Opinion Statement
Health care-associated infections can affect up to a third of all patients in low- and middle-income countries and represent a serious financial burden. Nevertheless, their control by means of hand hygiene faces various obstacles in this context such as the lack of adequately chlorinated water supplies, poor access to alcohol-based hand rub, lack of proper regulations and guidelines, and the scarcity of data on the impact of the hand hygiene programs on health care-associated infections in this setting. Notwithstanding the foregoing, there have been numerous efforts to implement strategies to improve hand hygiene. Outstanding among these is the World Health Organization strategies, which have been successfully implemented taking into account local context and resources. In addition to the WHO strategy is that of the International Nosocomial Infection Control Consortium (INICC) which implies hand hygiene guidelines for implementation exclusively in low- and middle-income countries. Moreover, various hospitals and health care facilities have developed their own multimodal strategies by using available resources with considerable success. There have been multiple efforts to implement hand hygiene programs around the world taking into account international strategies, while adapting them to local circumstances. This paper reviews these efforts to face the threat posed by HCAI in low- and middle-income countries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Even though there is ample evidence (IA) that hand hygiene contributes to the reduction in HCAI and has proven to be cost-effective, the percentages of adherence to the procedure in places where resources are scarce have been shown to be in many instances low, less than 50% in many instances which is lower than the reported in high-income countries [1,2,3,4], and even less than 10% in some cases [5]. In low- and middle-income countries where the burden of HCAI seems to be greater, affecting up to two out of ten admitted patients [4], the lack of resources, together with poor administration and the lack of data on HCAI and on the cost-effectiveness regarding their prevention, make hand hygiene improvements hard to attain [6]. Even though there are reports showing that the WHO and International Nosocomial Infection Control Consortium (INICC) multimodal strategies have been successfully established, while in other instances, some countries have opted for tailoring existing strategies or creating their own to improve hand hygiene within complex environments of limited resources, given that the evidence as regard the maintenance of programs is still scarce [7].
Implementing hand hygiene programs in hospitals with limited resources
Challenges in the implementation of a hand hygiene program in facilities with limited resources
Although it is difficult to improve adherence to hand hygiene in any context, it poses an even greater challenge in low-income countries. Difficulties in some cases start with inadequate governmental regulations and the scarcity of financial resources, which lead to the lack of infrastructure for hand hygiene programs or to the existence of poorly funded ineffective programs with insufficient resources and inadequately trained staff. Frequently, the nurses on the team are not engaged full-time in infection control, since they have other duties to attend, thus, limiting these efforts [8].
Moreover, the scant information available regarding the burden that HCAI represent prevents teams from providing clear proof to others that implementation of hand hygiene programs is cost-effective. In addition, teams frequently lack the required authority to implement relevant measures [9]. Despite their contribution to morbidity and mortality, clinicians often accept HCAI as an inevitable part of clinical practice [10]. Lack of institutional programs to deal with patient safety, including hand hygiene programs, perpetuates the culture of acceptance of avoidable risks as inevitable [10]. In many instances, hospitals in low-income countries do not have adequate microbiology laboratory services, thus, hampering HCAI surveillance as well as outbreak detection and control [8, 10].
Shortfalls in staff and hospital overcrowding are two of the major barriers to the implementation of infection control measures, including hand hygiene programs [6, 8]. Insufficient training and adequate infrastructure (safe water, wash basins, soap, disposable towels, and alcohol-based hand rub at the point of care) as well as shortages in the number of nurses and physicians all contribute to diminished adherence to hand hygiene [11, 12]. For example, Alp et al. report that in Turkey, there is one nurse for three to five patients in intensive care, while in Holland, the ratio is 1:1 [13]. Furthermore, mistaken perceptions among health care workers in regard to hand hygiene practice have been detected, such as the belief that it is only required when the patient has an infectious disease and not as a matter of routine [11].
Hand hygiene using alcohol-based hand rub (ABHR) has proven to be faster and more effective than washing with soap and water, thus, reducing the time taken by health care staff in this effort and fostering adherence [14,15,16]. Nevertheless, ABHR is difficult to obtain or unaffordable in some low-income countries [17], and therefore, WHO developed two formulas to be used in the local production of ABHR which have proven to be easy to produce at low cost, as well as acceptable for and well-tolerated in many institutions [18]. An additional barrier in this regard are the health care workers’ beliefs and attitudes, since a preference has been reported for hand washing over ABHR rubbing in countries with limited resources [13, 19].
Notwithstanding the scarcity of funding, resources are frequently misused in unnecessary practices such as culturing environmental samples or routinely using disposable shoe covers or gowns for visiting family members [8]. It is therefore necessary to prioritize the allocation of resources to the most effective infection control measures, starting with the availability of safe water and an adequate hand hygiene program.
