Abstract
Purpose of Review
The aim of this review is to discuss benefits of mindfulness for the treatment of attention deficit hyperactivity disorder (ADHD) in adolescents.
Recent Findings
ADHD is a developmental disorder that persists into adulthood for most of the cases. ADHD, an often lifelong condition, is characterized by prevalent impairment in numerous domains such as mental health, occupational, academic, and many more. Pharmacological treatment option (e.g., stimulant) is a core of treatment for ADHD. However, even after receiving proper pharmacological medications, numerous patients continue to experience impairment or inadequate symptom reduction. Moreover, many patients also desire to reduce consumption of medicines and pursue alternative approaches. Among available non-pharmacological treatment options, mindfulness meditation training has established mounting clinical interest and empirical support. Various studies have reported effects of mindfulness training in adolescents with ADHD.
Summary
This review will summarize the rationale behind the use of mindfulness training in adolescents with ADHD. Moreover, this review will also explain outcomes from various studies recommending use of mindfulness training as a treatment of ADHD in adolescents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
What Is Attention Deficit Hyperactivity Disorder (ADHD)?
Attention deficit hyperactivity disorder (ADHD) is a neurological developmental disorder. ADHD is characterized by inattention, hyperactive, and impulsive behavior [1,2,3]. The worldwide prevalence of ADHD is around 5.0% among children and 4.4% among adults [4]. The inception of ADHD happens at around the age of 12 years. Its symptoms endure to persist during adulthood. As per the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), the three principal symptoms of ADHD are inattention, hyperactivity, and impulsivity [5].
Children and adolescents suffering from ADHD tend to have difficulty following rules and resisting distractions. They also have difficulty with concentration and continued attention when completing a task. They tend to get restless or nervous and frequently disturb others [6•]. Hence, they have difficulties making friends, and they tend to perform inadequately compared with individuals without ADHD [7, 8].
Prevalence of ADHD in Adolescents
The prevalence of ADHD differs from country to country, with a significantly greater prevalence in the USA than in European countries [9]. Besides, the prevalence of ADHD keeps changing from time to time. For example, the National Health Interview Survey (NHIS) had reported a 33% increase in ADHD prevalence from 1997 to 1999 (5.7%) to 2006–2008 (7.6%) among children and adolescents aged 3 to 17 years [10]. Likewise, as reported by the National Survey of Children’s Health, the prevalence of ADHD was augmented by 42% between 2003 and 2011 among children and adolescents aged 4 to 17 years [11••]. Xu G et al. in 2018 reported that the estimated prevalence of diagnosed ADHD in US children and adolescents has been increased from 6.1 in 1997–1998 to 10.2% in 2015–2016 [12••].
Impact of ADHD in Adolescents
It has been reported that approximately 80–85% of preteens continue to suffer from ADHD symptoms into the adolescent years, and 60% of them continue to have ADHD symptoms into adulthood [13,14,15]. ADHD has a significant impact on day-to-day life of adolescents. For example, adolescents with ADHD have troubles in sustaining attention in usual tasks. They also tend to do poorly in studies [16]. Moreover, they have difficulty in maintaining peer relations and family cohesiveness [17,18,19,20]. If these individuals do not receive proper treatment, untreated patients might have greater rates of risky sexual behaviors [18], suicidal thoughts in college [21], imprisonments [19], car accidents [22, 23], professional difficulties, and medical encumbrance [24]. They also have inferior self-esteem, social functioning, economic achievement, and greater rates of substance use [25].
