Opinion statement
Deciding if a nursing home resident should receive an antimicrobial for a suspected urinary tract infection is challenging. One of the most frequently reported reasons nursing home staff suspect presence of a urinary tract infection (UTI) is change in a resident’s mental status. However, a change in mental status may be due to numerous causes, such as presence of underlying conditions like dementia, or reaction to a new medication. The evaluation for a UTI when a resident experiences change in mental status is further confounded by the high prevalence of asymptomatic bacteriuria, which leads to positive urine cultures in nursing home residents. Various organizations recommend testing and/or treating residents for UTIs only when they have presence of localizing signs and symptoms in order to reduce prescribing antimicrobials to residents with asymptomatic bacteriuria. Unnecessary antimicrobial use is contributing to the emergence of multidrug-resistant organisms and the increase in Clostridium difficile infections. Antimicrobial stewardship programs take measures to reduce inappropriate antimicrobial use including monitoring antibiotic use for residents with suspected urinary tract infections and reviewing the use of diagnostic tests as a driver for antibiotic use. Furthermore, additional methods such as educating nursing home staff on hand hygiene, urinary catheter use, and criteria for identifying signs and symptoms of a urinary tract infection along with discussing and including antimicrobial use in end-of-life goals may also aid in reducing antimicrobial use for UTIs. However, determining when a resident should be treated for a urinary tract infection is difficult, and more research is needed to help clinicians distinguish nursing home residents who have bacteriuria from the residents who have true urinary tract infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the USA, there are approximately 15,700 nursing homes that care for around 1.4 million residents each day [1]. The majority (70.2 %) of nursing home residents are at least 75 years old with 42.3 % of the residents being over 84 years [1]. Many residents have comorbidities that may contribute to acquiring urinary tract infections (UTIs) such as diabetes mellitus, cerebrovascular disease, dementia, benign prostate hyperplasia, cancer, constipation, and incontinence [2–5]. Additionally, nursing home residents are frequently hospitalized where they receive devices such as central lines, ventilators, or urinary catheters that increase their risk of acquiring bacteremia, pneumonia, and UTI. Compared to nursing home residents without devices, residents with a device are threefold more likely to acquire nursing home-associated infections [6].
Diagnosing UTIs in older adults is difficult, and challenges in diagnosis may contribute to the high rates of UTIs reported in the nursing home population. UTIs are the most commonly occurring infections in nursing home residents [7, 8]. Risk factors for UTIs in nursing home residents include urinary catheter use, female gender, older age, incontinence, poor hygiene, and cognitive dysfunction [9–11]. Alzheimer’s disease and other dementias impact almost half of nursing home residents [2]. It is estimated that up to 90 % of people with advanced dementia will reside in a nursing home, and 67 % of dementia residents will die in the nursing home [12, 13]. Suspected UTIs are the top infection among nursing home residents with dementia [14]. Diagnosing a UTI in residents with dementia is challenging since residents often cannot communicate common symptoms like urgency and pain. Urinalysis and culture are inadequate for differentiating symptomatic UTI from asymptomatic bacteriuria which frequently occurs in residents within long-term care facilities [15]. Fever response, typically considered necessary to diagnose UTI in the absence of other reported symptoms, can also be reduced in frail and older adults, making it more challenging to rely on this objective marker to help distinguish asymptomatic bacteriuria from UTI [16, 17]. Furthermore, UTIs in nursing home residents frequently contribute to emergency room visits and hospitalizations, though asymptomatic bacteriuria may also be misdiagnosed as a UTI in these settings [18].
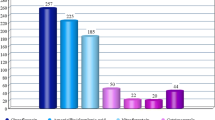
Determining when nursing home residents should receive antimicrobials for a suspected infection like a UTI can be challenging. As many as 56 % of antimicrobials used within the nursing home setting are for suspected urinary tract infections; however, a large proportion of antimicrobials may be inappropriate [19, 20••]. Before treating a UTI, nursing home residents should express signs or symptoms of infection and have a positive urine culture [16, 21, 22]. However, residents with asymptomatic bacteriuria who have a positive urine culture but no signs or symptoms of infection frequently receive antimicrobials [20••, 23]. Prescribing antimicrobials to residents who are colonized and not infected with an organism creates unnecessary risks for multidrug-resistant bacteria and Clostridium difficile infections. With the overuse and misuse of antimicrobials in the nursing home setting, antimicrobial stewardship programs will be essential in providing clarity and guidance on prescribing antimicrobials for UTIs.
Challenges with diagnosing and treating UTIs
Lack of standardized criteria for initiating treatment
Standardized criteria should be implemented throughout all nursing homes to determine when residents need to be treated for UTIs. McGeer et al. and Loeb et al. established the most recognized criteria for identifying UTIs in nursing home residents [22, 24]. However, the purpose for establishing the McGeer et al. and Loeb et al. criteria differs. The criteria from McGeer et al. along with the revisited criteria produced by Stone et al. were established to standardize surveillance definitions for UTIs, while Loeb et al. created criteria for initiating treatment in residents with UTIs [21, 22, 24]. Therefore, the criteria established by McGeer et al. and Stone et al. should not be used to determine when to treat residents for a UTI. A few guidelines and tools exist to assist with treating UTIs. Loeb et al. along with the Infectious Diseases Society of America recommend that nursing home residents be treated if they present with signs and symptoms of infection along with a positive urine culture (105 cfu/mL) [16, 22]. Crnich et al. has created an algorithm to provide guidance in determining when to prescribe antimicrobials for a UTI [25]. However, presently, no standardized methods exist and nursing home staff and physicians are conflicted regarding the appropriate time to treat a resident with a suspected UTI.
