Abstract
Objectives
Mindfulness-based interventions (MBIs) are increasingly used in adults with attention-deficit hyperactivity disorder (ADHD). The aim of the current study was to conduct a meta-analysis of the available studies on the effects of MBIs on ADHD symptoms, depression, and executive functioning in adults diagnosed with ADHD.
Methods
Screening and selection of peer-reviewed literature using PRISMA-P guidelines on PsycINFO, PubMed, SCOPUS, and ERIC databases from inception to July 2019
Results
A total of 14 studies were included in the meta-analysis, for an aggregated sample of 834 adults with ADHD. Overall, the results showed that MBIs are effective to treat ADHD symptoms in adults, as well as to reduce depression and dysexecutive problems post-intervention.
Conclusions
MBIs are useful to improve ADHD symptoms, negative affect, and cognition in adult ADHD. The results contribute to better understanding and encourage the use of non-pharmacological treatments in ADHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Attention-deficit hyperactivity disorder (ADHD) is characterized by inattention and/or hyperactivity, as well as impulsivity, which negatively affects executive function and emotion regulation (Beheshti et al. 2020; Sprafkin et al. 2016; Vitola et al. 2017). Inattentive or hyperactive/impulsive symptoms must be present in at least two settings, for example, at work and with relatives, and symptoms should be present before the age of 12 years (American Psychiatric Association 2013).
The prevalence of ADHD in adults has been estimated to be about 4.4% (Almeida Montes et al. 2007), and it is higher in males than in females (Amiri et al. 2014; London and Landes 2019). The most common treatment of ADHD consists of the administration of psychostimulant medications. However, pharmacotherapy has its limitations and is not well tolerated by some individuals due to undesirable side effects. This is why there is a search for new, non-pharmacological therapies for ADHD symptoms, including mindfulness-based interventions (MBIs). MBIs have already proven to be beneficial in reducing symptoms of various other mental health problems including depression/anxiety (Franca and Milbourn 2015; Hofmann and Gomez 2017) and substance use disorders (Bautista et al. 2019; Fahmy et al. 2018). Most MBIs involve somatically focused meditative techniques (e.g. seated and walking meditations, body scans, gentle yoga), and non-judgmental, mindful awareness of the present moment.
ADHD is often comorbid with internalizing and externalizing problems (Jacob et al. 2014). Among internalizing behaviors in adult ADHD, negative affect such as anxiety and depression often occur. Regarding externalizing behavior, adults with ADHD show higher novelty-seeking (exploratory interest in response to new stimuli), impulsive decision-making, loss of temper, and aversion to frustration (Downey et al. 1997; Jacob et al. 2007). Internalizing and externalizing behaviors might reflect an underlying emotional dysregulation disorder (Jacob et al. 2007). Moreover, emotional dysregulation is complicated by cognitive distortions (Barlow et al. 2011). Prevalence rates for emotional dysregulation range between 34 and 70% in adults with ADHD (Beheshti et al. 2020; Shaw et al. 2014), especially concerning anger (Able et al. 2007). Moreover, ADHD with emotional dysregulation has been associated with generally more severe inattention and/or hyperactivity (Corbisiero et al. 2017), and worse social or occupational functioning (Surman et al. 2013). Among problems with negative affect, depression (Strohmeier et al. 2016; Yang et al. 2013) and anxiety symptoms (Biederman et al. 2011; Grogan and Bramham 2016; Kessler et al. 2006; Michielsen et al. 2013; Simon et al. 2013) have been consistently associated with adult ADHD. Indeed, between 65 and 89% of all individuals with ADHD suffer from one or more additional psychiatric disorders in adulthood, above all mood and anxiety disorders. This situation complicates the clinical picture in terms of diagnosis, treatment, and outcome measures (Sobanski 2006).
Relative to the general population and ADHD-remitted individuals, those with persistent ADHD have higher rates of comorbid depression and anxiety disorders (Biederman et al. 2011). These comorbid symptoms increase in severity with age (Bramham et al. 2012). Conversely, ADHD symptom rates are elevated among individuals with a primary diagnosis of depression and anxiety disorders (Bron et al. 2016). Thus, we may say that anxiety and depression can contribute to attentional disorders observed in adult ADHD.
In addition to problems with emotion regulation and the comorbidity of depressive and anxiety symptoms, ADHD in adults is characterized by poor executive functioning (i.e., working memory, inhibitory control, switching) (Boonstra et al. 2005; Thorell et al. 2017). Kamradt et al. (2014) found that executive functions (e.g., time management) accounted for relational, professional, and daily living impairments. Consequently, neurocognitive deficits seem to contribute to impoverished interpersonal functioning in adults with ADHD. Clearly, there is a strong association of ADHD with executive deficits and negative affect. This is why it is important to assess these potential outcomes of MBIs in addition to any inattention and/or hyperactivity improvements.
A recent systematic review assessing cognitive and behavioral effects of MBIs on ADHD symptoms showed that there was an improvement on cognitive task performance and ADHD symptoms following MBIs compared with the pre-intervention levels (Poissant et al. 2019). The authors concluded that MBIs might be a valuable treatment option alongside treatment as usual for adult ADHD. However, the authors noted that the quality of studies was variable and questionable, such that several studies showed a high risk of bias (e.g., blinding of participants, random sequence generation, allocation concealment, and attrition rates). Two recent meta-analyses measured the impact of MBIs on children and adults combined (Cairncross and Miller 2016; Xue et al. 2019) or the effects of MBIs and other non-pharmacological treatments combined (López-Pinar et al. 2019) in adults, leaving space for the examination of MBIs in adult ADHD. Furthermore, the aforementioned meta-analyses focused only on inattention and hyperactivity symptoms, except for López-Pinar et al. (2019) who also considered comorbid-internalizing symptoms. Because of the presence of frequent comorbidity with executive dysfunction and emotion dysregulation in the ADHD population, which appear to be aggravated in adulthood, we considered essential to explore the impact of MBIs on these outcomes. We also examined the impact of the quality of studies (risk of bias) on the effect sizes reported in MBIs for adult ADHD.
