Opinion statement
Invasive aspergillosis is the cause of severe morbidity and mortality in immunocompromised patients. Given the challenges of fungal cultures, non-culture surrogates are crucial to the timely diagnosis of invasive aspergillosis (IA) to initiate expedited treatment. The Platelia™ Aspergillus EIA (Bio-Rad, Hercules, California) is a double-sandwich ELISA that detects the galactomannan (GM) of the fungal cell wall and was cleared by the FDA for use in serum and bronchoalveolar fluid (BAL) in 2003 and 2011, respectively. The population in which GM has been studied the most and has shown the greatest accuracy is that of hematologic malignancy. The optimal optical density index (ODI) cutoff to define test positivity in the serum is still a matter of debate because this value influences test performance. Using a lower ODI threshold (≥0.5 vs. ≥1 vs. ≥1.5) optimizes sensitivity at the expense of specificity and vice versa using a higher ODI threshold. One must be alert to the potential for false-positive results, particularly if a ODI cutoff of 0.5 is used in the serum. False positives can occur due to medications, i.e., piperacillin/tazobactam, though there is increasing evidence that newer formulations are less cross-reactive with GM, and false-positive results occur in the presence of other molds that cross-react with GM. As the use of mold-active antifungal prophylaxis increases, one must be aware that GM may not perform as well due to lower pre-test probability of IA and lower test sensitivity. Emerging evidence indicates that use of GM in combination with other tests, e.g., Aspergillus PCR or lateral flow device (LFD), may enhance diagnostic accuracy beyond GM alone; however, further validation of these diagnostics in combination are required before routine implementation can be recommended. BAL GM performs better than serum as it is significantly more sensitive, though the optimal ODI cutoff is also debated (≥0.5 vs. ≥1).False-positive results can be due to use of medications, as with serum GM. False negatives can occur with the use of certain agents which decrease the viscosity of the BAL fluid, and use of such agents need to be considered by the clinician when evaluating a test result. Again, BAL GM, in conjunction with other tests, e.g., PCR and LFD, are promising, but further studies are needed. GM in other fluids, i.e., CSF, urine, and tissue, may be useful, but the studies are very limited. In summary, when employed in the right clinical context and interpreted appropriately, serum and BAL GM can facilitate the diagnosis and early treatment of IA. While there are significant limitations and the landscape is evolving, the test has an important role in clinical practice today.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive aspergillosis (IA) is a severe, life-threatening fungal disease of primarily immunocompromised patients caused by Aspergillus spp. organisms. A major contributor to poor outcomes is delayed diagnosis. While a positive culture obtained from biopsy is the gold standard for diagnosing IA, this is fraught with challenges: obtaining a specimen is difficult and not without risk to the patient, sampling error can occur, and cultures are insensitive, particularly if patients are already receiving mold-active antifungal agents [1]. Therefore, new strategies involving non-culture-based tests are needed (Table 1).
The diagnosis of IA can be classified into three categories per the 2008 revised European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the Mycoses Study Group (EORTC/MSG) Consensus Group definition: (1) proven (based on histopathological evidence and a positive result of a culture from a normally sterile site), (2) probable (fulfillment of criteria within three categories: host factors, clinical features, mycological evidence), or (3) possible (fulfillment of host factors and clinical features criteria but lacking mycological evidence) [2].
Galactomannan (GM) is a polysaccharide cell wall component that is released by the organism during growth, and assays which detect galactomannan take advantage of this phenomenon. Initial GM assays, including a latex agglutination (Pastorex Aspergillus; Sanofi Diagnostics Pasteur), were found to have poorer sensitivity to subsequent assays and are no longer available.
The Platelia™ Aspergillus EIA (Bio-Rad, Hercules, California) is a “double-sandwich ELISA that incorporates the B 1–5 galactofuranose-specific EBA2 monoclonal antibody as both the detector and acceptor” for GM [1]. This assay is widely available and has been most extensively investigated in serum; it was cleared by the US Food and Drug Administraton (FDA) for use in serum since 2003. In 2008, GM detection of plasma, serum, bronchoalveolar lavage fluid (BAL), or cerebrospinal fluid (CSF) was added as an acceptable mycological criterion to the revised EORTC/MSG definition for probable IA [2]. In 2011, the FDA also cleared the Platelia™ assay for the testing of BAL. Recently, updated guidance is available which includes GM detection in serum and BAL (note: using different cutoffs for positivity than the FDA-cleared cutoffs) as mycological criteria for IA diagnosis in clinical treatment trials [3].
Herein, we will review the utility of the GM assay (specifically the Platelia™ Aspergillus EIA) stratified by the use in various diagnostic samples and patient populations, compare GM to other available and emerging tests, and offer recommendations about when and how to best implement the test in clinical practice.
Diagnosis
Serum GM
-
The primary goal of serum GM is to noninvasively diagnose invasive aspergillosis (IA). It has also been studied as a prognostic marker.
Serum GM Test Characteristics
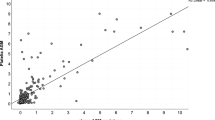
The GM test measures the absorbance (optical density; OD) of the monoclonal antibody-galactomannan-peroxidase complexes in specimens and controls determined with a spectrophotometer. The OD index (ODI) is calculated by dividing the specimen OD by a pre-specified cutoff control serum [1].
