Abstract
Purpose
Purpose Generalized anxiety disorder (GAD) is one of the most common anxiety disorders, afflicting approximately 6% of the general population in their lifetime. It has a chronic and episodic course, requiring a long-term treatment approach. A variety of pharmacological agents and psychological treatments have been shown to be efficacious as GAD treatments; however, remission effect sizes for first-line treatments are small. This review aims to examine the existing evidence for next-step pharmacological and psychological treatments for individuals who remain symptomatic after first-line treatment.
Recent Findings
Recent Findings Relatively few studies have examined next-step treatments for treatment-resistant GAD (TR-GAD). The bulk of the available treatment-resistant literature has investigated augmentation with atypical antipsychotics or pregabalin.
Summary
Summary Unfortunately, there is little information to guide clinicians in this area. The strongest evidence supports augmentation with pregabalin, however, this is based primarily upon one study. Approaches to consider when treating patients with TR-GAD are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Generalized anxiety disorder (GAD) is one of the most common anxiety disorders. It afflicts approximately 6% of the general population in their lifetime [1] and is even more prevalent in primary care settings [2]. It is associated with high rates of psychiatric comorbidity, particularly major depressive disorder and other anxiety disorders, as well as with medical comorbidity. GAD patients often present with chronic somatic complaints and are high utilizers of medical services. The course of GAD can be both chronic and episodic, requiring a long-term treatment approach. Unfortunately, there is little information to guide clinicians in this area.
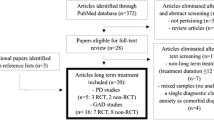
The evaluation of pharmacological treatments for GAD has spanned a broad range of drug classes. Antidepressants, anxiolytics, anticonvulsants, antipsychotics, and antihistamines have all been shown to be efficacious as GAD treatments, although selective serotonin reuptake inhibitors (SSRI’s) and serotonin-noradrenalin reuptake inhibitors (SNRI’s) are considered to be the gold standard, first-line treatments. These agents typically yield response rates of 60–75% when compared to placebo [3•], but have small effect sizes: 0.36 for SSRIs and 0.42 for SNRIs [4]. Cognitive behavioral therapy (CBT) is the gold standard psychological treatment for GAD. Meta-analysis-derived response rates for CBT in GAD are approximately 46% [5, 6•] when compared to treatment as usual or waitlist controls, although effect sizes appear to be large (.71–0.90) [7]. Therefore, rates of partial or non-response are also relatively high, indicating that many patients continue to experience impairing symptoms following first-line treatment [8]. Thus, achieving and maintaining remission in GAD is often difficult. Relatively few studies have examined next-step treatments for refractory GAD (TR-GAD). The bulk of the available treatment-resistant literature has investigated augmentation with atypical antipsychotics or pregabalin. This article will review the existing pharmacotherapy, psychotherapy, and alternative treatment literature for TR-GAD.
Each treatment-resistant strategy will be described by its level of evidence according to the Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress, and obsessive-compulsive disorders (Table 1) [9•]. Based on these guidelines, first-line treatments would typically be level 1 evidence or level 2 evidence plus clinical support; second-line treatments would be level 3 evidence or higher plus clinical support for safety and efficacy and third-line treatments would be level 4 evidence or higher plus clinical support for safety and efficacy [9•].
All treatments reviewed in this article are summarized in Table 2.
Treatment
Atypical antipsychotics
Although antipsychotics are most commonly used to treat psychosis and schizophrenia [10], the existing literature suggests that they may also be effective at treating anxiety and mood disorders [11]. More recently, second-generation, or atypical, antipsychotics have been explored in the treatment of TR-GAD. Unlike first-generation antipsychotics, they are less likely to cause extrapyramidal symptoms and tardive dyskinesia due to their lower fat solubility and affinity to D2 receptors [12, 13]. This improved side effect profile has caused a resurgence of interest in use of atypicals as an anxiolytic treatment. Interestingly, this class of medication has been shown to address a variety of anxiety and depressive symptoms in populations suffering from schizophrenia and schizoaffective disorders [14, 15]. Although the effects of these agents on the dopaminergic system are well-established, the mechanism of action of atypical antipsychotics on anxiety symptoms is also thought to involve the serotonin (5-HT) neurotransmitter system, more specifically, blocking 5-HT2A receptors [16, 17], partial agonism at 5-HT1A, or antagonism of central histamine receptors [18]. Atypical antipsychotics have been examined as both a monotherapy and adjunctive therapy in TR-GAD. According to the Canadian Treatment Guidelines, the level of evidence supporting use of adjunctive atypical antipsychotics in GAD ranges from level 1 for quetiapine XR monotherapy, adjunctive quetiapine, and adjunctive risperidone to level 3 for adjunctive aripiprazole and adjunctive quetiapine XR. Atypical antipsychotics are considered a second- or third-line treatment for GAD [9•].
