Abstract
Increasing the number of kidney transplantations results in the trend toward the utilization of marginal but acceptable kidneys for deceased donor renal transplantations (DDRT). At the same time, the acceptance of recipients with high medical, surgical, immunological, or psychosocial risks of poor transplant outcomes as we refer to here as “marginal recipients” has been increasing. The combination of both a low quality donor kidney and marginal kidney transplant recipient leads to unfavorable outcomes during the peri- and post-transplant periods. Since some of the risk factors are non-modifiable, living donor renal transplantation (LDRT) with high-quality kidneys and a well-planned operation could potentially mitigate unfavorable outcomes in high risk marginal recipients. In this article, we review common comorbid conditions and risk factors in marginal recipients. We then discuss the different outcomes between DDRT and LDRT in marginal recipients during the perioperative period and suggest potential strategies for utilizing living kidney organs to mitigate the poor outcomes of DDRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kidney transplantation is the treatment of choice for end-stage renal disease (ESRD) [1, 2]. Since the introduction of calcineurin inhibitors (CNI) in the 1980s, transplant outcomes in the early post-transplant period have improved; however, long-term outcomes have varied depending on several factors including quality of the donor kidneys and comorbidities of the recipients. Since the shortage of donor organs has persisted, the utilization of marginal deceased donor kidneys coupled with an increase in the number of kidney transplant recipients at high risk has resulted in suboptimal survival for both the renal allograft and the kidney transplant recipient. These recipients who carry medical, surgical, immunological, and psychosocial risks are referred to as “marginal recipients” in this article. The outcomes of living donor renal transplantation (LDRT) are generally better than those of deceased donor renal transplantation (DDRT). To improve kidney transplant outcomes and mitigate against the potential for unfavorable kidney transplant results, LDRT should be considered as one of the strategies to improve outcomes in marginal recipients whenever appropriate living kidney donors are available.
We will review the common comorbid conditions of marginal recipients encountered in clinical practice particularly those carrying risks for perioperative complications. Transplant outcomes of these marginal recipients will be discussed. We will also review the advantage of LDRT over DDRT. Some of the risks for poor long-term transplant outcomes generally result from complications of long-term immunosuppression. These include cardiovascular diseases (CVD), diabetes mellitus (DM), hypertension, cancer, and infection. We also suggest an algorithm for selecting the appropriate donors during the prekidney transplant evaluation period.
Marginal Recipient
Definition
Since advanced chronic kidney disease (CKD) and ESRD patients generally have underlying medical comorbid conditions, pretransplant evaluation becomes critical in identifying them. It also provides an opportunity to correct or minimize those conditions that adversely impact perioperative surgical-related and post-transplant medical complications. In addition, psychosocial factors need to be taken into consideration. These comorbid conditions, which could be either modifiable or non-modifiable, determine the candidacy of a patient for kidney transplantation. After completion of the pretransplant evaluation, patients are grouped into excellent, acceptable but high-risk, or unsuitable candidates for kidney transplantation. The latter group of patients has an absolute contraindications for kidney transplantation [3•, 4–9].
In this review, the acceptable but high-risk candidate for kidney transplantation is defined as a marginal recipient. These recipients commonly have significant medical and/or psychosocial conditions that potentially can cause perioperative medical and/or surgical complications which subsequently lead to poor short- and long-term transplant outcomes in both renal allograft and patient survivals. Table 1 summarizes the common medical and psychological conditions encountered in advanced stage CKD and ESRD patients. A single comorbid condition may not necessarily define the patient as a marginal recipient; however, combined multiple comorbid conditions in a borderline or low functional capacity patient such as an elderly candidate may make the patient a marginal recipient.
Common Conditions Leading the Patients to Become Marginal Recipients
Major underlying medical conditions that commonly lead to perioperative and post-transplant complications include CVD, peripheral arterial disease (PAD), pulmonary disease, metabolic diseases especially obesity, high sensitization, and advanced age.
CVD
CAD
CKD and ESRD are major risk factors for CVD, the most common cause of morbidity and mortality in kidney transplant recipients [10]. Around 50 % of long-term renal allograft loss is from death with a functioning allograft (DWFG), and the majority of DWFG is secondary to CVD [11].
A retrospective analysis using the United States Renal Data System (USRDS) and the United Network for Organ Sharing (UNOS) from 1995 to 2002, which included 105,181 kidney transplant patients, showed that 20,371 patients were diagnosed with CVD. CVD was defined as the presence of at least one of the following diagnoses: cardiac arrest, myocardial infarction, dysrhythmia, congestive heart failure, ischemic heart disease, peripheral vascular disease, or unstable angina. CVD was associated with 1.12 and 1.41 times decrease in allograft and recipient survival times, respectively. Moreover, renal allograft failure was significantly higher in the recipients with CVD at the time of onset of ESRD [12].
Severe Cardiomyopathy
ESRD patients who have severe ischemic cardiomyopathy may not be a candidate for kidney transplantation but should be considered for a combined heart-kidney transplantation if cardiac conditions are expected to irreversibly decline soon after kidney transplantation [13]. Approximately 8 % of renal transplant recipients are allocated from the combined heart-kidney transplant waiting list [14••].
