Opinion Statement
Purpose In this article, we present data incorporating heart rate variability (HRV) into a graded virtual reality protocol performed in both a combat environment and an active control (classroom) environment, for combat Veterans with and without PTSD.
Recent Findings Exposure therapy for PTSD has proven effective. There is increasing interest in the use of virtual reality exposure therapy (VRET)-customized environments incorporating auditory, visual, and olfactory sensory modalities, to augment exposure-based treatment for PTSD. Particularly for combat Veterans, VRET may offer the advantage of a more realistic in vivo exposure for treatment. When combined with concurrent psychophysiological data, VRET has the potential to inform PTSD diagnosis, predict therapeutic responsiveness, and provide objective indicators of treatment response. HRV was not different between Veteran with and without PTSD, but our group recently found that Veterans with PTSD had differential skin conductance responses compared with Veterans without PTSD.
Summary Virtual reality is a promising treatment for PTSD. Methodological factors may have influenced the absence of significant findings in the current data. Future research which optimizes the potential use of psychophysiological assessments for the development of biomarkers and prediction of PTSD treatment response, or to inform the process of PTSD treatment, remain important.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment
The lifetime prevalence of posttraumatic stress disorder (PTSD) in the general US adult population is estimated to be 6.8% [1]. Estimates among Veterans range from 30.9 to 18.7% in Vietnam-era Veterans [2]. Virtual reality exposure therapy (VRET) is growing as a treatment for posttraumatic stress disorder. VRET is relatively new, with the first case studies appearing in the treatment of Vietnam Veterans in 1999 and 2001 [3, 4]. The potential to utilize VRET for the benefit of a large number of Iraq and Afghanistan Veterans returning with PTSD was recognized early [5]. This, coupled with advances in VR technology, contributed to the proliferation of VRET as a treatment modality for PTSD.
Accumulating evidence supports the efficacy of VRET for PTSD treatment [6,7,8,9,10], and an additional advantage of VRET is the ability to tailor exposure to the individual. A recent meta-analysis suggests that VRET provides benefits similar to in vivo exposure with generalizable gains that can impact participant quality of life [11]. Additionally, data from Veterans undergoing PTSD treatment suggests VRET is well tolerated [12]. While combat Veterans in the Department of Veterans Affairs (VA) have benefitted from this innovation in treatment, additional biomarker data are needed to optimize VRET for individual patients and to understand the mechanisms of therapeutic action.
Heart rate variability
Heart rate variability (HRV) is a candidate psychophysiologic biomarker with potential to inform differential diagnosis, endophenotyping, or prediction of VRET effectiveness or other health outcomes in PTSD. HRV refers to beat-to-beat variability in heart rate as represented by the R-R interval in the electrocardiogram (Fig. 1). HRV is governed by the balance between sympathetic and parasympathetic outflow in the autonomic nervous system (ANS; [13, 14]) and can provide insight about central nervous system (CNS) function. Changes in HRV are clinically relevant, in that, reduced HRV has been associated with cardiovascular disease and adverse health-related outcomes [13]. HRV is particularly relevant to PTSD because this disorder is characterized by hyperarousal and increased autonomic reactivity to stimuli [15]. While HRV is transiently reduced during times of acute stress, anxiety, or emotional strain in healthy individuals [16, 17], PTSD has been associated with sustained reductions in HRV [18,19,20,21] at rest, suggesting a chronic sympathetic autonomic predominance. Recently, resting pre-deployment HRV demonstrating a relative sympathetic autonomic predominance was found to be associated with increased risk of post-deployment development of PTSD in the Marine Resiliency Study [22•]. Reduced HRV may also have negative health effects, suggested by findings that lower HRV in response to emotional scripts predicted impaired arterial function (an index of cardiovascular health) in relatively young Veterans [23].
