Abstract
Purpose of Review
Why around 5% of Trypanosoma cruzi–infected pregnant women transmit the parasite to their offspring whereas 95% do not? Answers to this main question are needed in order to improve the programs aiming to control or eliminate congenital Chagas disease (CCD), which has become an important global public health problem.
Recent Findings
Turnover of syncitiotrophoblast as a new innate defense mechanism of placenta and analyses of transcriptomic responses of placental genes and of new parasite DNA sequences have allowed a re-evaluation of the relationship between parasite diversity, placental tropism, and CCD transmission.
Summary
A synthetic view of the gradual interactions between the human placenta facing up the parasites present in the maternal blood and the occurrence and severity of CCD is proposed. Further researches on the role of parasite molecular diversity, maternal microbiomes, transfers of parasite and placenta exovesicles, and genetic features of infected mothers should improve our understanding of such maternal-fetal complex relationship.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital Chagas disease (CCD), caused by maternal-fetal/neonatal transmission of the parasite Trypanosoma cruzi, is frequently a silent disease with potential long-term consequences. It results from complex interactions between the parasite (virulence), the strengths and weaknesses of the placental barrier and of maternal and fetal/neonatal immune responses [1, 2••, 3••]. The present review will focus on such interactions highlighting mainly the central role of human placenta.
Congenital Chagas Disease at a Glance
CCD can arise in both acute and chronic phases of maternal infection, be recurrent at each pregnancy (i.e., during all the fertile period of woman life), and occur from one generation to another. This pattern of transmission, leading to family clustering of congenital transmission cases, facilitates uncontrolled spread of Chagas disease (CD) over time. So CCD remains an important global and neglected public health problem [1, 2••, 3••].
WHO estimates that 1,125,000 women in fertile age are infected with T. cruzi with an incidence of congenital infection of 8668 cases/year in the 21 Latin American countries where CD is currently endemic (with nearly 50% of CCD cases grouped in Mexico, Argentina, and Colombia) [4]. Most cases of congenital infection are derived from mothers infected by insect vectors since childhood by residing in endemic areas. The mean maternal-fetal transmission rate in chronic CD (the most frequent phase of infection) in Latin America is estimated to 4.7% [5]. Congenital transmission would be responsible for 22.5% of new annual infections in countries having controlled domestic vector infestation [4, 6]. Migrations of Latin American people have promoted CD as a global disease, now observed in non-endemic areas. Thereby, cases of CCD were reported mainly in Spain, but also in Italy, Sweden, Switzerland, USA, Canada, and Japan. The congenital route is the main transmission mode of T. cruzi in non-endemic areas, over blood transfusions and organ transplantations [2••, 7, 8]. Historically, CCD was associated with high levels of neonatal morbidity and mortality, while nowadays it is clear that most cases are asymptomatic. Some CCD cases can present non-specific symptoms (fever, low birth weight, prematurity, hepato-splenomegaly, pneumonitis, premature rupture of membranes), as seen in other intrauterine or perinatal infections (like Toxoplasma gondii, Treponema pallidum, rubella virus, cytomegalovirus, HIV, herpes simplex virus, and parvovirus infections). Sometimes, neonatal pejorative outcomes, including neonatal death, can be observed, particularly in case of acute or reactivated infections (as in maternal coinfection with HIV) [2••].
Congenital T. cruzi infection is an acute infection in newborns that can be efficiently treated with anti-parasitic therapy before 1 year of age, which justifies the use of accurate and sensitive laboratory diagnostic tools [9••]. When left untreated, the infection can progress to chronic CD later in life (susceptible to induce myocardiopathy or digestive megaviscera) with a drop in the cure rate. Moreover, untreated girls may transmit the infection to their offspring when reaching reproductive age.
Strengths and Weaknesses of the Placental Organ Facing Pathogens
Whether fetal contamination with parasites coming from amniotic fluid or uterine wall and/or eventually by breast feeding remains a possibility in acute or reactivated infection, these routes are unlikely in the most frequent maternal chronic infection [2••]. Placenta is therefore the key fetal organ facing the parasites present in the maternal blood within the intervillous space and from which transmission depends on. Such a route requires parasites to cross or skirt two main placental lines of defense.
Chorionic villi of the human placenta floating in the maternal intervillous blood are covered by the trophoblast (the first placental line of defense). It is a lining epithelium formed by two layers of cells: an outer layer called syncytiotrophoblast (deprived of intercellular junctions) and an inner proliferative and germinative layer termed cytotrophoblast. Trophoblast cells also cover non-villous structures (e.g., the chorionic plate) and migrate from the placenta into the uterine wall. To a great degree, only the syncytiotrophoblast is interposed between maternal blood and fetal tissues, since the cytotrophoblast cell number decreases during the gestation period [10]. The trophoblast is separated from the fetal connective tissue of the villous stroma that contains the fetal capillaries by a basal membrane. The basal membrane and the villous stroma are formed by a fibrinoid extracellular matrix (ECM) composed mainly by fibronectin, collagen, and laminin. Both constitute the second placental line of defense [10]. So, the trophoblast, the basal membrane, and the villous stroma constitute a physical barrier to pathogens present in maternal blood [11, 12] (Fig. 1). However, such placental barrier displays some weaknesses since some areas are not covered by trophoblast, such as the marginal zone joining the membranes to the chorionic and basal plates. The latter is constituted with smooth muscle cells embedded in an ECM, but only covered by a non-trophoblastic epithelium of both maternal and fetal origin [13, 14].
Strengths and weaknesses of the placental organ. The placenta is composed of a maternal side facing the uterus and the fetal side where the umbilical cord (UC) emerges from the chorionic plate (CP). At the marginal region of the placenta, the amniotic membrane (AM) joints the CP and the basal plate (BP). The placental barrier is located at the chorionic villi, where the first line of defense against pathogens is formed by the syncytiotrophoblast (STB), the superficial layer of the trophoblast in direct contact with the maternal blood (MB) and the cytotrophoblast (CTB), the germinative basal layer of this epithelium. The trophoblast undergoes a continuous epithelial turnover (TTO), where the CTB proliferates, then fuses into the STB (dashed cell limits) and apoptotic knots (AK) are released into the MB. The second line of defense is formed by the basal membrane (BM) that separates the trophoblast from the underlining villous stroma (VS), i.e., the fetal connective tissue that contains the fetal blood vessels (FBV). However, the marginal zone (MZ), located where CP and BP joints, constitutes a weakness of the placenta defenses, since the MZ is only covered by a non-trophoblastic epithelium of both maternal and fetal origin and is formed by smooth muscle cells embedded in extracellular matrix
The placenta is also an active immunological organ able to initiate an innate immune response. It can release pro-inflammatory cytokines, chemokines, reactive oxygen and nitrogen intermediates (NO), and anti-microbial peptides [12, 15], through trophoblast-expressed Toll-like receptors (TLRs) recognizing pathogen-associated molecular patterns (PAMPs) [16, 17]. Another facet of the placental innate immune response is the continuous turnover of the trophoblast epithelium (and the subsequent fusion of cytotrophoblast), resulting in the removing of attached pathogen to the superficial cell layer. This has been initially shown in T. cruzi infection (see below) [3••, 18,19,20] and associated also to resistance to viral infections [11].