Methods
Eligibility Criteria
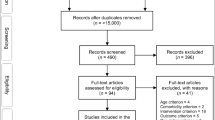
To conduct the meta-analysis, we used the criteria from the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) (Shamseer et al. 2015). A datasheet based on the PRISMA-P was completed with information extracted from each selected study based on (1) research design; (2) the characteristics of participants; (3) the type of the intervention; and (4) outcomes (i.e., “ADHD symptoms,” “depression,” “executive function,” and “emotional dysregulation”). A librarian helped the team to refine the search strategy. A reference manager software was used—EndNote X9 (Bramer 2018). We consulted PsycINFO, PubMed, SCOPUS, and ERIC databases from inception up to July 2019 and we included only “peer-reviewed” literature. For search terms, we followed a shortened, more restrictive version of the keywords from the review on meditation therapies for attention-deficit hyperactivity disorder (ADHD) of Krisanaprakornkit et al. (2010). For example, we excluded terms like vipassana, zen, yoga, pranayama, Sudarshan, and qigong present in the previous review. The search included keywords “ADHD AND meditation OR mindfulness,” “impulsivity,” “inattention,” and “hyperactivity,” in different combinations. We included “randomized” (RCT) and “non-randomized control trials” (N-RCT), “single,” and “comparison studies.” Studies were excluded if they (1) did not examine “treatment” effects; (2) did not include a group of “ADHD” or “ADD” or “hyperactivity disorder”; (3) did not include a “mindfulness” or “meditation-based treatment”; and (4) they were conducted with children but we included “adult,” “college student,” and “young adult.” We included different forms of “MBIs” as long as the intervention contained elements of mindfulness (e.g., “dialectical behavior therapy,” “DBT”). As for outcomes, besides the measures of “ADHD symptoms,” “inattention,” and “hyperactivity,” we included measures of “executive” or “cognitive functioning;” “attention;” and “emotional disturbance or dysregulation,” “depression,” “mood disorder,” and “anxiety.” “Self-rating” scales and “objective tasks” were accepted in the inclusion criteria. Measures of outcomes to assess ADHD symptoms included self-report scales, such as the “Conners’ Adult ADHD Rating Scales” (“CAARS-SR” OR CAARS-S OR the “ADHD Self-Report Scale” (“ASR”)). For executive functioning, objective tasks such as “Attention Network Test” (ANT) OR the “Conners’ Continuous Performance Test” (“CPT”) and subjective questionnaires were considered for inclusion (e.g., the “Behavior Rating Inventory of Executive Function,” “BRIEF”). Self-report measures of anxiety, depression, and other emotional disturbances were also included (e.g., “Beck Depression Inventory” and “Beck Anxiety Inventory”). The final literature search resulted in 721 studies. The search was conducted in three consecutive sessions, from October 2016 to January 2017, updated from April 2018 to July 2018 and finally to July 2019 (plus Google Scholar alerts until November 2019). Abstracts of all articles were included in an Excel file for further examination and updates. We first eliminated 178 duplicates and 1 erratum. Eligibility assessment for final selection was based on independent reviews by H.P. and A.M. After reviewing the abstracts, 458 studies were judged as irrelevant. From the remaining studies, 56 were reviews or meta-analyses and eliminated de facto (but we examined the references). Fifteen studies were conducted with children, adolescents, and/or their parents; therefore, they were excluded. A total of 14 studies conducted in “adults,” “young adults,” and “college students” with ADHD were selected according to all our criteria. The initial sample of studies was further trimmed as a result of the availability of the outcome measures: (a) ADHD symptoms (n = 11), (b) depression (n = 8), and (c) executive functioning (n = 9).
We adopted the Cochrane Collaboration (Higgins et al. 2011) guidelines to score potential bias for each study. The listed biases included (1) “sequence generation” (e.g., Is the allocation sequence of participants acceptably generated?); (2) “allocation concealment” (e.g., Is the allocation of participants acceptably concealed?); (3) “blinding of participants, personnel, and outcome assessors” (e.g., Is knowledge of the allocated treatment plenty prevented during the study?); and (4) “selective outcome reporting” (e.g., Are partial outcome data adequately addressed?). A positive answer indicates a low risk of bias whereas; a negative answer indicates high risk. Cochrane guidelines were chosen because they present a formal quality assessment procedure that we found relevant to the psychological nature (rather than strictly medical nature) of the selected studies. Moreover, the consultation of Krisanaprakornkit et al.’s (2010) Cochrane review (with a step by step demonstration of bias assessment) was used as a handy tool to exercise and practice our comprehension of the assessment of bias and thus limit false interpretation. The search strategy, the overview of a PICO description (i.e., Problem/Patient/Population, Intervention/Indicator, Comparison, Outcome), and the analysis of bias using the Cochrane Collaboration guidelines (O’Connor et al. 2008) for each study are fully described in Poissant et al. (2019).
Statistical Analysis
Comprehensive Meta-Analysis version 3 was used to calculate effect size estimates of the differences in performance scores (means and standard deviations) pre- and post-MBIs (Borenstein 2009; Borenstein and Rothstein 1999). The effect size estimates were calculated using Hedges’ unbiased g, which corrects for bias from small sample sizes (Hedges and Olkin 1985). Effect size estimates were separately calculated for ADHD symptoms, depression scores, and executive functioning. The primary analysis consisted of comparison of pre- to post-MBI scores at different time points to explore impact of MBIs on ADHD symptoms, depression levels, and executive functioning. Also, secondary analyses were conducted to estimate separately the effect size of studies with a comparison group (between-subject comparison) and without comparison groups (single-group pre-posttest comparison) to individually explore the effect of MBIs on ADHD symptoms, depression levels, and executive functioning.
