Abstract
Purpose
Bradycardia and abnormal cardiac autonomic function are related to increased mortality in anorexia nervosa (AN). The aim of this study was to assess heart rate (HR) and HR variability of young adolescents with AN as compared to controls by means of wearable sensors and wireless technologies.
Method
The ECG signal was recorded in 27 AN girls and 15 healthy girls at rest using a wearable chest strap. The tachogram, the mean intervals between R peaks (meanRR), the root mean square of successive differences (RMSSD), the power of low-frequency (LF) and high-frequency (HF) bands and the LF/HF ratio were assessed.
Results
All AN girls showed a reduced HR and an increased meanRR and RMSSD. An HF increase, a LF decrease, and a LF/HF reduction indicated a prevalence of the parasympathetic on sympathetic activity.
Conclusions
The instruments used in this pilot study were feasible, unobtrusive and extremely suitable in AN subjects who are burdened by high incidence of cardiovascular mortality; their application could open to new approaches of vital signs monitoring in hospitals as well as in home settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anorexia nervosa (AN) is a major eating disorder due to distortions of body shape and fear of gaining weight [1]; it is characterized by persistent behavior that interferes with weight gain.
The aggregate mortality rate in AN patients is approximately 5.6 % per decade [2]; a standardized mortality ratio in AN patients is 10.5 times higher than that of age-matched healthy controls [3].
Cardiac morpho-functional complications are frequently reported in AN such as reduction in left ventricular (LV) mass and modest and reversible reduction in LV function. Pericardial effusion is frequently encountered, however, only anecdotically it can lead to cardiac tamponade [4].
Sinus bradycardia is the most common cardiac complication. Extreme bradycardia with values <30 beats/min has also been reported [5] and ventricular arrhythmias represent one of the major concerns since they may lead to sudden death in AN patients [6]. Prolongation of the QT interval and abnormalities in QT dispersion have also been described in AN; however, the role of QT duration and QT dispersion is still controversial [7] as a cause of major cardiac arrhythmias.
Patients with eating disorders may present a wide range of autonomic disturbances, which have been mostly studied by means of heart rate variability (HRV) but also by blood pressure variability as well as baroreflex sensitivity, both in adults and in adolescents [8–22]. In the majority of patients, an increased HRV in AN subjects associated toparasympathetic/sympathetic imbalance with parasympathetic dominance has been described [8–14, 16, 20–22]. There is also a small group of studies that found a decrease of HRV or sympathetic excess in AN subjects [15, 17] and a fraction of studies that did not reveal any differences between AN and control group [18, 19]. The increased sympathetic activity is associated to high levels of anxiety and depression [23] of these subjects, therefore, co-morbid state of anxiety and depression might influence HRV measures.
Therefore, a recent meta-analysis has underlined the conflicting results, which have been reported to be due, at least in part, to the different methodologies applied so far [24].
Although prognostic data of HRV in AN subjects are not univocal, it should be considered that, as in other studied populations, HRV abnormalities may represent a predictor for cardiac mortality risk in AN [10, 18, 24]. Therefore, HRV monitoring may help to characterize those subjects who show more profound autonomic dysfunction, providing an important mean for intervention to avoid occurrence of major or even fatal arrhythmias.
In AN patients, short-term HRV analysis is currently performed by ECG recordings in supine position in adolescents or adult subjects [18], after drug administration to obtain complete cholinergic blockade [8] or alternating supine or standing position, which requires patient hemodynamic stability and cooperation [9].
At present, HRV evaluation is performed in the hospital setting for short-term acquisitions, while 24- or 48-h ECG Holter monitoring is used for long-term analysis, which can be performed also out-of-hospital. However, in the latter case some potential problems have to be taken into account: restricted recording time due to a limited storage capacity, and a large amount of wires connecting the device to the patient, which, especially in young subjects, may determine non-compliance to long-lasting recordings even in home settings.
In the last years, focus has been put on early onset (<13 years) AN suggesting that these patients may be at higher risk due to more rapid loss of weight [25].
In adolescents and, in particular, in subjects with early onset AN, monitoring of possible cardiovascular complications deserves particular attention and the use of unobtrusive technologies––which can be well tolerated by the patient––may represent an important choice for diagnosis and follow up.