When examining HRV, several indices can be calculated from the electrocardiogram and used to characterize the sympathovagal balance. Time-domain indices and frequency-domain indices impart information regarding components of autonomic control. Specifically, low-frequency HRV is indicative of sympathetic autonomic tone, while high-frequency HRV largely reflects parasympathetic tone [13]. The relative predominance of activity in these frequency bands provides insight into the balance between sympathetic and parasympathetic activity at a given point in time. Furthermore, low- and high-frequency power can be normalized to allow for comparisons between individuals or groups. The standard deviation of the R-R interval can be used as a global index of total HRV over a fixed recording time and compared between treatment conditions or portions of a protocol.
Our group recently found that sympathetic autonomic activity, as measured by galvanic skin response during a graded VR exposure, discriminated between combat Veterans with PTSD and those without [24••]. This finding underscored the notion that psychophysiologic data are useful for the evaluation of PTSD patients during times of heightened arousal or pathological sympathetic regulation, such as that experienced during VRET. Only two prior studies have examined HRV during VR, and these were confined to the study of cardiovascular responses to social stress or anxiety-provoking situations [25, 26]. No prior work on this topic has examined HRV during VR involving graded exposure stimuli with PTSD patients.
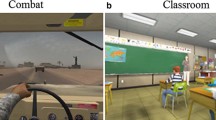
The purpose of the present study was to examine the HRV response of combat Veterans with and without PTSD to a series of combat-related VR events as well as to non-combat VR stimuli (classroom scenes). The classroom scenes were included to control for potential autonomic responses to neutral stimuli of increasing complexity in the virtual environment, in comparison with VR combat stimuli. We hypothesized that the PTSD group would demonstrate reductions in HRV (increased sympathetic autonomic predominance) compared to the non-PTSD group during combat scenes, and no difference during classroom scenes.
Methods
Participants
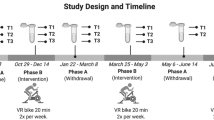
Nineteen adult Veterans with PTSD and 24 non-PTSD Veteran controls were recruited from the Providence, RI VA Medical Center (VAMC) where the study was performed. Treatment (psychopharmacology or therapy) is not provided in the suite where the VR equipment resides, and therefore, no participants were acclimated to the study environment specifically. All had combat exposure during operations in Iraq or Afghanistan, and PTSD patients were required to be currently engaged in treatment. Demographic and clinical data are presented in Table 1. Participants with an abnormal electrocardiogram and those taking benzodiazepines, beta-blockers, or alpha-2 agonists were excluded. PTSD diagnosis and symptom severity were evaluated using the Clinician-Administered PTSD Scale (CAPS; [27]) and the Structured Clinical Interview of DSM Disorders (SCID; [28]).
Virtual reality
Participants were randomized with regard to order of VR content (i.e., combat scenes or classroom scenes first) and a 5-min baseline period preceded each battery of scenes. VR content was delivered with visual, auditory, haptic, and olfactory stimuli in the combat scenarios, presented as six 1-min scenes which increased progressively in intensity with each scene (Table 2). Neutral, non-combat VR stimuli comprised a series of six 1-min classroom scenes, with visual and auditory stimuli that increased in complexity over time (Table 2). Between scenes, Veterans sat quietly for 2 min while wearing VR equipment and viewed a blank screen.
HRV
Electrocardiogram data were continuously acquired during the 5-min baseline and 15-min VR exposure + rest trials using a single-lead electrocardiogram, with one electrode positioned at approximately the 4th intercostal space to the right of the sternum and the other on the left wrist (Biopac Systems Inc., Goleta, CA). All data processing steps were done offline using specialized software to exclude ectopic beats and generate the HRV indices of interest (LabChart 8, ADI Instruments, Colorado Springs, CO). Activity in low-frequency (0.04 to 0.15 Hz) and high-frequency (0.15 to 0.4 Hz) HRV bands were analyzed in normalized units (LFnu) as well as the ratio between low- and high-frequency power (LF/HF) calculated by LabChart 8 software. A global measure of HRV, the standard deviation of the R-R intervals of the electrocardiogram (SDRR), was also calculated by the software.