For primary and secondary analyses, the direction of the effect was considered negative if ADHD symptoms and depression scores diminished following MBIs, and positive if ADHD symptoms and depression scores increased following MBIs. Inversely, for executive functioning, the direction of the effect size was considered positive when dysexecutive problems diminished following MBIs, and negative when dysexecutive problems increased following MBIs. According to the conventional standard of Cohen (1988), effect size estimates of 0.2, 0.5, and 0.8 were considered small, moderate, and large, respectively.
The usual way of assessing whether a set of studies are homogeneous is using the Q test. However, the Q test only informs about the presence or the absence of heterogeneity (it does not report on the extent of heterogeneity). The I2 index has been proposed to quantify the degree (true extent) of heterogeneity (Higgins and Thompson 2002). For that purpose, heterogeneity among effect size estimates was assessed with both statistics, that is, the Q test (Paulson and Bazemore 2010) and the magnitude of heterogeneity being evaluated with the I2 index (Lipsey and Wilson 2000). The I2 index describes the proportion of heterogeneity across the studies as low (25%), moderate (50%), and high heterogeneity (75%) (Higgins and Thompson 2002; Higgins et al. 2003). Thus, I2 index of 0 essentially means homogeneity of variance indicating that the pooling of studies in a meta-analysis is highly favorable (“apples with apples comparison”).
As the database was characterized by high heterogeneity, we employed random-effects which are more conservative than fixed-effect models, and appear to better address heterogeneity between studies and study populations (Cooper et al. 2009). To reduce heterogeneity, a composite effect size of all studies was calculated and a cutoff of two standard deviations away from this composite effect size was enforced to exclude outlier results (see below).
To estimate the effect of categorical (e.g., self-report versus other) and continuous variables (e.g., bias level: scores 0–14) on the effects of MBIs, we performed sub-analyses and meta-regression analyses, respectively. The influence of the following variables was investigated for the whole sample of selected studies: (a) “self-report” of ADHD symptoms versus “other” (researcher or relative), and (b) risk of bias or quality assessment. Despite their limitations, trimming procedures are recommended by several groups of investigators and developers (CMA, R, and Cochrane), and it is common practice to apply them. In previous meta-analyses from our research team, we have regularly applied such trimming procedures (seePotvin et al. 2014, 2018; Stavro et al. 2013). Limitations in conducting meta-regression and subgroup meta-analysis on a small number of studies are further discussed below.
Finally, the possibility of publication bias was examined with Begg and Mazumdar’s rank correlation test, and visual inspection of the funnel plot for the whole sample of selected studies (Begg and Mazumdar 1994). We chose this alternative over other options (like Duval and Tweedie’s procedure) relying on other assumptions, such as the observed asymmetry is due to publication bias rather than a “small-study effect.”
Results
Of 721 studies, a total of 14 were included in the meta-analysis, for an aggregated sample of 834 adults with ADHD participating in these studies. The effect sizes were calculated for 11 studies per ADHD symptoms, eight studies for depression and the nine studies for executive functioning. Also, the combined effect size was calculated for the three categories. We first look at effect sizes in each given study with the main focus on ADHD symptoms, depression, and executive functioning, as the main outcomes. Effect sizes were calculated with Comprehensive Meta-Analysis, CMA. We report effect sizes for each study by the outcome, as well as the combined effect sizes. Effect sizes were first examined separately for each outcome type: ADHD symptoms, depressive symptoms, and executive functioning. Secondly, we conducted a sub-group analysis to divide between-group studies (studies with a comparison group) from single-group studies (pre-post studies only).
ADHD Symptoms
Three studies were excluded from the analyses. That is, an outlier with an effect size of more than two standard deviations from the average effect sizes of the rest of the studies (Hesslinger et al. 2002) and two studies that did not report the data needed to be included in the meta-analysis (Cole et al. 2016; Fleming et al. 2015). As shown in Fig. 2a and based on eleven studies, the results showed that following MBIs, the combined effect size showed an improvement in ADHD symptoms (Hedge’s g = − 0.591, 95% CI = − 0.858 to − 0.324, p < 0.0001). The assessment of overall heterogeneity across studies indicated a significantly moderate-to-high heterogeneity (Q = 41.15, df = 10, p < 0.0001; I2 = 75.7%). The Begg and Mazumdar test revealed no publication bias (Tau = − 0.29, p = 0.21) (see Fig. 1).
As shown in Fig. 2b and based on nine studies with comparison groups, the results showed that following MBIs, the combined effect size showed an improvement in ADHD symptoms (Hedge’s g = − 0.610, 95% CI = − 0.988 to − 0.231, p = 0.002). The assessment of overall heterogeneity across studies indicated high heterogeneity (Q = 39.04, df = 8, p < 0.0001; I2 = 79.5%). As shown in Fig. 2c and based on two studies, the results showed that following MBIs, the combined effect size showed an improvement in ADHD symptoms (Hedge’s g = − 0.563, 95% CI = − 0.834 to − 0.292, p < 0.0001). The assessment of overall heterogeneity across studies indicated moderate heterogeneity (Q = 1.986, df = 1, p = 0.159; I2 = 49.6%). The meta-regression results indicated that the overall effect size was not moderated by the estimation based on the risk of bias (β = 0.03, SE = 0.44, p = 0.46). Besides, mixed-effect analyses indicate that the overall effect size was not moderated by the type of informant (i.e., self-report of ADHD symptoms versus other) (Q = 1.38, df = 1, p = 0.24).