Quetiapine
The evidence supporting use of quetiapine as an augmentation strategy for TR-GAD is currently equivocal. A 12-week open-label study found that in 32 TR-GAD patients, quetiapine augmentation (mean dose = 386 ± 230 mg/day) resulted in significant mean reductions of the Hamilton Anxiety Rating Scale (HAM-A − 20.6; p < 0.001). Significant changes were also noted in secondary outcome measures including the Clinical Global Impression–Severity (CGI-S −3.1; p < 0.001), Pittsburgh Sleep Quality Index (PSQI − 8.1; p < 0.001), Penn State Worry Questionnaire (PSWQ − 11.5; p < 0.001), Dysfunctional Beliefs and Attitudes about Sleep Scale (DBAS; − 13.6; p < 0.01), and all subscales of the Sheehan Disability Index (SDI work; − 2.1; p < 0.001, SDI family; − 1.8; p < 0.001, SDI social; − 2.7; p < 0.001) [19].
Additionally, a 2-phase prospective trial for quetiapine augmentation with controlled-release paroxetine (paroxetine CR) was conducted on patients with TR-GAD. In phase I, open-label paroxetine CR was administered for 10 weeks (47.3 ± 16.2 mg/day, N = 54), with non-remitters moving onto phase II. In the second phase, non-remitters (HAM-A ≤ 7) entered an 8-week randomized controlled trial (RCT) where quetiapine or placebo was added to paroxetine CR treatment (N = 22). At week 8, quetiapine augmentation (mean endpoint dose: 120.5 ± 100.5 mg/day) resulted in only modest changes in anxiety symptoms as per change in mean HAM-A (− 1.8 ± 5.2, p = 0.12) and CGI-S scores (− 0.6 ± − 1.0, p = 0.007). No significant benefit of quetiapine augmentation with continued paroxetine CR was noted with respect to achieved responder or remission status [20].
An 8-week RCT-treated patients who showed partial (reduction of HAM-A score between 25 and 50%) or no response (reduction of HAM-A score of ≥ 25%) to SSRI treatment with either adjunctive quetiapine (N = 10) (25–150 mg/day) or placebo (N = 10). By the end of the treatment, both groups showed significant improvements in HAM-A; however, the quetiapine group showed a statistically significant improvement over placebo (time effect: F = 64.87, p < 0.001; time-by-treatment effect: F = 5.19, p = 0.035; treatment effect: F = 0.14, p = 0.72) and CGI-S scores (time effect: F = 78.40, p < 0.001; time-by-treatment effect: F = 19.60, p ≤ 0.001; treatment effect: F = 0.001, p = 1.0). Additionally, the quetiapine group showed a greater number of responders (60 vs 30%) compared to the placebo group; however, this difference did not reach statistical significance (p = 0.37) [21].
A large, flexible-dose, parallel-group RCT (N = 409) looked at the efficacy of 8 weeks of adjunctive quetiapine XR (mean dose = 174.3 ± 49.0 mg/day) or placebo to SSRI/SNRI treatment. No significant differences were found between the two groups on the primary outcome measure, HAM-A. However, significant reductions were observed on CGI-S scores in the quetiapine group compared to placebo from randomization to week 8 (− 1.36 for quetiapine vs. − 1.13 for placebo, p < 0.05) [22].
Risperidone
To date, three studies have examined adjunctive risperidone in TR-GAD. An 8-week open-label study examined flexible-dose adjunctive risperidone (1.12 ± 0.68 mg/day) in a mixed anxiety disorder sample (N = 30; 16 primary GAD-only patients) who were currently being treated with an SSRI, SNRI, and/or benzodiazepine. In GAD-only patients, a significant decrease in HAM-A (6.75 ± 8.34 p < 0.0055) was found, while a significant decrease in HAM-A (5.97 ± 8.29, p = 0.0005) and CGI-S (1.53 ± 1.63, p < 0.000) was found across all three primary anxiety disorders (social anxiety disorder (SAD), panic disorder (PD), and GAD) [23].
A 5-week RCT (N = 39) comparing adjunctive risperidone to placebo in a complete TR-GAD population found that HAM-A scores significantly decreased in the risperidone group (mean dose = 1.1 ± 0.4 mg/day) compared to the placebo group (HAM-A − 9.8 ± 5.5 vs − 6.2 ± 4.9, p = 0.034). However, response rates as per CGI-I did not differ significantly with 58% achieving response in the adjunctive risperidone group compared to 35% in the placebo group (p = 0.152). Although patients in the risperidone group demonstrated greater improvements compared to those randomized to placebo on secondary outcome measures of the Hospital Anxiety and Depression (HAD) Scale anxiety subscale and the Montgomery-Asberg Depression Rating Scale (MADRS), these did not reach statistical significance [24].
Finally, an RCT (N = 417) compared efficacy of 4 weeks of adjunctive risperidone or placebo to either an antidepressant, a buspirone, or a benzodiazepine in a TR-GAD population. Using the Patient-Rated Troubling Symptoms for Anxiety (PaRTS-A) as the primary efficacy measure, a significant difference between the two treatment groups was not found at study endpoint (− 8.54 ± 0.63 vs − 7.61 ± 0.64, p = 0.265). However, a post hoc analysis revealed that PaRTS-A symptoms of moderate to severe severity at baseline suggested greater improvements with adjunctive risperidone than placebo (− 26.0 ± 20.4 vs − 21.8 ± 18.5, p = 0.040). Additionally, significant differences were also found in favor of risperidone on the Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q total 63.5 ± 13.0 vs 61.4 ± 14.0, p = 0.163), (Q-LES-Q Overall Life Satisfaction Score 3.2 ± 0.89 vs 3.0 ± 0.94, p = 0.046), (Q-LES-Q Medication Satisfaction Score 3.3 ± 0.95 vs 3.0 ± 1.01, p = 0.015) and the Patient Global Improvement Scale (PGIS 3.1 ± 1.2 vs 3.4 ± 1.0, p = 0.016) [25].