Maternal-Fetal Transfers Relevant to T. cruzi Infection
Whether fetal T. cruzi infection results primarily from the transplacental transmission of parasites, transmission of other molecules can also be relevant for the development of CCD, through modulation of the fetal/neonatal immune responses (maternal imprinting/priming; see below).
Blood Parasite Amounts in Mothers and Neonates
Parasitemia during pregnancy is a key factor for congenital transmission. Although it slightly increases during pregnancy (on second and third trimesters [21]), congenital transmission rate is on average 4.7% during chronic infection, occurring mainly in women displaying around 10–20 parasites (p)/mL (i.e., 10–20 times higher than in non-transmitting women) [5, 22,23,24,25,26,27]. However, this transmission rate jumps to 54% of reported cases of acute infection [28, 29] and 100% in reactivated CD (in case of coinfection with HIV), i.e., in pregnant women displaying extremely high parasitemias [2••, 30, 31].
On the other side, parasitemias at birth (umbilical cord) can be lower, similar or higher than in mothers (up to over 60,000 p/mL). In some cases, parasites are more easily detectable weeks or months after birth. Neonatal parasitic loads increase up to 1–3 months after birth, before decreasing as infection enters in the chronic phase. Indeed, morbidity and mortality of CCD are associated with the highest neonatal parasitemias [2••, 26, 32, 33].
Transfer of Maternal IgG Antibodies
The transplacental transfer of maternal IgG through the receptors for the Fc portion of immunoglobulins (FcRn) expressed on trophoblast [34, 35] occurs in CD (with levels and repertoire of T. cruzi–specific-antibodies similar to those of their mothers) as in other infections [36,37,38]. Such transferred antibodies can persist up to 8–9 months after birth [9••, 33, 39].
Transfer of Other Bio-Relevant Molecules
Parasitic-circulating antigens (excreted and secreted), parasitic-breakdown molecules with pro-inflammatory activity, and/or antigen surrogates (such as antibody idiotypes) are likely transferred through the placenta, as suggested in human and experimental infections with T. cruzi [37, 40, 41].
This is probably also the case for parasitic-breakdown DNA [42,43,44]. Indeed, transmission of circulating cell-free DNA, as well as transmission of maternal cells (microchimerism) to fetuses is known to occur in normal pregnancy and such cells can persist into adulthood [45, 46]. T. cruzi infection in pregnant women stimulates the production of pro-inflammatory cytokines [47], whose IL-6 can be transferred to fetus [48]. All these molecules and antibodies can modulate the fetal/neonatal responses to transmitted parasites.
Interactions Between T. cruzi and Human Placenta
Ex Vivo/In Vitro Interactions Between T. cruzi and Placenta
Ex vivo studies show the inhibiting role of placental subfractions on trypomastigote infectivity [49] and the slow multiplication of parasites in villous explants and their killing by NO produced by placental cells [50, 51], arguing for an activation of placental innate defenses in the presence of a limited amount of parasites. Indeed, in such experiments of ex vivo infection of placental explants, only few parasite antigens and DNA can be detected [50,51,52] and the typical amastigote nests are not observed. Other studies show that low concentrations of parasites incubated with placental explants or a trophoblastic cell line (BeWo®) induce a cell proliferation, followed by cell differentiation and finally cell death by forming apoptotic knots, related to the epithelial turnover of the syncytiotrophoblast clearing parasites out of the placental environment [3••, 18,19,20, 53]. The placental TLR-2 and caspase 8 activity are involved in the T. cruzi–induced epithelial turnover of trophoblast [54, 55]. In addition, T. cruzi induces a significant increase in TLR-2 and TLR-4 protein expression and of pro-inflammatory cytokines in ex vivo infected placental explants [54]. It has been also shown that parasites increase placenta-derived exosomes in human placental explants [3••, 56], but their role remains to be investigated (see below).
By contrast, high concentrations of parasites induce massive destruction of the trophoblast during ex vivo infection of placental explants [52]. During infection, T. cruzi calreticulin, expressed on the parasite surface, acts as virulence factor since it binds maternal classical complement component C1q that recognizes human calreticulin in placenta. The interaction of human and parasite calreticulin with C1q facilitates the parasite infection [57, 58]. Placental alkaline phosphatase is also used by the parasite to facilitate the infection [59]. During invasion, T. cruzi also induces a dis-assembly of actin cytosqueleton in the trophoblast [60] and modulates several signal transduction pathways, including the ERK1/2 MAPK (Mitogen activated protein kinases) and PLC-γ (Phospholipase C-gamma) pathways [61]. In addition, T. cruzi can activate placental matrix metalloproteinases (MMP-2 and MMP-9) which favors placental barrier degradation [62, 63].
Histopathologic Studies of Placentas from T. cruzi–Infected Versus Uninfected Neonates
In past studies of placentas of severe and mortal cases of CCD (rarely observed today), a severe placentitis/villitis occurs with large areas of trophoblast destruction and necrosis. Amastigote parasites are found in villous trophoblast and stromal cells [64, 65]. Immunohistochemical studies show important inflammatory responses in such placentas, with infiltrates mainly composed of CD68+ macrophages, CD8+ T lymphocytes and few natural killer (NK) cells, and an intense production of TNF-α [66].
In placentas of live neonates suffering mild congenital T. cruzi infection (frequent today), villitis is much less marked or not observed (despite some degree of reorganization of extracellular matrix). Parasites are not or hardly identified in the chorionic villi. Necrosis and lysis associated with infiltration of neutrophils and lymphocytes are more frequently detected in chorionic plate and membranes surrounding the fetus (chorioamnionitis) and umbilical cord (funisitis) [66, 67]. Similar results were found by using immunohistochemical and histochemical methods, showing slight destruction of the trophoblast and villous stroma, selective disorganization of the basal lamina, and disorganization of collagen I in the villous stroma [63, 66]. In serial biopsies performed in 19 placentas from infected live Bolivian newborns, an unexpected high density of parasites was observed at the level of marginal zone, joining the membranes to the chorionic and basal plates, with gradually decreasing densities in the chorionic plate and distant membranes. Infection of amniotic cells could be observed (likely occurring by contiguity with the membrane chorion) [2••, 68]. However, the release of parasites into amniotic fluid seems a rather rare event, suggesting that amniotic fluid is probably not contributing to parasite transmission to the fetus (see above) and not helpful for diagnosing congenital infection [69].
Histopathology of placentas of uninfected neonates born to infected mothers is similar to that of control newborns of uninfected mothers, or displays slight inflammation without lymphocyte infiltration [28].