Treatments of ADHD in Adolescents
The treatment approaches for ADHD in adolescents can be broadly classified into pharmacological and non-pharmacological. For pharmacological treatments, stimulant medications (amphetamine-based or methylphenidate-based preparations) are considered to be gold standard [26]. Non-stimulant medications such as bupropion, atomoxetine, and guanfacine-based preparations have some evidence [27•, 28, 29•]. However, the usage of medications depends on the personal preference of the patients due to various reasons such as cost, side effects, inability to tolerate the medicine, etc. [29•, 30]. Due to these and other reasons at individual level, patients tend to seek non-pharmacological treatments for ADHD. A subset of patient population may be willing to take psychopharmacological treatment but may prefer to add non-pharmacological treatments to counteract the symptoms that are persisting despite the adequate dosage of pharmacological treatment [30]. Some patients prefer non-pharmacological methods to achieve symptom reductions so as to reduce the dosages of pharmacologic treatments, whereas some patients are just holistic minded and prefer to try non-pharmacologic methods before going to pharmacological treatments [30].
Non-pharmacological Treatment Options for Adolescents with ADHD
Non-pharmacological interventions play a major role in the treatment of ADHD in adolescents. Adolescents with ADHD tend to have conflicts with their parents [31]. For example, teens may desire for more freedom and independence from their parents. Moreover, there may be forced interactions between the adolescents with ADHD and their parents as both may strive to accomplish their goals. Barkley et al. has established a four-factor model to differentiate these interchanges that comprise: “1) the adolescent’s characteristics; 2) parent characteristics; 3) family environment and stressors and 4) parenting practices” [32••]. Barkley and Robin have also developed and verified a manualized therapy to tackle teen-parent conflict [32••]. Their approach basically includes educating parents and adolescents on how ADHD affects the adolescent’s functioning and their interactions; and this way, they educate parents to “choose their battles” and reward positive behavior of the adolescent. Their approach is helpful for both parents and adolescents to understand on what to expect from one another, apply a problem-solving approach to discuss disagreements, and understand to utilize more effective communication skills by avoiding usage of ultimatums or negative comments [32••, 33]. The treatment approach comprises problem-solving communication training (PSCT) and behavior therapy (BT) with more emphasis on BT and has been moderately effective in improving conflict between adolescents with ADHD and their parents [32••]. It has been also reported that several components of BT comprising organizational skills have shown beneficial effects individually as well as in the school setting [34]. Another non-pharmacological treatment option for ADHD is mindfulness. In next few sections, effect of mindfulness for the treatment of ADHD in adolescents will be discussed.
What Is Mindfulness?
Mindfulness is a practice based on “Zen Buddhism.” It is a prevalent way of self-calming and self-regulating [35]. Jon Kabat-Zinn defined “mindfulness” as “paying attention in a particular way, on purpose, in the present moment, and nonjudgmentally” [36•]. It can also be interpreted as attending present moment without wanting to change the experience. The words such as non-judgemental awareness or loving awareness are often used to describe mindfulness [36•].
Effect of Mindfulness in Adolescents with ADHD
Mindfulness training helps individuals with ADHD to improve their attention in such a way that they gain awareness of how their mind becomes distracted. This way mindfulness helps them achieve self-regulatory skills. With mindfulness training, they can identify what is causing the distraction and can shift their attention back to their activity. Mindfulness training has been incorporated with therapeutic techniques to treat ADHD. Several types of mindfulness-based programs have been used such as mindfulness-based stress reduction [37•], mindfulness-based cognitive therapy [38,39,40], and acceptance and commitment therapy [41].
Various studies have reported beneficial effects of mindfulness-based interventions (MBIs) on children and adolescents diagnosed with or presenting symptoms of ADHD. For example, MBIs have been reported to reduce parent-rated inattention, hyperactivity, and impulsivity [42••]. MBIs have also been beneficial in reduction of internalizing and externalizing problems [38, 43]. Moreover, MBIs have been correlated with increased active engagement in instruction and augmentation of cognitive processes, comprising sustained attention [38, 43, 44].