Non-specific presentation of signs and symptoms
Traditional signs and symptoms for UTIs may not always be applicable to nursing home residents. Traditional diagnostic signs and symptoms for UTIs are mentioned in Table 1 and include fever, dysuria, and gross hematuria. However, comorbidities and older age can alter the presentation of these symptoms. For example, nursing home residents may not have a fever if they have a UTI due to an insufficient immune response. Their baseline body temperature is lower on average, and an increase from baseline temperature may be seen in an infection even if it does not meet the typical threshold for fever [17]. Additionally, atypical symptoms such as lethargy and anorexia have been reported in nursing home residents with UTIs [7]. The most common sign reported for UTIs is altered mental status which includes symptoms such as “confused, more irritable, crying, aggressive, agitated, and less compliant” [26]. Also, Sundvall et al. found no correlations between UTI symptoms and bacteriuria among 651 nursing home residents [27]. The lack of specificity of these symptoms can create challenges with diagnosing UTIs.
A change in mental status can be caused by almost any acute medical problem in susceptible patients, particularly those with preexisting dementia [28]. Patients with dementia can also have difficulty communicating their symptoms, further complicating diagnosis. The most common symptoms reported for UTIs are changes in mental status or changes in behavior, especially among residents with dementia [20••, 29, 30]. D’Agata et al. examined UTI episodes among 266 residents with advanced dementia in 25 nursing homes, 72 of whom experienced suspected UTIs [20••]. A mental status change was the only symptom in 36 % of suspected UTI episodes [20••]. Furthermore, many of these residents had positive urine cultures, but only 16 % of episodes met criteria to begin antimicrobial therapy, which were based on the Loeb criteria but liberalized by including mental status changes and rigor as symptoms supporting a UTI diagnosis [20••]. Of those episodes not meeting these criteria, 74 % resulted in antimicrobial treatment [20••]. This illustrates the challenges in UTI diagnosis in cognitively impaired patients. Similarly, delirium is an acute change in cognition, attention, and awareness caused by medical problems and represents a clinically important change in mental status. It is frequently associated with UTIs among nursing home residents. However, as with other non-specific symptoms, the causal relationship is not always clear. Recently, Balogun et al. performed a systematic review to examine the relationship between delirium and UTIs in the elderly [31]. Among the five selected articles from 1988 to 2011, higher rates of UTIs were reported among patients with delirium than patients without delirium (32 vs. 13 %) [31]. However, the five studies varied on defining UTIs (ICD-9-CM codes vs. symptoms with positive urine culture), and a causal relationship could not be established due to the cross-sectional design of the studies [31].
Determining when to treat nursing home residents with dementia or delirium for suspected UTIs is challenging if the resident has difficulty communicating about more specific symptoms such as dysuria and suprapubic or flank pain. A positive urinalysis or culture in a delirious patient, or one with dementia and non-specific behavioral symptoms, may lead to an assumption that a UTI is the cause of the symptoms. This is a risk, since it may cause providers to overlook other acute medical conditions or problems contributing to the symptoms and to prescribe unnecessary antibiotics that pose additional risks to a patient that is only colonized and not infected. More research needs to be done regarding when antimicrobials should be prescribed to residents with dementia, acute mental status changes, and positive urine cultures, given the challenges in differentiating UTIs from asymptomatic bacteriuria in this population. At a minimum, it is important to also thoroughly explore other potential causes of non-specific symptoms. It may be advisable to withhold antimicrobial treatment in many patients with positive urine cultures but only non-specific symptoms, instead ensuring adequate hydration and monitoring closely for more specific or severe symptoms that may indicate an active infection.
Interpreting urinalysis and culture results
Urine culture results may be impacted if samples are not collected and processed in a timely manner. For many nursing homes, on-site laboratories are not available. Therefore, samples may need to be stored before they are transported to the contracted laboratory. Inadequate storage and transport conditions can promote growth of organisms which may produce a false-positive result. Stone et al. recommend that urine samples be processed within 1–2 h of collection, and if not processed within 30 min, be stored in a refrigerator [21].
The organisms residing in biofilms on urinary catheters may produce false-positive results for a urine culture. If biofilm on a catheter is disrupted when collecting a urine sample, organisms will be found in the sample and grow when cultured, thus producing positive urine culture results [32]. Therefore, catheters should be changed before collecting urine samples from residents with suspected UTIs [16, 33, 34].
Urinalysis and urine culture are frequently ordered for patients suspected of having a UTI. Urinalysis and urine culture should only be performed on residents with signs and/or symptoms suggesting a UTI. The Infectious Diseases Society of America recommends a urinalysis be done prior to culture collection [16]. A positive urinalysis does not indicate that a resident has a UTI, but a negative urinalysis is typically adequate to rule out infection [33, 35••, 36, 37]. Even with a positive urinalysis result and positive urine cultures, without signs or symptoms of infection, residents might be only colonized with the organism thus experiencing asymptomatic bacteriuria.