Costs and cost-effectiveness
Financial assessments are of great use in enabling decision makers to support an intervention, in particular, in circumstances where human and financial resources may be limited. Such assessments facilitate decision-making throughout the system, while maintaining the patient at the center and taking into account human, administrative, and financial resources. The cost-benefit ratio in the implementation of hand hygiene programs has been found to vary between 5.08 and 23, according to various authors in high-income settings [20, 21]. Nevertheless, the information regarding sites in low- and middle-income countries is very scarce. In Vietnam, financial assessment was conducted only for intensive care units [22], by means of a quasi-experimental study before and after the introduction of a program to improve compliance to hand hygiene, which resulted in an increase from 25 to 57% in hand hygiene adherence. The HCAI rate fell from 31.7 to 20.3% as a result of this intervention, which represents a 36% decrease in HCAI. The number of prevented health care-associated infections was 11.4/100 patients, and the program was considered to be cost-saving ($1074 USD saved for each HCAI prevented). Luangasanatip analyzed the cost of a hand hygiene intervention at a middle-income site using a mathematical model that took into consideration the costs associated with MRSA as well as the years lost for disability or death arising from a HCAI. He found that the hand hygiene intervention was cost-effective provided an increase greater than 20% in compliance was attained, and was always cost-effective if the baseline adherence to hand hygiene had been less than 20% [23].
International strategies
Implementation of the WHO multimodal strategy at sites of limited resources
WHO implemented the Multimodal Hand Hygiene Improvement Strategy in 2009, which consists of five central components that involve system change that guarantees continuous access to a safe water supply, soap, towels, and readily accessible alcohol-based hand rub at the point of care, regular education of health care workers, evaluation and feedback, reminders in the workplace, and institutional safety climate (http://www.who.int/gpsc/5may/Guide_to_Implementation.pdf). As of February 2017, more than 19,000 hospitals and health care facilities in 177 countries or areas have registered their commitment to hand hygiene as part of the global campaign—SAVE LIVES: Clean Your Hands. The strategy has facilitated the implementation of hand hygiene programs and campaigns at low-income sites [24]. Nineteen out of 29 countries stated that the signing of the proposed commitment to ensure the engagement of health ministries in facing the challenge that HCAI poses acted as a catalyst in the initiation of activities involving hand hygiene improvement in their countries. Nevertheless, the authors pointed that there were many important barriers for the implementation mainly related with giving priority to hand hygiene strategies and having all the required resources needed for hand hygiene. [24].
In low- and middle-income countries, the implementation of the WHO Multimodal Strategy has required the involvement of local and state health authorities in formalizing the commitment, the preparation of an action plan to ensure infrastructure organization, the creation of a committee that includes the heads of health care institutions and the wards where the programs are to be implemented, the infection control experienced staff that is familiar with WHO hand hygiene principles and methods, and the education of health care workers regarding pathogen transmission by hands, hand hygiene principles, and best practices based on WHO methods. Several stages 3 to 6 months in length have been required: (1) ensuring the availability of alcohol-based hand rub at point of care, which can be locally produced; (2) baseline assessment of hand hygiene adherence and of knowledge; (3) campaign launching, education of health care workers; and (4) feedback. In addition, consideration has been given at all times to habits, culture, and available resources, and this helped to show the flexibility and adaptability of the WHO Multimodal Hand Hygiene Improvement Strategy [25, 26].
Up until 2013, 42 campaigns at national and subnational levels had been registered in the WHO CleanHandsNet, a network of leaders created to support the WHO Clean Care is Safer Care initiative; out of these, 15 (35.7%) were in low- and middle-income countries where promoting a change in the system probably faces greater limitations, particularly as regard budgetary concerns [26]. In the case of these countries, the support of WHO authorities during the implementation of the program must be taken into consideration. It has been reported that hand hygiene is not seen as a priority by authorities of hospitals from middle- and low-income countries [27] therefore is possible than the results of the campaigns may not have been the same without the external support. In addition, it is remarkable that the effect of the program has been greater in high-income countries than in low- and middle-income countries [26].
Implementation of the INICC multidimensional hand hygiene strategy
In 1998, the INICC was created with the aim to prevent and exercise surveillance on health care-associated infections in low- and middle-income countries, which represent 70% of the countries in the world and more than 75% of the world population [28].
The INICC reports about hand hygiene assessed the impact of the multidimensional approach to hand hygiene established by the INICC that includes (i) administrative support, (ii) supply availability, (iii) education and training, (iv) workplace reminders, (v) process surveillance, and (vi) feedback [29]. The impact of the INICC multidimensional approach has been assessed in several reports [29,30,31,32,33,34]. One of the largest, a 13-year-long study conducted in 19 developing countries, was published in 2013. The study established that baseline hand hygiene compliance by health care workers was 48.3%, being higher among nurses than doctors. Compliance increased after INICC interventions up to 71.4% after the implementation of the multidimensional strategy, while health care-associated infections diminished between 30 and 50%. The Mexican experience of the multimodal strategy was described in an observational, prospective study conducted from June 2002 to April 2006 at eight intensive care units in three cities in Mexico. The study reported 13,201 hand hygiene opportunities, and after the six components of the strategy had been implemented, in particular after administrative support and the available resources had been obtained, hand hygiene adherence in ICUs increased from 45 to 79% [30].