Even the prognosis for some patients with severe cardiomyopathy can be improved with kidney transplantation. For example, structural and functional abnormalities related to ESRD, so-called uremic cardiomyopathy, are common among ESRD patients who are on dialysis and include left ventricular hypertrophy and systolic dysfunction [15••, 16••, 17–20]. Although perioperative cardiac complications are higher in the recipients with severe ischemic cardiomyopathy, successful kidney transplantation has been associated with increased left ventricular ejection fraction. Improved post-transplant hemoglobin has also been associated with improved cardiac function and favorably predicts patient survival. Therefore, candidates with severe ischemic cardiomyopathy (ejection fraction <30 %), even though considered high risk, should be carefully evaluated and not necessarily excluded from kidney transplantation solely on the basis of poor cardiac function [15••, 19].
Valvular Heart Disease
Calcification of cardiac valves, especially mitral and aortic valves, is common in ESRD patients and is associated with abnormalities of calcium and phosphate metabolism [21]. One retrospective observational study demonstrated a decreased rate of kidney transplantation in ESRD patients with valvular heart disease, whereas the rate did not decrease in those undergoing pretransplant valve replacement surgery [22]. Moreover, post-transplant valve replacement was associated with a 20 % per year higher mortality. There were no statistically significant differences in 2-year patient survival between tissue and non-tissue valves (61.5 vs. 59.5 %) [23]. Therefore, uncorrected valvular heart disease leads to poorer transplant outcomes.
Arrhythmia
Atrial fibrillation (AF) is a very common arrhythmia in both the general population and kidney patients and leads to worse transplant outcomes. In a retrospective study of 62,706 kidney transplant recipients, 3794 patients (6.4 %) had preexisting (AF). There was a higher prevalence of death, graft failure, death-censored graft failure, and ischemic stroke in the patients with AF compared to those without AF. Since preexisting AF is associated with poorer transplant outcomes, the arrhythmia should be one of the main focuses for cardiac risk stratification during the pretransplant evaluation [24•].
Hypertension
Hypertension is another well-known traditional risk factor of CVD in both the pretransplant and post-transplant periods. Pretransplant hypertension is associated with post-transplant hypertension [25]. However, there is no recommended optimal blood pressure for ESRD patients who are on the transplant waiting list [4, 6, 26, 27]. Molner et al. conducted a retrospective study by using data from the Scientific Registry of Transplant Recipients (SRTR) which included 13,881 kidney transplant patients followed for a 5-year period. Predialysis diastolic blood pressure <50 mmHg and post-dialysis systolic blood pressure <110 was associated with higher post-transplant survival. However, post-transplant mortality was increased with increased post-dialysis diastolic blood pressure of ≥100 mmHg. Low pretransplant blood pressure and post-dialysis systolic blood pressure of <110 mmHg were associated with a lower risk of death-censored graft loss [28••]. Other retrospective studies also demonstrated poor transplant outcomes in pretransplant hypertensive patients [6, 29, 30] especially in African-American who are at higher risk of graft loss [30, 31].
PAD
PAD defined as peripheral arterial bypass or critical limb ischemia requiring amputation is commonly associated with CKD and ESRD, particularly patients with DM [32–34]. One retrospective study demonstrated the incidence of de novo PAD was 3.2 % and post-transplant PAD in the recipients with pretransplant PAD was up to 57 %. PAD was associated with shorter 10-year renal allograft and patient survival as well as increased DWFG [35]. Another larger retrospective study of 43,427 adult transplant recipients also revealed an almost twice greater incidence of de novo PAD post-transplantation as well as an increased risk of mortality in kidney transplant recipients with and without DM [36].
Pulmonary Diseases
The common underlying pulmonary diseases in ESRD patients are chronic obstructive pulmonary disease (COPD), obstructive sleep apnea, and smoking. Among these, smoking is a modifiable risk factor and is associated with 30 % greater risk of renal allograft failure in the patient with more than 25-pack-year history of smoking. Reduction of renal allograft failure was decreased to 34 % if the patient quit smoking 5 years before kidney transplantation. In addition, smoking leads to increased mortality and DWFG [37]. Smoking is a known risk factor for coronary artery diseases (CAD), cerebrovascular disease, PAD, and malignancy especially lung cancer. It is a relative contraindication for kidney transplantation in one guideline due to its potential psychosocial effect that may jeopardize kidney transplantation [5]. Other guidelines agree that active smoking is not an absolute contraindication for kidney transplantation, but pretransplant smoking cessation is recommended and should be offered for all active smokers [3•, 4, 6–9].
Metabolic Diseases and Obesity
DM
DM is one of the most common causes of ESRD in the USA and the most common cause of renal disease leading to kidney transplantation. Since DM patients generally have concomitant CAD and PAD as well as other traditional cardiovascular risks such as hyperlipidemia and obesity, evaluation and work-up for CVD in DM patients are warranted. In the post-transplant period, glycemic control is critical and very challenging since multiple immunosuppressive medications potentially worsen glycemic control and cause postoperative complications such as poor surgical wound healing or postoperative infections.
Simultaneous pancreas-kidney transplantation (SPK) is another option for type 1 DM patients with ESRD, although some transplant centers also perform SPK in type 2 DM. Given the high-risk of the operation, SPK can potentiate poor outcomes in the diabetic patient if an unsuccessful transplant occurs. Survival benefit and quality of life are the major advantage of SPK compared with dialysis [38]; however, it is unclear whether the survival advantage is from a well-functioning renal allograft as there is a lack of well-randomized control studies. During the first year after SPK transplant, the patients may encounter complications related to technical failure, post-transplant allograft thrombosis, post-transplant gastrointestinal side effects, high immunosuppression, prolonged initial hospital stay, and readmission.