Data analyses
Baseline HRV data, acquired with participants at rest while wearing the VR headset at the beginning of each session, were averaged across the 5-min baseline period preceding the start of VR stimuli. HRV data during VR stimuli were averaged across the 1-min stimuli periods. Data were analyzed using SPSS software (IBM corporation, Armonk, NY). Demographic and HRV indices during baseline were compared between PTSD and non-PTSD groups using chi-square or independent sample t tests, as appropriate. Group differences on HRV indices during combat and classroom VR scenarios were tested using a 6 (Scenario: 1–6) × 2 (VR content: combat vs classroom) × 2 (Group: PTSD vs non-PTSD) repeated measures ANCOVA, with Scenario and VR content as a within subject variable and Group as a between subject variable. Baseline HRV indices were entered as covariates. In cases where sphericity cannot be assumed, a Greenhouse-Geisser correction was performed. Pearson correlations were used to investigate potential associations between baseline HRV measures and PTSD symptoms based on total CAPS score. A Bonferroni correction was applied to this analysis to adjust the significance threshold appropriately given the number of correlations (.05/12 = .004).
Results
SDRR
Repeated measures ANCOVA demonstrated no significant main effect of Scenario (F(1.26,49.25) = .52, p = .76), suggesting that SDRR did not change over the VR scenarios. There was also no significant main effect of VR content (F(1,39) = .97, p = .33) suggesting that SDRR did not differ across all combat versus classroom scenes. Neither was there a significant main effect of Group (F(1,39) = .36, p = .55), demonstrating that Veterans with and without PTSD did not differ from each other on SDRR across all classroom and combat VR scenarios. Finally, none of the interactions between VR content, Scenario or Group (2-way or 3-way) were significant, all p > .05.
LFnu
A repeated measures ANCOVA demonstrated a significant main effect of Scenario on LFnu (F(5,35) = 2.67, p = .04), suggesting that LFnu increased over the course of the six VR classroom and combat scenarios. There was no significant main effect of VR content (F(1,39) = .02, p = .88), suggesting that LFnu in response to all six VR classroom scenarios did not differ from all six combat VR scenarios. Again, there was also no significant main effect of Group (F(1,39) = .33, p = .57), suggesting there were no significant differences on LFnu between PTSD and non-PTSD groups across scenes. Neither were any of the 2- or 3-way interactions significant, all p > .05.
LF/HF
Finally, for LF/HF, repeated measures ANCOVA revealed a non-significant main effect of Scenario (F(1.06,41.25) = .47, p = .79), suggesting no effect of increasing complexity of VR scenario on LF/HF. Neither was there a significant main effect of VR content (F(1,39) = .27, p = .61), again demonstrating no effect of VR combat or VR classroom content on LF/HF. Lastly, the main effect of Group was also non-significant (F(1,39) = 1.10, p = .30) as were all 2- and 3-way interactions, all p > .05, suggesting no differences in LF/HF as a function on PTSD, VR content, or increasing complexity.
Association between baseline HRV and PTSD symptoms
There were no significant correlations between any baseline HRV indices (SDRR, LFnu, LF/HF) and total CAPS score. For the PTSD group, correlations between total CAPS score and baseline SDRR, LFnu, and LF/HF prior to classroom scenes were r = .25, p = .31; r = .42, p = .08; r = .29, p = .22, respectively, and prior to combat scenes were r = .28, p = .25; r = .08, p = .76; r = .26, p = .40. Correlational analyses for the non-PTSD group between total CAPS scores and baseline SDRR, LFnu, and LF/HF prior to classroom scenes revealed r = −.03, p = .90; r = .27, p = .19; r = .08, p = .67, respectively, and prior to combat scenes r = .18, p = .39; r = .03, p = .89; r = .07, p = .73, respectively.