There are several contributing factors to the complexity of interpreting test accuracy. Most importantly is the ODI cutoff definition of test positivity: initially, the ODI cutoff in Europe was set at ≥1.5; however, upon review, the FDA cleared the GM for use with a positive ODI cutoff of ≥0.5. Since that time, there has been significant debate about the optimum cutoff values, as higher ODI cutoffs (e.g., ≥1 or ≥1.5) provide improved specificity at the expense of lower sensitivity. Further complicating matters, studies also have evaluated the utility of requiring two positive consecutive samples to define test positivity, a strategy that enhances test specificity. Also, the GM test appears to have different characteristics based on study population; the setting where the test has performed the best is in the hematologic malignancy patients. And finally, the gold standard diagnosis is suboptimal and reference criteria for case definitions have changed over time; one must pay close attention to the criteria employed when evaluating test performance. Currently, a reasonable and frequently used reference standard is a combined group of proven/probable IA per the 2008 revised EORTC/MSG criteria.
In a meta-analysis of 27 studies, Pfeiffer et al. found a sensitivity and specificity of serum GM for proven/probable IA of 61 and 93 %, respectively [4]. The sensitivity was higher in studies evaluating GM for only proven disease (71 %). For solid organ transplant population, the sensitivity (41 %) and specificity (85 %) appeared to be worse, although only 22 proven/probable cases in that population were reported. The ODI cutoff values impacted accuracy: for proven/probable IA, studies evaluating ODI cutoffs of ≥0.5, ≥1, and ≥1.5 showed sensitivities of 79, 65, and 48 % and specificities of 86, 94, and 95 %, respectively.
Subsequently, a Cochrane review (2008) included 30 studies with an updated dataset and methods and reported similar results, stratifying test performance by ODI cutoff for proven/probable IA as follows: as the ODI cutoff for positivity increased (≥0.5, ≥1, ≥1.5), GM sensitivity decreased (78, 75, 64 %) but GM specificity increased (81, 91, 95 %) [5]. The authors also found lower sensitivity (69, 63, and 57 % for ODI cutoffs of ≥0.5, ≥1, and ≥1.5, respectively) when the EORTC/MSG criteria were employed as a test reference. Requiring >1 positive sample to define test positivity vs. a single sample improved test specificity (95 vs. 84 % for ODI ≥1; 83 vs. 61 % for ODI ≥0.5) but sacrificed sensitivity.
The optimal cutoff is unclear, and clinicians using the test should be aware of this issue. In light of this uncertainty, the revised 2008 EORTC/MSG guidelines avoid recommending a specific ODI cutoff but defer to the manufacturer’s threshold [2]. Therefore, in the US using FDA-cleared cutoffs, an ODI threshold of 0.5 is positive; one must understand that this cutoff optimizes sensitivity.
In the aforementioned recent biomarker qualification summary review for the FDA (2014), the goal of which was to clarify the role of GM in clinical treatment trials of IA; the authors representing the MSG concluded a positive serum GM result may be used as mycological evidence based on a cutoff ODI ≥ 0.5 of two separate samples or a single sample with ODI value ≥1.0 in patients with hematologic malignancies or bone marrow transplants [3]. More stringent criteria than the FDA-cleared values were selected because the priority in the context of clinical treatment trial is to optimize test specificity (i.e., it is important to ensure patients in an aspergillosis treatment trial actually have IA).
Serum GM: Causes of False-Positive Tests
Certain known factors may contribute to false-positive results. As outlined in the FDA biomarker qualification review summary and the package insert, genera of certain molds demonstrate cross-reactivity with EB-A2 monoclonal Ab including Penicillium, Trichophyton, Blastomyces, Sporothrix, Histoplasma, Geotrichum, Alternaria, and Paecilomyces. Fortunately, these are relatively uncommonly encountered organisms in the patient population for which GM testing is typically indicated [6].
Certain medications have been associated with false-positive GM, most importantly, piperacillin/tazobactam. For example, Viscoli et al. demonstrated an increase in the serum GM positivity rate 10 % (38/386 patients) to 36 % (21/59 patients) in their center in 2003 and that increase was significantly associated with receipt piperacillin/tazobactam [7]. However, there may be a manufacturing issue rather than an inherent cross-reactivity with the piperacillin/tazobactam compound itself; in 2012, Mikulska et al. evaluated a newer formulation of piperacillin/tazobactam [8]. The rate of GM positivity in this report for patients who were and were not receiving piperacillin/tazobactam were 25/1606 (1.5 %) vs. 10/394 (2.5 %), respectively. Also in this study, 90 samples of piperacillin/tazobactam from 30 randomly selected batches tested negative for GM. Additionally, a study evaluating GM results associated with piperacillin/tazobactam use in the USA recently demonstrated a low positivity rate (0/32 lots; 1/27 serum samples in patients) [9]. While caution is prudent, it appears that with newer formulations, false positives by piperacillin/tazobactam may be less of a concern than previously thought.
Finally, gluconate-containing IV solution (e.g., Plasma-Lyte) have been shown to cross-react with the GM assay. In one report, a false-positive serum GM was obtained in a patient who had received Plasma-Lyte after bladder suspension surgery; investigators tested the product directly and those tests yielded positive results [10].
Serum GM Performance in Presence of Mold-Active Antifungal Agents
In an era of anti-mold prophylaxis (i.e., voriconazole, posaconazole) becoming increasingly common for at-risk patients, the utility of GM as a surveillance marker is being re-evaluated. Most importantly, patients receiving mold-active prophylaxis have a lower incidence of IA, leading to a lower pre-test probability and higher false-positive rate; for example, a recent report from Spain evaluated 2972 serum GM tests on at-risk patients who were receiving posaconazole prophylaxis. The patients had only a 1.9 % incidence of IA, and the positive predictive value of GM in this setting was only 12 %. However, the GM test was positive in all five true-positive cases; the authors concluded that routine GM surveillance should be reconsidered but GM can still be useful when a clinical suspicion of IA exists [11••]. Additionally, the sensitivity of GM assay may suffer in the presence of mold-active antifungal agents [12].