Ziprasidone
Snyderman et al. (2005) conducted a 7-week open-label pilot study (N = 13) using ziprasidone (20–80 mg/day) in a refractory GAD population. All primary and secondary outcomes were found to be significantly reduced from baseline to endpoint (mean change: HAM-A: 11.15, p < 0.001; CGI-S 1.54, p < 0.001; CGI-I = 2.08, p < 0.001; Hospital Anxiety and Depression Scale 4.73, p < 0.003; Hamilton Depression Scale (HAM-D) 7.10, p < 0.003; Sheehan Disability Scale (SDS) 6.81, p < 0.014) [26].
Lohoff et al. (2010) conducted an 8-week RCT examining the effect of ziprasidone (20–80 mg/day) (N = 41) versus placebo (N = 21) in TR-GAD. Within both groups, participants were treated either adjunctively or with ziprasidone/placebo monotherapy. Although improvements were found in both ziprasidone groups on the HAM-A, the findings did not achieve statistical significance. However, endpoint HAM-A scores were lower (i.e., more improved) in the ziprasidone monotherapy group compared to those of the augmented group or placebo groups (ziprasidone monotherapy 8.31 ± 6.55, ziprasidone augmented 15.8 ± 7.54, placebo monotherapy 13 ± 8.62, placebo only 11.14 ± 8.40, p = 0.22). Response rates (defined as CGI-I ≤ 2) were 73% for ziprasidone (both groups) and 50% for placebo (both groups) [27].
Olanzapine
In the only study examining adjunctive olanzapine in TR-GAD, patients began with 6 weeks of open-label fluoxetine treatment. Patients who remained symptomatic (either CGI-I ≥ 4 or < 50% reduction in HAM-A) while receiving 20 mg/day of fluoxetine moved onto phase II, a 6-week RCT of adjunctive olanzapine (N = 9) or placebo (N = 12). Although baseline to endpoint changes in HAM-A scores were not significant between the two groups, individuals randomized to adjunctive olanzapine were significantly more likely to be classified as responders (> 50% reduction in HAM-A): 56% in the olanzapine group vs. 8% in the placebo group (p = 0.046) [28].
Aripiprazole
Three open-label studies have examined aripiprazole in TR-GAD. One 12-week study examined 17 patients with depression and anxiety (24% with TR-GAD; N = 4) who were partial or non-responders to initial SSRI treatment. These patients received an average dose of 16.9 ± 6.6 mg/day of adjunctive aripiprazole and demonstrated significant decreases in the primary outcome measure (CGI-S mean change − 1.6, p < 0.001). Based on CGI-I criteria for response (CGI-I ≤ 2), 67% of patients showed full response at endpoint [29].
Another 6-week open-label study (N = 9) looked at the effects of aripiprazole augmentation (mean final dose = 13.9 mg/day) to existing antidepressant treatment in a TR-GAD sample (HAM-A ≥ 14 and CGI-S ≤ 4). They found significant reductions in mean HAM-A from baseline to endpoint (mean change − 12.0, p < 0.0001), in addition to 89% of patients achieving a CGI-I ≤ 2 at endpoint [30].
In an 8-week open-label study, Hoge et al. (2008) administered flexible dosages of aripiprazole in a mixed refractory GAD and panic disorder population. The 13 TR-GAD patients showed significant improvements from baseline to endpoint on the primary outcome measure, (CGI-S − 1.2, p < 0.01) and on all secondary outcome measures (HAM-A − 6.7, p < 0.1) [31].
Therefore, the results for adjunctive atypical antipsychotics as treatments in TR-GAD samples are not robust. Adjunctive quetiapine and risperidone both have mixed results, although the RCTs with the largest sample sizes were negative, making it difficult to recommend these agents for TR-GAD. Aripiprazole has demonstrated a signal; however, this requires further examination in RCTs and it would be considered a third-line treatment for TR-GAD.
Anticonvulsants
The mechanism of action of agents classified as anticonvulsants can be broadly grouped into three types: those which facilitate gamma-amino-butyric acid (GABA) transmission, those which block voltage-gated ion channels and reduce excitation, and those that block T-type calcium channels [32]. Pregabalin is the only anticonvulsant that has been examined in TR-GAD. It is a structural derivative of GABA which binds to calcium voltage-gated channels in pre-synaptic neurons and reduces the release of excitatory neurotransmitters—mainly glutamate and substance P [33]. Pregabalin is considered a first-line monotherapeutic treatment in GAD (level 1 evidence) and a second-line treatment when used adjunctively (level 2 evidence) [9].