The mindfulness training (MT) model combines features of mindfulness-based cognitive therapy and mindfulness-based stress reduction. Various studies have reported benefits of MT model in children and adolescents with ADHD [38, 39, 42]. MT was originally based on mindfulness-based cognitive therapy for the treatment of depression [6•]. In order to treat children and adolescents with ADHD, the following modifications have been made in MT model: a repeated assortment of breath meditation (e.g., focus on the feelings of breathing), concentrated short activities (such as yoga, mindful listening, mindful eating), sensory-based movement activities and empirical learning behaviors, extremely organized sessions (such as detailed agendas, mindfulness homework), and reinforcement of participation of parents through training and psychoeducation along with involvement in necessary activities at home [6•].
What Is the Rationale Behind Use of Mindfulness Training for the Treatment of ADHD?
Mindfulness-based treatment options have been reported to be beneficial for various mental health treatment targets [45,46,47]. Mindfulness meditation at the intervention level involves focusing attention on any specific task (e.g., breathing pattern) and refocusing on it again after any sort of distraction. This may help the patients with ADHD to be more attentive on one particular task/object at a time [48•]. Practicing mindfulness requires a regulation of attention and conflict detection, and this has been considered as a regulatory approach to attention that advances executive processes [49]. Like any other skill, the skill of attending to one task gets enhanced with practice, and this improves overall attention. As poor attention is a one of the core symptoms of ADHD, mindfulness may help to strengthen this aspect in patients with ADHD. Figure 1 represents a schematic indicating how mindfulness is beneficial for improving the attention and thus the treatment of ADHD. Various studies have reported that practicing mindfulness improves attention. For example, one study evaluated the effect of 5 days (20 min per day) of meditation against relaxation [50•]. This study reported that the participants in the meditation group could detect conflict significantly in a significantly greater manner during an attentional task than the participants in relaxation group. Another study reported similar outcomes where participants underwent 4 days of meditation training (20 min per day) and reported better outcomes on working memory and executive functioning compared with the participants in an active treatment comparison group [51•]. Several neuroimaging studies have suggested that mindfulness meditation stimulates neuroplastic modifications in brain areas correlated with attentional functioning that are usually impaired in patients with ADHD. For example, the anterior cingulate cortex region is involved with attentional processing in ADHD [52, 53] and detecting any conflict related to mismatched information [54]. Mindfulness studies have shown to improve the functions of this region [51•].
In addition to poor attention, the other areas affected in ADHD are emotional dysregulation/impulsivity and physical hyperactivity. It is well-known that patients with ADHD have difficulties in regulating their emotions, which contribute to substantial impairment [55,56,57]. Mindfulness training is reported to improve emotion regulation [58]. Mindfulness teaches patients to notice emotional states as momentary and transient phenomenon, which can be responded to in a non-reactive or considerate manner. Hence, it helps patients resist impetuous desires to act out on their emotions and thus reduces the emotional impulsivity that is associated with ADHD [56]. As mindfulness will be strengthening the aptitude to regulate emotions in patients, it is a good non-pharmacological treatment option. One study has reported that 5 days of meditation training (20 min per day) improved emotional measures such as depression, anger, and anxiety [50•]. Another study has discovered that 5 weeks of mindfulness training (5–16 min per day) leads to modifications in frontal electroencephalographic asymmetry configurations that is related with positive, approach-oriented emotions [59].
Neuroimaging studies have also revealed that overlapping brain regions are associated for emotion dysregulation in patients with ADHD [56] and mindfulness meditation. Certain regions in the brain such as the prefrontal cortex, hippocampus, and amygdala were correlated with enhancement in emotion regulation following mindfulness training [54]. It is important to note that these regions are also recognized to have their involvement in emotional functioning in patients with ADHD [56]. This section has explained that both inattention and emotional regulation can be improved by mindfulness training, and it explains why mindfulness training should be used for the treatment of adolescents with ADHD.
Outcomes of Mindfulness Treatment in Adolescents with ADHD
Mindfulness training can be implemented in different manners. For example, an adolescent with ADHD would receive mindfulness training, or along with the patient, the caregiver is also given simultaneous mindfulness training as well.