In Brazil, the impact of the strategy was assessed at four intensive care units in the course of 2 years. An increase in hand hygiene compliance from 27 to 58% for 4387 opportunities was observed, and as in the study mentioned above, improved adherence to hand hygiene was associated with administrative support and supply availability [31].
In the case of Argentina, the impact of the multidimensional program was assessed in the course of 9 years at 11 intensive care units. A total of 21,100 hand hygiene opportunities were reported. Hand hygiene compliance increased from a baseline of 28.3 to 65.7% after the intervention. In addition, the variables associated with poor hand hygiene were analyzed, finding that compliance was lower among males than females (56.8 vs 66.4%; P < .001) and among physicians than nurses (46.6 vs 67.8%; P < .001). Out of the six components of the multimodal approach, administrative support was reported in only 85.7% of the intensive care units, while the remaining components were present in 100% of the participating units [2].
The effectiveness of the program was likewise assessed in Colombia in the course of 7 years at ten intensive care units, involving the six components described above. A total of 13,187 opportunities were recorded, and an increase in compliance was observed from 50 to 77% [32].
Despite the large effort in recompilation and analyzing the large numbers reported by INICC, these results should be taken cautiously due to some factors shared by the abovementioned studies. One of them is that the studies addressed only hand hygiene before patient contact and before an aseptic task, thus, missing three of the five moments for hand hygiene developed by the WHO [29,30,31,32,33,34]. Therefore, the impact of the program on hand hygiene after touching the patient and his surroundings and after body fluid exposure is not known. In addition, the participant units in some reports exhibited important loss of follow-up, sometimes more than 50% [29, 31, 33]. It is not addressed in the publications if the missed units were similar than the others in any terms, or the causes of this loss [29,30,31,32,33,34]. This missed units could imply bias, also, if one is interested in implementing the INICC multimodal strategy, it might be helpful to know about the difficulties related with these losses. Lastly, the main focus in those studies are the intensive care units and not the other hospitalization areas, being that the generalizability of the results to a whole hospital areas which are very different in a matter of kind of patients and many times in allocation of resources could be barely possible [29,30,31,32,33,34].
To summarize, the studies conducted have shown the effectiveness of the implementation of the INICC hand hygiene multidimensional program, whereby hand hygiene adherence rates greater than 70% have been reached, thus, showing that even in developing countries high compliance can be obtained. But it is important to take this studies with caution about the strategies needed to address and attain an improvement in hand hygiene compliance, since only two of the five moments for hand hygiene proposed by the WHO were evaluated, and long-term follow-up was carried out only for a subset of the participating units.
Using available resources
Currently, there are several examples of strategies implemented to increase hand hygiene compliance in limited resources countries. In this section, we review some of the main strategies that have attained success and describe the barriers encountered, including the scarcity of human and financial resources. [1, 3, 35],
Hand hygiene observation
Obtaining valid and reliable data that allow for accurate analysis and decision is of paramount importance in approaching challenges in HCAI prevention. Therefore, having the most accurate hand hygiene observation data is of upmost importance in order to proceed with any strategy to improve hand hygiene. In order to accomplish this, observers have to be trained and, ideally, validated. This training and validation take time and extra resources; therefore, in low- and middle-income countries where insufficient staffing and low nurse-patient ratio are frequent problems [36], having staff dedicated to hand hygiene observation may be very difficult to achieve [1, 6]. Even in cases where such observation is possible, in many instances, the professional conducting the research has to serve as the hand hygiene observer with the concomitant risk of producing the so called “Hawthorne effect” and incurring in observer bias by not having an external, undercover, and neutral observer [1] which would be preferable [35]. This notwithstanding, some authors have analyzed how to use “free” staff for performing hand hygiene observation. Almaguer Leyva et al. reported that medical students could be efficient hand hygiene observers without incurring in extra resource expenditure [37]. Stevenson et al. recruited observers at low-income rural hospitals and trained them by using videos showing various hand hygiene scenarios [38]. At our institution, a pediatric referral teaching hospital, we have been aided by nurse interns, and in addition, we have trained administrative staff using WHO educational materials, which has enabled us to generate validated observers without incurring in additional costs.
The use of video-monitoring for observation purposes in hemodialysis areas has been reported in Mexico [39]. In this case, the surveillance cameras in the area were used for this purpose (verbal communication with the authors). They found a lower hand hygiene adherence when using video-monitoring compared to direct observation (p < 0.05) [39].
Finally, a last option used to assess hand hygiene compliance is the measurement of alcohol-based hand rub consumption before and after program implementation [40], an indirect parameter of hand hygiene adherence. Although this method might have several biases and is the least accurate, it can be a helpful option for settings where direct observation cannot be carried out [36].