Discussion
The results did not support our hypothesis that the Veterans in the PTSD group would demonstrate a pattern of reduction in HRV, indicative of greater sympathetic autonomic tone, as compared to non-PTSD Veterans when exposed to graded combat-related VR scenes. HRV assessments typically require an epoch longer than 1-min to reflect changes in autonomic regulation, as sufficient beats to perform reliable analyses (≥100 beats [13]) generally requires, a minimum of 2 min. Although the current protocol was therefore not optimized to detect changes in HRV, our results demonstrate that the acquisition of these data during graded VR is feasible. We evaluated this duration of VR presentation because during VRET, this might be the most sensitive window to examine psychophysiology, including HRV. However, 1 min may not be sufficient to provide an adequate amount of data for valid assessment. Hence, the absence of group difference within this dataset might be truly due to no differences between groups on HRV variables, or due to limited data collection time window for analyses. It is at this point not possible to distinguish these two potential reasons.
Recent work by our lab has elucidated the relationship between skin conductance and graded VR stimuli in these same participants [24••]. Skin conductance is regulated by the sympathetic autonomic nervous system, and changes may be seen on a shorter time scale than is required to reliably determine HRV responses. In these same participants, the PTSD group demonstrated skin conductance responses indicative of a more robust sympathetic autonomic response to combat scenes as compared with classroom scenes. These findings suggest that the collected HRV indices did not reveal differences in autonomic outflow and regulation in a graded protocol in Veterans with versus without PTSD as acquired in the present study. These negative data are informative for the development of potential biomarkers of VR treatment, and at least one prior study reported similar findings. Wilhelm et al. [29] examined heart rate and skin conductance responses to graded height exposure in participants reporting high or low levels of fear of heights. Utilizing a protocol with a very similar time course to the present study, the authors found that skin conductance responses, but not heart rate, differed between the two groups. While Wilhelm et al. did not examine HRV specifically, the same autonomic outflow that governs changes in HRV is also operant in the regulation of heart rate.
On the other hand, the work by Costanzo et al. (2014) showed significant psychophysiological responses to a virtual combat environment in a group of sub-clinical PTSD participants, with heart rate demonstrating the strongest correlation to Clinician-Administered PTSD Scale global symptoms [30•]. While heart rate variability was not calculated in the Costanzo study, the heart rate response in the subthreshold PTSD population suggests a significant change in sympathovagal balance during virtual combat environment exposure. Our non-PTSD comparison group had a mean CAPS score of 26 while subthreshold PTSD participants in the Costanzo study had a mean score of 31.4. Thus, it is possible that physiologic changes associated with subthreshold symptoms in our non-PTSD comparison group contributed to the lack of separation between groups. Categorical diagnostic approaches based on tools such as the CAPS may not capture more nuanced physiologic changes occurring across a broad spectrum of symptoms.
Conclusion
VRET is a promising approach for the treatment of PTSD, and combat Veterans have great potential to benefit from this as a therapeutic modality. Although HRV can provide important information on autonomic function and regulation, these results suggest that it is not an informative biomarker for a graded VR protocol of this design. While the findings of this study were negative, they can inform future efforts to integrate psychophysiological data collection into treatment and research protocols. Such efforts are important for the development of objective measures of treatment response, as well as biomarkers for the prediction of treatment response among those afflicted with PTSD.
References and Recommended Reading
Recently published papers of particular interest have been highlighted as:• Of importance,•• Of major importance
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602.
Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science. 2006;313(5789):979–82.
Rothbaum BO, Hodges L, Alarcon R, Ready D, Shahar F, Graap K, et al. Virtual reality exposure therapy for PTSD Vietnam veterans: a case study. J Trauma Stress. 1999;12(2):263–71.
Rothbaum BO, Hodges LF, Ready D, Graap K, Alarcon RD. Virtual reality exposure therapy for Vietnam veterans with posttraumatic stress disorder. J Clin Psychiatry. 2001;62(8):617–22.