The use of wearable sensors in medicine recognizes a growing research interest. Wireless technology can play a key role to gain the continuity of care in a person-centric model, focusing on a knowledge-based approach, which integrates past and current data of each subject together with statistical evidences. This approach provides the opportunity to monitor subjects in different pathologic conditions in an unobtrusive way [26].
To reach this goal, wearable devices need to be easy to use, comfortable to wear and efficient in power consumption, privacy compliant, with very low failure rates and high accuracy in triggering alarms.
At present, no studies are available on the possible role of wearable sensors in AN young adolescents. The present study was aimed to assess the feasibility of a method based on non-intrusive wearable sensors combined with wireless technologies for data acquisition for short time recordings of heart rate (HR) and HRV in a group of young adolescent girls affected by early onset AN restrictive subtype as well as to compare the results with those obtained in a group of healthy adolescents of comparable age. A chest strap-based wearable solution—developed in our Institute in collaboration with SHIMMER™ Research—able to extract one-lead ECG signal was applied as acquisition system.
Materials and methods
Participants
Twenty-seven adolescent girls with AN in line with DSM-IV and DSM-V standards [1] were consecutively enrolled to be part of the experimental group in the Child and Adolescent Eating Disorders Unit of the IRCCS Stella Maris Foundation.
Exclusion criteria were the presence of psychotic symptoms, the Wechsler Full Scale IQ < 80, the presence of pathologies not related to eating disorders, and current or previous episodes of substance abuse. Furthermore, patients with binging and/or purging behaviors were specifically excluded from the study.
Data collection together with blood samples were obtained in all subjects within 3 days of patient hospitalization before any pharmacologic treatment was started, if required.
A sample of 15 healthy adolescent girls was enrolled as control group. Controls were recruited from students of a middle and a high school in the metropolitan area of Pisa. All control subjects attended regular classes and schools without a support teacher.
The research protocol was approved by the Institutional Review Board of the IRCCS Stella Maris Foundation.
Baseline 12-lead ECG
A resting 12-lead ECG was recorder in both AN and controls at the beginning of each session. QT duration was measured from the beginning of the QRS complex to the end of the T wave; corrected QT (QTc) was calculated according to the Bazett formula.
Echocardiographic measurements
All the subjects underwent a cardiovascular examination comprehensive of a conventional 2D and M-mode Doppler echocardiographic examination by means of a commercially available instrument (General Electric Vivid I, USA). The echocardiographic examination was performed in the left lateral decubitus position and in the supine position for the subxifoid approach. M-mode echocardiography was used for quantitating dimensions of chambers and walls. The left ventricular internal dimensions were measured in end diastole (LVED) and in end systole (LVES). Interventricular septal wall thickness (IVSWT) and left ventricular posterior wall thickness (LVPWT) were measured in end diastole according to the American Society of Echocardiography [27]. LV mass index (LVMi) was calculated in each subject and related to body surface area. LV end-diastolic and systolic volumes and derived ejection fraction were assessed by the biplane summation method from the apical four-chamber view [28]. Pericardial effusion was defined as the presence of an epicardial to pericardial echo-free space in diastole with a minimum of 2 mm. For assessment of the transmitral flow, the transducer was positioned at the cardiac apex and flow measured by pulsed wave Doppler from the apical four-chamber view, with the sample volume placed at the level of mitral valve leaflet tips. E peak (peak transmitral flow velocity in early diastole), A peak (peak transmitral flow velocity in late diastole) and E/A ratio were analyzed.
ECG monitoring
After the complete echocardiographic exam, the electrocardiographic signals were acquired for 15 min while the patients lied in a supine position on an ambulatory bed in a quiet, shaded room. The patients were asked nothing except to relax.
The ECG was recorded from all the AN subjects using a wearable sensing set developed by CNR re-designing the ECG SHIMMER™ based-platform [29]. The wearable system is realized as a chest strap and embodying three disposable electrodes, the related electrical connections and a dedicated portable integrated electronic board placed at the level of the thorax. The three embedded electrodes were positioned as shown in Fig. 1a. In analogy with the Einthoven triangle electrode one corresponded to the right arm of the subject and electrode two to the left arm.
The electronic board includes the signal conditioning to reduce the number of artifacts and a low-power Bluetooth communication protocol for data transmission. The lightweight (~100 g) and compact form factor of the sensor makes it very suitable for physiological sensing applications. In Fig. 1, the wearable chest strap, which incorporates the compact device designed for continuous monitoring of ECG is shown. One of the most important applications of the wearable ECG chest strap is the HRV analysis, performed following the Heart Rate Variability Guidelines [30]. The wearable device was plugged into a lightweight strap, which is fully washable, guarantees an optimal and comfortable contact, adapting itself to the body shape.