Treating suspected UTIs
Asymptomatic bacteriuria
Due to asymptomatic bacteriuria, screening nursing home residents for UTIs or collecting a culture on residents for UTIs when symptoms are absent is not recommended [33, 37]. It is estimated that 25–50 % of women and 15–40 % of men residing in nursing homes have asymptomatic bacteriuria [15, 35••, 38–40]. However, antibiotics are often prescribed for residents with bacteriuria but no clear signs and symptoms of UTI. Among patients with reported urinary tract infections, Loeb et al. found that 30 % were treated for asymptomatic bacteriuria [41]. In residents with no sign or symptoms of a UTI, cultures are sometimes collected due to pressure from nursing home staff, physicians, or resident family and during annual check-ups [26]. Collecting unnecessary urine cultures has become a huge issue within the USA. As part of the Choosing Wisely® campaign, AMDA—the Society for Post-Acute and Long-Term Care Medicine (AMDA)—recommends that urine cultures should not be obtained unless signs or symptoms are present, with a goal of reducing unnecessary antimicrobial use [42]. Similarly, the American Geriatrics Society’s Choosing Wisely® recommendations include not using antimicrobials to treat bacteriuria in older adults unless specific urinary tract symptoms are present [43]. Antimicrobial stewardship programs can monitor the prescription of antimicrobial agents to nursing home residents with asymptomatic bacteriuria which will help to prevent the occurrence of multidrug-resistant infections, C. difficile infections, and other adverse events due to antimicrobials.
Consequences of unnecessary antimicrobial use
Increased and unnecessary antimicrobial use contributes to producing multidrug-resistant organisms (MDROs). Risk factors for UTIs with a MDRO include catheter use, previous hospitalization, and prior antimicrobial use [44, 45]. Fluoroquinolones are frequently prescribed for UTIs [14, 41]. However, resistance to fluoroquinolones among isolates collected from nursing home residents was reported in 1998–2003, suggesting resistance is likely to remain a problem today [46]. The time to acquiring colonization with fluoroquinolone-resistant gram-negative bacteria was, on average, less than 3 months, which was shorter than the time of acquiring either methicillin-resistant Staphylococcus aureus (MRSA) or vancomycin-resistant Enterococcus (VRE) [47].
The nursing home is a reservoir for MDROs. Colonization with MDROs occurs frequently among nursing home residents with approximately 60 % being colonized [14, 48, 49]. Many of these residents are colonized with multidrug-resistant gram-negative bacteria (MDRGNB). Mitchell et al. reported that among dementia residents, 36.9 % were colonized with MDRGNB, which was substantially more common than MRSA (12.8 %) or VRE (0.3 %) [14]. Furthermore, O’Fallon et al. also reported higher colonization rates among residents with a MDRGNB compared with VRE or MRSA (22.8 vs. 0.6 vs. 11.1 %) [50]. Nursing home residents are also frequently hospitalized, leading to transmission to the hospital setting and the possibility for residents to bring MDROs from the hospital back to the nursing home [51, 52].
C. difficile can also be transmitted between the nursing home environment and hospital setting through nursing home residents. Colonization with C. difficile among nursing home residents ranges from 5 to 51 % [53]. Because C. difficile is highly prevalent, unnecessary antimicrobials pose significant risk. In fact, Rotjanapan et al. reported that residents who received an antimicrobial for a UTI not meeting the McGeer criteria had eightfold greater odds of developing a C. difficile infection relative to other nursing home residents [54]. Overall, 12 % of 96 residents who received antibiotics for a suspected UTI developed C. difficile infection within 3 weeks, compared to none of 76 who did not receive antibiotics [54]. Interventions pertaining to antimicrobial stewardship have been demonstrated to reduce C. difficile infections among nursing home residents [55].
The burden of adverse drug events with antibiotics is significant. Gurwitz et al. found that, behind antipsychotics, antimicrobials were the second leading drug class causing adverse drug events among a large sample of nursing home residents [56]. Rashes and C. difficile diarrhea were the most common adverse events resulting from antibiotics. Other adverse events due to antimicrobial use can include toxicities to the liver, kidneys, gastrointestinal system, or central nervous system. Furthermore, most nursing home residents receive at least six different medications, increasing the risk of adverse events related to drug interactions with antibiotic administration [57].
Strategies to improve antimicrobial use
Methods to prevent UTIs in residents
Education of nursing home staff is a key component to identifying and reducing UTIs in nursing home residents. Nursing home staff is essential in determining if a resident may have signs or symptoms of a UTI and a culture may need to be ordered. Clinicians frequently rely on the nursing home staff to report changes in residents’ status which may be an indicator of a UTI [26]. Clinicians have less contact with the residents and may not be aware of these changes. Benoit et al. reported that among 4780 nursing home residents, physicians spent on average 6 min per resident per month [58]. Nurses and nurse aides may be the primary workers to target for education since they typically represent the majority of the nursing home staff. Nurses tend to lead clinical decision-making in the nursing home and communicate with prescribers about medication requests. Nurse aides provide direct care and communicate with nurses about observed symptoms, but educating nurse aides could be challenging due to high turnover. However, education on perirectal cleaning and appropriate hand hygiene practices when handling urinary catheters could also prevent residents from acquiring an infection, and nurse aides are important targets for such education. Education on hand hygiene is important since a hand hygiene deficiency has been cited in around 9 % of nursing homes [59].