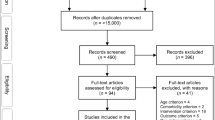
In one of the earliest studies by Zylowska et al., adolescents (n = 8; age group, 15–18 years) with ADHD received mindfulness training and were compared with a separate group of adults with ADHD [60••]. This study reported that despite of good attendance and higher satisfaction with the mindfulness treatment among the adolescents, there was a predisposition for inferior compliance with at-home practice compared with adults with ADHD.
In a study by Haydicky et al., male adolescents (n = 60; age group, 12–18 years) received a 20-week mindfulness training program, which also combined fundamentals of CBT and mixed martial arts [61]. These adolescents were compared with a waitlist control group. Various subgroup analyses in this study have established that mindfulness improves parent-rated externalizing behavior, monitoring skills, and social problems but does not cause improvement in symptoms of ADHD, parent report of executive functioning, social problems, externalizing symptoms, and self-reported measures of social problems. It is essential to remember that this study had a small sample size and there was a lack of random assignment to treatment conditions. Moreover, there was a lack of an active treatment comparison group.
Promising initial outcomes can be achieved if along with adolescents with ADHD, and their parents also receive mindfulness training. In one of the MYmind studies, it has been reported that when 14 adolescents with externalizing disorders and their parents received mindfulness training, there were improvements in self-reported externalizing behaviors, attention problems, personal goals, social problems, happiness, and mindful awareness. Similar outcomes were also observed at 8-week follow-up [38]. Moreover, self-reported internalizing symptoms and self-reported thinking problems also improved significantly after the treatment.
Another MYmind program study was conducted on 10 adolescents (age group, 11–15 years) with ADHD and their parents [39]. During this study, within-group evaluations were done right after the mindfulness training, at 8-week follow-up and at 16-week follow-up. This study noted that there were statistically significant enhancements in externalizing behavior (paternal report), parental stress (paternal report), and parental over-reactivity (maternal report). There were also improvements in attention problems (paternal report), internalizing problems (paternal report), metacognition (a component of executive functioning, paternal report), and behavioral regulation (a component of executive functioning, tutor report). However, these improvements were not statistically significant but approached significance during data analysis. At the time of 8-week follow-up, significant improvement in attention problems (as per the adolescent report) was reported. Improvements were also reported as per the paternal report for behavioral regulation, externalizing behaviors, metacognition, and parental stress. At 16-week follow-up, only adolescent assessments were collected. At 16 weeks, the enhancements in externalizing behaviors came close to gain statistical significance. Two computerized sustained attention tasks (a visual sustained attention task and an auditory sustained attention task) were given to the participants at post-treatment and both follow-ups. On a visual sustained attention task, adolescents showed an improvement in reaction speed; however, this was not sustained at either follow-up. When participants performed an auditory sustained attention task, the quantity of incorrect alarm responses diminished significantly, and this was sustained for both follow-up evaluations. At 8-week follow-up, the number of misses enhanced; however, it was not maintained at 16-week follow-up.
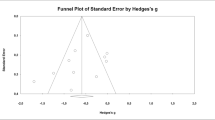
Haydicky et al. implemented the MYmind program to adolescents (n = 18; age group, 13–18 years) with ADHD and a discrete group for their parents (n = 17) [62]. This study focused on various assessments that included 4 weeks pre-treatment (baseline), pre-treatment, end of treatment, and 6-week follow-up. Parents’ and adolescents’ evaluations of inattentive, hyperactive/impulsive, conduct disorder, oppositional defiant disorder, symptoms of anxiety, and depression were also considered. Moreover, functional impairment was measured by acquiring parent-reported details of learning, executive functioning, and peer relations problems along with adolescent report of learning and family relations problems. According to the parent report, mindfulness training improved peer relations and symptoms of conduct disorder, whereas inattentive symptoms were close to achieving statistical significance. However, these outcomes were not significantly different at the time of follow-up. Improvements for adolescent report of depression, anxiety, and internalizing symptoms were also reported. Parent report of improvement in depression was also observed that was close to statistical significance. Supplementary assessments of parenting stress, family functioning, and mindfulness were also measured. Among the 12 parental stress outcomes, two outcomes improved at post-treatment, and three outcomes improved at follow-up. The findings of this study reported that mindful parenting enhanced the outcomes at post-treatment but not at follow-up, whereas parental acceptance enhanced only at the time of follow-up. The findings from different studies as mentioned here in this review demonstrate that that mindfulness training in adolescents diagnosed with ADHD is achievable and acceptable. None of the studies have reported any negative side effect of mindfulness. Hence, mindfulness is effective as well as safe and tolerable treatment modality.