Serum GM Performance Compared to PCR
In the USA, no polymerase chain reaction (PCR) test has been FDA-approved as a consensus on methodology has not yet been reached, resulting in widely varying sensitivities and specificities. However, certain PCR assays are approved in Europe (CE-marked, indicating a product’s compliance with European Union legislation). Two large meta-analyses determined a sensitivity of 84–88 % and specificity of 75–76 % of PCR of the serum [13, 14]. However, not surprisingly, both meta-analyses demonstrated significant heterogeneity between studies in the number of samples used to determine positivity, use of serum vs. whole blood, primers used and the type of DNA extraction techniques utilized. In an attempt to standardize methodology, the European Aspergillus PCR Initiative (EAPCRI) was launched to give specific recommendations on DNA extraction and amplification techniques [15, 16].
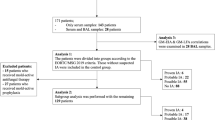
In a recently published, open-label, controlled trial in multiple Spanish hospitals, 219 hematologic malignancy patients undergoing either induction therapy or stem cell transplant were randomized to twice weekly monitoring with either GM or GM plus PCR [17••]. No patients received mold-active prophylaxis. PCR was developed within EAPCRI guidelines; positivity of GM was defined as two samples with ODI ≥0.5 or a single sample with ODI ≥0.7. Positivity of either assay prompted imaging and antifungal therapy. For the GM-PCR group, more cases of possible IA and fewer cases of probable/proven IA were diagnosed, the time to diagnosis of proven/probable IA was less (13 vs. 20 days), less empiric antifungal therapy was used (17 vs. 29 %), and a probable/proven IA-free survival advantage was shown (p = 0.027). Interestingly, GM was positive in four cases of PCR-negative probable/proven disease. Overall, authors concluded that both tests were complementary and PCR potentially moved up the diagnosis from probable/proven to possible before angioinvasion occurred.
More studies will be needed to validate and determine the best clinical use of PCR in the serum, whether it be in combination with or in place of GM.
Serum GM Compared to Aspergillus Lateral Flow Device
The Aspergillus lateral flow device (LFD) is a rapid, point-of-care test that was CE-marked for use in Europe in 2013; it is not (at this time) cleared for use in the USA [18]. The LFD “uses a mouse monoclonal antibody, known as JF5, to detect a glycoprotein antigen found the serum and BAL of patients with IA.” [19] While more BAL data are available (discussed below), in the largest initial study of the test in serum published in 2013, 103 adult hematology patients at risk for IA (22 diagnosed with proven/probable IA) were retrospectively analyzed in a case-control study. In this setting, the LFD performed similarly to GM (ODI threshold ≥0.5) and had a sensitivity of 81.8 % and specificity of 98 % [20]. The Aspergillus LFD has the distinct advantages of (a) ease-of-use, not requiring any technical expertise and (b) quick turn-around time for results (<15 min). More clinical data and FDA clearance will be necessary before implementation occurs in the USA.
Serum GM Compared to 1,3-β-D-glucan
1,3-β-D-glucan (BG) is a component of the cell wall of many different fungi including Aspergillus spp., and the ability of BG to activate an enzyme in the clotting cascade of the horseshoe crab led to the development the assay. Four tests have been commercialized, and each uses individualized cutoff values to define positivity; assays include Fungitell, which is the only FDA-cleared test (“Associates of Cape Cod, East Falmouth, MA), Fungitec-G (Seikagaku, Tokyo, Japan), Wako turbidimetric assay (Wako Pure Chemical Industries, Tokyo, Japan), and Maruha colorimetric assay (Maruha-Nichiro Foods, Tokyo, Japan”) [21]. Because it is pan-fungal, BG has been evaluated in studies focused not only on hematologic malignancy patients, often in conjunction with GM aimed at the detection of molds (and yeasts), but also high-risk intensive care unit patients aimed at detection of Candida and patients at risk for Pneumocystis jirovecii pneumonia (PCP). In a systematic review of six cohort studies limited to high-risk hematologic malignancy patients, the sensitivity of BG was 62 % and the specificity was 91 % [21]. Using a strategy similar to GM, the diagnostic performance of requiring two consecutive positive samples for test positivity was evaluated; the reported sensitivity was 50 % and specificity 99 %. Importantly, unlike GM (and PCR), the BG is pan-fungal and does not distinguish amongst fungi. BG is not found on certain fungi (biologic false negative results with Cryptococcus and agents of mucormycosis), and false positive has been reported with hemodialysis, surgery, amoxicillin-clavulanic acid, bacteremia, and immunoglobulin or albumin product administration [22–29].
Serum GM as a Prognostic Marker
Emerging data indicate that serum GM may also serve as a prognostic marker. Several studies have now demonstrated that both a higher initial serum GM and that the rate of GM decay are associated with worse treatment outcome [30–33]. A recent report indicated that different antifungal agents have disparate impact on the rate of GM decay [34]. However, at this time, firm recommendations on prognosis based on GM ODI would be premature as more clinical data are needed.
Galactomannan on Bronchoalveolar Lavage Fluid
-
The primary goal for GM of the BAL is to support a diagnosis of invasive aspergillosis (IA) and obviate the need for histopathology.