Another method to prevent UTIs is by removing unnecessary urinary catheters from nursing home residents. Between 5–22 % of residents in nursing homes have urinary catheters [6, 33, 60–64]. AMDA’s Choosing Wisely recommendations include not using an indwelling urinary catheter to manage urinary incontinence and specify that “appropriate indications for indwelling catheter placement include acute retention or outlet obstruction, to assist in healing of deep sacral or perineal wounds in patients with urinary incontinence, and to provide comfort at the end of life if needed.” [42]. Castle et al. used the nursing home Minimum Data Set to examine risk factors for UTIs and found that residents with indwelling catheters were threefold more likely to develop a UTI [9]. Additionally, the investigators identified that increased registered nurse staffing hours were associated with reduced incidence of UTIs, particularly among residents with indwelling catheters [9]. This lends support to the idea that more highly educated staff members may employ infection prevention strategies more effectively and pass those practices along to staff members, and that education of other staff on such practices may also be helpful. In a survey of 440 nursing home workers, Montoya et al. found similar results supporting the need for education [65]. Nursing home staff that were aware of the nursing home’s policies pertaining to hand hygiene during urinary catheter insertion had an increased odds of using gloves and performing hand hygiene before and after catheter insertion compared to the workers who were not familiar with the policies [65].
If a urinary catheter is required for the resident, nursing staff should be educated on using aseptic technique during catheter insertion, hand hygiene before and after catheter insertion, hydration, and storing the bag below the bladder [33]. Recently, Mody and colleagues performed a randomized controlled trial in 12 nursing homes which implemented a bundle of interventions that reduced catheter-related infections [66•]. The bundle included using gloves and gowns when caring for residents with urinary catheters or feeding tubes, performing active surveillance for MDROs, reporting back infection rates to facilities, and promoting multiple infection control practices [66•]. Additionally, Mody et al. are implementing a bundle to 500 nursing homes in 50 states to reduce catheter-associated urinary tract infections [63]. This bundle includes assessing and removing unnecessary catheters, using catheters only when needed, using aseptic technique when inserting catheters, educating staff and family on catheter care, and discussing incontinence care plans [63].
Incorporate treatment of infections within end-of-life goals
The end-of-life goals of the nursing home resident may determine if antimicrobials should be prescribed for suspected UTIs. These conversations are crucial since in the last 2 weeks of life 40 % of patients with dementia are given antimicrobials [67]. Additionally, using the Resident Assessment Instrument within the Minimum Data Set, Estabrooks et al. reported that symptoms of a UTI were reported for 9 to 10 % of the residents within the last quarter of life [68]. The primary goal for the majority of residents with advanced dementia is comfort [14]. Information is limited regarding whether antimicrobials provide comfort for these residents, and infections are very common, in part due to immune dysfunction. Furthermore, studies examining this issue are difficult to perform since it is challenging to measure comfort in residents with dementia [69]. In the CASCADE study, patients with pneumonia who were given antibiotics lived longer but had more discomfort [70]. Patients who were prescribed antimicrobials lived on average 273 days longer than patients who did not receive treatment [70]. However, the Symptom Management at End-Of-Life in Dementia scale scores were worse for patients who received antimicrobials than those who were untreated [70]. An advance directive that aligns with the resident’s wishes may include preferences for administration of antibiotics that could prolong life [69]. Having end-of-life conversations when residents enter nursing homes will be even more critical with the projected increase in the number of people who will develop Alzheimer’s disease [71].
Many residents with dementia require healthcare proxies and goals regarding the treatment of potential infections is often not discussed with residents or the healthcare proxies [72]. Nursing home residents frequently have advanced directives pertaining to hospitalizations or resuscitation. However, not all healthcare proxies are educated or aware of antimicrobial use or infections among residents [14, 73•]. Mitchell et al. examined infection management among nursing home residents with dementia using data from the Study of Pathogen Resistance and Exposure to Antimicrobial in Dementia (SPREAD) project [14]. This study found that 88 % of the nursing home residents had an advanced directive for not resuscitating whereas fewer residents had directives pertaining to no receipt of intravenous antimicrobials (16.9 %) or no oral, intramuscular, or intravenous antimicrobials (7.5 %) [14]. Only 32.9 % of proxies were counseled on infections in dementia residents and 37.8 % on antimicrobial use [14]. Furthermore, in the SPREAD study, Givens et al. reported that proxies were aware that the resident had an infection in only 39.5 % (156/395) of episodes even though a conversation was documented in the chart for 52.4 % of these episodes [73•]. Also, among the documented conversations, the majority of discussions occurred between the proxy and a nurse (56.0 %) [73•]. Therefore, infections among residents are not being clearly communicated to healthcare proxies, and nurses may need education on handling this topic with proxies.