Summary
This review has provided details on why mindfulness should be considered for the treatment of ADHD in adolescents. Current literature has reported benefits on mindfulness meditation training in adolescents diagnosed with ADHD and have provided preliminary support suggesting its effectiveness, safety, and tolerability in these patients. The efficacy is more robust if parents also receive the mindfulness training along with adolescents. Although the current literature is showing promising results on mindfulness as an effective non-pharmacological treatment modality in adolescents with ADHD, more systematically rigorous trials are required, predominantly larger randomized controlled trials and evaluation of long-term effects with valid measures.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kuntsi J, Wood AC, Rijsdijk F, Johnson KA, Andreou P, Albrecht B, et al. Separation of cognitive impairments in attention-deficit/hyperactivity disorder into 2 familial factors. Arch Gen Psychiatry [Internet]. 2010;67(11):1159–67 [cited 2019 Aug 23]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/21041617.
Liddle EB, Hollis C, Batty MJ, Groom MJ, Totman JJ, Liotti M, et al. Task-related default mode network modulation and inhibitory control in ADHD: effects of motivation and methylphenidate. J Child Psychol Psychiatry Allied Discip. 2011;52(7):761–71.
Sergeant J. The cognitive-energetic model: an empirical approach to attention-deficit hyperactivity disorder. Neurosci Biobehav Rev [Internet]. 2000;24(1):7–12 [cited 2019 Aug 23]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/10654654.
Polanczyk G, De Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–8.
Substance Abuse and Mental Health Services Administration. DSM-5 changes: Implications for child serious emotional disturbance. Rockville (MD): Substance abuse and mental health services Administration (US); 2016.
• Leeth CD, Villarreal V, Styck KM. Mindfulness interventions for children and adolescents with ADHD: a review of objectives and skills. J Creat Ment Health. 2019;14(4):436–46 This review article provides the details on how mindfulness improves skills in adolescents with ADHD.
Efron D, Bryson H, Lycett K, Sciberras E. Children referred for evaluation for ADHD: comorbidity profiles and characteristics associated with a positive diagnosis. Child Care Health Dev. 2016;42(5):718–24.
Marton I, Wiener J, Rogers M, Moore C. Friendship Characteristics of children with ADHD. J Atten Disord [Internet]. 2015;19(10):872–81 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/22967902.
Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Vol. 135, Pediatrics: American Academy of Pediatrics; 2015;134(4:):e994–1001. https://doi.org/10.1542/peds.2014-348.
Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, et al. Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatr Int. 2011;127(6):1034–42 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/21606152.
•• Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry [Internet]. 2014;53(1):34–46.e2 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/24342384. This study reports the details of parent-report of ADHD.
•• Xu G, Strathearn L, Liu B, Yang B, Bao W. Twenty-year trends in diagnosed attention-deficit/hyperactivity disorder among US children and adolescents, 1997-2016. JAMA Netw Open. 2018;1(4):e181471 This study provides the detailes on the trend of ADHD in adolescents.
Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry [Internet]. 1990;29(4):546–57 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/2387789.
Biederman J, Faraone S, Milberger S, Curtis S, Chen L, Marrs A, et al. Predictors of persistence and remission of ADHD into adolescence: results from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry [Internet]. 1996;35(3):343–51 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/8714323.