Pregabalin
Pregabalin has been examined as an adjunctive treatment in several TR-GAD studies. The Amplification of Definition of Anxiety (ADAN) study was a 6-month, Spanish prospective observational study in patients with GAD, whose purpose was to examine the impact of broadening the DSM-IV diagnostic criteria for DSM-5. In three post hoc analyses of the ADAN study data, the effects of pregabalin in the treatment of TR-GAD have been examined. One of these studies examined the improvements in a subset of the sample (n = 133) with SSRI/SNRI TR-GAD and significant depressive symptoms (MADRS ≥ 35) and began adjunctive pregabalin treatment (mean dose = 222 ± 120 mg/day) at study initiation. Participants demonstrated significant HAM-A reductions after 6 months (− 20.3, p < 0.0001). Additionally, both HAM-A psychic and somatic sub-scores improved at 6 months (HAM-A psychic − 10.9, p < 0.0001, HAM-A somatic − 9.4, p < 0.0001), as well as depressive symptoms, with a 56.6% mean reduction found on MADRS score (MADRS − 22.3, p < 0.0001). Overall, results suggested benefit of adjunctive pregabalin treatment in TR-GAD with significant depressive symptoms [34]. Another ADAN post hoc analysis examined GAD participants who had a partial response to an SSRI (HAM-A > 16) and were either treated with adjunctive pregabalin (n = 486) or were switched to either a different SSRI or anxiolytic agent (usual care) (n = 239). Adjunctive pregabalin was found to be superior to usual care based on mean reductions on HAM-A (HAM-A mean change (95% CI) − 15.2 (− 16.0; − 14.4) vs. − 10.7 (− 11.8; − 9.5), p < 0.001) [35]. All participant-rated measures also significantly favored pregabalin. Furthermore, this study also examined the economic impact of adjunctive pregabalin versus usual care and found that healthcare costs were significantly reduced in both groups, with similar 6-month costs [35].
In another cost-effectiveness post hoc analysis using the ADAN data, De Salas-Cansado et al. (2012) examined both the cost and efficacy of treatment with either pregabalin (adjunctive or monotherapy) or SSRI/SNRI (adjunctive or monotherapy) in benzodiazepine-refractory GAD (n = 282). No significant differences in efficacy were found between the two groups; however, pregabalin was found to be significantly more cost-effective [36].
There is currently only one RCT evaluating the efficacy of pregabalin in TR-GAD. This 8-week study (N = 356) examined the efficacy of adjunctive pregabalin versus placebo in patients with partial response to 8 weeks of open-label venlafaxine XR, escitalopram, or paroxetine treatment. Adjunctive pregabalin (150–600 mg/day) treatment resulted in significant improvements in GAD symptoms compared to placebo (HAM-A change − 7.6 ± 0.35 vs − 6.4 ± 0.36, p < 0.01). Rates of response, based on HAM-A scores (≥ 50% reduction from baseline), were significantly greater in the pregabalin group (47.5%) compared to those of placebo (35.2%, p = 0.0145), while no differences were noted in rates of remission (HAM-A ≤ 7). Similarly, CGI-S response rates (CGI-S ≤ 2) were also significantly higher in the pregabalin group (43.8%) compared to those receiving placebo (31.8%, p < 0.0097). No significant differences were found in CGI-I, HAM-D, and SDS scores from baseline to endpoint [37].
Valproate
Valproate is an anticonvulsant which has demonstrated efficacy in bipolar disorder. It has been examined in a wide variety of psychiatric conditions including PD, SAD, and posttraumatic stress disorder (PTSD) [38, 39, 40]. Although the mechanisms of its therapeutic actions are not well understood, valproate is thought to increase gamma-aminobutyric acid (GABA) levels in the brain and may alter the properties of voltage-dependent sodium channels [41]. The use of valproate has been examined in one published case report of a 45-year-old female patient with TR-GAD. Valproate treatment was initiated (initial dose of 1000 mg/day) while concurrently reducing existing venlafaxine treatment. After 1 month of valproate treatment, the patient reported being almost free of anxiety and tension (valproic acid level was 73 μg/mL). Once venlafaxine treatment was discontinued (day 4) and valproate maintained (1000 mg/day), the patient reported feeling completely relaxed and at 6 months of treatment, reported being free of any psychiatric symptoms [42].
Within the anticonvulsant class, adjunctive pregabalin has the strongest evidence for TR-GAD, however, this is based on one RCT. Nevertheless, this agent is often used in clinical practice with positive results and it is considered a first-line monotherapeutic treatment for non-refractory GAD. For TR-GAD, adjunctive pregabalin would therefore be considered a first-line treatment, as there is one RCT (level 2 evidence) with clinical support for safety and efficacy. Valproate would be considered a third-line treatment at this stage, as it only has level 4 evidence in TR-GAD.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is the first-line psychological treatment for GAD [9•]. The Coordinated Anxiety Learning and Management (CALM) intervention features individual, computer-based CBT that can be adapted to one of four anxiety disorders common in primary care settings (SAD, PD, PTSD, and GAD). This intervention has demonstrated superiority over usual care for reducing overall anxiety and disability [43] and numerous disorder-specific symptoms [44] in a large RCT in patients with principal or comorbid GAD, SAD, PD, or PTSD. A recent analysis of this data has examined the effects of CALM on refractory anxiety populations [45]. Of the 227 refractory patients examined in this study, 174 (76.65%) had TR-GAD. Participants were randomized to the CALM intervention (n = 117) or usual care (n = 110). Patients in the CALM condition could choose to have CALM-CBT (i.e., CBT with medication management) or CBT alone. Although no specific analyses were completed for TR-GAD participants, CALM-CBT was associated with greater response at 6 months (AOR = 3.78, 95% CI 2.02–7.07) and 12 months (AOR = 2.49, 95% CI 1.36–4.58) compared to usual care based on the Brief Symptom Inventory. Additionally, CALM-CBT was also associated with increased odds of remission at these time points; 44.3% were considered remitted at 6 months compared to 21.9% of the usual care condition (p < 0.001). No significant differences were found between individuals who received medication management and those receiving CBT alone; however, the authors concluded that a higher CBT dose may have been associated with improved outcomes [45].