Some Keys to Understand How T. cruzi–Placenta Interactions Lead to CCD
Role of Parasitic Diversity in the T. cruzi–Placenta Interactions
Based on different molecular approaches, T. cruzi has been classified into seven phylogenetic lineages, so-called discrete typing units (DTUs) named TcI to TcVI plus the lately added TcBat [70, 71]. Five T. cruzi DTUs (TcI, TcII, TcIII, TcV, and TcVI) and associations of them (coinfections) were identified in human cases of congenital infection. The DTU TcV has been reported in 80 to 100% of congenital cases in Argentina, Bolivia, Southern Brazil, Chile, and Paraguay [23, 43, 72,73,74,75,76,77,78,79]. The distribution of DTUs identified in congenital cases is similar to that found in the local population [72, 74, 78]. The same DTUs are generally detected in mothers and their infected newborns, as well as in congenitally infected twins or siblings born in consecutive gestations [23, 74].
So, using the current molecular markers of T. cruzi DTUs, there is no clear evidence of a relationship between DTUs and congenital infection in humans. However, various parasite populations can belong to each DTU. Indeed, using phylogenetic analysis of other specific sequences (e.g., the mini-exon intergenic region of T. cruzi DNA), a strong association could be observed between parasite haplotypes and congenital infection of newborns [80]. Besides, fingerprinting of minicircle signatures of natural parasite populations detected in placental tissues and peripheral blood of T. cruzi–infected pregnant women showed minicircle fragments in placental portions not detectable in blood, suggesting placental tropism of parasite clones [75, 81]. These observations all together open the door to a re-evaluation of possible relationship between parasite diversity, placental tropism, and CCD transmission.
Role of Maternal Immunological and Genetic Factors in the Development of CCD
Maternal immunity is likely a factor limiting transmission of infections in fetus/neonate. T. cruzi–specific IgG antibodies play a protective role by favoring the clearance of circulating parasites through activated phagocytes expressing FcR, likewise contributing to limiting parasitemia.
Analyses of innate immune defenses in pregnant women show that monocytes from transmitting women display a less activated phenotype and release less TNF-α as compared with non-transmitting subjects [82,83,84,85]. As expected, infected pregnant women display an adaptive response to parasites with higher blood cell production and circulating levels of IFN-γ than in non-infected ones [22, 47, 84]. However, T cells from those transmitting T. cruzi to their fetuses produce three times less IFN-γ than cells from non-transmitting women, which probably contributes to increase their parasitemia [22]. Altogether, such results indicate that (i) women transmitting congenital infection present some defect of their innate and adaptive immune responses; (ii) such defect mainly relies on a lower capacity to produce IFN-γ in response to T. cruzi.
Moreover, a strong maternal innate immune response is associated with the absence of congenital transmission in non-transmitting infected women [47]. The fact that around 95% of chronically infected pregnant women do not transmit parasites to their fetuses suggests that the physiological immune environment of pregnancy is likely not contributing to the immune defect of transmitting women. The pro-inflammatory environment occurring at different stages of gestation [86] might rather re-boost the innate responses during chronic infection to keep infected women away from congenital transmission.
The role of maternal genetic factors in favoring parasite transmission remains to explore. Indeed, the familial clustering of congenital cases (see above), as well as the persistence after delivery of the defective capacity of IFN-γ response to parasites in transmitting mothers [22], suggests that some mothers might display a “transmitter” phenotype/genotype.
Role of Fetal/Neonatal Immunological and Genetic Factors in the Development of CCD
The development of CCD depends on the following: (i) the amount of parasites transmitted from the mothers (see above); (ii) the capacity of the infecting parasite strain(s) to invade and multiply into cells/tissues (virulence; see above) and/or to limit the efficiency of immune responses in fetuses/neonates [1, 3••]; (iii) the local placental immune responses [3••, 19]; (iv) the time allowed for parasite multiplication from the transmission time point during pregnancy [76]; and, finally, (v) the amplitude of the own individual fetal/neonatal innate and/or adaptive immune responses against parasites, modulated according to the maternal imprinting/priming (reviewed in [1]).
Indeed, comparative studies in infected and non-infected neonates of T. cruzi–infected mothers indicate that (as for the mothers) congenitally infected neonates display weak innate immune responses [83, 85, 87, 88], but are able to mount T cell responses, mainly based on CD8+ cells with cytotoxic activities and producing IFN-γ (type 1 immune response) [89]. However, such adaptive response seems partially able to control parasitic load, but insufficient, to completely cure the congenital infection. The cell capacity of infected neonates to produce IFN-γ determines their parasitic load and the subsequent severity of CCD [1, 2••, 32].
The role of fetal/neonatal genetic factors in the development of CCD, as for mothers remains to be explored. However, if genetic factors derived from mothers (as, e.g., “transmitter” genotype) are involved, they might have different effects, since half of the genetic background of newborns was also derived from their fathers.
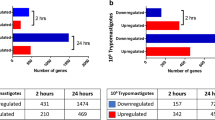
Placental Transcriptomic Responses to T. cruzi
Global transcriptomic analysis by RNA sequencing in placentas from non-transmitting infected women versus non-infected mothers shows that parasite infection induces an upregulation of genes related to inflammation and a downregulation of the anti-inflammatory cytokine IL-38 gene [90•]. Moreover, a microarray-based transcriptomics study carried out in ex vivo infected human placental explants corroborates most data obtained by RNA sequencing in whole placentas [91•]. These findings are in line with the changes observed in the immune responses of non-transmitting infected women described above.
On another side, in placentas from seropositive women, the genes encoding kisspeptin and human chorionic gonadotrophin (hCG) were downregulated with respect to those collected from non-infected women [90•]. Low serum levels of these proteins have been linked to preeclampsia and intrauterine growth constraint and are markers of miscarriage. Low expression levels of kisspeptin gene are associated to recurrent pregnancy loss. In contrast, the gene encoding neurokinin B (NKB), expressed by syncytiotrophoblasts was upregulated in placentas from CD mothers [90•]; the over-expression of this protein has been also associated with preeclampsia by decreasing blood flow to the placenta and increasing vasoconstrictor substances in the endometrium. Interestingly, kisspeptin and NKB play a key role in the placental expression of hCG in response to estradiol [92].
Furthermore, single nucleotide mutations (SNPs) in the placental genes for the disintegrin and metalloproteinases ADAM12 and MMP2 are associated to the susceptibility to congenital infection with T. cruzi [93]. Whether such mutations in placental genes are sufficiently frequent to contribute to parasite transmission remains to be determined.