Water, soap, and alcohol-based hand rub availability
Access to safe drinking water has increased worldwide in the past several decades. Currently, more than 91% of the world’s population use improved drinking water sources according to the WHO report [41]. Even though this is encouraging for the implementation of hand hygiene programs in limited resource settings, the fact that one in three persons worldwide do not have adequate access to sanitation has to be taken into account. Without sanitation facilities, hands can be grossly contaminated, which may compromise the effectiveness of alcohol-based hand rubbing, and there is a theoretic possibility that neglected tropical diseases (such as soil transmitted helminths and schistosomiasis) associated with poor sanitation could infect patients even in the hospital setting.
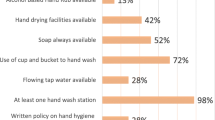
In some hospitals with adequate water supply, the access to soap and alcohol rub differ between health care workers and patients, and the use of soap and water could be more prevalent than that of alcohol-based hand rub. In a study conducted in Bangladesh involving 875 facilities, Horng et al. found that washbasin and soap availability prevailed over that of alcohol-based hand rub, and that access to hand hygiene products differed between healthcare workers and family caregivers. Soap was available at 78 to 92% of the washbasin stations for health care workers, while availability ranged from 4 to 35% at washing stations for family members. Alcohol sanitizer was available at 32–39% of hand washing locations for doctors, 39–51% for nurses, but only 0–1% for patients or family caregivers. In addition, bar soaps or powder/detergent, which can be easily contaminated were available more often that liquid soap [12].
Production and availability of alcohol-based hand rubs
Even though alcohol-based hand rubs may replace washbasins at sites where the installation of the latter may not be feasible or practical due to infrastructure or cost concerns [10], the cost at which these are sold by their manufacturing companies may be very high. Therefore, numerous low- and middle-income countries have opted to locally produce their own alcohol-based hand rubs with good results as regard costs (considerable less than those produced by the industry), tolerance, and acceptability. In addition, they can be produced from local alcohol sources such as sugar cane, corn, manioc, mahogany, or walnut [18]. Nevertheless, several difficulties in their production need to be overcome, such as insufficient properly trained workers (25% were neither pharmacists or technicians), finding adequate dispensers and reusing them, as well as the lack of quality controls, which in many instances were non-existent [18].
Alcohol-based hand rubs must be readily available, be if possible conspicuous in appearance, and placed prominently at the patient’s bedside [1]. They should also be placed outside of the patient’s hospital room or ward [35]. Individual dispensers should also be available. It should be pointed out that hand rub availability has not been described as being in itself a strategy to improve hand hygiene adherence but rather that it must be part of a multimodal program [1, 35, 38, 42].
Reminders
The use of communications and reminders is essential to make a hand hygiene program work [3, 35, 43], and such communications and reminders must be changed frequently [35]. Successful hand hygiene programs have used graphical reminders tailored for each site or have used those designed by WHO that are freely available in several languages [44]. Rodriguez et al. used in addition a storyboard showing the hand hygiene measures that had been taken [3], while Mathai proposes in addition oral reminders and self-awareness questionnaires [1].
Lastly, in 2014, Egidio et al. proposed an economical reminder device which consists in a blinking red light that flashes over the alcohol-rub dispenser placed at the hospital entrance. Even though it was used in a high-income country, it would be an economical and effective strategy to be used in low-income sites, since the cost involved was $40.50 USD per device, and adherence increased from 12 to 27% [45]. The use of cups, pens, and computer wallpapers has also been recommended for reminders [35].
Education
Education is a fundamental part of every hand hygiene program [1]. In general, it has adopted the form of group educational sessions [1, 3]. No studies have been conducted on the use of online or virtual sessions or videos in the setting of low resources places [35]. Grayson suggested that working hygiene programs require that the personality profile of the health care worker be taken into account. He found that doctors seem to be more individualistic, skeptical about rules, and independent, while nurses tend to work in teams and seek to meet immediate goals [46]. Although this study was conducted in a high-income country, we have conducted educational efforts at our center per type of staff and have obtained a better response than in group sessions. We have undertaken peer education, doctors to doctors, and nurses to nurses in participative sessions. These sessions have dealt with the impact of HCAI on costs, mortality, and morbidity, using local and international data and then comparing such data taking into account hand hygiene impact. For attending physicians, who are usually the group with the lowest adherence and show poor response to hand hygiene programs [1, 47], we opted for conducting sessions by specialty with groups of 3–8 doctors, without the presence of medical interns or residents. They were educated in hand hygiene in seminars that were part of their academic training. With these measures, we were able to increase hand hygiene adherence from less than 30% to approximately 70% in both groups. In the education of patients and their family members, we have resorted to groups of volunteers, social workers, and public relations staff that have assumed this responsibility voluntarily once they have been informed on the impact such a simple act as hand hygiene has on diminishing the morbidity of health care-associated infections.