Faraone SV, Biederman J, Mennin D, Gershon J, Tsuang MT. A prospective four-year follow-up study of children at risk for ADHD: psychiatric, neuropsychological, and psychosocial outcome. J Am Acad Child Adolesc Psychiatry [Internet]. 1996;35(11):1449–59 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/8936911.
Breslau J, Miller E, Breslau N, Bohnert K, Lucia V, Schweitzer J. The impact of early behavior disturbances on academic achievement in high school. Pediatr Int. 2009;123(6):1472–6 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/19482756.
Scholtens S, Rydell A-M, Yang-Wallentin F. ADHD symptoms, academic achievement, self-perception of academic competence and future orientation: a longitudinal study. Scand J Psychol [Internet]. 2013;54(3):205–12 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/23510262.
Harpin V, Mazzone L, Raynaud JP, Kahle J, Hodgkins P. Long-Term Outcomes of ADHD: a systematic review of self-esteem and social function. J Atten Disord [Internet]. 2016;20(4):295–305 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/23698916.
Klein RG, Mannuzza S, Ramos Olazagasti MA, Roizen Belsky E, Hutchison JA, Lashua-Shriftman E, et al. Clinical and functional outcome of childhood ADHD 33 years later. Arch Gen Psychiatry. 2012;69(12):1295–303.
Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. Ambul Pediatr [Internet]. 2007;7(1 Suppl):82–90 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/17261487.
Patros CHG, Hudec KL, Alderson RM, Kasper LJ, Davidson C, Wingate LR. Symptoms of attention-deficit/hyperactivity disorder (ADHD) moderate suicidal behaviors in college students with depressed mood. J Clin Psychol [Internet]. 2013;69(9):980–93 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/23775306.
Barkley RA, Cox D. A review of driving risks and impairments associated with attention-deficit/hyperactivity disorder and the effects of stimulant medication on driving performance. J Saf Res [Internet]. 2007;38(1):113–28 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/17303170.
Narad M, Garner AA, Brassell AA, Saxby D, Antonini TN, O’Brien KM, et al. Impact of distraction on the driving performance of adolescents with and without attention-deficit/hyperactivity disorder. JAMA Pediatr. 2013;167(10):933–8.
Nigg JT. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin Psychol Rev [Internet]. 2013;33(2):215–28 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/23298633.
Willcutt EG. The prevalence of DSM-IV ADHD: a meta-analytic review. Neurotherapeutics [Internet]. 2012;9(3):490–9 [cited 2020 Feb 11]; Available from: http://springerlink.bibliotecabuap.elogim.com/article/10.1007/s13311-012-0135-8/fulltext.html.
Jensen PS. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 1999;56(12):1073–86.
• Durell TM, Adler LA, Williams DW, Deldar A, McGough JJ, Glaser PE, et al. Atomoxetine treatment of attention-deficit/hyperactivity disorder in young adults with assessment of functional outcomes: a randomized, double-blind, placebo-controlled clinical trial. J Clin Psychopharmacol [Internet]. 2013;33(1):45–54 [cited 2020 Feb 29]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/23277268. This clinical trial reports that atomoxetine is beneficial for the treatment of ADHD in adolescents.
Wilens TE, Robertson B, Sikirica V, Harper L, Young JL, Bloomfield R, et al. A randomized, placebo-controlled trial of guanfacine extended release in adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry [Internet]. 2015;54(11):916–25.e2 [cited 2020 Feb 29];Available from: http://www.ncbi.nlm.nih.gov/pubmed/26506582.
• Banaschewski T, Roessner V, Dittmann RW, Santosh PJ, Rothenberger A. Non-stimulant medications in the treatment of ADHD. Eur Child Adolesc Psychiatry [Internet]. 2004;13 Suppl 1(1):I102–16 [cited 2020 Feb 29]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/15322961. This article provides details on available non-stimulant medicines for ADHD.
Brahmbhatt K, Hilty DM, Hah M, Han J, Angkustsiri K, Schweitzer J. Diagnosis and treatment of ADHD during adolescence in the primary care setting: review and future directions. J Adolesc Health. 2016;59(2):135–43.