CBT is a commonly used modality in clinical practice for individuals with GAD that is refractory to pharmacological treatments. Based upon the current evidence (level 3 at best), adjunctive CBT would be considered a second-line treatment for TR-GAD, however, additional RCTs may yield a stronger signal, making adjunctive CBT a first-line treatment for pharmacological TR-GAD.
Novel treatment strategies for TR-GAD
Ketamine is a non-competitive antagonist of the NMDA receptor (a type of glutamate receptor). It has demonstrated antidepressant and anti-obsessional effects [46] and is administered intravenously. The efficacy of ketamine was evaluated in 12 non-depressed participants with TR-GAD and/or TR-SAD using an ascending single-dose study design at weekly intervals (0.25, 0.5, 1 mg/kg administered subcutaneously). Within 1 h of dosing, patients reported reduced anxiety. Eighty-three percent of the sample reported a > 50% reduction in the HAM-A and/or Fear Questionnaire scores following doses of 0.5 or 1 mg/kg [47]. At present, ketamine would have level 3 evidence and be considered a third-line treatment for TR-GAD, but given the now strong literature for ketamine in MDD and preliminary signal in OCD, this agent may hold promise for the treatment of TR-GAD, but warrants further investigation.
Discussion
Unfortunately, the literature examining next-step treatments in GAD are woefully limited. Considering this disorder has both a high prevalence and high rates of treatment-resistance, this is problematic for both clinicians and patients. Based on the available treatment-resistant literature, the strongest evidence appears to be for pregabalin augmentation [37], however, this study ended early due to observed benefit, therefore the results may have been over-estimated. With the exception of open-label evidence using aripiprazole augmentation, there also appears to be little support for antipsychotic augmentation. This conclusion is supported by a recent meta-analysis of treatment-resistant anxiety disorders [48•] which included 3 TR-GAD studies. No significant treatment effect was found in a sub-group analysis of TR-GAD in terms of response (CGI-I ≤ 2) or change in HAM-A scores using augmentation with olanzapine [28], quetiapine [21], or pregabalin [37].
In the non-refractory GAD literature, SSRIs and SNRIs yield the highest rates of response and remission [49]. One meta-analysis found that fluoxetine had the highest rates of both response and remission, while sertraline was the best tolerated [3•]. Although benzodiazepines have demonstrated comparable effect sizes to SSRIs and SNRIs in GAD, they are typically only recommended as acute treatments due to the potential adverse events associated with long-term use, including addiction [9•, 49]. While CBT has also demonstrated efficacy in GAD, few studies have directly compared it to pharmacotherapy. Mitte (2005) conducted a meta-analysis comparing the two modalities in GAD and found no significant differences [50]. Bandelow et al. (2015) also conducted a meta-analysis of treatments for anxiety disorders and included both pharmacotherapy and psychotherapy [51•]. For GAD, the largest effect size (6.04) was found for CBT and drug combinations [52, 53] based on the two studies included in the meta-analysis. One of the studies [52] found that diazepam plus CBT was superior to CBT alone, diazepam alone and CBT plus placebo, however, the other included study found no difference between venlafaxine plus CBT and venlafaxine alone [53].
In the clinical experience of this author, the combination of two first-line, evidence-based agents, pregabalin, or benzodiazepines (in particular) to an SSRI/SNRI has been the most beneficial strategy for TR-GAD patients. In addition, selecting agents with the lowest adverse event profile is very important in this population, given the propensity of GAD patients to experience somatic distress.
Comorbid medical and psychiatric conditions are essential to consider when treating GAD. Upwards of 98% of GAD patients report comorbid anxiety, mood or substance use disorders [54]. Cognizance of the patient’s comorbid conditions is important, as these conditions may be affecting choice of agent and treatment response. For example, comorbid depression has been shown to be a poor prognostic indicator of GAD symptoms response [55]. In addition, comorbid medical conditions such as thyroid, cardiac, respiratory, and gastro-intestinal conditions all occur at high rates in GAD patients, and the treatment of these medical comorbidities may also impact GAD symptoms [54]. While further work in this area is required to elucidate specific treatments for TR-GAD, future research should examine GAD with comorbidity, as this how it most commonly presents in both primary and tertiary cares. Given the chronic waxing and waning course of GAD, improvements in functional impairment as well as symptom remission should be the focus of treatment. In light of limited evidence, next-step treatments for refractory patients should be individualized based on the stage of illness, comorbidities, and treatment response to past modalities.