Feedback
Most of the published studies show that feedback takes place in group sessions with either those who have set up the program [38, 48], with those who are involved in implementing hand hygiene [1, 38] or else individually when an omission is detected, as reported by Mathai et al. [1] who by using this strategy as part of a multimodal program observed and increase in hand hygiene from 68 to 95%.
Feedback can also take place by handing out leaflets or visibly placing the information on hand hygiene adherence rates per area or job position [35]. This course of action can be very effective in fostering competition and improving adherence. Moreover, Marra et al. in Brazil and Tanzania proposed using the same feedback to devise strategies geared towards achieving positive results by either the implementation of the best strategy or setting an example by publicizing the results of the best service [3, 48], thus, achieving an increase from 46 to 62% in hand hygiene adherence (p < 0.001) [48]. Among the novel strategies reported in this study, the use of theatrical plays or the granting of awards (Dr. Bacteria) handed out to those who did not participate in the hand hygiene program are worthy of mention. It should be pointed out that positive deviation use did not require extra staff.
In India, Radhakrishna proposed real-time identification of hand hygiene opportunities using radiofrequency. The equipment was a novelty and proved to be successful. Nevertheless, the calculated cost was $20,000. They were of the opinion that this was a strategy to be taken into consideration at low-income sites if the equipment were to be mass produced, thus, lowering the cost [40].
In México, Sánchez Carrillo et al. used video recordings to provide confidential report feedback to the staff under observation. They were thus able to improve hand hygiene adherence by 30.6% [39]. The video recordings were also used to analyze factors relating to hand hygiene adherence or non-adherence [39]. At our center, we used feedback relating to hand hygiene adherence and to the activities undertaken under the program, and we received proposals at existing meetings held prior to hand hygiene program implementation to discuss matters relating to HCAI with department heads and surgical groups. In addition, we implemented monthly meetings with the nursing staff. We currently distribute a monthly printout showing hand hygiene adherence and HCAI trend rates to every department, and the department with best adherence is granted recognition.
Optimization of standard operating processes
Even though studies on the improvement in standard operating processes to reduce hand hygiene opportunities and recontamination have been conducted only in high-income countries, this aspect might be taken into consideration for application at sites of limited resources where overcrowding, the lack of staff, and excessive workload are common [8, 13]. Scheithauer et al. were able to improve hand hygiene from 21 to 45% by designing flow paths that focused on specific tasks such as blood culture sampling, central venous catheter management, wound dressing, and placement of urinary catheter at emergency room services, which increased hand hygiene opportunities up to 70% [21]. This same author reports a hand hygiene improvement from 30 to 62% at hemodialysis centers when the same process was applied [42]. In both, these studies individual alcohol-based hand rub dispensers were also provided.
Role of patients
Studies addressing the general participation of patients are scarce. In 2016, Ahmed et al. found that patients are reluctant to ask health care staff whether they have washed their hands. However, by educating patients on a daily basis at small sessions and reminding doctors, the authors were able to raise patient awareness, increase hand hygiene patient requests, and also observed that as a result there was an increase in adherence from 5 to 20% in a short lapse of time (10 days) [41]. We were not able to identify studies in low- and middle-income countries regarding patient participation in hand hygiene promotion. However, there are descriptions regarding the limited access patients have to water, soap, and towels to dry their hands when compared to doctors. Despite the foregoing, patient hand hygiene is better than that of doctors (an adherence of 48% for patients vs 10% for doctors), even though patients only used water to wash their hands [12].
Conclusions
Low-income sites, located mostly in low- and middle-income nations may lack information regarding HCAI, costs, hand hygiene, hospital bed overcrowding, deficient organization, and policies that can hamper the implementation of any hand hygiene program. Successful implementation at low-income sites generally requires multimodal strategies involving at least the use of reminders, education, feedback, and the use of alcohol-based hand rub, locally produced if possible, in order to economize on resources. Existing options available to improve the success of programs at sites with limited resources might be the implementation of novel strategies such as the optimization of processes, positive deviation, the use of existing staff, and persons available (students and interns) especially for observation or the use of graphic and non-graphic reminders, among others. At low-income sites, it is convenient to resort to existing hospital staff and set up pre-established sessions to foster commitment with the hand hygiene programs and useful participation. The evidence as regard the cost-effectiveness of implementing hand hygiene programs at sites of limited resources is still scarce.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mathai AS, George SE, Abraham J. Efficacy of a multimodal intervention strategy in improving hand hygiene compliance in a tertiary level intensive care unit. Indian J Crit Care Med. 2011;15(1):6–15. doi:10.4103/0972-5229.78215.
Rosenthal VD, Viegas M, Sztokhamer D, Benchetrit G, Santoro B, Lastra CE, et al. Impact of INICC multidimensional hand hygiene approach in ICUs in four cities in Argentina. J Nurs Care Qual. 2015;30(4):E17–25. doi:10.1097/NCQ.0000000000000134.