Stefanini JR, Scherer ZAP, Scherer EA, Cavalin LA, Guazzelli MS. Adolescents with attention deficit hyperactivity disorder and exposure to violence: parents’ opinion. Rev Lat Am Enfermagem [Internet]. 2015;23(6):1090–6 [cited 2020 Feb 29]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/26626000.
•• Jerome L. Defiant teens: a clinician’s manual for assessment and family intervention. Can Child Adolesc Psychiatry Rev. 2003;12(2):45 This study reports the potential teen-parent conflicts in adolescnets with ADHD and proposes interventions as well.
Canu WH, Eddy LD. Attention-deficit hyperactivity disorder: a handbook for diagnosis and treatment (4th ed.). Cogn Behav Ther. 2015;44(6):526–6.
Evans SW, Schultz BK, DeMars CE, Davis H. Effectiveness of the challenging horizons after-school program for young adolescents with ADHD. Behav Ther. 2011 Sep;42(3):462–74.
Nelson JB. Mindful Eating: the art of presence while you eat. Diabetes Spectr [Internet]. 2017;30(3):171–4 [cited 2019 Dec 12]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/28848310.
• Stress, Pain, and Illness. The Body-Scan. New York: Delta Book; 1990. p. 76–7. This book chapter provides definition of mindfulness.
• Carboni JA, Roach AT, Fredrick LD. Impact of mindfulness training on the behavior of elementary students with attention-deficit/hyperactive disorder. Res Hum Dev. 2013;10(3):234–51 This study reports the benefits of mindfulness on ADHD.
Bögels S, Hoogstad B, Van Dun L, De Schutter S, Restifo K. Mindfulness training for adolescents with externalizing disorders and their parents. Behav Cogn Psychother. 2008;36(2):193–209.
van de Weijer-Bergsma E, Formsma AR, de Bruin EI, Bögels SM. The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. J Child Fam Stud. 2012;21(5):775–87.
van der Oord S, Bögels SM, Peijnenburg D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J Child Fam Stud. 2012;21(1):139–47.
Murrell AR, Steinberg DS, Connally ML, Hulsey T, Hogan E. Acting out to ACTing on: a preliminary investigation in youth with ADHD and co-morbid disorders. J Child Fam Stud. 2015;24(7):2174–81.
•• Van der Oord S, Prins PJM, Oosterlaan J, Emmelkamp PMG. Efficacy of methylphenidate, psychosocial treatments and their combination in school-aged children with ADHD: a meta-analysis. Clin Psychol Rev [Internet]. 2008;28(5):783–800 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/18068284. This study reports the beneficial effects of methylphenidate in children with ADHD.
Semple RJ, Reid EFG, Miller L. Treating anxiety with mindfulness: an open trial of mindfulness training for anxious children. J Cogn Psychother. 2005;19(4):379–92.
Singh NN, Lancioni GE, Karazsia BT, Felver JC, Myers RE, Nugent K. Effects of samatha meditation on active academic engagement and math performance of students with attention deficit/hyperactivity disorder. Mindfulness (N Y). 2016;7(1):68–75.
Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J Psychosom Res [Internet]. 2010;68(6):539–44 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/20488270.
Fjorback LO, Arendt M, Ornbøl E, Fink P, Walach H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: a systematic review of randomized controlled trials. Acta Psychiatr Scand [Internet]. 2011;124(2):102–19 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/21534932.
Chiesa A, Serretti A. Mindfulness-based interventions for chronic pain: a systematic review of the evidence. J Altern Complement Med. 2011;17:83–93.
• Keng SL, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev. 2011;31:1041–56 This study reports the details on how mindfulness is beneficial for psychological health.
Chiesa A, Calati R, Serretti A. Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clin Psychol Rev [Internet]. 2011;31(3):449–64 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/21183265.