The sampling frequency of signals was 100 Hz. Although an optimal range should be 250–500 Hz because a low sampling rate may produce a jitter in the estimation of the R peaks, which considerably alters the spectrum, a sampling frequency ≥100 Hz may behave satisfactorily if an algorithm of interpolation (e.g. parabolic) is used to refine the R peaks [31, 32].
ECG chest strap validation
The chest strap was validated prior to the present study in a group of healthy subjects [33]. The performance of the system was evaluated at rest and during working activity. In all the scenarios, the chest strap and the gold standard Holter device (ELA medical, Milan, Italy) simultaneously recorded the ECG for 3 h.
The resulting waveform confirmed the signal quality was comparable to that acquired by the ELA Holter [30]. Moreover, the ECG chest strap provided readable signals for more than 95 and 99 % of the time of acquisition while the subjects were at work and at rest, respectively.
The R peaks detected using the developed algorithm for the ECG chest strap were compared to the ones annotated in different report provided by the ECG Holter.
The mean percentage of RR measurements was lower than the 10 % (maximum value established by the CEI ISO60601-2-47 about RR calculation) during the whole validation.
The information provided by spectral analysis, was equal to the one obtained by ELA Holter. This validation study confirmed that the ECG chest strap system has a high accuracy in terms of HRV assessment, and so it can be use in clinical applications. Recently, the same method was applied during stress [34] and for the monitoring of patients with congestive heart failure [35].
Signal analysis
ECG signals were pre-processed in Matlab through a stepwise filtering process oriented to remove typical ECG artifacts and interferences. A Kalman filter was initially applied to the signal and then an IIR filter (band-pass) of order 29 and bandwidth 25–35 Hz was used. A parabolic interpolation was applied to the signal to avoid the jitter problems induced by the low sampling rate.
Once pre-processed the Pan-Tompkins method for the detection of QRS complex was applied [36] and the tachogram extracted, which was first submitted to a time-domain analysis to obtain temporal features of HR and HRV.
From the tachogram, the RR intervals that are defined the time measurements between the R wave of one heartbeat and the R wave of the preceding heartbeat were extracted. The following parameter were extracted: mean HR, the mean RR intervals (RRmean), the standard deviation of RR intervals (RRdevstd), the difference between the longest and shortest RR interval (diffRR) and the root mean square of successive differences (RMSSD). RRmean, RRdevstd, diffRR and RMSSD are all indices of HRV.
The power spectrum density (PSD) was calculated using the parametric autoregressive Yule-Walker model of order 9 [37, 38]. The features extracted from the PSD and estimated for each frequency band, low frequency (LF: 0.03–0.15 Hz) and high frequency (HF: 0.15–0.40 Hz), included absolute powers, peak frequencies (Max LF and Max HF) and the LF/HF power ratio. The power of each band was normalized to the total power of the spectrum.
Statistical analysis
Statistical comparisons of the autonomic function outcome measures were performed using SPSS software (SPSS Inc, Chicago, IL, USA) [39]. The Shapiro–Wilk test was applied to test the normality of the variables. Type I error for statistical tests of hypothesis was equal to 0.05. When the variables had non-normal distribution data were compared using the Kolmogorov–Smirnov non-parametric test for independent samples. A comparison between patients and controls was performed. The AN girls and the controls girls were described in term of demographic, personal, cardiovascular echocardiographic and HRV data. The analyses were repeated also using BMI as covariate in an MANCOVA test. When a non-parametric test was required, variables and covariate were transformed in ranks and a MANCOVA on ranks was performed.
Bivariate correlations between the outcome measures and age, BMI and E/A ratio were also investigated using Pearson’s correlation coefficient analysis both in AN girls and in controls. In AN subjects, the correlations between HR and HRV parameters and the age of onset or the duration of disease as well with the biochemical data were also investigated.