Hyperlipidemia
Hyperlipidemia is a known traditional risk factor of CVD in the general population. Since vascular lesions in experimental models of CAD were associated with higher cholesterol levels [39], several studies have demonstrated a correlation between pretransplant and post-transplant lipid profile abnormalities and transplant outcomes including chronic allograft dysfunction. A prospective study of 151 kidney transplant recipients revealed that pretransplant total cholesterol, low-density lipoprotein (LDL) cholesterol, and LDL triglyceride were associated with renal allograft loss at 6 months post-transplant. In addition, high pretransplant serum cholesterol ≥6.9 mmol/l was associated with acute rejection, worse graft function, vascular intimal hyperplasia, and glomerular mesangial changes detected by 6 months post-transplant biopsies as well as elevated serum creatinine >160 mmol/l at 6 months post-transplant [40]. Chronic allograft dysfunction with transplant vasculopathy from protocol biopsies at 3 months post-transplant could be strongly predicted by pretransplant total cholesterol levels [41]. Another study with longer follow-up showed high cholesterol level at pretransplant and at 6 months post-transplant was associated with poorer renal allograft function at 2 years [42]. Post-transplant elevated lipid profiles are also associated with poor renal allograft outcomes. In addition, post-transplant hypertriglyceridemia [43, 44] and fibrinogenemia [44] were independent risk factors for chronic allograft dysfunction. A more recent study showed pretransplant and post-transplant triglyceride, and lipoprotein A levels were both associated with chronic allograft dysfunction [45].
As the data shows, hyperlipidemia is a risk factor for not only CVD during the perioperative period, but it also predicts long-term renal allograft outcomes. Therefore, hyperlipidemia, a commonly overlooked comorbid condition, should be aggressively treated in both the pretransplant and post-transplant periods.
Obesity
Based on a meta-analysis of 21 studies involving 9296 patients, obesity was associated with delayed graft function (DGF). If only the studies conducted after year 2000 were used, obesity did not increase the incidence of renal allograft loss or mortality, but it was a risk factor for dying from CVD [46••]. Obesity is also a risk factor of delayed surgical wound healing, post-transplant hyperglycemia or DM, and other postoperative complications. Obesity defined as body mass index (BMI) >30 kg/m2 is not a contraindication for kidney transplantation, but obese patients should be carefully screened for CVD risks and offered a weight reduction program [6, 7]. For those patients whose BMI is greater than 40 kg/m2, kidney transplantation is unlikely to provide benefit [8, 47].
Elderly, Frailty, and Cognitive Impairment
Since the number of elderly continues to increase, common comorbid conditions as mentioned above are also more prevalent in this population. The phenotype of frailty was first described in 2001 and is an important topic in Geriatric Medicine with readily defined features. Among the transplant community, frailty as well as functional status are subjectively assessed during the pretransplant evaluation. Frailty is objectively defined by containing at least three of the following features: unintentional weight loss (10 lbs in the past year), self-reported exhaustion, weakness (grip strength), slow walking speed, and low physical activity [48]. One single-center, prospective study reported a 1.94-fold risk of DGF in kidney transplant recipients with pretransplant frailty [49]. Retrospective studies from the same group demonstrated a 61 % higher risk of hospital readmission within 30 days of initial post-transplant discharge and 2.17-fold increased mortality in frail kidney transplant recipients regardless of age [50••, 51••]. In addition to impaired functional status, which was diagnosed on the basis of frailty, impaired cognitive function is another significant risk factor of poor kidney transplant outcomes in the elderly. Although there is no standard objective method to assess frailty and cognitive impairment, our kidney transplant center routinely screens for impaired functional status and evaluates cognitive function by using the “Timed up and go test” (TUG) and the Montreal cognitive assessment (MoCA), for elderly patients ≥65 years old or any patients who have evidence of limited functional status or cognitive impairment. These screening tools guide our transplant team to triage and refer the patients to a geriatrician and/or neuropsychiatrist for further work-up.
The Highly Sensitized Patient
Acquired human leukocyte antigen (HLA) antibodies occur in the following three settings: blood transfusion, pregnancy, or prior transplantation. A large prospective multi-center trial demonstrated that 1-year graft survival was significantly lower in kidney transplant recipients with HLA antibodies than those without the antibodies (6.6 vs. 3.3 %). In recipients with de novo HLA antibodies, graft survival was also shorter than those without the antibodies (8.6 vs. 3.0 %) [52]. More details about sensitization will be discussed below.
Psychosocial Situations Also Lead Patients to Become Marginal Recipients
Three main psychological issues that are routinely assessed during the pretransplant evaluation include behavioral, socioeconomic problems, and health disparity. Many kidney transplant centers carefully identify these issues and refer the patients to a psychiatrist, psychologist, psychosocial rehabilitation, or behavioral management if indicated. Although psychosocial barriers are not a common reason to exclude some patients for kidney transplantation, some kidney transplant recipients who underwent successful kidney transplantations reveal underlying behavioral or psychological problems that are manifested by non-medication adherence, lack of treatment motivation, failure to follow-up, or lack of social support. Often, these lead to loss of renal allograft from rejection, immunosuppressive medications-related complications, or high morbidity and mortality.
Transplant Disparity
Health disparity is defined as a particular type of difference in health or in the most important influences on health that could potentially be shaped by policies; it is a difference in which disadvantaged social groups (such as the poor, racial/ethnic minorities, women, or other groups that have persistently experienced social disadvantage or discrimination) systematically experience worse health or greater health risks than more advantaged groups [53].