Depression
As shown in Fig. 4a and based on a total sample of eight studies, the results showed that following MBIs, the combined effect size showed a diminution in depressive symptoms (Hedge’s g = − 0.462, 95% CI = − 0.648 to − 0.277, p < 0.0001). The assessment of overall heterogeneity across studies indicated moderate heterogeneity (Q = 12.23, df = 7, p = 0.093; I2 = 42.7%). The Begg and Mazumdar test revealed no publication bias (Tau = − 0.32, p = 0.26) (see Fig. 3).
As shown in Fig. 4b and based on five studies with comparison group, the results showed that following MBIs, the combined effect size showed a diminution in depressive symptoms (Hedge’s g = − 0.355, 95% CI = − 0.559 to − 0.151, p = 0.001). The assessment of overall heterogeneity across studies indicated low heterogeneity (Q = 3.194, df = 4, p = 0.526; I2 = 0%). Based on three single-group pre-post studies, Fig. 4c shows the results that following MBIs, the combined effect size showed a diminution in depressive symptoms (Hedge’s g = − 0.650, 95% CI = − 1.058 to − 0.241, p = 0.002). The assessment of overall heterogeneity across studies indicated high heterogeneity (Q = − 8.292, df = 2, p = 0.016; I2 = 75.8%). The meta-regression results indicated that the overall effect size was not moderated by the estimation based on the risk of bias (β = 0.02, SE = 0.06, p = 0.68). Because all scores were self-reported, we did not conduct additional analysis here.
Executive Functioning
Figure 6a is based on a total sample of nine studies indicating an improvement in dysexecutive problems (Hedge’s g = 0.395, 95% CI = 0.136 to 0.653, p < 0.005) following MBIs. The assessment of overall heterogeneity across studies indicated moderate heterogeneity (Q = 19.45, df = 8, p < 0.05; I2 = 58.8%). The Begg and Mazumdar test revealed no publication bias (Tau = 0.000001, p = 1) (see Fig. 5).
As shown in Fig. 6b and based on seven studies with comparison groups, the results showed that following MBIs, the combined effect size showed an improvement in dysexecutive problems (Hedge’s g = 0.260, 95% CI = 0.027 to 0.492, p < 0.05). The assessment of overall heterogeneity across studies indicated low heterogeneity (Q = 8.57, df = 6, p = 0.19; I2 = 30.02%). As shown in Fig. 6c and based on two single-group pre-post studies, the results indicated that following MBIs, the combined effect size demonstrate an improvement in dysexecutive problems (Hedge’s g = 0.810, 95% CI = 0.493 to 1.128, p < 0.001). The assessment of overall heterogeneity across studies indicated low heterogeneity (Q = 1.10, df = 1, p = 0.29; I2 = 9.53%). The meta-regression results indicated that the overall effect size was not moderated by the estimation based on the risk of bias (β = − 0.04, SE = 0.04, p = 0.40).
Discussion
This meta-analysis addresses both negative affect and cognitive functioning of adults with ADHD, in addition to inattention/hyperactivity, following MBIs. Moreover, we controlled our analyses by reporting bias using the Cochrane guidelines (O’Connor et al. 2008). Overall, the results revealed that MBIs are effective to treat global ADHD symptoms in adults supporting previous meta-analyses on the topic. Specifically, following MBIs, inattention and hyperactivity show a moderate reduction in adults with ADHD. Importantly, the risk of bias (quality assessment of studies) did not have a significant impact on the positive effect documented in this meta-analysis. However, a moderate-to-high heterogeneity between studies remains a limitation indicating that this result still needs further confirmation. This meta-analysis also indicates a moderate improvement of depressive symptoms following MBIs. Again, the overall effect size was not affected by the estimation based on the risk of bias. Finally, the results revealed the improvement of the executive functioning in adults with ADHD following MBIs with a low-to-moderate heterogeneity across studies. As with ADHD symptoms and depression, effect size does not appear to be affected by the quality assessment of studies. Finally, publication bias (as measured with the Begg and Mazumdar test) was not found to be significant for any of the three outcomes documented in the current meta-analytic study. However, the small number of considered studies demands caution.
To our knowledge, only Cairncross and Miller (2016) and Xue et al. (2019) have conducted similar meta-analyses with mixed samples of children and adults to measure the impact of MBIs on ADHD symptoms. Cairncross and Miller (2016) found evidence that MBIs were more effective in reducing inattention symptoms. Knowing that adults are more often characterized as inattentive instead of hyperactive, they may show a better response to treatment using MBIs as compared with children. However, the number of studies with adults in their study was very limited (n = 4). Of the eleven eligible studies, Xue et al. (2019) concluded that MBIs had large effects on inattention and hyperactivity/impulsivity. Subgroup analyses between self and other ratings on ADHD symptoms revealed that the effect of MBIs was significant regardless of the rater. Most importantly, Xue et al. (2019) found that the age of the participants significantly affected heterogeneity (adults versus children). The authors suggested that adults may have a better understanding of their condition and thus be more involved in their treatment than children. This was an additional justification for conducting the present meta-analysis with adults only.
Another limitation of the previous studies is the absence of a comprehensive evaluation of the risk of bias other than publication bias. This is an important aspect because it allows identifying studies with poor quality. The current study followed the example of the previous systematic review of Krisanaprakornkit et al. (2010) on meditation therapies for ADHD. By the end of their extensive Cochrane review, they retained only four studies (years 1983, 1987, 2004, and 2006) and could not conclude on the efficacy of any therapies due to insufficient quality of the selected studies. López-Pinar et al. (2019) followed a similar approach to determine the efficacy of different psychotherapies in improving internalizing symptoms such as depression in adults with ADHD. The authors found a significant effect of MBIs (but not dialectical behavior therapy or neurofeedback) to ameliorate emotional dysregulation. It should be mentioned that the authors observed a high risk of bias in the selected studies, which might limit their results.