Further Possible Keys Remaining to Explore
The role of the placenta microbiome [94] in the transmission of congenital infection deserves further investigations, as well as the immunomodulating role of the maternal vaginal and gut microbiomes, which are normally transmitted to the infant [95]. Particularly, the gut microbiota induces the production of anti-Gal antibodies, which are lytic for T. cruzi and susceptible to contribute to inflammatory reactions in CD [96]. A cesarean section instead of a vaginal delivery prevents the transmission of the maternal vaginal and gut microbiota. The effect of the mode of delivery in modulating infection control after birth and the severity of CCD remains to explore.
T. cruzi, as other cells, can release extracellular vesicles so-called exovesicles [97,98,99]. Such exovesicles contain trans-sialidase, cruzipain, and immature mucin-associated surface proteins. They can alter host cell functions and interfere with the host immune responses [100]. The placenta is also known to produce exovesicles related to maternal-placental-fetal communications and resistance to some infections [101, 102]. The role of such exovesicles in modulating the interactions between the parasite T. cruzi, the placenta, and CCD remains to investigate.
Synthetic and Interpretative Approach of T. cruzi Interactions with Placenta and the Occurrence of CCD
Based on the observations mentioned above, we can depict four main scenarios of interactions between the parasite and the placenta, considering the importance of placental lesions and the occurrence of transmission.
-
1.
Huge parasite loads in the intervillous space overflow the placental defenses, leading to infection and rupture of the placental anatomic barrier. This results in the transmission of large quantities of free trypomastigotes, as well as of amastigote-infected cells and to severe and mortal CCD. In such situation, the placental innate defenses are strongly activated. The placental inflammation (placentitis) is sorely marked and has pathological instead of protective effects (inflammatory/cytokinic storm), with the substantial release of TNF-α contributing to the rupture of the trophoblast and villous stroma, as well as to fetal and neonatal mortality [103]. The high local production of other inflammatory mediators, such as reactive oxygen species, NO, and peroxynitrite, has deleterious effects on placental vascularization [104]. This is probably what occurred in the observations of abortions, stillbirths, or alive neonates with severe CCD born to women displaying particularly high parasitemias, or in case of acute or reactivated infection during pregnancy.
-
2.
In the presence of moderate parasite amounts in the intervillous space, the placental innate defenses are activated. However, such activation remains limited, since T. cruzi, being partially deficient in strong PAMPs [105], can hardly stimulate the TLRs expressed on the trophoblast [16, 54]. The placental barrier is not broken off and its activation is sufficient enough to prevent the trophoblast crossing. The parasite population present into the intervillous space can infect the epithelial cells of the marginal zone deprived of trophoblast (see above; [13]). T. cruzi can bind to ECM molecules such as glycosaminoglycans, fibronectin, and laminin, using surface molecules such as gp85 and gp83 [106, 107] and disorganize the placental ECM thanks to several proteases such as cruzipain, able to destroy collagen I. This facilitates the parasite motility in the tissue and its entrance into other cells [52, 63]. Parasites surviving the mesenchymal second placental line of defense can easily spread by successive infections of fibroblasts, myofibroblasts, and macrophages (Hofbauer cells) within the chorion. They finally infect myocytes and endothelial cells lining fetal vessels embedded in chorionic plate or umbilical cord, and gain access to the fetal circulation [1, 2••, 68]. Additionally, the infection spreading in membranes surrounding the fetus induces their embrittlement, leading to their premature rupture and premature birth, which can be observed in these cases (see above). This situation likely corresponds to the common mild congenital T. cruzi infections observed in the 4.7% of live newborns of chronically infected women [5]
-
3.
In case of low parasite amounts in intervillous blood, there is neither parasite transmission, nor disruption of the placental barrier. The placental innate inflammatory response is either not or scarcely activated, whereas the trophoblast turnover contributes to impairing parasite transmission. This might concern the 95% of chronically infected pregnant women displaying low parasitemias and delivering uninfected newborns. (Fig. 2)
-
4.
Transmission of parasites (trypomastigotes as well as amastigote-infected cells) occurs at delivery, when placental breaches/tears appear naturally with labor contractions. This route, which can be avoided by cesarean delivery, is used for transmission of HIV-infected leucocytes [108]. It is independent of the activation of placental innate defenses. The percentage of congenital infection due to this transmission mode remains to be determined. However, the reported data [24] and those in our possession (Carlier et al., unpublished data) do not show significant differences comparing transmission rates in vaginal and cesarean deliveries. This indicates that, likely, most transmissions occur before childbirth, but does not exclude possible later additional transmission during labor.
Interactions between T. cruzi and placenta and occurrence of congenital infection. A detailed description of the different T. cruzi–placenta interactions is given in the manuscript’s text. Briefly: (i) huge parasitemia in maternal blood of intervillous spaces overflow the placental defenses, break up the trophoblast, and induce severe and mortal CCD; (ii) moderate parasite amounts in the intervillous space infect the epithelial cells of the marginal zone deprived of trophoblast and induce mild congenital T. cruzi infections; (iii) low parasite amounts in intervillous blood are eliminated by the trophoblast turnover, impairing parasite transmission. AC amniotic cavity, AK apoptotic knot, AM amniotic membrane, BM basal membrane, BP basal plate, CP chorionic plate, CTB cytotrophoblast, FBV fetal blood vessels, MB maternal blood, MZ marginal zone, STB syncytiotrophoblast, TLR Toll-like receptor, TTO trophoblast turnover, UC umbilical cord, VS villous stroma
Another speculative/theoretical possibility (difficult to objectify) might concern self-cured slight congenital infection in neonates having developed sufficiently strong immune responses to kill parasites previously transferred through the placenta.
Conclusions
Altogether, the data presented herein contribute to answer the main question mentioned in the introduction: why around 5% of T. cruzi–infected pregnant women transmit the parasite to their fetus/neonate whereas 95% do not? Indeed, they indicate the following: (i) the central role of the human placenta to control the transfer of parasites from the pregnant women to their fetuses and that of the immune responses in pregnant women to limit the maternal parasitemia to levels compatible with the defense capacity of placenta, which likely occurs in almost 95% of infected pregnant women not transmitting parasites to their fetuses; (ii) that most cases of congenital transmission of parasites observed nowadays (around 5%) results from an escape of low levels of parasites profiting from a placental weakness at the level of marginal zone deprived of syncitiotrophoblast to invade fetuses; (iii) a very little proportion of CCD likely results from huge maternal parasitemia out of control by the immune responses of mothers and placental defenses, as in case of acute or reactivated maternal infection; (iv) the severity of CCD mainly depends on the capacity of fetal/neonatal immune responses to control parasite multiplication, which is nowhere near as weak as previously thought, and likely explain that most cases of congenital T. cruzi infection are asymptomatic. Nevertheless, such considerations have to be completed with new investigations on parameters which might modify such maternal-fetal complex relationship (parasite molecular diversity, maternal microbiomes, exovesicles and host genetics) in order to improve the programs aiming to control or eliminate CCD.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Carlier Y, Truyens C. Congenital Chagas disease as an ecological model of interactions between Trypanosoma cruzi parasites, pregnant women, placenta and fetuses. Acta Trop. 2015;151:103–15.