Results
Group characteristics
All subjects completed the baseline cardiovascular examination. There were no significant between-group differences in age (AN group: mean age: 14.6 ± 2.2 years, range 8–18 years; control group: mean age: 14.5 ± 1.5 years, range 11–17 years; p = 0.34), while, as expected, BMI was found significantly lower in AN patients than in controls (AN group mean BMI 15.7 ± 2.1 kg/m2; control group mean BMI 20.5 ± 2.2 kg/m2; p < 0.001). The mean value of the age of onset in AN group was 13.2 ± 1.7 years while the mean value of duration of disease (from the age of onset to the moment of the hospitalization) was 1.5 ± 1.2 years. The main clinical and biochemical characteristics of the AN subjects are reported in Table 1. It is evident that no significant biochemical abnormalities were observed: in particular, one AN girl only showed a slightly reduced TSH value, and four presented a fT4 level mildly below lower limit. The electrolyte balance was normal in all subjects, except in one girl who showed a borderline K+ value.
All patients showed typical psychiatric comorbidities on Axis I, such as Major Depressive Episode (59.23 %), Dysthymic Disorder (37 %), Generalized Anxiety Disorder (11.11 %), Oppositional Defiant Disorder (3.7 %).
Basal 12-lead ECG
HR was significantly lower in AN than in controls (AN mean: 65.04 ± 10.80 bpm, controls mean: 78.54 ± 10.11 bpm, p = 0.001).The QT values were: AN: 393 ± 23 ms, controls: 380 ± 22 ms p = 0.04, and QTc: 405 ± 25 vs 428 ± 7.5 ms, p = 0.001. Applying the correction for BMI only QTc difference remained significant (p = 0.04). None in the AN group as well as in the controls showed a QTc >440 ms.
2D Doppler echocardiography
A normal LV function (LV ejection fraction ranging from 60 to 72 %, mean 64 %) was found in all the studied AN girls and was comparable to the control group (mean LV ejection fraction 65 %). No clinically significant valvular pathologies could be reported in both patients and controls. LVMi was lower in AN subjects as compared to controls (AN mean: 68.24 ± 10.91, controls mean: 75.66 ± 11.12, p = 0.04). AN girls showed a reduced E peak velocity as compared to controls (AN: 83.29 ± 14.83 cm/s, controls: 93.13 ± 13.87 cm/s, p = 0.042) and A peak velocity (AN: 38.73 ± 9.49 cm/s, controls: 53.97 ± 13.71 cm/s, p < 0.001); consequently E/A ratio was greater in the AN group (AN: 2.16 ± 0.64, controls: 1.67 ± 0.24, p = 0.002). After correcting for BMI only A peak (p = 0.02) and E/A (p = 0.04) remained significant.
A mild, localized, not hemodynamically significant pericardial effusion (max 4 mm in end diastole) was detected in ten AN girls and in none of the controls. No relation between presence of pericardial effusion and TSH levels could be reported for the AN girls.
HR and HRV analysis
The procedure was well tolerated by all the subjects under study, who were all able to complete the required recording without complaining about the chest strap during the 15-min recording.
All recordings were suitable for off line analysis. Results are summarized in Table 2.
The comparison of the individual temporal features showed that in AN subjects mean HR was decreased (AN: 62.05 ± 13.84, controls: 77.97 ± 10.31, p < 0.001). RRmean (AN: 1000 ± 250 ms, controls: 790 ± 90 ms, p = 0.002), diffRR (AN: 270 ± 70 ms, controls: 210 ± 30 ms, p = 0.006), RMSSD (AN: 130 ± 110 ms, controls: 50 ± 20 ms, p = 0.008) and RRdevstd [AN: 77 (45–13) ms, controls: 60 (40–70) ms, p = 0.028] were increased in AN with respect to controls.
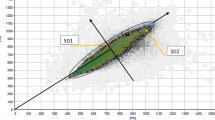
The comparison between AN and controls of the frequency features showed a decreased normalized LF power (mean: 0.42 ± 0.18, vs 0.62 ± 0.19, p = 0.001) and an increased normalized HF power (mean: 0.62 ± 0.17 vs 0.46 ± 0.18, p = 0.001) is. Overall, the ratio between LF and HF was lower in AN than in controls [AN mean: 0.69 (0.43–0.27), controls mean: 2.07 (0.85–5.29), p = 0.002]. All these comparisons remained significant after BMI correction except for RRdevstd (Table 1, last column).
In Fig. 2, two examples of PSD spectra of a control girl and a girl with AN are reported. It is evident the increase of high frequencies in the patient when compared to the healthy control.