Overall, the results indicate moderate-to-high heterogeneity among studies, although with a lower heterogeneity for studies addressing executive functions. Heterogeneity is a common problem in previous meta-analyses and can be accounted for by several factors. We included randomized (RCT) and non-randomized control trials (N-RCT). Removing N-RCTs from our analyses could have resulted in more homogeneity, but it would also decrease the statistical power. Another problem may reside in the fact that most participants were receiving medication before and during MBIs, psychostimulants like methylphenidate (MPH) being the most frequently reported. Psychostimulants and other dopamine agonists are commonly used to treat ADHD symptoms; their efficacy is attributed to the inhibition of dopamine and norepinephrine reuptake in the prefrontal cortex (Hosenbocus and Chahal 2012). Comorbidity was present in all examined studies, with major depressive disorders and anxiety disorders being the most frequently reported. Thus, future meta-analyses with more studies should be able to include depression and anxiety as moderators. Other comorbidities, including oppositional defiant disorder, bipolar disorder, borderline personality disorder, and substance abuse, were not frequently reported across the present studies. MBIs were also diverse across studies. They included mindfulness and/or meditation as the main or partial component of the intervention (e.g., that included various adaptations of dialectical behavior therapy, mindful awareness program, and mindfulness-based/cognitive training). The duration of treatment (from 6 to 96 hours) and the degree of experience of therapist (e.g., clinical psychologists, mindfulness instructors, graduate students) also varied considerably across studies. These factors may have acted as confounding variables so it is premature to conclude on the efficacy of one intervention over the other. Another source of heterogeneity arises from the use of self-rating scales versus objective measures of outcomes. Whereas ADHD and depression symptoms were, for the most part, assessed with self-reported scales (e.g., Conners’ Adult ADHD Rating Scale, CAARS-SR, Beck Depression Inventory (BDI)), executive functions were most frequently measured with objective tasks (e.g., Attention Network Test). The existence of a gold standard to assess depression probably accounts for the high homogeneity (I2 = 0%) found in studies with a comparison group for this outcome.
Limitations
One of the main limitations of this meta-analysis is the small number of studies evaluating different outcomes (symptoms, depression, and executive functioning). A small number of studies could limit the statistical power of the statistical analyses (e.g., meta-regressions) and thus the generalizability of the findings. This is meaningful considering that publication bias statistics are generally less appropriate for use in small meta-analyses. Estimates of “self-report” versus “other” and of bias level might as well be tempered by the small number of studies. Also, differences in study design might count for the differences in efficacy. In a previous systematic review, Poissant et al. (2019) found that the majority of studies included in the present meta-analysis were considered at high risk of “selection bias.” Selection bias relates to “random sequence generation” and “allocation concealment.” According to Cochrane Collaboration’s criteria (Higgins et al. 2011), a study is rated as a low-risk study if the way to allocate sequence produces equivalent groups and when the method to conceal the allocation sequence cannot be predicted in advance. Although we did not find a significant impact of the risk of bias on the outcomes, the existence of elevated risk related to random sequence generation, allocation concealment, and blinding of participants and staff requires more consideration. As mentioned by López-Pinar et al. (2019), knowledge of the allocated treatment by participants and/or staff by itself might affect the validity of results. This is a crucial matter since it is not usual or advantageous to blind trainers and participants in this type of interventions. Thus, the risk of bias may be unpreventable. The assessment of the attrition is also of concern since it was found high (or unclear) risk in more than half of the studies in this meta-analysis. The reason for dropout is not specified so it is difficult to decide if it might be related to some incidental reasons or discomfort with treatment.
References
*Selected studies for meta-analysis
Able, S. L., Johnston, J. A., Adler, L. A., & Swindle, R. W. (2007). Functional and psychosocial impairment in adults with undiagnosed ADHD. Psychological Medicine, 37(1), 97–107. https://doi.org/10.1017/S0033291706008713.
Almeida Montes, L. G., Hernandez Garcia, A. O., & Ricardo-Garcell, J. (2007). ADHD prevalence in adult outpatients with nonpsychotic psychiatric illnesses. Journal of Attention Disorders, 11(2), 150–156. https://doi.org/10.1177/1087054707304428.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington: Author.
Amiri, S., Ghoreishizadeh, M. A., Sadeghi-Bazargani, H., Jonggoo, M., Golmirzaei, J., Abdi, S., Safikhanlo, S., & Asadollahi, A. (2014). Prevalence of adult attention deficit hyperactivity disorder (adult ADHD): Tabriz. Iranian Journal of Psychiatry, 9(2), 83–88.
*Bachmann, K., Lam, A. P., Soros, P., Kanat, M., Hoxhaj, E., Matthies, S., Feige B, Müller, H., Özyurt, J., Thiel, C.M., & Philipsen, A. (2018). Effects of mindfulness and psychoeducation on working memory in adult ADHD: a randomised, controlled fMRI study. Behaviour Research and Therapy, 106, 47-56. doi:https://doi.org/10.1016/j.brat.2018.05.002
Barlow, D. H., Ellard, K. K., Fairholme, C., Farchione, T. J., Boisseau, C., Allen, L., & Ehrenreich-May, J. (2011). Unified protocol for the transdiagnostic treatment of emotional disorders. New York: Oxford University Press.
Bautista, T., James, D., & Amaro, H. (2019). Acceptability of mindfulness-based interventions for substance use disorder: a systematic review. Complementary Therapies in Clinical Practice, 35, 201–207. https://doi.org/10.1016/j.ctcp.2019.02.012.