Rodriguez V, Giuffre C, Villa S, Almada G, Prasopa-Plaizier N, Gogna M, et al. A multimodal intervention to improve hand hygiene in ICUs in Buenos Aires, Argentina: a stepped wedge trial. Int J Qual Health Care. 2015;27(5):405–11. doi:10.1093/intqhc/mzv065.
White CM, Statile AM, Conway PH, Schoettker PJ, Solan LG, Unaka NI, et al. Utilizing improvement science methods to improve physician compliance with proper hand hygiene. Pediatrics. 2012;129(4):e1042–50. doi:10.1542/peds.2011-1864.
Shobowale EO, Adegunle B, Onyedibe K. An assessment of hand hygiene practices of healthcare workers of a semi-urban teaching hospital using the five moments of hand hygiene. Niger Med J. 2016;57(3):150–4. doi:10.4103/0300-1652.184058.
Clements A, Halton K, Graves N, Pettitt A, Morton A, Looke D, et al. Overcrowding and understaffing in modern health-care systems: key determinants in meticillin-resistant Staphylococcus aureus transmission. Lancet Infect Dis. 2008;8(7):427–34. doi:10.1016/S1473-3099(08)70151-8.
Vindigni SM, Riley PL, Jhung M. Systematic review: handwashing behaviour in low- to middle-income countries: outcome measures and behaviour maintenance. Tropical Med Int Health. 2011;16(4):466–77. doi:10.1111/j.1365-3156.2010.02720.x.
•• Alp E, Damani N. Healthcare-associated infections in intensive care units: epidemiology and infection control in low-to-middle income countries. J Infect Dev Ctries. 2015;9(10):1040–5. doi:10.3855/jidc.6832. Is a recent and comprehensive review of HAI epidemiology in low resources countries, it also approaches how they have faced the challenges in that context
Yuan CT, Dembry LM, Higa B, Fu M, Wang H, Bradley EH. Perceptions of hand hygiene practices in China. J Hosp Infect. 2009;71(2):157–62. doi:10.1016/j.jhin.2008.09.017.
Sarma JB, Ahmed GU. Infection control with limited resources: why and how to make it possible? Indian J Med Microbiol. 2010;28(1):11–6. doi:10.4103/0255-0857.58721.
Mearkle R, Houghton R, Bwonya D, Lindfield R. Barriers to hand hygiene in ophthalmic outpatients in Uganda: a mixed methods approach. J Ophthalmic Inflamm Infect. 2016;6(1):11. doi:10.1186/s12348-016-0077-0.
Horng LM, Unicomb L, Alam MU, Halder AK, Shoab AK, Ghosh PK, et al. Healthcare worker and family caregiver hand hygiene in Bangladeshi healthcare facilities: results from the Bangladesh National Hygiene Baseline Survey. J Hosp Infect. 2016;94(3):286–94. doi:10.1016/j.jhin.2016.08.016.
Alp E, Leblebicioglu H, Doganay M, Voss A. Infection control practice in countries with limited resources. Ann Clin Microbiol Antimicrob. 2011;10:36. doi:10.1186/1476-0711-10-36.
Pittet D. Improving adherence to hand hygiene practice: a multidisciplinary approach. Emerg Infect Dis. 2001;7(2):234–40. doi:10.3201/eid0702.700234.
Tvedt C, Bukholm G. Alcohol-based hand disinfection: a more robust hand-hygiene method in an intensive care unit. J Hosp Infect. 2005;59(3):229–34. doi:10.1016/j.jhin.2004.10.003.
Voss A, Widmer AF. No time for handwashing!? Handwashing versus alcoholic rub: can we afford 100% compliance? Infect Control Hosp Epidemiol. 1997;18(3):205–8.
Allegranzi B, Pittet D. Healthcare-associated infection in developing countries: simple solutions to meet complex challenges. Infect Control Hosp Epidemiol. 2007;28(12):1323–7. doi:10.1086/521656.
•• Bauer-Savage J, Pittet D, Kim E, Allegranzi B. Local production of WHO-recommended alcohol-based handrubs: feasibility, advantages, barriers and costs. Bull World Health Organ. 2013;91(12):963–9. doi:10.2471/BLT.12.117085. The study provides useful evidence about local production of alcohol-based handrubs and the challeges to overcome in order to succed in this
Diwan V, Gustafsson C, Rosales Klintz S, Joshi SC, Joshi R, Sharma M, et al. Understanding healthcare workers self-reported practices, knowledge and attitude about hand hygiene in a medical setting in rural India. PLoS One. 2016;11(10):e0163347. doi:10.1371/journal.pone.0163347.
Chen YC, Sheng WH, Wang JT, Chang SC, Lin HC, Tien KL, et al. Effectiveness and limitations of hand hygiene promotion on decreasing healthcare-associated infections. PLoS One. 2011;6(11):e27163. doi:10.1371/journal.pone.0027163.