Correlations
A significant positive correlation was found only between BMI and mean HR (r = 0.4, p = 0.04) in AN group. No relation could be reported between the studied HRV parameters and clinical data as age of onset or duration of the disease, electrolytes, TSH and fT4. When HRV parameters were related to E/A ratio, a mild, although not significant, negative relation was reported with RRdevst. No significant correlations between the abovementioned parameters were found in the control group.
Discussion
The results of this study show that wearable sensors combined with wireless technologies are feasible in young AN adolescents, providing useful information on HR and HRV.
As compared to controls, young AN adolescent girls have significantly lower heart rate (HR) and higher heart rate variability (HRV), lower low-frequency components, elevated high-frequency components, and decreased low to high-frequency power ratio. Therefore, AN patients show a reduced cardiovascular sympathetic and an increased parasympathetic responsiveness when compared with healthy controls despite a normal regional and global LV function. A relation between HR and BMI in the AN group was reported and supports already published data in young adults with AN [40]. In the AN group, QT duration was slightly prolonged as compared to controls; QTc according to Bazett formula, which takes into account RR duration, was shorter in AN, due to the reduced baseline HR, as compared to controls.
No relation could be found between electrocardiographic and echocardiographic parameters. Besides the documentation of non-hemodynamically significant pericardial effusion, the only interesting cardiovascular finding was the lower LVMi as compared to controls, in line with previous reports [41]. An increased E/A ratio of the transmitral flow due to the significant reduction in A wave peak, was found in the studied population, according to previously published data [13, 42]. No significant relation between E/A ratio and HRV parameters could be reported, although in our study group, a mild-negative relation between RRdevst and E/A ratio was observed, comparable to previously published data [13].
We did not record menstrual cycles nor in AN subjects or controls and they are known to impact on HRV measures [43]. However, Bomba et al. [22] have shown that in AN patients with normogonadotropic functional hypothalamic amenorrhea, HRV values were largely similar to controls in spite of the absence of cycles. Moreover, in DSM-V the possibility of excluding amenorrhea from the diagnostic criteria of AN has been evaluated [43]. A second limitation is the lack of biochemical data that have been shown to be associated to autonomic function [44, 45].
At present, changes of autonomic nervous system in AN are not univocally reported: some studies showed a parasympathetic/sympathetic imbalance with parasympathetic dominance and decreased sympathetic modulation; other studies described sympathetic dominance; and a small but not negligible group of papers could not identify any autonomic differences in comparison to control samples [24]. Differences in the previous studies maybe partially due to differences in the method of measurements and in the characteristics of patients. First, as pointed out in the “Introduction”, parasympathetic/sympathetic balance is influenced by anxiety and depression of subjects. Correlating HR and HRV parameters with parameters measuring stress of patients might be useful in the future to clarify the role of these co-morbid states in HRV changes. In addition, only two studies have been performed on adolescents [13, 22]. In both studies, the authors found an increased RMSSD, SDRR and HF and a decreased LF/HF. The results of these studies confirmed by ours suggest that, at least in adolescence, there is a parasympathetic prevalence of autonomic function in anorexia. Lower HR in AN group also confirms the result of increased parasympathetic activity. This physiological response in AN patients could be considered as a possible mechanism of compensation to starvation to reduce energy consumption [46] and also as a protective factor for arrhythmic risk [47].
The agreement between the results of the present study with previous findings on adolescent girls with AN strengthen the clinical validity of our technologies in assessing HR and HRV in anorexia.
Since still HRV assessment represents a tool for evaluation of AN subjects who are at increased arrhythmic risk, recent papers warrant the use of new methodological approaches for a more thorough comprehension of the autonomic system in this specific high-risk group of patients [24]. In this respect, the use of wireless technologies may represent a completely new approach for HRV assessment in AN.
These technologies provide a more naturalistic and unobtrusive way of recording with respect to standard method; this is particularly important in patients with a reduced compliance to medical evaluations, such as AN and in particular young patients. In addition, this technical opportunity could also provide a better understanding of the physiological phenomenon, since a large amount of data (more than with conventional ECG recording) can be collected, thus providing the substrate for a more extensive medical interpretation and possibly offering a personalized therapeutic model of intervention.