BAL GM Test Characteristics
The measurement of BAL GM has also been extensively evaluated for the diagnosis of pulmonary IA, and the test is more sensitive than serum GM. The FDA-cleared GM for use on BAL in 2011 after review of data which included an ODI cutoff of ≥0.5 [35]. However, as has been debated with serum, the optimal ODI cutoff value is still uncertain and discussed below.
GM in BAL faces the same challenges as in the serum with false positives (e.g., prior use of piperacillin/tazobactam and cross-reactivity with certain fungal species). False negative test results have recently been reported as a result of BAL sample pretreatment with the anti-viscosity agent Sputasol® (Oxoid Microbiological Products) [36]. BAL GM can also be falsely negative if less fluid than the recommended amount is tested (technical issue) or with antifungal administration (biologic negative).
In 2010, Guo et al. published a bivariate meta-analysis and systemic review of 13 studies and found an overall sensitivity and specificity of BAL GM of 90 and 94 %, respectively, when using cutoffs provided by the study authors [37]. When analyzed by OD index threshold (0.5 vs. 0.1), the sensitivity was similar (86 vs. 85 %) but specificity was enhanced (89 vs. 94 %). Subsequently, a meta-analysis of 30 studies evaluated BAL GM was published by Zou et al. in 2012 [38]. The sensitivity, specificity, and diagnostic odds ratios for proven/probable IA were 86, 95 %, and 113, respectively, when using an OD index value ≥1 and 87, 89 %, and 53 if using a cutoff of ≥0.5; the authors concluded that optimal test performance (i.e., best diagnostic odds ratio) is achieved using a cutoff of ≥1.
The utility of GM may be best analyzed on a continuum. D’Haese et al. analyzed BAL GM retrospectively on 251 consecutive at-risk patients and found the optimal GM cutoff to for proven/probable diagnosis of IA was ≥0.8, which corresponded to an 86 and 91 % sensitivity and specificity, respectively [39]. However, the specificity of the test was 100 % if one used a cutoff of 3 and test sensitivity was 93 % if the cutoff was set at ≥0.5.
The accuracy of BAL GM does not appear to be impacted as much as the serum test by the type of host or underlying disease, although most data in the largest meta-analysis came from patients with hematologic malignancy [35, 38].
BAL GM Compared to PCR
PCR on BAL has been available for over 20 years but has struggled to find a place in clinical practice, primarily due to a lack of standardization with investigators unable to agree on a methodology and interpretation. Two meta-analyses published in 2011 and 2012 (highly overlapping datasets) found BAL PCR had a pooled sensitivity and specificity of 91 and 90 % with a specificity of 92 and 96 %, respectively [40, 41]. Avni et al. performed a subset analysis of the nine cohort studies which used EORTC/MSG diagnostic reference standard and found a reduced sensitivity of 77 % [40]. In this meta-analysis, PCR was also compared to BAL GM and found to have a modestly higher sensitivity (4–7 % depending on OD index cutoff used).
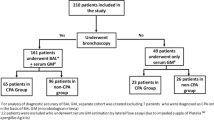
Using BAL GM and PCR together to optimize the diagnosis of IA is another possible approach. However, the following well-conceived study did not show an obvious benefit of employing both tests. Heng et al. evaluated 116 patients with hematologic malignancies (68 % of who had received mold-active antifungal agents) at three Australian centers who underwent BAL for investigation of new lung infiltrates [42]. Without including the GM or PCR results, 3, 15, and 50 patients were diagnosed with proven, probable, and possible IA, respectively. BAL GM and PCR upgraded seven probable cases based on positive microscopy would have been confirmed as Aspergillus infections and 24 possible IA cases would have been upgraded to probable. The optimal cutoff value of BAL GM in this study was found to be 0.8; using that cutoff, sensitivity for proven/probable disease was 61 % and specificity was 93 %. In contrast, BAL PCR sensitivity and specificity were 78 and 79 %, respectively. The lower sensitivity of BAL GM in this report as compared to prior studies may have been due to the high number of patients receiving mold-active antifungal agents. The authors concluded that the use of either test is helpful for IA diagnosis, each test has known strengths and weaknesses, and the benefit of combining GM plus PCR was unclear and would require investigation in a larger study.
Until commercially available and/or standardized PCR methods become available, it will be difficult to incorporate PCR in routine clinical practice.
BAL GM Compared to Aspergillus Lateral Flow Device
The Aspergillus LFD (as explained above in the GM serum portion) is a rapid, point-of-care, easy-to-use device which has been studied somewhat more in BAL as compared to serum. In a small study of 39 patients (including hematology and solid organ transplant patients), Hoenigl et al. found a sensitivity and specificity of 100 and 81 %, respectively [43]. Of the five “false-positive” cases, three had BAL GM indices >0.5 but <1, which was the cutoff chosen for the study (indicating that potentially these were true-positive cases). Another small study showed that LFD had a 91 and 83 % sensitivity and specificity, respectively, in 47 solid organ transplant patients suspected of IA [44]. Miceli et al. retrospectively tested prospectively collected BAL specimens of 96 patients at risk for IPA; 89 of whom were non-hematologic patients and only 3 of whom were diagnosed with IPA [45]. LFD and GM both detected 2/3 cases of IPA (2 probable, 1 possible); interestingly, specificity was 94 % for LFD and only 52 % for GM owing primarily to false-positive results in the lung transplant population.