Begg, C. B., & Mazumdar, M. (1994). Opetagins characteristics of a rank correlation test for publication bias. Biometrics, 1088–1101.
Beheshti, A., Chavanon, M. L., & Christiansen, H. (2020). Emotion dysregulation in adults with attention deficit hyperactivity disorder: a meta-analysis. BMC Psychiatry, 20(1), 120. https://doi.org/10.1186/s12888-020-2442-7.
Biederman, J., Petty, C. R., Clarke, A., Lomedico, A., & Faraone, S. V. (2011). Predictors of persistent ADHD: an 11-year follow-up study. Journal of Psychiatric Research, 45(2), 150–155.
Boonstra, A., Oosterlaan, J., Sergeant, J. A., & Buitelaar, J. K. (2005). Executive functioning in adult ADHD: a meta-analytic review. Psychological Medicine, 35(8), 1097–1108. https://doi.org/10.1017/s003329170500499x.
Borenstein, M. (2009). Introduction to meta-analysis. Chichester: John Wiley & Sons.
Borenstein, M., & Rothstein, H. (1999). Comprehensive meta-analysis: a computer program for research synthesis. New Jersey: Englewoods.
Bramer, W. M. (2018). Reference checking for systematic reviews using Endnote. Journal of the Medical Library Association, 106(4), 542–546.
Bramham, J., Murphy, D., Xenitidis, K., Asherson, P., Hopkin, G., & Young, S. (2012). Adults with attention deficit hyperactivity disorder: an investigation of age-related differences in behavioural symptoms, neuropsychological function and co-morbidity. Psychological Medicine, 42(10), 2225–2234.
Bron, T. I., Bijlenga, D., Verduijn, J., Penninx, B. W., Beekman, A. T., & Kooij, J. S. (2016). Prevalence of ADHD symptoms across clinical stages of major depressive disorder. Journal of Affective Disorders, 197, 29–35.
*Bueno, V. F., Kozasa, E. H., da Silva, M. A., Alves, T. M., Louza, M. R., & Pompeia, S. (2015). Mindfulness meditation improves mood, quality of life, and attention in adults with attention deficit hyperactivity disorder. BioMed Research International, Article 962857. doi:https://doi.org/10.1155/2015/962857
Cairncross, M., & Miller, C. J. (2020). The effectiveness of mindfulness-based therapies for ADHD: a meta-analytic review. Journal of Attention Disorders, 24(5), 627–643.https://doi.org/10.1177/1087054715625301.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale: L. Erlbaum Associates.
*Cole, P., Weibel, S., Nicastro, R., Hasler, R., Dayer, A., Aubry, J. M., . . . Perroud, N. (2016). CBT/DBT skills training for adults with attention deficit hyperactivity disorder (ADHD). Psychiatra Danubina, 28(Suppl-1), 103-107. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27663817
Cooper, H., Hedges, L. V., & Valentine, J. C. (2009). The handbook of research synthesis and meta-analysis. New York: Russell Sage Foundation.
Corbisiero, S., Morstedt, B., Bitto, H., & Stieglitz, R. D. (2017). Emotional dysregulation in adults with attention-deficit/hyperactivity disorder-validity, predictability, severity, and comorbidity. Journal of Clinical Psychology, 73(1), 99–112. https://doi.org/10.1002/jclp.22317.
Downey, K. K., Stelson, F. W., Pomerleau, O. F., & Giordani, B. (1997). Adult attention-deficit/hyperactivity disorder: psychological test profiles in a clinical population. Journal of Nervous and Mental Disorders, 185(1), 32–38.
*Edel, M. A., Holter, T., Wassink, K., & Juckel, G. (2017). A comparison of mindfulness-based group training and skills group training in adults with ADHD. Journal of Attention Disorders, 21(6), 533-539. doi:https://doi.org/10.1177/1087054714551635
Fahmy, R., Wasfi, M., Mamdouh, R., Moussa, K., Wahba, A., Wittemann, M., et al. (2018). Mindfulness-based interventions modulate structural network strength in patients with opioid dependence. Addictive Behaviors, 82, 50–56. https://doi.org/10.1016/j.addbeh.2018.02.013.
*Fleming, A. P., McMahon, R. J., Moran, L. R., Peterson, A. P., & Dreessen, A. (2015). Pilot randomized controlled trial of dialectical behavior therapy group skills training for ADHD among college students. Journal of Attention Disorders, 19(3), 260-271. doi:https://doi.org/10.1177/1087054714535951
Franca, R. D., & Milbourn, B. (2015). A meta-analysis of mindfulness based interventions (MBIs) show that MBIs are effective in reducing acute symptoms of depression but not anxiety. Australian Occupational Therapy Journal, 62(2), 147–148. https://doi.org/10.1111/1440-1630.12198.
Grogan, K., & Bramham, J. (2016). Current mood symptoms do not affect the accuracy of retrospective self-ratings of childhood ADHD symptoms. Journal of Attention Disorders, 20(12), 1039–1046.
*Gu, Y., Xu, G., & Zhu, Y. (2018). A randomized controlled trial of mindfulness-based cognitive therapy for college students with ADHD. Journal of Attention Disorders, 22(4), 388-399. doi:https://doi.org/10.1177/1087054716686183
Hedges, L. V., & Olkin, I. (1985). Statistical methods for meta-analysis. Orlando. Montréal: Academic Press.
