2006.192
Sacks HS, Fain JN (2007) Human epicardial adipose tissue: a review. Am Heart J 153:907–917. doi:10.1016/j.ahj.2007.03.019
Iacobellis G, Pistilli D, Gucciardo M et al (2005) Adiponectin expression in human epicardial adipose tissue in vivo is lower in patients with coronary artery disease. Cytokine 29:251–255. doi:10.1016/j.cyto.2004.11.002
Mazurek T, Zhang L, Zalewski A et al (2003) Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 108:2460–2466. doi:10.1161/01.CIR.0000099542.57313.C5
Baker AR, Silva NF, Quinn DW et al (2006) Human epicardial adipose tissue expresses a pathogenic profile of adipocytokines in patients with cardiovascular disease. Cardiovasc Diabetol 13:1. doi:10.1186/1475-2840-5-1
Chaldakov GN, Fiore M, Stankulov IS et al (2004) Neurotrophin presence in human coronary atherosclerosis and metabolic syndrome: a role for NGF and BDNF in cardiovascular disease? Prog Brain Res 146:279–289. doi:10.1016/S0079-6123(03)46018-4
Kremen J, Dolinkova M, Krajickova J et al (2006) Increased subcutaneous and epicardial adipose tissue production of proinflammatory cytokines in cardiac surgery patients: possible role in postoperative insulin resistance. J Clin Endocrinol Metab 91:4620–4627. doi:10.1210/jc.2006-1044
Xu Y, Cheng X, Hong K, Huang C, Wan L (2012) How to interpret epicardial adipose tissue as a cause of coronary artery disease: a meta-analysis. Coron Artery Dis 23(4):227–233. doi:10.1097/MCA.0b013e328351ab2c
Iacobellis G, Assael F, Ribaudo MC, Zappaterreno A, Alessi G, Di Mario U, Leonetti F (2003) Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Obes Res 11(2):304–310
Iacobellis G, Ribaudo MC, Assael F et al (2003) Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J Clin Endocrinol Metab 88:5163–5168. doi:10.1210/jc.2003-030698
Iacobellis G, Ribaudo MC, Zappaterreno A, Iannucci CV, Leonetti F (2004) Relation between epicardial adipose tissue and left ventricular mass. Am J Cardiol 94:1084–1087. doi:10.1016/j.amjcard.2004.06.075
Iacobellis G, Leonetti F (2005) Epicardial adipose tissue and insulin resistance in obese subjects. J Clin Endocrinol Metab 90:6300–6302. doi:10.1210/jc.2005-1087
Iacobellis G, Singh N, Leonetti F, Sharma AM (2007) Relationship of epicardial adipose tissue with atrial dimensions and diastolic function in morbidly obese subjects. Int J Cardiol 115:272–273. doi:10.1016/j.ijcard.2006.04.016
Flegal KM, Ogden CL (2011) Childhood obesity: are we all speaking the same language? Adv Nutr 2(2):159S–166S. doi:10.3945/an.111.000307
Simmons RK, Alberti KG, Gale EA, Colagiuri S, Tuomilehto J, Qiao Q, Ramachandran A, Tajima N, Brajkovich Mirchov I, Ben-Nakhi A, Reaven G, Hama Sambo B, Mendis S, Roglic G (2010) The metabolic syndrome: useful concept or clinical tool? Report of a WHO expert consultation. Diabetologia 53(4):600–605. doi:10.1007/s00125-009-1620-4
Golley RK, Magarey AM, Steinbeck KS, Baur LA, Daniels LA (2006) Comparison of metabolic syndrome prevalence using six different definitions in overweight pre-pubertal children enrolled in a weight management study. Int J Obes (Lond) 30(5):853–860. doi:10.1038/sj.ijo.0803195
Hizli S, Ozdemir O, Abaci A, Razi CH, Kabakuş N (2010) Relation of subepicardial adipose tissue thickness and clinical and metabolic parameters in obese prepubertal children. Pediatr Diabetes 11(8):556–562. doi:10.1111/j.1399-5448.2010.00644.x
Mazur A, Ostański M, Telega G, Małecka-Tendera E (2010) Is epicardial fat tissue a marker of metabolic syndrome in obese children? Atherosclerosis 211(2):596–600. doi:10.1016/j.atherosclerosis.2010.02.036
Manco M, Morandi A, Marigliano M, Rigotti F, Manfredi R, Maffeis C (2013) Epicardial fat, abdominal adiposity and insulin resistance in obese pre-pubertal and early pubertal children. Atherosclerosis 226(2):490–495. doi:10.1016/j.atherosclerosis.2012.11.023
Abaci A, Ozdemir O, Hizli S, Razi CH, Kabakus N (2010) Subepicardial adipose tissue thickness and its relation with anthropometric and clinical parameters in pubertal obese children. J Endocrinol Invest 33(10):715–719. doi:10.3275/6972
Ozdemir O, Hizli S, Abaci A, Agladioglu K, Aksoy S (2010) Echocardiographic measurement of epicardial adipose tissue in obese children. Pediatr Cardiol 31(6):853–860. doi:10.1007/s00246-010-9720-y
Haffner SM (2007) Abdominal adiposity and cardiometabolic risk: do we have all the answers? Am J Med 120(9 Suppl 1):S10–S16. doi:10.1016/j.amjmed.2007.06.006
Wang Y, Chen H-J. Use of percentiles and Z-scores in anthropometry. http://www.springer.com/cda/content/document/cda_downloaddocument/9781441917874-c1.pdf?SGWID=0-0-45-1313138-p174264865
Lohman TG, Roche AF, Martorell R (1988) Anthropometric standardization reference manual. Human Kinetics Books
World Health Organization (1995) Physical status: the use and interpretation of anthropometry. Report of a WHO expert committee. World Health Organ Tech Rep Ser 854:1–452
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR (1977) High density lipoprotein as a protective factor against coronary heart disease. the Framingham Study. Am J Med 62(5):707–714
Rubenfire M, Brook RD (2013) HDL Cholesterol and Cardiovascular Outcomes: what is the evidence? Curr Cardiol Rep 15(4):349. doi:10.1007/s11886-013-0349-3
Ma Ma Y, Li Y, Chiriboga DE, Olendzki BC, Hebert JR, Li W, Leung K, Hafner AR, Ockene IS (2006) Association between carbohydrate intake and serum lipids. J Am Coll Nutr 25(2):155–163
Yang EJ, Chung HK, Kim WY, Kerver JM, Song WO (2003) Carbohydrate intake is associated with diet quality and risk factors for cardiovascular disease in US adults: NHANES III. J Am Coll Nutr 22(1):71–79
Marshall JA, Kamboh MI, Bessesen DH, Hoag S, Hamman RF, Ferrell RE (1996) Associations between dietary factors and serum lipids by apolipoprotein E polymorphism. Am J Clin Nutr 63(1):87–95
Truswell AS (1994) Food carbohydrates and plasma lipids–an update. Am J Clin Nutr 59(3 Suppl):710S–718S
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study “Epicardial adipose tissue and signs of metabolic syndrome in children” by Andrea Vania and co-workers was approved by the ethics committee of Rome University’s Policlinico Umberto I, Italy
Informed consent
Written informed consent were obtained from all participants.
Rights and permissions
About this article
Cite this article
Barbaro, G., Piedimonte, A., Podagrosi, M. et al. Epicardial adipose tissue and signs of metabolic syndrome in children. Eat Weight Disord 21, 269–276 (2016). https://doi.org/10.1007/s40519-015-0221-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-015-0221-0