Rizzo A, Pair J, McNerney PJ, Eastlund E, Manson B, Gratch J, et al. Development of a VR therapy application for Iraq war military personnel with PTSD. Stud Health Technol Inform. 2005;111:407–13.
Botella C, Serrano B, Banos RM, Garcia-Palacios A. Virtual reality exposure-based therapy for the treatment of post-traumatic stress disorder: a review of its efficacy, the adequacy of the treatment protocol, and its acceptability. Neuropsychiatr Dis Treat. 2015;11:2533–45.
Goncalves R, Pedrozo AL, Coutinho ES, Figueira I, Ventura P. Efficacy of virtual reality exposure therapy in the treatment of PTSD: a systematic review. PLoS One. 2012;7(12):e48469.
McLay RN, Wood DP, Webb-Murphy JA, Spira JL, Wiederhold MD, Pyne JM, et al. A randomized, controlled trial of virtual reality-graded exposure therapy for post-traumatic stress disorder in active duty service members with combat-related post-traumatic stress disorder. Cyberpsychol Behav Soc Netw. 2011;14(4):223–9.
Miyahira SD, Folen RA, Hoffman HG, Garcia-Palacios A, Spira JL, Kawasaki M. The effectiveness of VR exposure therapy for PTSD in returning warfighters. Stud Health Technol Inform. 2012;181:128–32.
Reger GM, Holloway KM, Candy C, Rothbaum BO, Difede J, Rizzo AA, et al. Effectiveness of virtual reality exposure therapy for active duty soldiers in a military mental health clinic. J Trauma Stress. 2011;24(1):93–6.
Morina N, Ijntema H, Meyerbroker K, Emmelkamp PM. Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments. Behav Res Ther. 2015;74:18–24.
Kramer TL, Savary PE, Pyne JM, Kimbrell TA, Jegley SM. Veteran perceptions of virtual reality to assess and treat posttraumatic stress disorder. Cyberpsychol Behav Soc Netw. 2013;16(4):293–301.
Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996;93(5):1043–65. doi:10.1161/01.CIR.93.5.1043
Laborde S, Mosley E, Thayer JF. Heart rate variability and cardiac vagal tone in psychophysiological research—recommendations for experiment planning, data analysis, and data reporting. Front Psychol. 2017;8:213.
Bedi US, Arora R. Cardiovascular manifestations of posttraumatic stress disorder. J Natl Med Assoc. 2007;99(6):642–9.
Chalmers JA, Heathers JA, Abbott MJ, Kemp AH, Quintana DS. Worry is associated with robust reductions in heart rate variability: a transdiagnostic study of anxiety psychopathology. BMC Psychol. 2016;4(1):32.
Fisher AJ, Newman MG. Heart rate and autonomic response to stress after experimental induction of worry versus relaxation in healthy, high-worry, and generalized anxiety disorder individuals. Biol Psychol. 2013;93(1):65–74.
Liddell BJ, Kemp AH, Steel Z, Nickerson A, Bryant RA, Tam N, et al. Heart rate variability and the relationship between trauma exposure age, and psychopathology in a post-conflict setting. BMC Psychiatry. 2016;16:133.
Shah AJ, Lampert R, Goldberg J, Veledar E, Bremner JD, Vaccarino V. Posttraumatic stress disorder and impaired autonomic modulation in male twins. Biol Psychiatry. 2013;73(11):1103–10.
Hauschildt M, Peters MJ, Moritz S, Jelinek L. Heart rate variability in response to affective scenes in posttraumatic stress disorder. Biol Psychol. 2011;88(2–3):215–22.
Tan G, Dao TK, Farmer L, Sutherland RJ, Gevirtz R. Heart rate variability (HRV) and posttraumatic stress disorder (PTSD): a pilot study. Appl Psychophysiol Biofeedback. 2011;36(1):27–35.