Scheithauer S, Kamerseder V, Petersen P, Brokmann JC, Lopez-Gonzalez LA, Mach C, et al. Improving hand hygiene compliance in the emergency department: getting to the point. BMC Infect Dis. 2013;13:367. doi:10.1186/1471-2334-13-367.
• Thi Anh Thu L, Thi Hong Thoa V, Thi Van Trang D, Phuc Tien N, Thuy Van D, Thi Kim Anh L, et al. Cost-effectiveness of a hand hygiene program on health care-associated infections in intensive care patients at a tertiary care hospital in Vietnam. Am J Infect Control. 2015;43(12):e93–9. doi:10.1016/j.ajic.2015.08.006. The study is one of the very few papers about cost-effectiveness of hand hygiene tath take place in a low resource facility using actual data
Luangasanatip N HM, Lubell Y, Limmathurotsakul D, Srisamang P, Day N et al. Cost-effectiveness of hand hygiene promotion for MRSA blood stream infection in ICU settings. Antimicrobial Resistance and Infection Control. 2015;Suppl 1:O50.
Mathai E, Allegranzi B, Kilpatrick C, Bagheri Nejad S, Graafmans W, Pittet D. Promoting hand hygiene in healthcare through national/subnational campaigns. J Hosp Infect. 2011;77(4):294–8. doi:10.1016/j.jhin.2010.10.012.
•• Allegranzi B, Gayet-Ageron A, Damani N, Bengaly L, McLaws ML, Moro ML, et al. Global implementation of WHO's multimodal strategy for improvement of hand hygiene: a quasi-experimental study. Lancet Infect Dis. 2013;13(10):843–51. doi:10.1016/S1473-3099(13)70163-4. This study evaluates the effect of implementation of WHO's hand-hygiene strategy showing positive results in a range of indicators, including strategy feasibility and adaptability to the local context and available resources
• Allegranzi B, Sax H, Pittet D. Hand hygiene and healthcare system change within multi-modal promotion: a narrative review. J Hosp Infect. 2013;83(Suppl 1):S3–10. doi:10.1016/S0195-6701(13)60003-1. The study relates the importance of auditing the hand hygiene infrastructure to achieve system change using available resources
Caniza MA, Duenas L, Lopez B, Rodriguez A, Maron G, Hayden R, et al. A practical guide to alcohol-based hand hygiene infrastructure in a resource-poor pediatric hospital. Am J Infect Control. 2009;37(10):851–4. doi:10.1016/j.ajic.2009.05.009.
Bennett JV, Jarvis WR, Brachman PS. Bennett & Brachman's hospital infections. 5th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2007.
•• Rosenthal VD, Pawar M, Leblebicioglu H, Navoa-Ng JA, Villamil-Gomez W, Armas-Ruiz A, et al. Impact of the international nosocomial infection control Consortium (INICC) multidimensional hand hygiene approach over 13 years in 51 cities of 19 limited-resource countries from Latin America, Asia, the Middle East, and Europe. Infect Control Hosp Epidemiol. 2013;34(4):415–23. doi:10.1086/669860. This is one of the largest study of the INICC, it explores the feasibility and effectiveness of the multidimensional hand higiene approach and shows how specific programs could improve the adherence even in limited-resource countries
Miranda-Novales MG, Sobreyra-Oropeza M, Rosenthal VD, Higuera F, Armas-Ruiz A, Perez-Serrato I, et al. Impact of the international nosocomial infection control Consortium (INICC) multidimensional hand hygiene approach during 3 years in 6 hospitals in 3 Mexican cities. J Patient Saf. 2015; doi:10.1097/PTS.0000000000000210.
Medeiros EA, Grinberg G, Rosenthal VD, Bicudo Angelieri D, Buchner Ferreira I, Bauer Cechinel R, et al. Impact of the international nosocomial infection control Consortium (INICC) multidimensional hand hygiene approach in 3 cities in Brazil. Am J Infect Control. 2015;43(1):10–5. doi:10.1016/j.ajic.2014.10.001.
Barahona-Guzman N, Rodriguez-Calderon ME, Rosenthal VD, Olarte N, Villamil-Gomez W, Rojas C, et al. Impact of the international nosocomial infection control Consortium (INICC) multidimensional hand hygiene approach in three cities of Colombia. Int J Infect Dis. 2014;19:67–73. doi:10.1016/j.ijid.2013.10.021.
Chakravarthy M, Myatra SN, Rosenthal VD, Udwadia FE, Gokul BN, Divatia JV, et al. The impact of the international nosocomial infection control Consortium (INICC) multicenter, multidimensional hand hygiene approach in two cities of India. J Infect Public Health. 2015;8(2):177–86. doi:10.1016/j.jiph.2014.08.004.