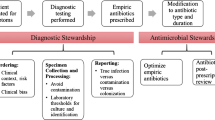
Monitoring antimicrobials use through antimicrobial stewardship programs
Antimicrobial stewardship programs within nursing homes can aid in tracking antibiotic use for UTIs. The CDC recently created “The Core Elements of Antibiotic Stewardship for Nursing Homes” to guide nursing homes in establishing a stewardship program within their facilities [74••]. An antimicrobial stewardship program within a nursing home could monitor and follow-up on residents with suspected UTIs to determine if the symptoms pertaining to the infection subside either within a couple of days or after antimicrobial treatment if such treatment is warranted. If residents still have symptoms of infection after antimicrobial treatment, then other factors should be considered such as worsened cognitive impartment due to advancing dementia or acute medical problems. Furthermore, the program could examine medications prescribed to residents with UTI symptoms to determine if symptoms may be attributed to changes in medication use or adverse effects caused by polypharmacy. In fact, it is advisable to evaluate all these other potential causes of symptoms before using an antimicrobial if the symptoms suggestive of a UTI are non-specific, such as a change in mental status.
Antimicrobial stewardship programs within nursing homes have resulted in a decrease of antimicrobial use. Zimmerman et al. implemented an educational intervention to clinicians, nursing home staff, and resident families within six nursing homes on prescribing guidelines and situations where antimicrobials are not needed [75••]. Furthermore, they provided feedback on antimicrobial use to the providers and nursing home staff each month [75••]. After initiating this intervention, Zimmerman et al. reported a significant decline in antimicrobial use for all infections including urinary tract infections (incidence rate ratio 0.86; 95 % confidence interval 0.79–0.95) [75••]. However, when examining only urinary tract infections, the intervention decreased antimicrobial use but this association was not statistically significant (incidence rate ratio 0.84; 95 % confidence interval 0.66–1.05) [75••]. Fleet et al. performed a randomized controlled study that examined an antimicrobial stewardship tool which included a “Resident Antimicrobial Management Plan” within 30 nursing homes in London [76••]. The resident management plan comprised of a form to be completed by nursing home staff at the initiation of therapy and review of the treatment 48–72 h after beginning therapy. This intervention decreased antimicrobial use by 4.9 % (P = 0.02) within 12 weeks [76••].
Conclusion
Nursing home residents are among the largest consumers of antimicrobials, and a significant proportion of these antimicrobials are utilized for suspected UTIs. Understanding when to initiate treatment for UTIs is complicated. Recommendations suggest that residents be treated with an antimicrobial only if they have both signs and symptoms of an infection and a positive urine culture. However, many nursing home residents have symptoms that could suggest a UTI but are non-specific and might instead be caused by underlying health conditions. Furthermore, many nursing home residents will present with bacteriuria if a urine culture is collected due to chronic colonization. Antimicrobial stewardship programs are needed within nursing homes to educate nursing home staff on identifying and preventing UTIs in residents and to monitor and follow-up on residents with suspected UTIs. Antimicrobial stewardship programs are essential in reducing antimicrobial use for UTIs with the nursing home setting.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Centers for Disease Control and Prevention. Long-term care services in the United States: 2013 Overview. Hyattsville, Maryland: DHHS Publication; 2013. Available at http://www.cdc.gov/nchs/data/nsltcp/long_term_care_services_2013.pdf. Accessed 31 Aug 2015.
Moore KL, Boscardin WJ, Steinman MA, Schwartz JB. Age and sex variation in prevalence of chronic medical conditions in older residents of U.S. nursing homes. J Am Geriatr Soc. 2012;60(4):756–64.
Eberle CM, Winsemius D, Garibaldi RA. Risk factors and consequences of bacteriuria in non-catheterized nursing home residents. J Gerontol. 1993;48(6):M266–71.
Powers JS, Billings FT, Behrendt D, Burger MC. Antecedent factors in urinary tract infections among nursing home patients. South Med J. 1988;81(6):734–5.
Genao L, Buhr GT. Urinary tract infections in older adults residing in long-term care facilities. Ann Longterm Care. 2012;20(4):33–8.
Tsan L, Langberg R, Davis C, Phillips Y, Pierce J, Hojlo C, et al. Nursing home-associated infections in Department of Veterans Affairs community living centers. Am J Infect Control. 2010;38(6):461–6.
Matthews SJ, Lancaster JW. Urinary tract infections in the elderly population. Am J Geriatr Pharmacother. 2011;9(5):286–309.
Nicolle LE, Strausbaugh LJ, Garibaldi RA. Infections and antibiotic resistance in nursing homes. Clin Microbiol Rev. 1996;9(1):1–17.
Castle N, Engberg JB, Wagner LM, Handler S. Resident and facility factors associated with the incidence of urinary tract infections identified in the nursing home Minimum Data Set. J Appl Gerontol. 2015.
Omli R, Skotnes LH, Romild U, Bakke A, Mykletun A, Kuhry E. Pad per day usage, urinary incontinence and urinary tract infections in nursing home residents. Age Ageing. 2010;39(5):549–54.
Rotjanapan P, Dosa D. Asymptomatic versus symptomatic urinary tract infections in long-term-care-facility residents. Med Health R I. 2009;92(11):377–9.
Smith GE, Kokmen E, O'Brien PC. Risk factors for nursing home placement in a population-based dementia cohort. J Am Geriatr Soc. 2000;48(5):519–25.