Transplant outcomes are affected by sociocultural (racial/ethnic, gender, age, educational), socioeconomic (income, insurance), and geographic disparities [54]. In this current review, racial and ethnic disparities are discussed.
Blacks and Hispanics
Overall, renal allograft function and graft survival are lower in black recipients than others [55–60]. Chronic allograft nephropathy is also higher [61]. These poorer outcomes in black recipients are also seen in terms of patient survival [2, 62, 63]. The reasons for these differences are likely multifactorial [64] and involve the interplay between immunological and non-immunological factors.
Compared to Hispanics and Asian populations, black recipients have a greater variation of HLA polymorphisms, immune responses, and immunosuppressive medication requirements [56, 65–69]. Drug absorption also differs among different ethnicities, and Blacks may have lower drug absorption for unknown reasons [70–72].
For non-immunological factors, comorbid conditions, time on dialysis, donor characteristics, organ characteristics, socioeconomic status, medication adherence, access to care, and health policies contribute to transplant outcomes [31, 63, 73–75]. These factors are worse in Blacks and Hispanics. In addition, they are less likely to receive preemptive kidney transplantation and more likely to stay longer on the waiting list [63, 76, 77].
Since there is an increase in transplantation in the elderly, one large retrospective study focusing on racial disparity showed that racial and ethnic disparities affect transplant outcomes in the elderly which was similar to other age groups. Graft failure was higher in elderly blacks than whites; however, patient survival was greater in the black population as compared to white recipients. Moreover, the “Hispanic paradox” in which Hispanics have equal or lower mortality than non-Hispanic whites despite having a lower economic status persists in this elderly population [75, 78••, 79]. In contrast, Asians, a minority of this cohort, had the longest renal allograft and patient survivals [78••].
Non-adherence
Adherence is a combination of compliance and persistence [80]. Compliance in adhering to the prescribed medication regimens requires consistency and accuracy [81]. Persistence relates to the perseverance that the patients must maintain in following a drug regimen until it is discontinued [81]. Several studies have demonstrated the significant impact of non-adherence on renal allograft survival [82–86]. Compared with adherent recipients, the non-adherent had 7-fold greater risk of renal allograft failure. This is important because approximately 30 % of kidney transplant recipients do not adhere to taking their medications [82, 87•, 88]. One prospective study demonstrated that acute antibody-mediated rejection (ABMR) was correlated with non-adherence in up to half of the transplant patients. This study examined the causes of renal allograft loss from 315 recipients with “for cause” transplant renal biopsies. Rejection accounted for the majority of the graft losses (64 %), and ABMR occurred in every case of rejection loss. Forty-seven percent of rejection losses were linked to non-adherence [89]. A more recent study also demonstrated that non-adherence was a predictor of de novo donor-specific antibody (DSA) (OR 8.75), which leads to poor graft outcomes. This study showed that 15 % of 315 recipients without pretransplant DSA developed de novo DSA and recipients with de novo DSA had a lower median 10-year graft survival compared to those without de novo DSA [90].
In addition to non-adherence, self-management is very important in successful health outcomes particularly for the management of a highly complex immunosuppressive medication regimen. Self-management is undertaken by the patient in order to live with a chronic condition(s). It requires having the confidence to deal with medical management by understanding his or her role and being emotionally ready to manage his or her condition [91].
Recent meta-analysis of 50 studies including 1238 recipients aged 18 to 82 years showed the critical role of self-sufficiency in optimizing transplant outcomes. Several interventions promoting the recipients’ self-management and adherence include personalized care planning, education, psychosocial support, decision aids, self-monitoring, and pragmatic tools that may improve transplant outcomes [92••].
Why Living Donor Renal Transplantation?
An increase in the demand of donor kidneys leads to several strategies to enhance available organs. By utilizing marginal kidneys for non-conventional DDRT, the discard rate for offered organs has been decreasing. However, DDRT may not always lead to acceptable outcomes, particularly from marginal donor organs. If DDRT is performed in marginal kidney transplant recipients, transplant outcomes in terms of renal allograft and patient survival will be even poorer.
LDRT is another way to overcome these barriers. It provides a high-quality organ, while allowing adequate preparation for surgery. The living donor kidney is culled from carefully and thoroughly well-screened healthy individuals who are related or unrelated to the recipient. Since the majority of ESRD patients have several comorbidities and are more than likely to be marginal recipients, LDRT should strongly be considered as a strategy to mitigate against poor transplant outcomes.
Although short-term, 1-year survivals are not different for DDRT and LDRT, there is a greater long-term (3 years) renal allograft and patient survival for LDRT as compared to DDRT [93•].
The source of a donor kidney is one of the most important factors determining transplant outcomes. In this article, we review data related to transplant outcomes of DDRT and LDRT in marginal recipients with different comorbid conditions.
Uniformly Healthy Living Donor Kidneys Versus Universally Injured Deceased Donor Kidneys
Terasaki reported a retrospective study comparing the 3-year renal allograft survival between different types of donor kidneys. Kidney transplantation from an HLA-identical sibling led to the highest graft survival [94]. Comparing LRRT and LURT, there was similar allograft survival from parent-donor grafts with one HLA-haplotype mismatch and LURT with two HLA-haplotype mismatches and higher survival than DDRT with two HLA-haplotype mismatches [94–98]. Although the average numbers of HLA-A, B, and DR mismatches in LURT and DDRT were 4.1 and 3.6, respectively, LURT had greater renal allograft survival. Therefore, it was not immunological factors but a uniformly healthy kidney donor that was the main factor for better renal allograft outcomes in LDRT [94].