Rosenthal VD, Guzman S, Safdar N. Reduction in nosocomial infection with improved hand hygiene in intensive care units of a tertiary care hospital in Argentina. Am J Infect Control. 2005;33(7):392–7. doi:10.1016/j.ajic.2004.08.009.
Yazaji EA. Hand hygiene strategies. J Community Hosp Intern Med Perspect. 2011;1(2). doi:10.3402/jchimp.v1i2.7200.
Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level. Geneva: World Health Organization; November 2016.
Almaguer-Leyva M, Mendoza-Flores L, Padilla-Orozco M, Sanchez-Hinojosa R, Espinosa-Santacruz D, Camacho-Ortiz A. Integrating medical students as covert observers in the evaluation of hand hygiene compliance. Am J Infect Control. 2014;42(8):937–9. doi:10.1016/j.ajic.2014.04.010.
•• Stevenson KB, Searle K, Curry G, Boyce JM, Harbarth S, Stoddard GJ, et al. Infection control interventions in small rural hospitals with limited resources: results of a cluster-randomized feasibility trial. Antimicrob Resist Infect Control. 2014;3(1):10. doi:10.1186/2047-2994-3-10. It is a carefully conducted study about how to implement the whole hand hygiene program with the available resources. It also provides comprehensive information about implementation of the program in this setting and is one of the few using a cluster-randomized trial methodology
Sanchez-Carrillo LA, Rodriguez-Lopez JM, Galarza-Delgado DA, Baena-Trejo L, Padilla-Orozco M, Mendoza-Flores L, et al. Enhancement of hand hygiene compliance among health care workers from a hemodialysis unit using video-monitoring feedback. Am J Infect Control. 2016;44(8):868–72. doi:10.1016/j.ajic.2016.01.040.
Radhakrishna K, Waghmare A, Ekstrand M, Raj T, Selvam S, Sreerama SM, et al. Real-time feedback for improving compliance to hand sanitization among healthcare workers in an open layout ICU using radiofrequency identification. J Med Syst. 2015;39(6):68. doi:10.1007/s10916-015-0251-1.
Ahmed Awaji M, Al-Surimi K. Promoting the role of patients in improving hand hygiene compliance amongst health care workers. BMJ Qual Improv Rep. 2016;5(1). doi:10.1136/bmjquality.u210787.w4336.
Scheithauer S, Eitner F, Mankartz J, Haefner H, Nowicki K, Floege J, et al. Improving hand hygiene compliance rates in the haemodialysis setting: more than just more hand rubs. Nephrol Dial Transplant. 2012;27(2):766–70. doi:10.1093/ndt/gfr365.
Ling ML, How KB. Impact of a hospital-wide hand hygiene promotion strategy on healthcare-associated infections. Antimicrob Resist Infect Control. 2012;1(1):13. doi:10.1186/2047-2994-1-13.
Progress on Sanitation and Drinking Water: 2015 Update and MDG Assessment. United States of America: World Health Organization; June 2015.
D'Egidio G, Patel R, Rashidi B, Mansour M, Sabri E, Milgram P. A study of the efficacy of flashing lights to increase the salience of alcohol-gel dispensers for improving hand hygiene compliance. Am J Infect Control. 2014;42(8):852–5. doi:10.1016/j.ajic.2014.04.017.
Grayson ML, Macesic N, Huang GK, Bond K, Fletcher J, Gilbert GL, et al. Use of an innovative personality-mindset profiling tool to guide culture-change strategies among different healthcare worker groups. PLoS One. 2015;10(10):e0140509. doi:10.1371/journal.pone.0140509.
van Dalen R, Gombert K, Bhattacharya S, Datta SS. Mind the mind: results of a hand-hygiene research in a state-of-the-art cancer hospital. Indian J Med Microbiol. 2013;31(3):280–2. doi:10.4103/0255-0857.115639.
Marra AR, Noritomi DT, Westheimer Cavalcante AJ, Sampaio Camargo TZ, Bortoleto RP, Durao Junior MS, et al. A multicenter study using positive deviance for improving hand hygiene compliance. Am J Infect Control. 2013;41(11):984–8. doi:10.1016/j.ajic.2013.05.013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Daniela de la Rosa-Zamboni declares that she has no conflict of interest. Dr. Almudena Laris-González declares that she has no conflict of interest. Dr. Carlos Augusto Gómez-Ponce declares that he has no conflict of interest. Dr. Rodolfo Norberto Jiménez-Juárez declares that he has no conflict of interest. Dr. Alicia Elhain de la Garza-López declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Treatment and Prevention of Hospital Infections
Rights and permissions
About this article
Cite this article
de la Rosa-Zamboni, D., Laris-González, A., Gómez-Ponce, C.A. et al. Implementing Hand Hygiene Programs in Hospitals with Limited Resources. Curr Treat Options Infect Dis 9, 129–141 (2017). https://doi.org/10.1007/s40506-017-0115-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40506-017-0115-y