• Tang YY, Ma Y, Wang J, Fan Y, Feng S, Lu Q, et al. Short-term meditation training improves attention and self-regulation. Proc Natl Acad Sci U S A. 2007;104(43):17152–6 This study reports the effects of short-term mediatation.
• Zeidan F, Johnson SK, Diamond BJ, David Z, Goolkasian P. Mindfulness meditation improves cognition: evidence of brief mental training. Conscious Cogn. 2010;19(2):597–605 This study reports the benefits of short-term mental training.
Cubillo A, Halari R, Smith A, Taylor E, Rubia K. A review of fronto-striatal and fronto-cortical brain abnormalities in children and adults with Attention Deficit Hyperactivity Disorder (ADHD) and new evidence for. Cortex [Internet]. 2012;48(2):194–215. [cited 2020 Feb 11]; Available from:. https://doi.org/10.1016/j.cortex.2011.04.007.
Passarotti AM, Sweeney JA, Pavuluri MN. Emotion processing influences working memory circuits in pediatric bipolar disorder and attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry [Internet]. 2010;49(10):1064–80 [cited 2020 Feb 11]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/20855051.
Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci. 2011;6(6):537–59.
Barkley RA, Fischer M. Predicting impairment in major life activities and occupational functioning in hyperactive children as adults: self-reported executive function (EF) deficits versus EF tests. Dev Neuropsychol [Internet]. 2011;36(2):137–61 [cited 2020 Feb 12]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/21347918.
Barkley RAMK. Deficient emotional self-regulation in adults with attention-deficit/hyperactivity disorder (ADHD): the relative contributions of emotional impulsiveness and ADHD symptoms to adaptive impairments in major life activities. J ADHD Relat Disord [Internet]. 2010;1(4):5–28 Available from: https://www.semanticscholar.org/paper/Deficient-Emotional-Self-Regulation-in-Adults-With-Barkley-Murphy/79bd6b652d4a145bf9e7bd74c93cf1ff73a309b8.
Mitchell JT, Nelson-Gray RO, Anastopoulos AD. Adapting an emerging empirically supported cognitive-behavioral therapy for adults with AD/HD and comorbid complications: an example of two case studies. Clin Case Stud. 2008;7(5):423–48. https://doi.org/10.1177/1534650108316934 Clin Case Stud. 2009;8(1):95.
Chambers R, Gullone E, Allen NB. Mindful emotion regulation: an integrative review. Clin Psychol Rev. 2009;29:560–72.
Moyer CA, Donnelly MPW, Anderson JC, Valek KC, Huckaby SJ, Wiederholt DA, et al. Frontal electroencephalographic asymmetry associated with positive emotion is produced by very brief meditation training. Psychol Sci [Internet]. 2011;22(10):1277–9 [cited 2020 Feb 12]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/21921291.
•• Zylowska L, Ackerman DL, Yang MH, Futrell JL, Horton NL, Hale TS, et al. Mindfulness meditation training in adults and adolescents with ADHD: a feasibility study. J Atten Disord [Internet]. 2008;11(6):737–46 [cited 2019 Aug 28]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/18025249. This study reports the benefits of mindfulness in adolescents with ADHD.
Haydicky J, Wiener J, Badali P, Milligan K, Ducharme JM. Evaluation of a mindfulness-based intervention for adolescents with learning disabilities and co-occurring ADHD and anxiety. Mindfulness (N Y). 2012;3(2):151–64.
Haydicky J, Shecter C, Wiener J, Ducharme JM. Evaluation of MBCT for adolescents with ADHD and their parents: impact on individual and family functioning. J Child Fam Stud. 2013;24(1):76–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on ADHD
Rights and permissions
About this article
Cite this article
Deshmukh, P., Patel, D. Mindfulness and ADHD (Attention Deficit Hyperactivity Disorder) in Adolescents. Curr Dev Disord Rep 7, 93–99 (2020). https://doi.org/10.1007/s40474-020-00197-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40474-020-00197-8