•• Carlier Y, Truyens C. Maternal-fetal transmission of Trypanosoma cruzi. In: Telleria J, Tibayrenc M, editors. American trypanosomiasis-Chagas disease. One hundred years of research. 2nd ed. UK, USA: Elsevier; 2017. p. 517–59. chap 23, ISBN 978-0-12-801029-7. This book chapter provides a comprehensive review on clinical aspects of congenital Chagas disease and factors and mechanisms leading to parasite transmission.
•• Kemmerling U, Osuna A, Schijman AG, Truyens C. Congenital transmission of Trypanosoma cruzi: a review about the interactions between the parasite, the placenta, the maternal and the fetal/neonatal immune responses. Front Microbiol. 2019;10:1854. This review provides an exhaustive review about host–parasite interactions during congenital transmission of T. cruzi.
WHO. Chagas disease in Latin America: an epidemiological update based on 2010 estimates. Relev Epidemiol Hebd. 2015;90:33–43.
Howard E, Xiong X, Carlier Y, Sosa-Estani S, Buekens P. Frequency of the congenital transmission of Trypanosoma cruzi : a systematic review and meta-analysis. BJOG Int J Obstet Gynaecol. 2014;121:22–33.
Picado A, Cruz I, Redard-Jacot M, Schijman AG, Torrico F, Sosa-Estani S, et al. The burden of congenital Chagas disease and implementation of molecular diagnostic tools in Latin America. BMJ Glob Health. 2018;3:e001069.
Basile L, Jansà JM, Carlier Y, Salamanca DD, Angheben A, Bartoloni A, et al. Chagas disease in european countries: the challenge of a surveillance system. Eurosurveillance. 2011;16:37.
Rodari P, Angheben A, Gennati G, Trezzi L, Bargiggia G, Maino, et al. Congenital Chagas disease in a non-endemic area: results from a control programme in Bergamo province, northern Italy. Travel Med Infect Dis. 2018;25:31–4.
•• Carlier Y, Altcheh J, Angheben A, Freilij H, Luquetti AO, Schijman AG, et al. Congenital Chagas disease: updated recommendations for prevention, diagnosis, treatment, and follow-up of newborns and siblings, girls, women of childbearing age, and pregnant women. PLoS Negl Trop Dis. 2019. 13(10):e0007694. https://doi.org/10.1371/journal.pntd.0007694This paper specifies the target populations and the WHO recommendations for laboratory diagnosis and treatment in order to prevent and control congenital Chagas disease.
Benirschke K, Kaufmann P, Baergen P. Pathology of the human placenta. 6th ed. New York: SpringerLink; 2012.
McConkey CA, Delorme-Axford E, Nickerson CA, Kim KS, Sadovsky Y, Boyle JP, et al. A three-dimensional culture system recapitulates placental syncytiotrophoblast development and microbial resistance. Sci Adv. 2016;2:e1501462.
Heerema-McKenney A. Defense and infection of the human placenta. APMIS. 2018;126:570–88.
Nanaev AK, Kosanke G, Kemp B, Frank HG, Huppertz B, Kaufmann P. The human placenta is encircled by a ring of smooth muscle cells. Placenta. 2000;21:122–5.
Ockleford CD. The allo-epi-endothelial lining of the intervillous space. Placenta. 2010;31:1035–42.
Zeldovich VB, Clausen CH, Bradford E, Fletcher DA, Maltepe E, Robbins JR, et al. Placental syncytium forms a biophysical barrier against pathogen invasion. PLoS Pathog. 2013;9:e1003821.
Koga K, Izumi G, Mor G, Fujii T, Osuga Y. Toll-like receptors at the maternal-fetal interface in normal pregnancy and pregnancy complications. Am J Reprod Immunol. 2014;72:192–205.
Mor G, Aldo P, Alvero AB. The unique immunological and microbial aspects of pregnancy. Nat Rev Immunol. 2017;17:469–82.
Liempi A, Castillo C, Duaso J, Droguett D, Sandoval A, Barahona K, et al. Trypanosoma cruzi induces trophoblast differentiation: a potential local antiparasitic mechanism of the human placenta? Placenta. 2014;35:1035–42.
Liempi A, Castillo C, Carrillo I, Muñoz L, Droguett D, Galanti N, et al. A local innate immune response against Trypanosoma cruzi in the human placenta: the epithelial turnover of the trophoblast. Microb Pathog. 2016;99:123–9.
Droguett D, Carrillo I, Castillo C, Gómez F, Negrete M, Liempi A, et al. Trypanosoma cruzi induces cellular proliferation in the trophoblastic cell line BeWo. Exp Parasitol. 2017;173:9–17.
Brutus L, Ernould J-C, Postigo J, Romero M, Schneider D, Santalla J-A. Influence of pregnancy on Trypanosoma cruzi parasitemia in chronically infected women in a rural Bolivian community. Am J Trop Med Hyg. 2011;84:808–12.
Hermann E, Truyens C, Alonso-Vega C, Rodriguez P, Berthe A, Torrico F, et al. Congenital transmission of Trypanosoma cruzi is associated with maternal enhanced parasitemia and decreased production of interferon- gamma in response to parasite antigens. J Infect Dis. 2004;189:1274–81.
Virreira M, Truyens C, Alonso-Vega C, Brutus L, Jijena J, Torrico F, et al. Comparison of Trypanosoma cruzi lineages and levels of parasitic DNA in infected mothers and their newborns. Am J Trop Med Hyg. 2007;77:102–6.
Salas NA, Cot M, Schneider D, Mendoza B, Santalla JA, Postigo J, et al. Risk factors and consequences of congenital Chagas disease in Yacuiba, South Bolivia. Trop Med Int Health. 2007;12:1498–505.
Brutus L, Castillo H, Bernal C, Salas NA, Schneider D, Santalla J-A, et al. Detectable Trypanosoma cruzi parasitemia during pregnancy and delivery as a risk factor for congenital Chagas disease. Am J Trop Med Hyg. 2010;83:1044–7.
Bua J, Volta BJ, Velazquez EB, Ruiz AM, De Rissio AM, Cardoni RL. Vertical transmission of Trypanosoma cruzi infection: quantification of parasite burden in mothers and their children by parasite DNA amplification. Trans R Soc Trop Med Hyg. 2012;106:623–8.
Rendell VR, Gilman RH, Valencia E, Galdos-Cardenas G, Verastegui M, Sanchez L, et al. Trypanosoma cruzi-infected pregnant women without vector exposure have higher parasitemia levels: implications for congenital transmission risk. PLoS One. 2015;10:e0119527.
Bittencourt AL. Possible risk factors for vertical transmission of Chagas’ disease. Rev Inst Med Trop Sao Paulo. 1992;34:403–8.