The Aspergillus LFD has also been evaluated in ICU patients without underlying hematological malignancies; authors excluded solid organ transplant recipients and included patients that had been in the ICU for four or more days. Eigl et al. demonstrated a sensitivity of 80 % and specificity of 81 % in 133 patients, 18 of whom had proven/probable IA. In contrast, BAL fungal culture had a sensitivity of 50 % and specificity of 85 % [46].
A recent multi-assay comparison study evaluated BAL GM, LFD, PCR, and beta-D-glucan from 78 adult immunocompromised patients (60 % hematology patients). Three, 14, 17, and 44 patients were diagnosed using EORTC/MSG criteria with proven, probable, possible, and no IA. GM, PCR, and LFD all had sensitivities between 70–88 %, specificities >90 %, and high diagnostic odds ratios. Fungal culture and beta-D-glucan suffered from poor sensitivity and specificity, respectively. Interestingly, combining GM with either PCR or LFD appeared to enhance sensitivity without sacrificing specificity. The authors concluded that, individually, the tests are helpful but in particular, GM in combination with PCR, or if not available, LFD, provided both a sensitive and specific diagnosis of IA [47••].
Evaluation of the Aspergillus LFD alone and in combination with GM will be of great interest as we move forward towards a rapid, sensitive, and specific diagnosis of IA. Further study will better define the diagnostic role of this assay.
Galactomannan on Other Body Fluids
-
GM may be utilized on sterile body fluid other than serum and BAL fluid to diagnose IA.
Galactomannan has also been studied in off-label use in other sterile body fluids, most notably in cerebrospinal (CSF) fluid and urine.
CSF GM
Cerebral aspergillosis is not a common site for primary IA but is the most common secondary site of infection. It is detected in 10–20 % of cases of IA and it is highly fatal [48]. Diagnosis is difficult as cultures can be falsely negative due to collection bias or specimen handling techniques and other CSF fluid indicators, i.e., protein and glucose can be nonspecific [49]. Studies regarding the use of GM in CSF are limited. One study included five bone marrow transplant patients diagnosed with probable IA by EORTC/MSG criteria and 16 control patients. A statistically significant difference between the CSF GM indexes between bone marrow transplant patients and those in the control group (median CSF GM OD index 10.5 vs. 0.3) was found [50]. Also, PCR may be useful in CNS disease; in one study of eight patients with proven or probable IA, the sensitivity of CSF PCR was 100 % and the specificity was 93 % [51]. To our knowledge, no study has directly compared the performance of GM to PCR in CSF.
Of recent interest, the diagnosis of Exserohilum rostratum in the multi-state fungal meningitis outbreak was an important topic, but in initial evaluation, GM was not found to be helpful; the diagnosis relied mainly on real-time PCR assay specific for E. rostratum [52, 53].
GM in Urine
There are even fewer data on the performance of GM in urine samples [54]. As it is noninvasive to obtain a urine sample, use of GM in urine would theoretically be quite useful. GM can be detected in the urine of patient with IA, but there is little known regarding the pharmacokinetics of galactomannan and clearance by the kidney [55].
In a recent study, serum and urine GM were collected twice weekly as part of routine care from 75 patients with hematological malignancies [56]. A total of 21/242 samples from 13 patients were positive in the serum; comparing same-day urine results to the serum using an OD index cutoff of >0.1, sensitivity was 48 % and specificity was 86 %. While the sensitivity was relatively poor, this noninvasive screening tool could have some adjunctive role in the diagnosis of IA, but certainly, more study is required before adoption of this practice.
In a proof-of-concept study using a novel monoclonal antibody that recognizes GM-like antigens from Aspergillus, Dufresne et al. demonstrated antigenuria in urine samples in both guinea pigs and human subjects. Prospective clinical data would be required to optimize the test and establish performance characteristics [57].
Conclusion
IA is a serious threat to immunocompromised patients, and GM testing can be a useful adjunct for IA diagnosis. This FDA-cleared test has demonstrated moderate and high accuracy in serum and BAL, respectively. Increasing the ODI cutoff for positivity (e.g., from 0.5 to 1.5) threshold increases specificity but sacrifices sensitivity. Biologic false-positive tests occur because the test cross-reacts with certain other, much less common molds. Fortunately, it appears the issues with false-positive GM due to piperacillin/tazobactam administration may be resolved. Emerging issues which will be the subject of future study will be the utility of this test in combination with PCR-based technology or the Aspergillus LFD. Also, because anti-mold prophylaxis has become increasingly common in patients at-risk for IA, the performance of GM (and other tests) in clinical practice will be impacted and new diagnostic strategies will be required.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
http://www.bio-rad.com/webroot/web/pdf/inserts/CDG/en/62796_881045_EN.pdf. Accessed 15 June 2015.
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813–21. doi:10.1086/588660.
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM420234.pdf. Accessed 15 June 2015.
Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis. 2006;42(10):1417–27. doi:10.1086/503427.
Leeflang MM, Debets-Ossenkopp YJ, Visser CE, Scholten RJ, Hooft L, Bijlmer HA, et al. Galactomannan detection for invasive aspergillosis in immunocompromized patients. Cochrane Database Syst Rev. 2008;4, CD007394. doi:10.1002/14651858.CD007394.
Fukuda T, Boeckh M, Carter RA, Sandmaier BM, Maris MB, Maloney DG, et al. Risks and outcomes of invasive fungal infections in recipients of allogeneic hematopoietic stem cell transplants after nonmyeloablative conditioning. Blood. 2003;102(3):827–33. doi:10.1182/blood-2003-02-0456.