This study was aimed to test the feasibility of wearable technologies in a pathologic condition not previously studied with this new approach and characterized by high mortality. The promising results obtained in a quite ambulatory room may foresee the use of wearable systems for signal acquisition of cardiovascular parameters also in a natural environment like home setting, without interferences and possible pitfalls due to the use of wires. Thus, future research on the possible shifting from invasive approaches (e.g. multi-electrodes ECG holters) to minimally invasive techniques for the extraction of physiologic parameters during daily life is warranted for a simpler, more natural, and less stressful monitoring of young adolescents.
Limitations of the study
The main limitation of the study is represented by the lack of a head-to-head comparison between chest strap-derived ECG parameters and 24 h ECG Holter monitoring. However, since the chest strap equipment has been previously validated in healthy subjects and used in pathologic conditions, it was considered reliable also in the population that was particularly not compliant in terms of additional long-lasting recordings. Moreover, we did not investigate laboratory data in controls. However, only one AN girl had a borderline serum potassium level and another one a borderline TSH level, which could have influenced the results. Finally, a relatively small sample size of the subjects may represent another limitation of the study.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington
Sullivan PF (1995) Mortality in anorexia nervosa. Amer J Psychiatry 152:1073–1074
Birmingham CL, Su J, Hlynsky JA, Goldner EM, Gao M (2005) The mortality rate from anorexia nervosa. Int J Eat Disord 38:143–146. doi:10.1002/eat.20164
Polli N, Blengino S, Moro M, Zappulli D, Scacchi M, Cavagnini F (2006) Pericardial effusion requiring pericardiocentesis in a girl with anorexia nervosa. Int J Eat Disord 39(7):609–611. doi:10.1002/eat.20307
Casiero D, Frishman WH (2006) Cardiovascular complications of eating disorders. Cardiol Rev 14(5):227–231. doi:10.1097/01.crd.0000216745.96062.7c
Neumarker KJ (1997) Mortality and sudden death in anorexia nervosa. Int J Eat Disord 21(3):205–212. doi:10.1002/(SICI)1098-108X(199704)21:3<205:AID-EAT1>3.0.CO;2-O
Nussinovitch M, Gur E, Kaminer K, Volovitz B, Nussinovitch N, Nussinovitch U (2012) QT variability among weight-restored patients with anorexia nervosa. Gen Hosp Psychiatry 34(1):62–65. doi:10.1016/j.genhosppsych.2011.06.012
Kollai M, Bonyhay I, Jokkel G, Szonyi L (1994) Cardiac vagal hyperactivity in adolescent anorexia nervosa. Eur Heart J 15(8):1113–1138
Kreipe RE, Goldstein B, De King DE, Tipton R, Kempski MH (1994) Heart rate power spectrum analysis of autonomic dysfunction in adolescents with anorexia nervosa. Int J Eat Disord 16(2):159–165. doi:10.1002/1098-108X(199409)16:2<159:AID-EAT2260160207>3.0.CO;2-H
Petretta M, Bonaduce D, Scalfi L, de Filippo E, Marciano F, Migaux ML, Themistoclakis S, Ianniciello A, Contaldo F (1997) Heart rate variability as a measure of autonomic nervous system function in anorexia nervosa. Clin Cardiol 20(3):219–224. doi:10.1002/clc.4960200307
Rechlin T, Weis M, Ott C, Blechner F, Joraschky P (1998) Alterations of autonomic cardiac control in anorexia nervosa. Biol Psychiatry 43(5):358–363. doi:10.1016/S0006-3223(97)00026-7
Casu M, Patrone V, Gianelli MV, Marchegiani A, Ragni G, Murialdo G, Polleri A (2002) Spectral analysis of R–R interval variability by short-term recording in anorexia nervosa. Eat Weight Disord 7(3):239–243. doi:10.1007/BF03327462
Galetta F, Franzoni F, Prattichizzo F, Rolla M, Santoro G, Pentimone F (2003) Heart rate variability and left ventricular diastolic function in anorexia nervosa. J Adolesc Health 32(6):416–421. doi:10.1016/S1054-139X(03)00048-X