Moretti E, Basso B, Castro I, Carrizo Paez M, Chaul M, Barbieri G, et al. Chagas’ disease: study of congenital transmission in cases of acute maternal infection. Rev Soc Bras Med Trop. 2005;38:53–5.
Freilij H, Altcheh J, Guillermo M. Perinatal human immunodeficiency virus infection and congenital Chagas’ disease. Pediatr Infect Dis J. 1995;14:161–2.
Scapellato PG, Bottaro EG, Rodríguez-Brieschke MT. Mother-child transmission of Chagas disease: could coinfection with human immunodeficiency virus increase the risk? Rev Soc Bras Med Trop. 2009;42:107–9.
Torrico MC, Solano M, Guzman JM, Parrado R, Suarez E, Alonzo-Vega C, et al. Estimation of the parasitemia in Trypanosoma cruzi human infection: high parasitemias are associated with severe and fatal congenital Chagas disease. Rev Soc Bras Me Trop. 2005;38(Suppl 2):58–61.
Bern C, Verastegui M, Gilman RH, Lafuente C, Galdos-Cardenas G, Calderon M, et al. Congenital Trypanosoma cruzi Transmission in Santa Cruz, Bolivia. Clin Infect Dis. 2009;49:1667–74.
Simister NE. Placental transport of immunoglobulin G. In: Vaccine: Elsevier BV; 2003. p. 3365–9.
Martinez DR, Fouda GG, Peng X, Ackerman ME, Permar SR. Noncanonical placental Fc receptors: what is their role in modulating transplacental transfer of maternal IgG? PLoS Pathog. 2018;14:e1007161.
Miles MA, Macedo V, Castro C, Draper CC. Trypanosoma cruzi-prenatal transfer of maternal antibody in man. Trans R Soc Trop Med Hyg. 1975;69:286.
Truyens C, Hermann E, Alonso-Vega C, Rodriguez P, Vekemans J, Torrico F, et al. Immune responses of non-infected neonates of mothers infected with Trypanosoma cruzi. Rev Soc Bras Med Trop. 2005;38(Suppl 2):96–100.
Sosa-Estani S, Gamboa-León MR, Del Cid-Lemus J, Althabe F, Alger J, Almendares O, et al. Short report: use of a rapid test on umbilical cord blood to screen for Trypanosoma cruzi infection in pregnant women in Argentina, Bolivia, Honduras, and México. Am J Trop Med Hyg. 2008;79:755–9.
Chippaux JP, Clavijo ANS, Santalla JA, Postigo JR, Schneider D, Brutus L. Antibody drop in newborns congenitally infected by Trypanosoma cruzi treated with benznidazole. Trop Med Int Health. 2010;15:87–93.
Neves SF, Elói-Santos S, Ramos R, Rigueirinho S, Gazzinelli G, Correa-Oliveira R. In utero sensitization in Chagas’ disease leads to altered lymphocyte phenotypic patterns in the newborn cord blood mononuclear cells. Parasite Immunol. 1999;21:631–9.
Didoli GL, Davila HO, Feldman S, Di Masso R, Revelli SS, Bottasso OA. Protected Trypanosoma cruzi infection in rats born to mothers receiving interferon-gamma during gestation is associated with a decreased intramacrophage parasite growth and preferential synthesis of specific IgG2b antibodies. Int J Immunopharmacol. 2000;22:45–55.
Alarcón M, Pérez MC, Villarreal J, Araujo S, Goncalves L, González A, et al. Detection of Trypanosoma cruzi DNA in the placenta and fetuses of mice with Chagasic acute infection. Investig Clin. 2009;50:335–45.
Cencig S, Coltel N, Truyens C, Carlier Y. Fertility, gestation outcome and parasite congenital transmissibility in mice infected with TcI, TcII and TcVI genotypes of Trypanosoma cruzi. PLoS Negl Trop Dis. 2013;7:e2271.
Buekens P, Cafferata ML, Alger J, Althabe F, Belizán JM, Bustamante N, et al. Congenital transmission of Trypanosoma cruzi in Argentina, Honduras, and Mexico: an observational prospective study. Am J Trop Med Hyg. 2018;98:478–85.
Maloney S, Smith A, Furst DE, Myerson D, Rupert K, Evans PC, et al. Microchimerism of maternal origin persists into adult life. J Clin Invest. 1999;104:41–7.
AbdelHalim RM, Ramadan DI, Zeyada R, Nasr AS, Mandour IA. Circulating maternal total cell-free DNA, cell-free fetal DNA and soluble Endoglin levels in preeclampsia: predictors of adverse fetal outcome? A cohort study. Mol Diagn Ther. 2016;20:135–49.
Vekemans J, Truyens C, Torrico F, Solano M, Torrico MC, Rodriguez P, et al. Maternal Trypanosoma cruzi infection upregulates capacity of uninfected neonate cells to produce pro- and anti-inflammatory cytokines. Infect Immun. 2000;68:5430–4.
Jonakait GM. The effects of maternal inflammation on neuronal development: possible mechanisms. Int J Dev Neurosci. 2007;25:415–25.
Frank F, Sartori MJ, Asteggiano C, Lin S, de Fabro SP, Fretes RE. The effect of placental subfractions on Trypanosoma cruzi. Exp Mol Pathol. 2000;69:144–51.
Luján CD, Triquell MF, Sembaj A, Guerrero CE, Fretes RE. Trypanosoma cruzi: productive infection is not allowed by chorionic villous explant from normal human placenta in vitro. Exp Parasitol. 2004;108:176–81.
Díaz-Luján C, Triquell MF, Schijman A, Paglini P, Fretes RE. Differential susceptibility of isolated human trophoblasts to infection by Trypanosoma cruzi. Placenta. 2012;33:264–70.
Duaso J, Rojo G, Cabrera G, Galanti N, Bosco C, Maya JDJD, et al. Trypanosoma cruzi induces tissue disorganization and destruction of chorionic villi in an ex vivo infection model of human placenta. Placenta. 2010;31:705–11.
Díaz-Luján C, Triquell MFF, Castillo C, Hardisson D, Kemmerling U, Fretes REE. Role of placental barrier integrity in infection by Trypanosoma cruzi. Acta Trop. 2016;164:360–8.
Carrillo I, Droguett D, Castillo C, Liempi A, Muñoz L, Maya JD, et al. Caspase-8 activity is part of the BeWo trophoblast cell defense mechanisms against Trypanosoma cruzi infection. Exp Parasitol. 2016;168:9–15.
Castillo C, Muñoz L, Carrillo I, Liempi A, Medina L, Galanti N, et al. Toll-like receptor-2 mediates local innate immune response against Trypanosoma cruzi in ex vivo infected human placental chorionic villi explants. Placenta. 2017;60:40–6.
Castillo C, Carrillo I, Liempi A, Medina L, Navarrete A, López P, et al. Trypanosoma cruzi exosomes increases susceptibility to parasite infection in human placental chorionic villi explants. Placenta. 2017;51:123–4.