*Hepark, S., Janssen, L., de Vries, A., Schoenberg, P. L. A., Donders, R., Kan, C. C., & Speckens, A. E. M. (2019). The efficacy of adapted MBCT on core symptoms and executive functioning in adults with ADHD: a preliminary randomized controlled trial. Journal of Attention Disorders, 23(4), 351-362. doi:https://doi.org/10.1177/1087054715613587
*Hesslinger, B., Tebartz van Elst, L., Nyberg, E., Dykierek, P., Richter, H., Berner, M., & Ebert, D. (2002). Psychotherapy of attention deficit hyperactivity disorder in adults-a pilot study using a structured skills training program. European Archives of Psychiatry and Clinical Neuroscience, 252(4), 177-184. doi:https://doi.org/10.1007/s00406-002-0379-0
Higgins, J. P., & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21(11), 1539–1558. https://doi.org/10.1002/sim.1186.
Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327(7414), 557–560. https://doi.org/10.1136/bmj.327.7414.557.
Higgins, J., Green, S., & Cochrane Collaboration (2011). Cochrane handbook for systematic reviews of interventions. Cochrane Collaboration.
Hofmann, S. G., & Gomez, A. F. (2017). Mindfulness-based interventions for anxiety and depression. Psychiatric Clinics of North America, 40(4), 739–749. https://doi.org/10.1016/j.psc.2017.08.008.
Hosenbocus, S., & Chahal, R. (2012). A review of executive function deficits and pharmacological management in children and adolescents. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 21(3), 223-229.
*Hoxhaj, E., Sadohara, C., Borel, P., D’Amelio, R., Sobanski, E., Muller, H., . . . Philipsen, A. (2018). Mindfulness vs psychoeducation in adult ADHD: a randomized controlled trial. European Archives of Psychiatry and Clinical Neuroscience, 268(4), 321-335. doi:https://doi.org/10.1007/s00406-018-0868-4
Jacob, C., Romanos, J., Dempfle, A., Heine, M., Windemuth-Kieselbach, C., Kruse, A., Reif, A., Walitza, S., Romanos, M., Strobel, A., Brocke, B., Schäfer, H., Schmidtke, A., Böning, J., & Lesch, K.-P. (2007). Co-morbidity of adult attention-deficit/hyperactivity disorder with focus on personality traits and related disorders in a tertiary referral center. European Archives of Psychiatry and Clinical Neuroscience, 257, 309–317.
Jacob, C., Gross-Lesch, S., Jans, T., Geissler, J., Reif, A., Dempfle, A., & Lesch, K. P. (2014). Internalizing and externalizing behavior in adult ADHD. Attention Deficit and Hyperactivity Disorders, 6(2), 101–110.
*Janssen, L., Kan, C. C., Carpentier, P. J., Sizoo, B., Hepark, S., Schellekens, M. P. J., . . . Speckens, A. E. M. (2018). Mindfulness-based cognitive therapy vs. treatment as usual in adults with ADHD: a multicentre, single-blind, randomised controlled trial - ERRATUM. Psychological Medicine, 48(11), 1920. doi:https://doi.org/10.1017/S0033291718000776
Kamradt, J. M., Ullsperger, J. M., & Nikolas, M. A. (2014). Executive function assessment and adult attention-deficit/hyperactivity disorder: tasks versus ratings on the Barkley Deficits in Executive Functioning Scale. Psychological Assessment, 26(4), 1095–1105.
Kessler, R., Adler, L., Barkley, R., Biederman, J., Conners, C., Demler, O., et al. (2006). The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. The American Journal of Psychiatry, 163(4), 716–723.
Krisanaprakornkit, T., Ngamjarus, C., Witoonchart, C., & Piyavhatkul, N. (2010). Meditation therapies for attention-deficit/hyperactivity disorder (ADHD). Cochrane Database of Systematic Reviews, 16(6), CD006507. https://doi.org/10.1002/14651858.
Lipsey, M. W., & Wilson, D. B. (2000). Practical meta-analysis. London: SAGE publications.
London, A. S., & Landes, S. D. (2019). Cohort change in the prevalence of ADHD among U.S. adults: evidence of a gender-specific historical period effect. Journal of Attention Disorders, 1087054719855689. https://doi.org/10.1177/1087054719855689.
López-Pinar, C., Martínez-Sanchís, S., Carbonell-Vayá, E., Sánchez-Meca, J., & Fenollar-Cortés, J. (2019). Efficacy of nonpharmacological treatments on comorbid internalizing symptoms of adults with attention-deficit/hyperactivity disorder: a meta-analytic review. Journal of Attention Disorders, 24(3), 456–478. https://doi.org/10.1177/1087054719855685.
Michielsen, M., Comijs, H. C., Semeijn, E. J., Beekman, A. T., Deeg, D. J., & Kooij, J. S. (2013). The comorbidity of anxiety and depressive symptoms in older adults with attention-deficit/hyperactivity disorder: a longitudinal study. Journal of Affective Disorders, 148(2-3), 220–227.
*Mitchell, J. T., McIntyre, E. M., English, J. S., Dennis, M. F., Beckham, J. C., & Kollins, S. H. (2017). A pilot trial of mindfulness meditation yraining for ADHD in adulthood: impact on core symptoms, executive functioning, and emotion dysregulation. Journal of Attention Disorders, 21(13), 1105-1120. doi:https://doi.org/10.1177/1087054713513328
*Morgensterns, E., Alfredsson, J., & Hirvikoski, T. (2016). Structured skills training for adults with ADHD in an outpatient psychiatric context: an open feasibility trial. Attention Deficit and Hyperactivity Disorders, 8(2), 101-111. doi:https://doi.org/10.1007/s12402-015-0182-1
O’Connor, D. A., Green, S. E., & Higgins, J. P. T. (2008). Defining the review question and developing criteria for including studies. In J. P. T. Higgins & S. Green (Eds.), Cochrane handbook for systematic reviews of interventions (pp. 83–94). UK: John Wiley & Sons.
Paulson, J. F., & Bazemore, S. D. (2010). Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. Journal of the American Medical Association, 303, 1961–1969.