References and Recommended Reading
Recently published papers of particular interest have been highlighted as: • Of importance
Kessler R, Berglund P, Demler O, Jin R, Merikangas K, Walters E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. https://doi.org/10.1001/archpsyc.62.6.593.
Wittchen H. Generalized anxiety disorder: prevalence, burden and cost to society. Depress Anxiety. 2002;16:162–71. https://doi.org/10.1002/da.10065.
Baldwin D, Waldman S, Allgulander C. Evidence-based pharmacological treatment of generalized anxiety disorder. Int J Neuropsychp. 2011;14:697–710. https://doi.org/10.1017/S1461145710001434. Up to date systematic review and meta-analysis of pharmacological treatments for GAD.
Hidalgo R, Tupler R, Davidson J. An effect-size analysis of pharmacological treatments for generalized anxiety disorder. J Psychopharmacol. 2007;21:864–72. https://doi.org/10.1177/0269881107076996.
Hofmann S, Asnaani A, Vonk I, Sawyer A, Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. 2012;36:427–40. https://doi.org/10.1007/s10608-012-9476-1.
• Hunot V, Churchill R, Silva de Lima M, Teixeira V. Psychological therapies for generalised anxiety disorder. Cochrane Database of Systematic Reviews. 2007;1:CD001848. https://doi.org/10.1002/14651858.CD001848. Good review of psychological treatment strategies for GAD.
Covin R, Ouimet A, Seeds P, Dozois D. A meta-analysis of CBT for pathological worry among clients with GAD. J Anxiety Disord. 2008;22:108–16. https://doi.org/10.1016/j.janxdis.2007.01.002.
Murrough J, Yaqubi S, Sayed S, Charney D. Emerging drugs for the treatment of anxiety. Expert Opin Emerg Dr. 2015;20:393–406. https://doi.org/10.1517/14728214.2015.1049996.
• Katzman M, Bleau P, Blier P, Chokka P, Kjernisted K, Van Amerigan E. Canadian Clinical Practice Guidelines for the Management of Anxiety, post-traumatic stress and obsessive-compulsive disorders. BMC Psychiatry. 2014;14(S1):1–83. https://doi.org/10.1186/1471-244X-14-S1-S1. A good summary of treatments for all of the anxiety disorders, including GAD, provides levels of scientific evidence and treatment recommendations.
Lieberman J, Stroup S, McEvoy J, Swartz M, Rosenheck R, Perkins D, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New Engl J Med. 2005;353:1209–23. https://doi.org/10.1056/NEJMoa051688.
Gao K, Muzina D, Gajwani P, Calabrese J. Efficacy of typical and atypical antipsychotics for primary and comorbid anxiety symptoms or disorders: a review. J Clin Psychiat. 2016;67:1327–40.
Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiatr. 2002;47:27–38. https://doi.org/10.1177/070674370204700106.
Van Ameringen M, Pollack M. Pharmacotherapy. In: Van Ameringen M, Pollack M, editors. Generalized anxiety disorder. New York: Oxford University Press; 2012. p. 39–65.
Buckley P. Efficacy of quetiapine for the treatment of schizophrenia: a combined analysis of three placebo-controlled trials. Curr Med Res Opin. 2004;20:1357–63. https://doi.org/10.1185/030079904125004510.
Mullen J, Jibson MD, Sweitzer D. A comparison of the relative safety, efficacy, and tolerability of quetiapine and risperidone in outpatients with schizophrenia and other psychotic disorders: the quetiapine experience with safety and tolerability (QUEST) study. Clin Ther. 2001;23(11):1839–54. https://doi.org/10.1016/S0149-2918(00)89080-3.
Shayegan D, Stahl S. Atypical antipsychotics: matching receptor profile to individual patient’s clinical profile. CNS Spectrums. 2004;9(10, Supp 11):6–14. https://doi.org/10.1017/S1092852900025086.
Yatham LN, Goldstein JM, Vieta E, Bowden CL, Grunze H, Post RM, et al. Atypical antipsychotics in bipolar depression: potential mechanisms of action. J Clin Psychiat. 2005;66(Suppl 5):40–8.
Lorenz R, Jackson C, Saitz M. Adjunctive use of atypical antipsychotics for treatment-resistant generalized anxiety disorder. Pharmacotherapy. 2010;30(9):942–51. https://doi.org/10.1592/phco.30.9.942.
Katzman M, Vermani M, Jacobs L, Marcus M, Kong B, Lessard S, et al. Quetiapine as an adjunctive pharmacotherapy for the treatment of non-remitting generalized anxiety disorder: a flexible-dose open-label pilot trial. J Anxiety Disord. 2008;22(8):1480–6. https://doi.org/10.1016/j.janxdis.2008.03.002.
Simon N, Connor K, LeBeau R, Hoge E, Worthington J, Zhang W, et al. Quetiapine augmentation of paroxetine CR for the treatment of refractory generalized anxiety disorder: preliminary findings. Psychopharmacology. 2008;197(4):675–81. https://doi.org/10.1007/s00213-008-1087.