Mitchell SL, Teno JM, Miller SC, Mor V. A national study of the location of death for older persons with dementia. J Am Geriatr Soc. 2005;53(2):299–305.
Mitchell SL, Shaffer ML, Loeb MB, Givens JL, Habtemariam D, Kiely DK, et al. Infection management and multidrug-resistant organisms in nursing home residents with advanced dementia. JAMA Intern Med. 2014;174(10):1660–7.
Nicolle LE. Urinary tract infections in the elderly. Clin Geriatr Med. 2009;25(3):423–36.
High KP, Bradley SF, Gravenstein S, Mehr DR, Quagliarello VJ, Richards C, et al. Clinical practice guideline for the evaluation of fever and infection in older adult residents of long-term care facilities: 2008 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(2):149–71.
Castle SC, Norman DC, Yeh M, Miller D, Yoshikawa TT. Fever response in elderly nursing home residents: are the older truly colder? J Am Geriatr Soc. 1991;39(9):853–7.
Hsiao CJ, Hing E. Emergency department visits and resulting hospitalizations by elderly nursing home residents, 2001–2008. Res Aging. 2014;36(2):207–27.
Loeb M, Brazil K, Lohfeld L, McGeer A, Simor A, Stevenson K, et al. Optimizing antibiotics in residents of nursing homes: protocol of a randomized trial. BMC Health Serv Res. 2002;2(1):17.
D'Agata E, Loeb MB, Mitchell SL. Challenges in assessing nursing home residents with advanced dementia for suspected urinary tract infections. J Am Geriatr Soc. 2013;61(1):62–6. Antimicrobials are frequently given to nursing home residents with advanced dementia for a suspected urinary tract infection since the typical signs and symptoms of infections are not always presented in these residents.
Stone ND, Ashraf MS, Calder J, Crnich CJ, Crossley K, Drinka PJ, et al. Surveillance definitions of infections in long-term care facilities: revisiting the McGeer criteria. Infect Control Hosp Epidemiol. 2012;33(10):965–77.
Loeb M, Bentley DW, Bradley S, Crossley K, Garibaldi R, Gantz N, et al. Development of minimum criteria for the initiation of antibiotics in residents of long-term-care facilities: results of a consensus conference. Infect Control Hosp Epidemiol. 2001;22(2):120–4.
Phillips CD, Adepoju O, Stone N, Moudouni DK, Nwaiwu O, Zhao H, et al. Asymptomatic bacteriuria, antibiotic use, and suspected urinary tract infections in four nursing homes. BMC Geriatr. 2012;12:73.
McGeer A, Campbell B, Emori TG, Hierholzer WJ, Jackson MM, Nicolle LE, et al. Definitions of infection for surveillance in long-term care facilities. Am J Infect Control. 1991;19(1):1–7.
Crnich CDP. Improving the management of urinary tract infections in nursing homes: it’s time to stoop the tail from wagging the dog. Ann Long Term Care. 2014;22(9).
Walker S, McGeer A, Simor AE, Armstrong-Evans M, Loeb M. Why are antibiotics prescribed for asymptomatic bacteriuria in institutionalized elderly people? A qualitative study of physicians’ and nurses’ perceptions. CMAJ. 2000;163(3):273–7.
Sundvall PD, Ulleryd P, Gunnarsson RK. Urine culture doubtful in determining etiology of diffuse symptoms among elderly individuals: a cross-sectional study of 32 nursing homes. BMC Fam Pract. 2011;12:36.
Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157–65.
Juthani-Mehta M, Quagliarello V, Perrelli E, Towle V, Van Ness PH, Tinetti M. Clinical features to identify urinary tract infection in nursing home residents: a cohort study. J Am Geriatr Soc. 2009;57(6):963–70.
Juthani-Mehta M, Drickamer MA, Towle V, Zhang Y, Tinetti M, Quagliarello V. Nursing home practitioner survey of diagnostic criteria for urinary tract infections. J Am Geriatr Soc. 2005;53(11):1986–90.
Balogun SA, Philbrick JT. Delirium, a symptom of UTI in the elderly: fact or fable? A systematic review. Can Geriatr J. 2014;17(1):22–6.
Warren JW, Tenney JH, Hoopes JM, Muncie HL, Anthony WC. A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis. 1982;146(6):719–23.
Smith PW, Bennett G, Bradley S, Drinka P, Lautenbach E, Marx J, et al. SHEA/APIC guideline: infection prevention and control in the long-term care facility, July 2008. Infect Control Hosp Epidemiol. 2008;29(9):785–814.
Raz R, Schiller D, Nicolle LE. Chronic indwelling catheter replacement before antimicrobial therapy for symptomatic urinary tract infection. J Urol. 2000;164(4):1254–8.
Sundvall PD, Elm M, Ulleryd P, Molstad S, Rodhe N, Jonsson L, et al. Interleukin-6 concentrations in the urine and dipstick analyses were related to bacteriuria but not symptoms in the elderly: a cross sectional study of 421 nursing home residents. BMC Geriatr. 2014;14:88. Positive urine cultures and interleukin-6 were not associated with any symptoms for urinary tract infections.
Stamm WE. Measurement of pyuria and its relation to bacteriuria. Am J Med. 1983;75(1B):53–8.
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40(5):643–54.