As we know, every deceased donor kidneys has some degree of acute kidney injury. In addition, the underlying condition of the deceased donor kidney varies. A combination of these factors leads to classification of deceased donor kidneys into standard criteria deceased donor (SCD), expanded criteria donor (ECD), donation after brain death donor (DBD), and donation after circulatory death donor (DCD). In general, renal allograft survival for all of these types of donor kidneys is less than from a donor from an LDRT.
There are several important factors contributing to transplant outcomes from DDRT. Although there is a high possibility of an HLA-haplotype mismatch from the donor kidney, donor kidney function is always affected by physiological changes from brain death, long cold ischemic time (CIT), and ischemic reperfusion injury [61, 99]. Two main reasons for the poor outcomes of DDRT are related to the donor kidney source and mechanism of injuries from inflammatory process sustained during brain and/or cardiac death leading to DGF.
As previously mentioned, renal allograft survival of DDRT and LURT was similar if the DDRT was functioning on the first day. Otherwise, DGF is the main unfavorable factor for poorer renal allograft outcomes in DDRT [94]. Not only does the presence of DGF lead to unfavorable renal allograft function, but also prolonged duration of DGF also worsens transplant outcomes. A single-center retrospective study from Brazil demonstrated that the longer the duration of DGF, the worse the 1-year renal allograft function, allograft loss, and patient survival [100••].
Apart from traditional risk factors for CVD, impaired renal allograft function is also a CVD risk as a result of immunosuppressive medications, graft rejection, graft dysfunction, and anemia [101]. DGF, which commonly occurs in DDRT, is an important risk factor for renal allograft rejection, dysfunction, and CVD. Increased immunosuppression with corticosteroids for acute rejection increases cardiovascular risk [102, 103]. In non-transplant patients, declining renal function is associated with a higher risk of death and cardiovascular events [104]. Similar results were found in the Assessment of Lescol in the Renal Transplantation (ALERT) trial. There was a higher independent risk for all-cause, non-cardiovascular and cardiac mortality, major adverse cardiac event, and graft loss in transplant recipients with elevated baseline serum creatinine [105]. Post hoc analysis of the Folic Acid for Vascular Outcome Reduction in Transplantation (FAVORIT) trial also showed an increased risk of post-transplant CVD and death in patients with a lower estimated glomerular filtration rate (eGFR) [106]. Other biomarkers related to renal dysfunction such as proteinuria, homocystinemia, and vascular calcification are also associated with increased cardiovascular risk and mortality [107–112]. Overall, renal allograft rejection and dysfunction lead to renal allograft failure, returning to dialysis, and significantly higher mortality [113]. A well-functioning renal allograft from a high-quality living donor kidney will avoid DGF and improve transplant outcomes.
Well-Prepared Operation of LDRT Versus An Elective Surgery Performed Under Emergent Conditions
Timing is critical in determining transplant outcomes. One of the most crucial factors contributing to DGF in DDRT is CIT. Several reasons for CIT in DDRT evolve from the procurement and surgical process.
Recipient Conditions
For DDRT, the potential kidney transplant recipients may not be in optimal condition for receiving a transplant. Some unsuitable acute conditions for surgery such hyperkalemia, volume overload, or other electrolyte disturbance require pretransplant dialysis and potentially prolongs CIT. As such, the operation may need to be performed under emergent conditions.
Although transplantation from any type of donor kidney provides renal allograft survival benefit, DDRT leads to the worst outcomes. In addition, long-term renal allograft survival (5-years) is greater in the renal transplant recipients with preemptive kidney transplantation or <1 year on dialysis [114]. Given the prolonged average waiting time in the USA, the majority of recipients receiving a preemptive kidney transplant or a transplant shortly after initiating dialysis most likely undergo LDRT. Prior kidney donors and those patients waiting on a combined organ transplant list also receive higher priority on the kidney transplant list and may receive a kidney transplant (DDRT) with less than 1 year on dialysis. In general, it is more likely that preemptive kidney transplantation will occur almost exclusively in LDRT.
Donor and Organ Procurement Process
Similar to the recipient, donors need to be in acceptable health in order to donate a kidney. With careful evaluation, living kidney donors are universally healthy.
In contrast, time of organ procurement for DDRT is generally unpredictable and deceased donor kidneys are always affected by some degrees of inflammation and pathophysiological changes from brain death. This causes prolonged CIT and DGF.
Surgical and Medical Staff
LDRT provides opportunities in determining an appropriate time for not only donors and recipients but also surgical and medical staff to arrange the most suitable time for operation.
In addition to an unpredictable procurement process, an unscheduled operation and lack of staff during non-working hours can potentially lead to delay in kidney transplantation and subsequently result in prolonged CIT and DGF for DDRT.