Viscoli C, Machetti M, Cappellano P, Bucci B, Bruzzi P, Van Lint MT, et al. False-positive galactomannan platelia Aspergillus test results for patients receiving piperacillin-tazobactam. Clin Infect Dis. 2004;38(6):913–6. doi:10.1086/382224.
Mikulska M, Furfaro E, Del Bono V, Raiola AM, Ratto S, Bacigalupo A, et al. Piperacillin/tazobactam (Tazocin) seems to be no longer responsible for false-positive results of the galactomannan assay. J Antimicrob Chemother. 2012;67(7):1746–8. doi:10.1093/jac/dks111.
Vergidis P, Razonable RR, Wheat LJ, Estes L, Caliendo AM, Baden LR, et al. Reduction in false-positive Aspergillus serum galactomannan enzyme immunoassay results associated with use of piperacillin-tazobactam in the United States. J Clin Microbiol. 2014;52(6):2199–201. doi:10.1128/JCM.00285-14.
Surmont I, Stockman W. Gluconate-containing intravenous solutions: another cause of false-positive galactomannan assay reactivity. J Clin Microbiol. 2007;45(4):1373. doi:10.1128/JCM.02373-06.
Duarte RF, Sanchez-Ortega I, Cuesta I, Arnan M, Patino B, Fernandez de Sevilla A, et al. Serum galactomannan-based early detection of invasive aspergillosis in hematology patients receiving effective antimold prophylaxis. Clin Infect Dis. 2014;59(12):1696–702. doi:10.1093/cid/ciu673. This study shows lower incidence of IA in setting of prophylaxis and calls for new roll of GM surveillance.
Marr KA, Laverdiere M, Gugel A, Leisenring W. Antifungal therapy decreases sensitivity of the Aspergillus galactomannan enzyme immunoassay. Clin Infect Dis. 2005;40(12):1762–9. doi:10.1086/429921.
Arvanitis M, Ziakas PD, Zacharioudakis IM, Zervou FN, Caliendo AM, Mylonakis E. PCR in diagnosis of invasive aspergillosis: a meta-analysis of diagnostic performance. J Clin Microbiol. 2014;52(10):3731–42. doi:10.1128/JCM.01365-14.
Mengoli C, Cruciani M, Barnes RA, Loeffler J, Donnelly JP. Use of PCR for diagnosis of invasive aspergillosis: systematic review and meta-analysis. Lancet Infect Dis. 2009;9(2):89–96. doi:10.1016/S1473-3099(09)70019-2.
White PL, Bretagne S, Klingspor L, Melchers WJ, McCulloch E, Schulz B, et al. Aspergillus PCR: one step closer to standardization. J Clin Microbiol. 2010;48(4):1231–40. doi:10.1128/JCM.01767-09.
White PL, Mengoli C, Bretagne S, Cuenca-Estrella M, Finnstrom N, Klingspor L, et al. Evaluation of Aspergillus PCR protocols for testing serum specimens. J Clin Microbiol. 2011;49(11):3842–8. doi:10.1128/JCM.05316-11.
Aguado JM, Vazquez L, Fernandez-Ruiz M, Villaescusa T, Ruiz-Camps I, Barba P, et al. Serum galactomannan versus a combination of galactomannan and polymerase chain reaction-based Aspergillus DNA detection for early therapy of invasive aspergillosis in high-risk hematological patients: a randomized controlled trial. Clin Infect Dis. 2015;60(3):405–14. doi:10.1093/cid/ciu833. This study demonstrated utility of PCR plus GM for early IA diagnosis.
http://www.olmdiagnostics.com/published-data/2/aspergillosis. Accessed 15 June 2015.
Thornton CR. Development of an immunochromatographic lateral-flow device for rapid serodiagnosis of invasive aspergillosis. Clin Vaccine Immunol CVI. 2008;15(7):1095–105. doi:10.1128/CVI.00068-08.
White PL, Parr C, Thornton C, Barnes RA. Evaluation of real-time PCR, galactomannan enzyme-linked immunosorbent assay (ELISA), and a novel lateral-flow device for diagnosis of invasive aspergillosis. J Clin Microbiol. 2013;51(5):1510–6. doi:10.1128/JCM.03189-12.
Lamoth F, Cruciani M, Mengoli C, Castagnola E, Lortholary O, Richardson M, et al. beta-Glucan antigenemia assay for the diagnosis of invasive fungal infections in patients with hematological malignancies: a systematic review and meta-analysis of cohort studies from the Third European Conference on Infections in Leukemia (ECIL-3). Clin Infect Dis. 2012;54(5):633–43. doi:10.1093/cid/cir897.
Kanamori H, Kanemitsu K, Miyasaka T, Ameku K, Endo S, Aoyagi T, et al. Measurement of (1–3)-beta-D-glucan derived from different gauze types. Tohoku J Exp Med. 2009;217(2):117–21.
Kimura Y, Nakao A, Tamura H, Tanaka S, Takagi H. Clinical and experimental studies of the limulus test after digestive surgery. Surg Today. 1995;25(9):790–4.
Marty FM, Lowry CM, Lempitski SJ, Kubiak DW, Finkelman MA, Baden LR. Reactivity of (13)-beta-d-glucan assay with commonly used intravenous antimicrobials. Antimicrob Agents Chemother. 2006;50(10):3450–3. doi:10.1128/AAC.00658-06.