Sundvall PD, Gunnarsson RK. Evaluation of dipstick analysis among elderly residents to detect bacteriuria: a cross-sectional study in 32 nursing homes. BMC Geriatr. 2009;9:32.
Nicolle LE. Urinary tract infections in long-term-care facilities. Infect Control Hosp Epidemiol. 2001;22(3):167–75.
Hedin K, Petersson C, Wideback K, Kahlmeter G, Molstad S. Asymptomatic bacteriuria in a population of elderly in municipal institutional care. Scand J Prim Health Care. 2002;20(3):166–8.
Loeb M, Simor AE, Landry L, Walter S, McArthur M, Duffy J, et al. Antibiotic use in Ontario facilities that provide chronic care. J Gen Intern Med. 2001;16(6):376–83.
AMDA-The Society for Post-Acute and Long Term Care Medicine. Choosing Wisely. Ten things physicians and patients should question. Available at: http://www.choosingwisely.org/wp-content/uploads/2015/02/AMDA-Choosing-Wisely-List.pdf. Accessed 31 Aug 2015.
American Geriatrics Society identifies five things that healthcare providers and patients should question. J Am Geriatr Soc. 2013;61(4):622–31.
Khawcharoenporn T, Vasoo S, Singh K. Urinary tract infections due to multidrug-resistant Enterobacteriaceae: prevalence and risk factors in a Chicago Emergency Department. Emerg Med Int. 2013;2013:258517.
Wright SW, Wrenn KD, Haynes M, Haas DW. Prevalence and risk factors for multidrug resistant uropathogens in ED patients. Am J Emerg Med. 2000;18(2):143–6.
Viray M, Linkin D, Maslow JN, Stieritz DD, Carson LS, Bilker WB, et al. Longitudinal trends in antimicrobial susceptibilities across long-term-care facilities: emergence of fluoroquinolone resistance. Infect Control Hosp Epidemiol. 2005;26(1):56–62.
Fisch J, Lansing B, Wang L, Symons K, Cherian K, McNamara S, et al. New acquisition of antibiotic-resistant organisms in skilled nursing facilities. J Clin Microbiol. 2012;50(5):1698–703.
Toubes E, Singh K, Yin D, Lyu R, Glick N, Russell L, et al. Risk factors for antibiotic-resistant infection and treatment outcomes among hospitalized patients transferred from long-term care facilities: does antimicrobial choice make a difference? Clin Infect Dis. 2003;36(6):724–30.
Trick WE, Weinstein RA, DeMarais PL, Kuehnert MJ, Tomaska W, Nathan C, et al. Colonization of skilled-care facility residents with antimicrobial-resistant pathogens. J Am Geriatr Soc. 2001;49(3):270–6.
O'Fallon E, Schreiber R, Kandel R, D'Agata EM. Multidrug-resistant gram-negative bacteria at a long-term care facility: assessment of residents, healthcare workers, and inanimate surfaces. Infect Control Hosp Epidemiol. 2009;30(12):1172–9.
Lee DC, Barlas D, Ryan JG, Ward MF, Sama AE, Farber BF. Methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci: prevalence and predictors of colonization in patients presenting to the emergency department from nursing homes. J Am Geriatr Soc. 2002;50(8):1463–5.
Mody L, Bradley SF, Strausbaugh LJ, Muder RR. Prevalence of ceftriaxone- and ceftazidime-resistant gram-negative bacteria in long-term-care facilities. Infect Control Hosp Epidemiol. 2001;22(4):193–4.
Jump RL, Donskey CJ. Clostridium difficile in the long-term care facility: prevention and management. Curr Geriatr Rep. 2015;4(1):60–9.
Rotjanapan P, Dosa D, Thomas KS. Potentially inappropriate treatment of urinary tract infections in two Rhode Island nursing homes. Arch Intern Med. 2011;171(5):438–43.
Jump RL, Olds DM, Seifi N, Kypriotakis G, Jury LA, Peron EP, et al. Effective antimicrobial stewardship in a long-term care facility through an infectious disease consultation service: keeping a LID on antibiotic use. Infect Control Hosp Epidemiol. 2012;33(12):1185–92.
Gurwitz JH, Field TS, Avorn J, McCormick D, Jain S, Eckler M, et al. Incidence and preventability of adverse drug events in nursing homes. Am J Med. 2000;109(2):87–94.
Bernabei R, Gambassi G, Lapane K, Sgadari A, Landi F, Gatsonis C, et al. Characteristics of the SAGE database: a new resource for research on outcomes in long-term care. SAGE (Systematic Assessment of Geriatric drug use via Epidemiology) Study Group. J Gerontol A Biol Sci Med Sci. 1999;54(1):M25-33
Benoit SR, Nsa W, Richards CL, Bratzler DW, Shefer AM, Steele LM, et al. Factors associated with antimicrobial use in nursing homes: a multilevel model. J Am Geriatr Soc. 2008;56(11):2039–44.
Castle N, Wagner L, Ferguson J, Handler S. Hand hygiene deficiency citations in nursing homes. J Appl Gerontol. 2014;33(1):24–50.
Warren JW, Steinberg L, Hebel JR, Tenney JH. The prevalence of urethral catheterization in Maryland nursing homes. Arch Intern Med. 1989;149(7):1535–7.