Cong ND, Saikawa R, Ogawa R, Hara M, Takahashi N, Sakata T (2004) Reduced 24 h ambulatory blood pressure and abnormal heart rate variability in patients with dysorexia nervosa. Heart 90(5):563–564. doi:10.1136/hrt.2003.024356
Melanson EL, Donahoo WT, Krantz MJ, Poirier P, Mehler PS (2004) Resting and ambulatory heart rate variability in chronic anorexia nervosa. Amer J Cardiol 94(9):1217–1220. doi:10.1016/j.amjcard.2004.07.103
Roche F, Barthelemy JC, Garet M, Costes F, Pichot V, Duverney D, Kadem M, Millot L, Estour B (2004) Chronotropic incompetence to exercise separates low body weight from established anorexia nervosa. Clin Physiol Funct Imaging 24(5):270–275. doi:10.1111/j.1475-097X.2004.00561.x
Platisa MM, Nestorovic Z, Damjanovic S, Gal V (2006) Linear and non-linear heart rate variability measures in chronic and acute phase of anorexia nervosa. Clin Physiol Funct Imaging 26(1):54–60. doi:10.1111/j.1475-097X.2005.00653.x
Murialdo G, Casu M, Falchero M, Brugnolo A, Patrone V, Cerro PF, Ameri P, Andraghetti G, Briatore L, Copello F, Cordera R, Rodriguez G, Ferro AM (2007) Alterations in the autonomic control of heart rate variability in patients with anorexia or bulimia nervosa: correlations between sympathovagal activity, clinical features, and leptin levels. J Endocrinol Invest 30(5):356–362. doi:10.1007/BF03346310
Vigo DE, Castro MN, Dörpinghaus A, Weidema H, Cardinali DP, Siri LN et al (2008) Nonlinear analysis of heart rate variability in patients with eating disorders. World J Biol Psychiatry 9:183–189. doi:10.1080/15622970701261604
Ishizawa T, Yoshiuchi K, Takimoto Y, Yamamoto Y, Akabayashi A (2008) Heart rate and blood pressure variability and baroreflex sensitivity in patients with anorexia nervosa. Psychosom Med 70(6):695–700. doi:10.1097/PSY.0b013e31817bb090
Jacoangeli F, Mezzasalma FS, Canto G, Jacoangeli F, Colica C, de Lorenzo A, Iellamo F (2013) Baroreflex sensitivity and heart rate variability are enhanced in patients with anorexia nervosa. Int J Cardiol 162(3):263–264. doi:10.1016/j.ijcard.2012.10.073
Bomba M, Corbetta F, Gambera A, Nicosia F, Bonini L, Neri F, Tremolizzo L, Nacinovich R (2014) Heart rate variability in adolescents with functional hypothalamic amenorrhea and anorexia nervosa. Psychiatry Res 215(2):406–409. doi:10.1016/j.psychres.2013.11.012
Jarrett ME, Burr RL, Cain KC, Hertig V, Weisman P, Heitkemper MM (2003) Anxiety and depression are related to autonomic nervous system function in women with irritable bowel syndrome. Dig Dis Sci 48:386–394. doi:10.1023/A:1021904216312
Mazurak N, Enck P, Muth E, Teufel M, Zipfel S (2011) Heart rate variability as a measure of cardiac autonomic function in anorexia nervosa: a review of the literature. Eur Eating Disord Rev 19:87–99. doi:10.1002/erv.1081
Smink FR, van Hoeken D, Hoek HW (2012) Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 14(4):406–414. doi:10.1007/s11920-012-0282-y
Yilmaz T, Foster R, Hao Y (2010) Detecting vital signs with wearable wireless sensors. Sensors 10(12):10837–10862. doi:10.3390/s101210837
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18(12):1440–1463. doi:10.1016/j.echo.2005.10.005
Schiller NB, Acquatella H, Ports TA, Drew D, Goerke J, Ringertz H et al (1979) Left ventricular volume from paired biplane two-dimensional echocardiography. Circulation 60(3):547–555. doi:10.1161/01.CIR.60.3.547
Burns A, Greene BR, McGrath MJ, O’Shea TJ, Kuris B, Ayer SM, Stroiescu F, Cionca V (2010) SHIMMER™: a wireless sensor platform for noninvasive biomedical research. IEEE Sens J 10(9):1527–1534. doi:10.1109/JSEN.2010.2045498
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93(5):1043–1065. doi:10.1161/01.CIR.93.5.1043
Merri M, Farden DC, Mottley JG, Titlebaum EL (1990) Sampling frequency of the electrocardiogram for the spectral analysis of heart rate variability. IEEE Trans Biomed Eng 37(1):99–106. doi:10.1109/CIC.1988.72585