Hanson KE, Pfeiffer CD, Lease ED, Balch AH, Zaas AK, Perfect JR, et al. beta-D-glucan surveillance with preemptive anidulafungin for invasive candidiasis in intensive care unit patients: a randomized pilot study. PLoS One. 2012;7(8):e42282. doi:10.1371/journal.pone.0042282.
Mohr JF, Sims C, Paetznick V, Rodriguez J, Finkelman MA, Rex JH, et al. Prospective survey of (13)-beta-D-glucan and its relationship to invasive candidiasis in the surgical intensive care unit setting. J Clin Microbiol. 2011;49(1):58–61. doi:10.1128/JCM.01240-10.
Mennink-Kersten MA, Warris A, Verweij PE. 1,3-beta-D-glucan in patients receiving intravenous amoxicillin-clavulanic acid. N Engl J Med. 2006;354(26):2834–5. doi:10.1056/NEJMc053340.
Mennink-Kersten MA, Ruegebrink D, Verweij PE. Pseudomonas aeruginosa as a cause of 1,3-beta-D-glucan assay reactivity. Clin Infect Dis. 2008;46(12):1930–1. doi:10.1086/588563.
Pickering JW, Sant HW, Bowles CA, Roberts WL, Woods GL. Evaluation of a (1- > 3)-beta-D-glucan assay for diagnosis of invasive fungal infections. J Clin Microbiol. 2005;43(12):5957–62. doi:10.1128/JCM.43.12.5957-5962.2005.
Hadrich I, Makni F, Cheikhrouhou F, Neji S, Amouri I, Sellami H, et al. Clinical utility and prognostic value of galactomannan in neutropenic patients with invasive aspergillosis. Pathol Biol. 2012;60(6):357–61. doi:10.1016/j.patbio.2011.10.011.
Fisher CE, Stevens AM, Leisenring W, Pergam SA, Boeckh M, Hohl TM. The serum galactomannan index predicts mortality in hematopoietic stem cell transplant recipients with invasive aspergillosis. Clin Infect Dis. 2013;57(7):1001–4. doi:10.1093/cid/cit393.
Chai LY, Kullberg BJ, Johnson EM, Teerenstra S, Khin LW, Vonk AG, et al. Early serum galactomannan trend as a predictor of outcome of invasive aspergillosis. J Clin Microbiol. 2012;50(7):2330–6. doi:10.1128/JCM.06513-11.
Marr KA, Schlamm HT, Herbrecht R, Rottinghaus ST, Bow EJ, Cornely OA, et al. Combination antifungal therapy for invasive aspergillosis: a randomized trial. Ann Intern Med. 2015;162(2):81–9. doi:10.7326/M13-2508.
Chai LY, Kullberg BJ, Earnest A, Johnson EM, Teerenstra S, Vonk AG, et al. Voriconazole or amphotericin B as primary therapy yields distinct early serum galactomannan trends related to outcomes in invasive aspergillosis. PLoS One. 2014;9(2), e90176. doi:10.1371/journal.pone.0090176.
http://www.accessdata.fda.gov/cdrh_docs/pdf9/K093678.pdf. Accessed 15 June 2015.
Prattes J, Koidl C, Eigl S, Krause R, Hoenigl M. Bronchoalveolar lavage fluid sample pretreatment with Sputasol((R)) significantly reduces galactomannan levels. J Infect. 2015;70(5):541–3. doi:10.1016/j.jinf.2014.11.005.
Guo YL, Chen YQ, Wang K, Qin SM, Wu C, Kong JL. Accuracy of BAL galactomannan in diagnosing invasive aspergillosis: a bivariate metaanalysis and systematic review. Chest. 2010;138(4):817–24. doi:10.1378/chest.10-0488.
Zou M, Tang L, Zhao S, Zhao Z, Chen L, Chen P, et al. Systematic review and meta-analysis of detecting galactomannan in bronchoalveolar lavage fluid for diagnosing invasive aspergillosis. PLoS One. 2012;7(8), e43347. doi:10.1371/journal.pone.0043347.
D’Haese J, Theunissen K, Vermeulen E, Schoemans H, De Vlieger G, Lammertijn L, et al. Detection of galactomannan in bronchoalveolar lavage fluid samples of patients at risk for invasive pulmonary aspergillosis: analytical and clinical validity. J Clin Microbiol. 2012;50(4):1258–63. doi:10.1128/JCM.06423-11.
Avni T, Levy I, Sprecher H, Yahav D, Leibovici L, Paul M. Diagnostic accuracy of PCR alone compared to galactomannan in bronchoalveolar lavage fluid for diagnosis of invasive pulmonary aspergillosis: a systematic review. J Clin Microbiol. 2012;50(11):3652–8. doi:10.1128/JCM.00942-12.
Sun W, Wang K, Gao W, Su X, Qian Q, Lu X, et al. Evaluation of PCR on bronchoalveolar lavage fluid for diagnosis of invasive aspergillosis: a bivariate metaanalysis and systematic review. PLoS One. 2011;6(12), e28467. doi:10.1371/journal.pone.0028467.
Heng SC, Chen SC, Morrissey CO, Thursky K, Manser RL, De Silva HD, et al. Clinical utility of Aspergillus galactomannan and PCR in bronchoalveolar lavage fluid for the diagnosis of invasive pulmonary aspergillosis in patients with haematological malignancies. Diagn Microbiol Infect Dis. 2014;79(3):322–7. doi:10.1016/j.diagmicrobio.2014.03.020.
Hoenigl M, Koidl C, Duettmann W, Seeber K, Wagner J, Buzina W, et al. Bronchoalveolar lavage lateral-flow device test for invasive pulmonary aspergillosis diagnosis in haematological malignancy and solid organ transplant patients. J Infect. 2012;65(6):588–91. doi:10.1016/j.jinf.2012.10.003.