Poissant, H., Mendrek, A., Talbot, N., Khoury, B., & Nolan, J. (2019). Behavioral and cognitive impacts of mindfulness-based interventions on adults with attention-deficit hyperactivity disorder: a systematic review. Behavioural Neurology, 2019, 5682050. https://doi.org/10.1155/2019/5682050.
Potvin, S., Stavro, K., Rizkallah, E., & Pelletier, J. (2014). Cocaine and cognition: a systematic quantitative review. Journal of Addictive Medicine., 8(5), 368–376.
Potvin, S., Pelletier, J., Grot, S., Hébert, C., Barr, A. M., & Lecomte, T. (2018 May). Cognitive deficits in individuals with methamphetamine use disorder: a meta-analysis. Addictive Behaviors, 80, 154–160.
*Schoenberg, P. L., Hepark, S., Kan, C. C., Barendregt, H. P., Buitelaar, J. K., & Speckens, A. E. (2014). Effects of mindfulness-based cognitive therapy on neurophysiological correlates of performance monitoring in adult attention-deficit/hyperactivity disorder. Clinical Neurophysiology, 125(7), 1407-1416. doi:https://doi.org/10.1016/j.clinph.2013.11.031
Shamseer, L., Moher, D., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. British Medical Journal (Clinical Research Ed.), 349(1), G7647.
Shaw, P., Stringaris, A., Nigg, J., & Leibenluft, E. (2014). Emotion dysregulation in attention deficit hyperactivity disorder. American Journal of Psychiatry, 171(3), 276–293. https://doi.org/10.1176/appi.ajp.2013.13070966.
Simon, V., Czobor, P., & Bitter, I. (2013). Is ADHD severity in adults associated with the lifetime prevalence of comorbid depressive episodes and anxiety disorders? European Psychiatry, 28(5), 308–314.
Sobanski, E. (2006). Psychiatric comorbidity in adults with attention-deficit/hyperactivity disorder (ADHD). European Archives of Psychiatry and Clinical Neuroscience, 256(1), 126–131.
Sprafkin, J., Steinberg, E. A., Gadow, K. D., & Drabick, D. A. (2016). Agreement among categorical, dimensional, and impairment criteria for ADHD and common comorbidities. Journal of Attention Disorders, 20(8), 665–673. https://doi.org/10.1177/1087054712475083.
Stavro, K., Pelletier, J., & Potvin, S. (2013). Widespread and sustained cognitive deficits in alcoholism: a meta-analysis. Addiction Biology, 18(2), 203–213.
Strohmeier, C. W., Rosenfield, B., DiTomasso, R. A., & Ramsay, J. R. (2016). Assessment of the relationship between self-reported cognitive distortions and adult ADHD, anxiety, depression, and hopelessness. Psychiatry Research, 238, 153–158. https://doi.org/10.1016/j.psychres.2016.02.034.
Surman, C. B., Biederman, J., Spencer, T., Miller, C. A., McDermott, K. M., & Faraone, S. V. (2013). Understanding deficient emotional self-regulation in adults with attention deficit hyperactivity disorder: a controlled study. Attention Deficit and Hyperactivity Disorders, 5(3), 273–281. https://doi.org/10.1007/s12402-012-0100-8.
Thorell, L. B., Holst, Y., Chistiansen, H., Kooij, J. J. S., Bijlenga, D., & Sjowall, D. (2017). Neuropsychological deficits in adults age 60 and above with attention deficit hyperactivity disorder. European Psychiatry, 45, 90–96. https://doi.org/10.1016/j.eurpsy.2017.06.005.
Vitola, E. S., Bau, C. H., Salum, G. A., Horta, B. L., Quevedo, L., Barros, F. C., et al. (2017). Exploring DSM-5 ADHD criteria beyond young adulthood : phenomenology, psychometric properties and prevalence in a large three-decade birth cohort. Psychological Medicine, 47(4), 744–754. https://doi.org/10.1017/S0033291716002853.
Xue, J., Zhang, Y., & Huang, Y. (2019). A meta-analytic investigation of the impact of mindfulness-based interventions on ADHD symptoms. Medicine, 98(23), e15957. https://doi.org/10.1097/MD.0000000000015957.
Yang, H. N., Tai, Y. M., Yang, L. K., & Gau, S. S. (2013). Prediction of childhood ADHD symptoms to quality of life in young adults: adult ADHD and anxiety/depression as mediators. Research in Developmental Disabilities, 34(10), 3168–3181. https://doi.org/10.1016/j.ridd.2013.06.011.
*Zylowska, L., Ackerman, D. L., Yang, M. H., Futrell, J. L., Horton, N. L., Hale, T. S., . . . Smalley, S. L. (2008). Mindfulness meditation training in adults and adolescents with ADHD: a feasibility study. Journal of Attention Disorders, 11(6), 737-746. doi:https://doi.org/10.1177/1087054707308502
Funding
This research was funded by The Quebec Research Funds
Author information
Authors and Affiliations
Contributions
HP designed and executed the study, assisted with the data analyses, and wrote the paper. AM (Moreno) conducted the data analyses and collaborated with the writing of the results section of the study. SP collaborated with the data analyses and editing of the final manuscript. AM (Mendrek) contributed to the systematic review and analysis of bias and editing of the final manuscript.
Corresponding author
Ethics declarations
The manuscript does not contain clinical studies or patient data.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Poissant, H., Moreno, A., Potvin, S. et al. A Meta-analysis of Mindfulness-Based Interventions in Adults with Attention-Deficit Hyperactivity Disorder: Impact on ADHD Symptoms, Depression, and Executive Functioning. Mindfulness 11, 2669–2681 (2020). https://doi.org/10.1007/s12671-020-01458-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-020-01458-8