• Minassian A, Maihofer AX, Baker DG, Nievergelt CM, Geyer MA, Risbrough VB, et al. Association of predeployment heart rate variability with risk of postdeployment posttraumatic stress disorder in active-duty marines. JAMA Psychiatry. 2015;72(10):979–86. This study established the association between heart rate variability and posttraumatic stress disorder. Their results suggest heart rate variability may have potential as a biomarker for identifying those at risk for development of postraumatic stress disorder after trauma exposure
Clausen AN, Aupperle RL, Sisante JF, Wilson DR, Billinger SA. Pilot investigation of PTSD, autonomic reactivity, and cardiovascular health in physically healthy combat veterans. PLoS One. 2016;11(9):e0162547.
•• van’t Wout M, Spofford CM, Unger WS, Sevin EB, Shea MT. Skin conductance reactivity to standardized virtual reality combat scenes in veterans with PTSD. Applied Psychophysiology and Biofeedback. 2017; doi:10.1007/s10484-017-9366-0. This study demonstrates differences in skin conductance responses to virtual reality combat exposure between groups of Veterans with and without posttraumatic stress disorder. These results suggest skin conductance may be a viable biomarker for use during treatment, to discriminate between patient groups and substantiates posited differences in autonomic regulation between those with and without posttraumatic stress disorder
Cristea IA, Valenza G, Scilingo EP, Szentagotai Tatar A, Gentili C, David D. Autonomic effects of cognitive reappraisal and acceptance in social anxiety: evidence for common and distinct pathways for parasympathetic reactivity. J Anxiety Disord. 2014;28(8):795–803.
Jonsson P, Wallergard M, Osterberg K, Hansen AM, Johansson G, Karlson B. Cardiovascular and cortisol reactivity and habituation to a virtual reality version of the Trier Social Stress Test: a pilot study. Psychoneuroendocrinology. 2010;35(9):1397–403.
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8(1):75–90.
Spitzer RL, Williams JB, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID). I: history, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–9.
Wilhelm FH, Pfaltz MC, Gross JJ, Mauss IB, Kim SI, Wiederhold BK. Mechanisms of virtual reality exposure therapy: the role of the behavioral activation and behavioral inhibition systems. Appl Psychophysiol Biofeedback. 2005;30(3):271–84.
• Costanzo ME, Leaman S, Jovanovic T, Norrholm SD, Rizzo AA, Taylor P, et al. Psychophysiological response to virtual reality and subthreshold posttraumatic stress disorder symptoms in recently deployed military. Psychosom Med. 2014;76(9):670–7. This paper demonstrates a link between sub-clinical posttraumatic stress disorder and psychophysiologic responses to a virtual reality combat environment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Carpenter reports personal fees from the Brown Department of Psychiatry and Human Behavior, during the conduct of the study.
Dr. Philip reports grants from the US Dept. of Veterans Affairs, during the conduct of the study.
Samuel J. Ridout declares that he has no conflict of interest.
Christopher M. Spofford declares that he has no conflict of interest.
Mascha van’t Wout-Frank declares that she has no conflict of interest.
William S. Unger declares that he has no conflict of interest.
Audrey R. Tyrka declares that she has no conflict of interest.
Tracie Shea reports grants from the US Dept. of Veterans Affairs, during the conduct of the study.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Funding/Disclosures
This work was supported by U.S. Department of Defense W81XWH-07-1-0689, R25 MH101076 (SJR) and IK2 CX000724 (NSP). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or National Institutes of Health. The authors report no relevant conflicts of interest.
Additional information
This article is part of the Topical Collection on Post-Traumatic Stress Disorders
Rights and permissions
About this article
Cite this article
Ridout, S.J., Spofford, C.M., van’t Wout-Frank, M. et al. Heart Rate Variability Responses to a Standardized Virtual Reality Exposure in Veterans with PTSD. Curr Treat Options Psych 4, 271–280 (2017). https://doi.org/10.1007/s40501-017-0118-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40501-017-0118-9