Ramírez G, Valck C, Molina MC, Ribeiro CH, López N, Sánchez G, et al. Trypanosoma cruzi calreticulin: a novel virulence factor that binds complement C1 on the parasite surface and promotes infectivity. Immunobiology. 2011;216:265–73.
Castillo C, Ramírez G, Valck C, Aguilar L, Maldonado I, Rosas C, et al. The interaction of classical complement component C1 with parasite and host Calreticulin mediates Trypanosoma cruzi infection of human placenta. PLoS Negl Trop Dis. 2013;7:e2376. https://doi.org/10.1371/journal.pntd.0002376.
Sartori MJ, Lin S, Frank FM, Malchiodi EL, De Fabro SP. Role of placental alkaline phosphatase in the interaction between human placental trophoblast and Trypanosoma cruzi. Exp Mol Pathol. 2002;72:84–90.
Sartori MJ, Pons P, Mezzano L, Lin S, de Fabro SP. Trypanosoma cruzi infection induces microfilament depletion in human placenta syncytiotrophoblast. Placenta. 2003;24:767–71.
Castillo C, Villarroel A, Duaso J, Galanti N, Cabrera G, Maya JDJD, et al. Phospholipase C gamma and ERK1/2 mitogen activated kinase pathways are differentially modulated by Trypanosoma cruzi during tissue invasion in human placenta. Exp Parasitol. 2013;133:12–7.
Castillo C, López-Muñoz RA, Duaso J, Galanti N, Jaña F, Ferreira J, et al. Role of matrix metalloproteinases 2 and 9 in ex vivo Trypanosoma cruzi infection of human placental chorionic villi. Placenta. 2012;33:991–7.
Duaso J, Yanez E, Castillo C, Galanti N, Cabrera G, Corral G, et al. Reorganization of extracellular matrix in placentas from women with asymptomatic chagas disease: mechanism of parasite invasion or local placental defense? J Trop Med. 2012;2012:1–8. https://doi.org/10.1155/2012/758357.
Bittencourt AL. Congenital Chagas disease. Am J Dis Child. 1976;130:97–103.
Bittencourt AL. Chagasic placentitis and congenital transmission of Chagas’ disease. Rev Inst Med Trop Sao Paulo. 1963;5:62–7.
Altemani AM, Bittencourt AL, Lana AMA. Immunohistochemical characterization of the inflammatory infiltrate in placental Chagas’ disease: a qualitative and quantitative analysis. Am J Trop Med Hyg. 2000;62:319–24.
Azogue E, La Fuente C, Darras C. Congenital chagas’ disease in Bolivia: epidemiological aspects and pathological findings. Trans R Soc Trop Med Hyg. 1985;79:176–80.
Fernandez-Aguilar S, Lambot M-A, Torrico F, Alonso-Vega C, Córdoba M, Suarez E, et al. Placental lesions in human Trypanosoma cruzi infection. Rev Soc Bras Med Trop. 2005;38(Suppl 2):84–6.
Virreira M, Martinez S, Alonso-Vega C, Torrico F, Solano M, Torrico MC, et al. Amniotic fluid is not useful for diagnosis of congenital Trypanosoma cruzi infection. Am J Trop Med Hyg. 2006;75:1082–4.
Zingales B, Miles MA, Campbell DA, Tibayrenc M, Macedo AM, Teixeira MM, et al. The revised Trypanosoma cruzi subspecific nomenclature: rationale, epidemiological relevance and research applications. Infect Genet Evol. 2012;12:240–53.
Lima L, Espinosa-Álvarez O, Ortiz PA, Trejo-Varón JA, Carranza JC, Pinto CM, et al. Genetic diversity of Trypanosoma cruzi in bats, and multilocus phylogenetic and phylogeographical analyses supporting Tcbat as an independent DTU (discrete typing unit). Acta Trop. 2015;151:166–77.
Virreira M, Alonso-Vega C, Solano M, Jijena J, Brutus L, Bustamante Z, et al. Congenital Chagas disease in Bolivia is not associated with DNA polymorphism of Trypanosoma cruzi. Am J Trop Med Hyg. 2006;75:871–9.
Ortiz S, Zulantay I, Solari A, Bisio M, Schijman A, Carlier Y, et al. Presence of Trypanosoma cruzi in pregnant women and typing of lineages in congenital cases. Acta Trop. 2012;124:243–6.
Burgos JM, Altcheh J, Bisio M, Duffy T, Valadares HM, Seidenstein ME, et al. Direct molecular profiling of minicircle signatures and lineages of Trypanosoma cruzi bloodstream populations causing congenital Chagas disease. Int J Parasitol. 2007;37:1319–27.
Bisio M, Seidenstein ME, Burgos JM, Ballering G, Risso M, Pontoriero R, et al. Urbanization of congenital transmission of Trypanosoma cruzi: prospective polymerase chain reaction study in pregnancy. Trans R Soc Trop Med Hyg. 2011;105:543–9.
Bua J, Volta BJ, Perrone AE, Scollo K, Velázquez EB, Ruiz AM, et al. How to improve the early diagnosis of Trypanosoma cruzi infection: relationship between validated conventional diagnosis and quantitative DNA amplification in congenitally infected children. PLoS Negl Trop Dis. 2013;7:e2476.
Garcia A, Ortiz S, Iribarren C, Bahamonde MI, Solari A. Congenital co-infection with different Trypanosoma cruzi lineages. Parasitol Int. 2014;63:138–9.
Corrales RM, Mora MC, Negrette OS, Diosque P, Lacunza D, Virreira M, et al. Congenital Chagas disease involves Trypanosoma cruzi sub-lineage IId in the northwestern province of Salta, Argentina. Infect Genet Evol. 2009;9:278–82.
Diez CN, Manattini S, Zanuttini JC, Bottasso O, Marcipar I. The value of molecular studies for the diagnosis of congenital Chagas disease in northeastern Argentina. Am J Trop Med Hyg. 2008;78:624–7.
Herrera C, Truyens C, Dumonteil E, Alger J, Sosa-Estani S, Cafferata ML, et al. Phylogenetic analysis of Trypanosoma cruzi from pregnant women and newborns from Argentina, Honduras, and Mexico suggests an association of parasite haplotypes with congenital transmission of the parasite. J Mol Diagn. 2019;21:1095–100.
Medina L, Castillo C, Liempi A, Herbach M, Cabrera G, Valenzuela L, et al. Differential infectivity of two Trypanosoma cruzi strains in placental cells and tissue. Acta Trop. 2018;186:35–40.
Cardoni RL, García MM, De Rissio AM. Proinflammatory and anti-inflammatory cytokines in pregnant women chronically infected with Trypanosoma cruzi. Acta Trop. 2004;90:65–72.