Altamura A, Serati M, Buoli M, Dell-Osso B. Augmentative quetiapine in partial/non-responders with generalized anxiety disorder: a randomized, placebo-controlled study. Int Clin Psychopharmacol. 2011;26(4):201–5. https://doi.org/10.1097/YIC.0b013e3283457d73.
Khan A, Atkinson S, Mezhebovsky I, She F, Leathers T, Pathak S. Extended-release quetiapine fumarate (quetiapine XR) as adjunctive therapy in patients with generalized anxiety disorder and a history of inadequate treatment response: a randomized, double-blind study. Ann Clin Psychiatry. 2014;25(4):7–22.
Simon N, Hoge E, Fischmann D, Worthington J, Christian K, Kinrys G, et al. An open-label trial of risperidone augmentation for refractory anxiety disorders. J Clin Psychiat. 2006;67(3):381–5.
Brawman-Mintzer O, Knapp R, Nietert P. Adjunctive risperidone in generalized anxiety disorder: a double-blind, placebo-controlled study. J Clin Psychiat. 2005;66(10):1321–5.
Pandina G, Canuso C, Turkoz I, Kujawa M, Mahmoud R. Adjunctive risperidone in the treatment of generalized anxiety disorder: a double-blind, prospective, placebo-controlled, randomized trial. Psychopharmacol Bull. 2007;40(3):42–56.
Snyderman S, Rynn M, Rickels K. Open-label pilot study of ziprasidone for refractory generalized disorder. J Clin Psychopharmacol. 2005;25(5):497–9.
Lohoff F, Etemad B, Mandos L, Gallop R, Rickels K. Ziprasidone treatment of refractory generalized anxiety disorder: A placebo-controlled double-blind study. J Clin Psychopharmacol. 2010;30(2):185–9. https://doi.org/10.1097/JCP.0b013e3181d21951.
Pollack M, Simon N, Zalta A, Worthington J, Hoge E, Mick E, et al. Olanzapine augmentation of fluoxetine for refractory generalized anxiety disorder: a placebo controlled study. Biol Psychiatry. 2006;59(3):211–5. https://doi.org/10.1016/j.biopsych.2005.07.005.
Worthington J, Kinrys G, Wygant L, Pollack M. Aripiprazole as an augmentor of selective serotonin reuptake inhibitors in depression and anxiety disorder patients. Int Clin Psychopharm. 2005;20(1):9–11.
Menza M, Dobkin R, Marin H. An open-label trial of aripirazole augmentation for treatment-resistant generalized anxiety disorder. J Clin Psychopharmacol. 2007;27(2):207–10. https://doi.org/10.1592/phco.30.9.942.
Hoge E, Bui E, Marques L, Metcalf C, Morris L, Robinaugh D, et al. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J Clin Psychiat. 2013;74(8):786–92. https://doi.org/10.4088/JCP.12m08083.
Czapinski P, Blaszczyk B, Czuczwar S. Mechanism of action of antiepileptic drugs. Curr Top Med Chem. 2005;5:3–14. https://doi.org/10.2174/1568026053386962.
Baldwin D, Ajel K. Role of pregabalin in the treatment of generalized anxiety disorder. Neuropsych Dis Treat. 2007;3(2):185–91.
Olivares J, Alvarez E, Carrasco J, Paramo M, Lopez-Gomez V. Pregabalin for the treatment of patients with generalized anxiety disorder with inadequate treatment response to antidepressants and severe depressive symptoms. Int Clin Psychopharm. 2015;30(5):265–71. https://doi.org/10.1097/YIC.0000000000000087.
Alvarez E, Olivares J, Carrasco J, Lopez-Gomez V, Rejas J. Clinical and economic outcomes of adjunctive therapy with pregabalin or usual care in generalized anxiety disorder patients with partial response to selective serotonin reuptake inhibitors. Ann Gen Psychiat. 2015;14(2):1–12. https://doi.org/10.1186/s12991-014-0040-0.
De Salas-Cansado M, Olivares J, Alvarez E, Carrasco J, Barrueta A, Rejas J. Pregabalin versus SSRIs and SNRIs in benzodiazepine-refractory outpatients with generalized anxiety disorder: a post hoc cost-effectiveness analysis in usual medical practice in Spain. Clinico Econ Outcomes Res. 2012;4:157–68. https://doi.org/10.2147/CEOR.S31102.
Rickels K, Shiovitz T, Ramey T, Weaver J, Knapp L, Micelli J. Adjunctive therapy with pregabalin in generalized anxiety disorder patients with partial response to SSRI or SNRI. Int Clin Psychopharm. 2012;27(3):142–50. https://doi.org/10.1097/YIC.0b013e328350b133.
Keck PE, Taylor VE, Tugrul KC, McElroy SL, Bennett JA. Valproate treatment of panic disorder and lactate-induced panic attacks. Biol Psychiatry. 1993;33(7):542–6. https://doi.org/10.1016/0006-3223(93)90010-B.
Kinrys G, Pollack MH, Simon NM, Worthington JJ, Nardi AE, Versiani M. Valproic acid for the treatment of social anxiety disorder. Int Clin Psychopharm. 2003;18(3):169–72. https://doi.org/10.1016/0006-3223(93)90010-B.