Willinger B, Lackner M, Lass-Florl C, Prattes J, Posch V, Selitsch B, et al. Bronchoalveolar lavage lateral-flow device test for invasive pulmonary aspergillosis in solid organ transplant patients: a semiprospective multicenter study. Transplantation. 2014;98(8):898–902. doi:10.1097/TP.0000000000000153.
Miceli MH, Goggins MI, Chander P, Sekaran AK, Kizy AE, Samuel L, et al. Performance of lateral flow device and galactomannan for the detection of Aspergillus species in bronchoalveolar fluid of patients at risk for invasive pulmonary aspergillosis. Mycoses. 2015;58(6):368–74. doi:10.1111/myc.12327.
Eigl S, Prattes J, Lackner M, Willinger B, Spiess B, Reinwald M, et al. Multicenter evaluation of a lateral-flow device test for diagnosing invasive pulmonary aspergillosis in ICU patients. Crit Care. 2015;19:178. doi:10.1186/s13054-015-0905-x.
Hoenigl M, Prattes J, Spiess B, Wagner J, Prueller F, Raggam RB, et al. Performance of galactomannan, beta-d-glucan, Aspergillus lateral-flow device, conventional culture, and PCR tests with bronchoalveolar lavage fluid for diagnosis of invasive pulmonary aspergillosis. J Clin Microbiol. 2014;52(6):2039–45. doi:10.1128/JCM.00467-14. This study demonstrated utility of rapid, point-of-care test for BAL testing of Aspergillus LFD.
Maertens J, Verhaegen J, Demuynck H, Brock P, Verhoef G, Vandenberghe P, et al. Autopsy-controlled prospective evaluation of serial screening for circulating galactomannan by a sandwich enzyme-linked immunosorbent assay for hematological patients at risk for invasive Aspergillosis. J Clin Microbiol. 1999;37(10):3223–8.
Coates M, Wilson J. Central nervous system aspergillus infection complicating renal transplantation. Australas Radiol. 2001;45(3):338–42.
Viscoli C, Machetti M, Gazzola P, De Maria A, Paola D, Van Lint MT, et al. Aspergillus galactomannan antigen in the cerebrospinal fluid of bone marrow transplant recipients with probable cerebral aspergillosis. J Clin Microbiol. 2002;40(4):1496–9.
Reinwald M, Buchheidt D, Hummel M, Duerken M, Bertz H, Schwerdtfeger R, et al. Diagnostic performance of an Aspergillus-specific nested PCR assay in cerebrospinal fluid samples of immunocompromised patients for detection of central nervous system aspergillosis. PLoS One. 2013;8(2), e56706. doi:10.1371/journal.pone.0056706.
Suwantarat N, Lee R, Carroll KC, Zhang SX. Questionable utility of galactomannan testing for diagnosis of Exserohilum rostratum infection. J Clin Microbiol. 2014;52(7):2742–3. doi:10.1128/JCM.01148-14.
Lockhart SR, Pham CD, Gade L, Iqbal N, Scheel CM, Cleveland AA, et al. Preliminary laboratory report of fungal infections associated with contaminated methylprednisolone injections. J Clin Microbiol. 2013;51(8):2654–61. doi:10.1128/JCM.01000-13.
Klont RR, Mennink-Kersten MA, Verweij PE. Utility of Aspergillus antigen detection in specimens other than serum specimens. Clin Infect Dis. 2004;39(10):1467–74. doi:10.1086/425317.
Haynes KA, Latge JP, Rogers TR. Detection of Aspergillus antigens associated with invasive infection. J Clin Microbiol. 1990;28(9):2040–4.
Duettmann W, Koidl C, Troppan K, Seeber K, Buzina W, Wolfler A, et al. Serum and urine galactomannan testing for screening in patients with hematological malignancies. Med Mycol. 2014;52(6):647–52. doi:10.1093/mmy/myu019.
Dufresne SF, Datta K, Li X, Dadachova E, Staab JF, Patterson TF, et al. Detection of urinary excreted fungal galactomannan-like antigens for diagnosis of invasive aspergillosis. PLoS One. 2012;7(8), e42736. doi:10.1371/journal.pone.0042736.
Acknowledgments
The authors would like to thank Graeme Forrest, MBBS, for his thoughtful review of the manuscript.
Compliance with Ethics Guidelines
Conflict of Interest
Corinne Klein declares that she has no conflict of interest. Christopher Pfeiffer declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Fungal Infections
Rights and permissions
About this article
Cite this article
Klein, C.N., Pfeiffer, C.D. Diagnosis of Invasive Aspergillosis: Use of the Galactomannan Assay. Curr Treat Options Infect Dis 7, 163–175 (2015). https://doi.org/10.1007/s40506-015-0055-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40506-015-0055-3
Keywords
- Diagnosis
- Culture
- Blood culture, invasive aspergillosis
- Aspergillus, galactomannan
- Beta-d-glucan
- PCR
- Aspergillus lateral flow device
- Bronchoalveolar lavage
- Serum
- FDA
- Platelia
- Treatment
- Prognosis
- Invasive fungal disease
- Piperacillin/tazobactam
- False positive
- Antifungal therapy
- Performance
- Accuracy
- Diagnostic odds ratio
- Meta-analysis
- Systematic review
- Optical density index
- Plasma-Lyte
- Voriconazole
- Posaconazole
- Epidemiology