Improved Transplant Outcomes by LDRT in Marginal Kidney Transplant Recipients With/Without Modifiable Perioperative Risks
CAD
Timing is critical in the pretransplant evaluation process and determines the onset of activation on the transplant waiting list particularly in the patients having or at risk for cardiac disease
Not only increasing the posttransplant complications, cardiac work-up and therapeutic interventions are one of the main reasons that the patients with CVD require to be inactive on the waiting list. Cardiac risk stratification during always involves in extensive cardiovascular work-up [115]. Even though the benefit of screening for CVD in asymptomatic patients is still unclear due to limited data from observational studies with inconsistent results, screening and eventual therapeutic interventions are very common in practice [116•]. The work-up includes echocardiography, exercise or pharmacological cardiac stress tests, or cardiac catheterization. If the patients need further definitive therapeutic intervention such as percutaneous transluminal coronary angioplasty (PTCA) with stent placement or coronary artery bypass grafting (CABG), after successfully treated, they needs post-procedure recovery period particularly when the patients require dual antiplatelet therapy which may take 1 or up to 12 months for bare metal or drug-eluting stent placements, respectively [32, 117, 118].
The appropriate waiting time for kidney transplantation following coronary stent placement may be challenging with DDRT since the time of organ availability is unpredictable. For instance, cardiac stent thrombosis is common in the first 2 weeks following the intervention and very rare after 4 weeks after BMS placement [119, 120]. The optimal waiting time for surgery is between 3 and 6 months after BMS placement in order to allow endothelialization to occur and avoid restenosis [115]. As a result, kidney transplantation is necessarily postponed, and the patients stay longer on the waiting list. Increased cumulative cardiac and non-cardiac complications occur from the longer stay on dialysis. Since organ availability is unpredictable in DDRT, LDRT shortens the time on dialysis and allows for a well-planned operation.
CVD impacts all renal transplant recipients irrespective of their age. ESRD is a cardiovascular risk factor, and CVD commonly exists in the ESRD population. Successful kidney transplantation does not correct non-modifiable cardiovascular risks; on the other hand, it could potentially worsen the preexisting risks or introduce new risks. Advancing age is a traditional risk for CVD, and the elderly are more likely to have pretransplant CVD than younger recipients. However, increased utilization of ECD kidneys may worsen outcomes especially from CVD mortality in any age group particularly in young recipients. In a recent study using data from the Australian and New Zealand Dialysis and Transplant Registry from 1997 to 2009 showed that young recipients age <60 years old who received ECD kidneys had a higher risk of all-cause mortality and DWFG compared with those received SCD kidneys. CVD was the major cause of mortality. Interestingly, there was no significant difference in mortality in the elderly (age ≥60 years old) with ECD compared to those with SCD [121••].
Hypertension
Although there is no recommended pretransplant blood pressure, there are some studies about post-transplant blood pressure and its relationship to transplant outcomes. The results of these studies provide us with guidance regarding optimal post-transplant blood pressure control. There is a 17–18 % increased risk of transplant failure and mortality for each 10 mmHg increase in post-transplant systolic blood pressure [122]. Animal models and human studies have demonstrated that the kidney plays a partial role in mediating genetic hypertension [123]. Curtis et al. demonstrated that six kidney transplantations (two LRRT and four DDRT) lead to normalization of post-transplant blood pressure without the need for antihypertensive medication in all six recipients who had ESRD secondary to hypertensive nephrosclerosis [124]. In another observational study, 85 kidney transplant recipients with pertinent family history of hypertension in both donors and recipients were followed on average for 8 years. Recipients who had no family history of hypertension and received a kidney transplant from donors who had family history of hypertension required more antihypertensive medications as compared with those recipients who had no family history of hypertension and received a kidney transplant from a donor without a family history of hypertension. However, the difference did not exist in the recipients with a family history of hypertension. Additionally, recipients without a family history of hypertension who received a transplant from a donor with a history of hypertension required ten times greater antihypertensive medications as compared with those receiving normotensive kidneys [125, 126]. These same patients also had higher diastolic blood pressures and more severe renal damage during acute rejection [127].
Since the increasing use of ECD kidney with a higher prevalence of history of hypertension in the donors, DDRT conveys the risk of hypertension in recipients. On the other hand, LDRT, which is rarely performed from living donors with hypertension, usually mitigates the risk of post-transplant hypertension in the recipients.
Regardless, both recipients from LDRT and DDRT should not have aggressive blood pressure control during the immediate pretransplant period. One retrospective study of 142 young kidney transplant recipients (mean age, 29.7 ± 9.43 years, 114 LRRT and 28 DDRT) showed that pretransplant systolic blood pressure <120 mmHg was significantly associated with DGF particularly in LDRT [128].
Diabetes Mellitus
There are several transplant options for type 1 DM (and some type 2 DM) patients with ESRD including kidney transplantation alone (KTA), SPK, and pancreas after kidney transplantation (PAK). Each of these modalities has different patient and allograft survival benefits. Overall, these transplant options lead to better patient survival compared with dialysis.
Compared with KTA, patients undergoing SPK have lower mortality only when compared with DDRT but not with LDRT [129–131]. However, patients with SPK with a functioning pancreatic allograft 1 year post-transplant have the highest survival benefit than LDRT, followed by SPK without functioning graft, and then DRRT [132]. PAK (after LDRT) that occurs within the first year post-kidney transplantation does not increase survival benefit but does increase initial mortality compared with KTA (with LDRT) with a functioning renal allograft at 1 year [133].
For renal allograft survival, patients with SPK have the same renal allograft survival compared with LDRT and it is higher than DDRT [134]. This renal allograft benefit for the recipients undergoing SPK with a functioning pancreatic graft at 1 year is higher than the benefit in those undergoing DDRT and LDRT; however, renal allograft failure and mortality are higher in SPK with a failed pancreatic graft at 1 year [132]. With regard to the long-term renal allograft outcomes of SPK, the renal allograft is less likely to fail after 10 years post-transplant compared with DDRT [135]. In the minority of type 1 diabetes patients who are relatively young, preemptive SPK may occur and this can increase renal allograft [136] and patient survival [137].