Kunin CM, Douthitt S, Dancing J, Anderson J, Moeschberger M. The association between the use of urinary catheters and morbidity and mortality among elderly patients in nursing homes. Am J Epidemiol. 1992;135(3):291–301.
Ribeiro BJ, Smith SR. Evaluation of urinary catheterization and urinary incontinence in a general nursing home population. J Am Geriatr Soc. 1985;33(7):479–82.
Mody L, Meddings J, Edson BS, McNamara SE, Trautner BW, Stone ND, et al. Enhancing resident safety by preventing healthcare-associated infection: a national initiative to reduce catheter-associated urinary tract infections in nursing homes. Clin Infect Dis. 2015;61(1):86–94.
Rogers MA, Mody L, Kaufman SR, Fries BE, McMahon Jr LF, Saint S. Use of urinary collection devices in skilled nursing facilities in five states. J Am Geriatr Soc. 2008;56(5):854–61.
Montoya A, Chen S, Galecki A, McNamara S, Lansing B, Mody L. Impact of health care worker policy awareness on hand hygiene and urinary catheter care in nursing homes: results of a self-reported survey. Am J Infect Control. 2013;41(6):e55–7.
Mody L, Krein SL, Saint S, Min LC, Montoya A, Lansing B, et al. A targeted infection prevention intervention in nursing home residents with indwelling devices: a randomized clinical trial. JAMA Intern Med. 2015;175(5):714–23. A bundle that included using gloves and gowns when caring for residents with urinary catheters or feeding tubes, performing active surveillance for multidrug resistance organisms, reporting back infection rates to facilities, and promoting multiple infection control practices can reduce catheter-associated urinary tract infection rates within nursing homes.
D'Agata E, Mitchell SL. Patterns of antimicrobial use among nursing home residents with advanced dementia. Arch Intern Med. 2008;168(4):357–62.
Estabrooks CA, Hoben M, Poss JW, Chamberlain SA, Thompson GN, Silvius JL, et al. Dying in a nursing home: treatable symptom burden and its link to modifiable features of work context. J Am Med Dir Assoc. 2015;16(6):515–20.
Mitchell SL. CLINICAL PRACTICE. Advanced Dementia. N Engl J Med. 2015;372(26):2533–40.
Givens JL, Jones RN, Shaffer ML, Kiely DK, Mitchell SL. Survival and comfort after treatment of pneumonia in advanced dementia. Arch Intern Med. 2010;170(13):1102–7.
Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80(19):1778–83.
Givens JL, Kiely DK, Carey K, Mitchell SL. Healthcare proxies of nursing home residents with advanced dementia: decisions they confront and their satisfaction with decision-making. J Am Geriatr Soc. 2009;57(7):1149–55.
Givens JL, Spinella S, Ankuda CK, D'Agata E, Shaffer ML, Habtemariam D, et al. Healthcare proxy awareness of suspected infections in nursing home residents with advanced dementia. J Am Geriatr Soc. 2015;63(6):1084–90. Healthcare proxies for nursing home residents with advanced dementia are not usually aware when the resident has an infection and are not frequently involved with decisions regarding treatment.
Centers for Disease Control and Prevention. The core elements of antibiotic stewardship for nursing homes. 2015. Available at http://www.cdc.gov/longtermcare/prevention/antibiotic-stewardship.html. Accessed 21 Sept 2015. Core components to include in an antimicrobial stewardship program within a nursing home.
Zimmerman S, Sloane PD, Bertrand R, Olsho LE, Beeber A, Kistler C, et al. Successfully reducing antibiotic prescribing in nursing homes. J Am Geriatr Soc. 2014;62(5):907–12. After implementing an educational bundle focusing on antibiotic prescribing given to nursing home staff, residents, and residents’ families, antibiotic prescribing declined in a nursing home.
Fleet E, Gopal Rao G, Patel B, Cookson B, Charlett A, Bowman C, et al. Impact of implementation of a novel antimicrobial stewardship tool on antibiotic use in nursing homes: a prospective cluster randomized control pilot study. J Antimicrob Chemother. 2014;69(8):2265–73. Antibiotic use in nursing homes was reduced when nurses within the nursing homes monitored residents’ antibiotic prescribing and administration through “Resident Antimicrobial Management Plans”.
Acknowledgments
We thank Dr. Nimalie Stone for providing us with her guidance and expertise on this manuscript. Dr. Carnahan is supported by a Patient-Centered Outcomes Research Institute (PCORI) program award (1131) and a Geriatric Workforce Enhancement Program award (1 U1Q HP28731-01) from the Health Resources and Services Administration. All statements in this manuscript, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee, or the Health Resources and Services Administration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ryan M. Carnahan declares that he has no conflicts of interests.
Jennifer S. McDanel reports grants from Cubist Pharmaceuticals and speaker honorarium from Biomerieux, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Additional information
This article is part of the Topical Collection on Antimicrobial Stewardship
Rights and permissions
About this article
Cite this article
McDanel, J.S., Carnahan, R.M. Antimicrobial Stewardship Strategies in Nursing Homes: Urinary Tract Infections. Curr Treat Options Infect Dis 8, 102–114 (2016). https://doi.org/10.1007/s40506-016-0077-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40506-016-0077-5