Bianchi AM, Mainardi LT, Petrucci E, Signorini MG, Mainardi M, Cerutti S (1993) Time-variant power spectrum analysis for the detection of transient episodes in HRV signal. IEEE Trans Biomed Eng 40(2):136–144. doi:10.1109/10.212067
Solar H, Fernández E, Tartarisco G, Pioggia G, Cvetković B, Kozina S, Luštrek M, Lampe J (2012) A non invasive, wearable sensor platform for multi-parametric remote monitoring in CHF patients impact analysis of solutions for chronic disease prevention and management. Lect Notes Comput Sci 7251:140–147. doi:10.1007/978-3-642-30779-9_18
Tartarisco G, Baldus G, Corda D, Raso R, Arnao A, Ferro M, Gaggioli A, Pioggia G (2012) Personal health system architecture for stress monitoring and support to clinical decisions. Comput Commun 35(11):1296–1305. doi:10.1016/j.comcom.2011.11.015
Solar H, Fernández E, Tartarisco G, Pioggia G, Cvetković B, Kozina S, Luštrek M, Lampe J (2013) A non invasive, wearable sensor platform for multi-parametric remote monitoring in CHF patients. Health Technol 3(2):99–109. doi:10.1007/978-3-642-30779-9_18
Pan J, Tompkins WJ (1985) A real-time QRS detection algorithm. IEEE Trans Biomed Eng BME 32(3):230–236. doi:10.1109/TBME.1985.325532
Yule GU (1927) On a method of investigating periodicities in disturbed series, with special reference to Wolfer’s sunspot numbers. Philos Trans Roy Soc Lond Ser A 226:267–298. doi:10.1098/rsta.1927.0007
Walker G (1931) On periodicity in series of related terms. Proc Roy Soc Lond Ser A 131:518–532. doi:10.1098/rspa.1931.0069
IBM Corp. Released (2012) IBM SPSS statistics for Windows, Version 21.0. IBM Corp, Armonk
Lesinskiene S, Barkus A, Ranceva N, Dembinskas A (2008) A meta-analysis of heart rate and QT interval alteration in anorexia nervosa. World J Biol Psychiatry 9(2):86–91. doi:10.1080/15622970701230963
Olivares JL, Vázquez M, Fleta J, Moreno LA, Pérez-González JM, Bueno M (2005) Cardiac findings in adolescents with anorexia nervosa at diagnosis and after weight restoration. Eur J Pediatr 164(6):383–386. doi:10.1007/s00431-005-1647-6
De Simone G, Scalfi L, Galderisi M, Celentano A, Di Biase G, Tammaro P, Garofalo M, Mureddu GF, de Divitiis O, Contaldo F (1994) Cardiac abnormalities in young women with anorexia nervosa. Br Heart J 71(3):287–292. doi:10.1136/hrt.71.3.287
Bai X, Li J, Zhou L, Li X (2009) Influence of the menstrual cycle on non linear properties of heart rate variability in young women. Amer J Physiol Heart Circul Physiol 297(2):H765–H774. doi:10.1152/ajpheart.01283.2008
Attia E, Roberto CA (2009) Should amenorrhea be a diagnostic criterion for anorexia nervosa? Int J Eat Disord 42(7):581–589. doi:10.1002/eat.20720
Farquharson CA, Struthers AD (2002) Increasing plasma potassium with amiloride shortens the QT interval and reduces ventricular extrasystoles but does not change endothelial function or heart rate variability in chronic heart failure. Heart 88(5):475–480. doi:10.1136/heart.88.5.475
Yoshida NM, Yoshiuchi K, Kumano H, Sasaki T, Kuboki T (2006) Changes in heart rate with refeeding in anorexia nervosa: a pilot study. J Psychosom Res 61(4):571–575. doi:10.1016/j.jpsychores.2006.02.009
Theorell T, Kjellberg J, Palmblad J (1978) Electrocardiographic changes during total energy deprivation (fasting). Acta Med Scand 203(1–2):13–19. doi:10.1111/j.0954-6820.1978.tb14824.x
Conflict of interest
The authors of this manuscript certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Billeci, L., Tartarisco, G., Brunori, E. et al. The role of wearable sensors and wireless technologies for the assessment of heart rate variability in anorexia nervosa. Eat Weight Disord 20, 23–31 (2015). https://doi.org/10.1007/s40519-014-0135-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-014-0135-2