García MM, De Rissio AM, Villalonga X, Mengoni E, Cardoni RL. Soluble tumor necrosis factor (TNF) receptors (sTNF-R1 and -R2) in pregnant women chronically infected with Trypanosoma cruzi and their children. Am J Trop Med Hyg. 2008;78:499–503.
Cuna WR, Choque AGH, Passera R, Rodriguez C. Pro-inflammatory cytokine production in chagasic mothers and their uninfected newborns. J Parasitol. 2009;95:891–4.
Hermann E, Alonso-Vega C, Berthe A, Truyens C, Flores A, Cordova M, et al. Human congenital infection with Trypanosoma cruzi induces phenotypic and functional modifications of cord blood NK cells. Pediatr Res. 2006;60:38–43.
Racicot K, Kwon J-Y, Aldo P, Silasi M, Mor G. Understanding the complexity of the immune system during pregnancy. Am J Reprod Immunol. 2014;72:107–16.
Mayer JP, Biancardi M, Altcheh J, Freilij H, Weinke T, Liesenfeld O. Congenital infections with Trypanosoma cruzi or Toxoplasma gondii are associated with decreased serum concentrations of interferon-γ and interleukin-18 but increased concentrations of interleukin-10. Ann Trop Med Parasitol. 2010;104:485–92.
Fernández-Villegas A, Thomas MC, Carrilero B, Téllez C, Marañón C, Murcia L, et al. The innate immune response status correlates with a divergent clinical course in congenital Chagas disease of twins born in a non-endemic country. Acta Trop. 2014;140:84–90.
Hermann E, Truyens C, Alonso-Vega C, Even J, Rodriguez P, Berthe A, et al. Human fetuses are able to mount an adultlike CD8 T-cell response. Blood. 2002;100:2153–8.
• Juiz NA, Torrejón I, Burgos M, Torres AMF, Duffy T, Cayo NM, et al. Alterations in placental gene expression of pregnant women with chronic Chagas disease. Am J Pathol. 2018;188:1345–53 First extensive study about gene expression of placentas from women infected with T. cruzi.
• Castillo C, Carrillo I, Libisch G, Juiz N, Schijman AG, Robello C, et al. Host-parasite interaction: changes in human placental gene expression induced by Trypanosoma cruzi. Parasit Vectors. 2018;11:1–13 First extensive study about placental gene expression in response to ex vivo T. cruzi infection.
Oride A, Kanasaki H, Mijiddorj T, Sukhbaatar U, Ishihara T, Kyo S. Regulation of kisspeptin and gonadotropin-releasing hormone expression in rat placenta: study using primary cultures of rat placental cells. Reprod Biol Endocrinol. 2015;13:90. https://doi.org/10.1186/s12958-015-0083-3.
Juiz NA, Cayo NM, Burgos M, Salvo ME, Nasser JR, Búa J, et al. Human polymorphisms in placentally expressed genes and their association with susceptibility to congenital Trypanosoma cruzi infection. J Infect Dis. 2016;213:1299–306.
Aagaard K, Ma J, Antony KM, Ganu R, Petrosino J, Versalovic J. The placenta harbors a unique microbiome. Sci Transl Med. 2014;6:237ra65. https://doi.org/10.1126/scitranslmed.3008599.
Romano-Keeler J, Weitkamp JH. Maternal influences on fetal microbial colonization and immune development. Pediatr Res. 2015;77:189–95.
Truyens C, Carlier Y. Protective host response to Trypanosoma cruzi and its limitations. In: Telleria J, Tibayrenc M, editors. American trypanosomiasis-Chagas disease. One hundred years of research. 2nd ed, chap 25. UK, USA: Elsevier; 2017. p. 579–604.
Garcia-Silva MR, Cabrera-Cabrera F, Cura Das Neves RF, Souto-Padrón T, De Souza W, Cayota A. Gene expression changes induced by Trypanosoma cruzi shed microvesicles in mammalian host cells: relevance of tRNA-derived halves. Biomed Res Int. 2014;2014:1–11. https://doi.org/10.1155/2014/305239.
Marcilla A, Martin-Jaular L, Trelis M, de Menezes-Neto A, Osuna A, Bernal, et al. Extracellular vesicles in parasitic diseases. J Extracell Vesicles. 2014;3:25040.
de Pablos Torró LM, Retana Moreira L, Osuna A. Extracellular vesicles in Chagas disease: a new passenger for an old disease. Front Microbiol. 2018;9:1190.
Retana Moreira L, Rodríguez Serrano F, Osuna A. Extracellular vesicles of Trypanosoma cruzi tissue-culture cell-derived trypomastigotes: induction of physiological changes in non-parasitized culture cells. PLoS Negl Trop Dis. 2019;13:e0007163.
Ouyang Y, Mouillet JF, Coyne CB, Sadovsky Y. Review: placenta-specific microRNAs in exosomes - good things come in nano-packages. Placenta. 2014;35:S69–73.
Schorey JS, Harding CV. Extracellular vesicles and infectious diseases: new complexity to an old story. J Clin Invest. 2016;126:1181–9.
Haider S, Knöfler M. Human tumour necrosis factor: physiological and pathological roles in placenta and endometrium. Placenta. 2009;30:111–23.
Myatt L, Cui X. Oxidative stress in the placenta. Histochem Cell Biol. 2004;122:369–82.
Kurup SP, Tarleton RL. Perpetual expression of PAMPs necessary for optimal immune control and clearance of a persistent pathogen. Nat Commun. 2013;4:2616. https://doi.org/10.1038/ncomms3616.
Lima APCA, Almeida PC, Tersariol ILS, Schmitz V, Schmaier AH, Juliano L, et al. Heparan sulfate modulates kinin release by Trypanosoma cruzi through the activity of cruzipain. J Biol Chem. 2002;277:5875–81.
Maeda FY, Cortez C, Izidoro MA, Juliano L, Yoshida N. Fibronectin-degrading activity of Trypanosoma cruzi cysteine proteinase plays a role in host cell invasion. Infect Immun. 2014;82:5166–74.
Biggar RJ, Lee TH, Wen L, Broadhead R, Kumwenda N, Taha TE, et al. The role of transplacental microtransfusions of maternal lymphocytes in HIV transmission to newborns. AIDS. 2008;22:2251–6.
Acknowledgments
We acknowledge Dr. Ana Liempi for her help with the figure design and drawing.
Funding
This research was funded by Fondecyt 1190341 (U.K.); ERANET-LAC grant ERANET17/HLH-0142 (U.K.; A.G.S).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on The Placenta, Tropical Diseases, and Pregnancies
Rights and permissions
About this article
Cite this article
Carlier, Y., Schijman, A.G. & Kemmerling, U. Placenta, Trypanosoma cruzi, and Congenital Chagas Disease. Curr Trop Med Rep 7, 172–182 (2020). https://doi.org/10.1007/s40475-020-00210-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-020-00210-5