In summary, SPK for type 1 DM patients leads to the same patient and renal allograft outcomes as compared with living donor KTA, but SPK with a 1-year functioning pancreatic graft will provide the higher benefit. Outcomes of SPK are worse when the pancreatic graft fails within 1 year post-transplant. Patient and renal allograft outcomes are better in LDRT than DDRT, and preemptive transplantation of both SPK and KTA improves transplant outcomes.
Preemptive KTA is more likely to occur in LDRT than in DDRT, and LDRT has better transplant outcomes as compared with DDRT. Consequently, LDRT definitely mitigates the potential unfavorable transplant outcomes of DDRT in DM patients.
However, given the survival benefit of ECD kidney compared with dialysis, DM patients should be offered ECD kidneys if the organs are allocated in the organ procurement organizations (OPO) with short waiting times. Moreover, in OPOs with long waiting times, ECD kidneys provide significant survival benefit for patients older than 40 years of either sex and race, un-sensitized patients, and those with diabetes or hypertension [138].
Elderly and Frailty
Utilizing ECD or high KDPI kidneys has been one of the strategies to increase the number of kidney transplants in the elderly in order to increase life expectancy and longevity. This dovetails with previous data demonstrating that elderly kidney transplant recipients older than 65 years old had survival benefit when they received kidney transplants within 2 years of ESRD. This benefit is comparable between ECD and SCD kidney transplantations (5.6 vs. 5.3 years of longer life expectancy). However, it is a common scenario that these elderly patients will not receive a kidney transplant within 2 years of dialysis initiation because of underlying comorbid conditions that need to be corrected. Elderly candidates may even be delisted because of death or new conditions that prevent them from receiving a kidney transplant. Since the average deceased donor kidney waiting time in the USA is around 3–5 years, the majority of these elderly patients are unlikely to receive DDRT within 2 years of dialysis initiation. The poor outcomes from transplant waiting time are eliminated by LDRT. The study revealed that life expectancy increases by as much as 5.5 years if the elderly received LDRT within 4 years of starting dialysis. Thus, LDRT provides survival benefits in older candidates [139].
LDRT in elderly recipients also dramatically decreases perioperative and early post-transplant mortality. Compared to dialysis patients on the waiting list, time to equal survival was 521 and 130 days for ECD DDRT and LDRT, respectively. Therefore, LDRT decreases early post-transplant mortality in the elderly [140••].
The prevalence of CVD is twice as high in elderly patients with CKD and survival decreased with each rising stage of CKD. The 2-year survival from acute myocardial infarction (AMI) was only 30 % for patients with stage 4–5 CKD [141••]. CVD still is the most common cause of mortality in kidney transplant recipients, and this complication is highest during the early post-transplant period [116•, 142, 143]. One large study of 50,000 Medicare beneficiaries demonstrated an overall benefit of transplantation with a 17 % lower adjusted risk of AMI for those receiving a kidney transplant versus those remaining on dialysis. Compared to DDRT, LDRT had a lower relative risk (versus those remaining on dialysis) for AMI both early (≤3 months) and late (>3 months) post-transplantation [142]. Another recent cross-sectional study from Brazil also demonstrated a significantly higher prevalence of CVD in terms of left ventricular hypertrophy, coronary vascular calcification, and arrhythmia in the first 2 months post-transplant in DDRT as compared to LDRT; however, these differences did not exist when adjusted for age and dialysis vintage [143]. Elderly recipients generally carry multiple comorbid conditions and are at higher risk for perioperative mortality than younger recipients. The study also showed that recipients who were older than 65 years old had a greater risk for AMI and then the recipients age 18–34 years old and the risk rose 2-fold during the early post-transplant period [142]. LDRT provides elderly transplant recipients cardiovascular and survival benefits as compared to DDRT.
The Obese Transplant Recipient
In the general population, obesity (BMI ≥30 kg/m2) is a risk factor for cardiovascular morbidity and mortality [144–147], but paradoxically, it provides a survival benefit for ESRD patients [148]. The benefit of obesity in ESRD patient is lost upon receipt of a renal transplant due to shortened renal allograft and patient survivals following kidney transplantation. This change in survival is called “reverse epidemiology” [149–151].
Obese patients have a survival advantage from LDRT as compared to DDRT. DDRT by SCD kidneys does provide a survival advantage 1 year post-transplant by reducing the risk of death in patients with BMI ≥40 kg/m2 by 48 %. The risk of death is further reduced by 66 % for patient with BMI <40 kg/m2. In LDRT, the risk of death is reduced by 66 % for any degree of obesity [152••].
LDRT Potentially Decreases Immunological Barriers
Desensitization
Although utilizing marginal deceased donor kidneys is one way of overcoming the organ shortage, the numbers of patients who are on the kidney transplant waiting list are still far more than the number of total kidney transplantations done each year [14••]. In addition, highly sensitized patients have less of an opportunity to receive a kidney transplant. With the advancement of immunological technology for determining and detecting unacceptable antigens and antibodies, novel pretransplant and post-transplant therapeutic modalities such as desensitization increase the possibility for kidney transplantation in highly sensitized patients.