Otte C, Wiedemann K, Yassouridis A, Kellner M. Valproate monotherapy in the treatment of civilian patients with non-combat-related posttraumatic stress disorder: an open-label study. J Clin Psychopharmacol. 2004;24(1):106–8. https://doi.org/10.1097/01.jcp.0000106234.36344.a4.
Rosenberg G. The mechanisms of action of valproate in neuropsychiatric disorders: can we see the forest for the trees? Cell Mol Life Sci. 2007;64(16):2090–103. https://doi.org/10.1007/Fs00018-007-7079.
Vayisoglu S. Treatment response to valproate in case with generalized anxiety disorder resistant to antidepressants. Psychiatry and clinical. Psychopharmacology. 2017;27(2):207–9. https://doi.org/10.1080/24750573.2017.1317382.
Roy-Byrne P, Craske M, Sullivan G, Rose R, Edlund M, Lang A, et al. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 2010;303(19):1921–8. https://doi.org/10.1001/jama.2010.608.
Craske M, Stein M, Sullivan G, Sherbourne C, Bystritsky A, Rose R, et al. Disorder-specific impact of coordinated anxiety learning and management treatment for anxiety disorders in primary care. Arch Gen Psychiatry. 2011;68(4):378–88. https://doi.org/10.1001/archgenpsychiatry.2011.25.
Campbell-Sills L, Byrne P, Craske M, Bystritsky A, Sullivan G, Stein M. Improving outcomes for patients with medication-resistant anxiety: effects of collaborative care with cognitive behavioural therapy. Depress Anxiety. 2016;33(12):1099–106. https://doi.org/10.1002/da.22574.
Rodriguez C, Kegeles L, Levinson A, Feng T, Marcus S, Vermes D, et al. Randomized controlled crossover trial of ketamine in obsessive-compulsive disorder: proof-of-concept. Neuropsychopharmacology. 2013;38:2475–83. https://doi.org/10.1038/npp.2013.150.
Glue P, Medlicott N, Harland S, Neehoff S, Anderson-Fahey B, Nedelec M, et al. Ketamine’s dose-related effects on anxiety symptoms in patients with treatment refractory anxiety disorders. J Psychopharmacol. 2017:1–4. https://doi.org/10.1177/0269881117705089.
• Patterson B, Van Ameringen M. Augmentation strategies for treatment-resistant anxiety disorders: a systematic review and Meta-Analysis. Depress Anxiety. 2016;33:728–36. https://doi.org/10.1002/da.22525. An up to date meta-analysis of treatment resistant anxiety disorders, including GAD.
Koen N, Stein D. Pharmacotherapy of anxiety disorders: a critical review. Dialog Clin Neurosci. 2011;13(4):423–37.
Mitte K. Meta-analysis of cognitive-behavioural treatments for generalized anxiety disorder: a comparison with pharmacotherapy. Psychol Bull. 2005;131(5):785–95. https://doi.org/10.1037/0033-2909.131.5.785.
• Bandelow B, Reitt M, Rover C, Michaelis S, Gorlich Y, Wedekind D. Efficacy of treatments for anxiety disorders: a meta-analysis. Int Clin Psychopharm. 2015;30:183–92. https://doi.org/10.1097/YIC.0000000000000078. Unique meta-analysis which compares psychological and pharmacological treatments for the anxiety disorders, includes sub-analyses for each disorder examined.
Power K, Simpson R, Swanson V, Wallace L. A controlled comparison of cognitive-behaviour therapy, diazepam, and placebo, alone and in combination, for the treatment of generalised anxiety disorder. J Anxiety Disord. 1990;4:267–92. https://doi.org/10.1016/0887-6185(90)90026-6.
Crits-Christoph P, Newman M, Rickels K, Gallop R, Gibbons M, Hamilton J, et al. Combined medication and cognitive therapy for generalized anxiety disorder. J Anxiety Disord. 2011;25(8):1087–94. https://doi.org/10.1016/j.janxdis.2011.07.007.
Patterson B, Van Ameringen M, Pollack MH. Clinical features of GAD. In: Van Ameringen M, Pollack MH, editors. Generalized anxiety disorder. New York: Oxford University Press; 2012. p. 13–28.
Reinhold J, Mandos L, Rickels K, Lohoff F. Pharmacological treatment of generalized anxiety disorder. Exp Opin Pharmaco. 2011;2011(12):2457–67. https://doi.org/10.1517/14656566.2011.618496.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Michael Van Ameringen reports personal fees from Purdue, Allergan, and Lundbeck and grants from Janssen-Ortho, Pfizer, and Shire, outside the submitted work.
Beth Patterson, Jasmine Turna, Amy Pipe, and Hajer Nakua declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Anxiety, Obsessive Compulsive, and Related Disorders
Rights and permissions
About this article
Cite this article
Van Ameringen, M., Patterson, B., Turna, J. et al. The Treatment of Refractory Generalized Anxiety Disorder. Curr Treat Options Psych 4, 404–417 (2017). https://doi.org/10.1007/s40501-017-0129-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40501-017-0129-6