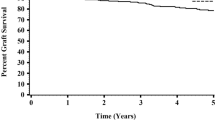
There are several desensitization strategies which include plasmapheresis plus low-dose intravenous immunoglobulin (IVIG) ± rituximab, high-dose IVIG (2 g/kg), and different induction therapies, e.g., daclizumab, basiliximab, thymoglobulin, or alemtuzumab. As expected, acute cellular rejection, ABMR, and long-term renal allograft outcomes are worse in desensitized recipients compared to non-sensitized patients. Because different desensitization protocols have been used in different transplant centers, this heterogeneity leads to difficulty in comparing outcomes between different desensitization protocols. In a meta-analysis of 21 studies between 2000 and 2010 involving 725 patients with donor-specific anti-HLA antibodies (DSA) who underwent desensitization, the rate of acute rejection and ABMR in the desensitized patients was 36 and 28 %, respectively, which was significantly higher than those of non-sensitized patients. At the 2-year median follow-up, the renal allograft survival was 86 % and patient survival was 95 % [153]. The long-term allograft outcome of a positive crossmatch for LDRT is also worse. A long-term single center retrospective study comparing renal allograft outcomes between positive flow cytometry crossmatch with plasmapharesis/IVIG conditioning and control groups during 9 years of follow-up revealed 1- and 5-year graft survival rates of 89.9 and 69.4 % for the positive crossmatch group and 97.6 and 80.6 % for the controls, respectively. Although the positive crossmatch increased the risk of graft loss, 1-year serum creatinine and patient survival did not change. Moreover, this study demonstrated that short-term allograft outcomes were favorable despite a positive crossmatch for LDRT. The medium–long-term outcomes were worse and even comparable to SCD DDRT [154]. However, a study from the John Hopkins group showed a higher long-term patient survival benefit of LDRT with a desensitization protocol utilizing plasmapheresis and low-dose IVIG in HLA sensitization patients as compared to a matched control group of patients undergoing either dialysis or HLA-compatible transplantation or on a waiting list for kidney transplantation who continued on dialysis. Moreover, patient survival improved 2-fold in LDRT after desensitization compared to patients that remained on the waiting list [155]. A more recent study from the Mayo Clinic group showed that the 5-year death-censored graft survival was inferior for a positive crossmatch, but allograft survival was higher in subgroup of recipients with antibody against donor class I antigens as compared with antibody against class II antigens [156••]. As a novel therapy, eculizumab demonstrated some promising results in LDRT with a positive crossmatch. Twenty-six highly sensitized recipients of LDRT were treated with post-transplant eculizumab and plasma exchange and were compared to a historical control group of sensitized patients treated with plasma exchange alone. The incidence of ABMR was 7.7 % (2/26) and 41.2 % (21/51) in the eculizumab and control groups, respectively [157].
Despite the poorer renal allograft outcomes, potential serious complications such as infection, malignancy, and high cost, successful kidney transplantation with desensitization in sensitized patients still provides survival benefits as compared to patients remaining on dialysis. In addition, the annual cost for the former is lower than the latter [158, 159].
Because the waiting time for available deceased donor kidneys is unpredictable, a desensitization protocol for LDRT appears to be advantageous. If there is an immunological barrier for kidney transplantation between donors and recipients, a desensitization protocol is another option to overcome that barrier in the setting of LDRT or combined desensitization with KPD. This is an important consideration in highly sensitized patients with low-level DSA. Compared to DDRT, LDRT provides the better option and mitigates against a poor outcome in DDRT for a high-risk sensitized patient.
KPD
Highly sensitized patients have fewer opportunities to receive a kidney transplant. KPD can overcome this barrier by increasing the number of compatible living donor transplants and improve long-term outcomes of living donor transplants through better matching of compatible pairs.
In a single-center prospective study, 22 LDRT in recipients with ABO or highly sensitized HLD incompatibilities were compared with their incompatible live donors by KPD. The graft survival rates were comparable with directed, compatible live donor transplants [160].
Psychosocial Issues by LDRT
Potential Elimination of Ethnic Disparity by LDRT
As mentioned above, Black and Hispanic recipients are the main groups affected by racial disparities. LDRT is one of the potential strategies to overcome this barrier and improve transplant outcomes. As an example, the Hispanic Kidney Transplant Program (HKTP) at Northwestern Comprehensive Transplant Center was implemented in 2008. Rates of Hispanics on the kidney transplant waiting list and LDKT have significantly increased. The Hispanic to non-Hispanic white LDKT ratio also increased by 70 %, and the waiting list among Hispanics increased by 91 % in contrast to only 4 % for non-Hispanic whites [161••].
Therefore, LDKT should be utilized whenever possible in order to eliminate disparities of kidney transplantation and improve transplant outcomes.
No Difference in Medication Non-adherence Between LDRT and DDRT
Although several unfavorable transplant outcomes have been reported for DDRT, non-adherence seems to be less problematic in DDRT.
Donor type may influence the recipients’ attitudes and beliefs regarding self-management. Recipients with deceased donor kidneys take more responsibility for taking care of the donated kidneys as a result of guilt over the death of their donors, but those with living donor kidneys feel responsible for their health without obligation to their donors [92••, 162].
From one cross-sectional study in Europe, LDRT had two to three times higher non-medication adherence compared to DDRT. However, there was no difference in medication non-adherence between LURT and DDRT as well as LRRT and LURT. The authors of this study concluded that health belief about the immunosuppressive medication requirement might contribute to less medication non-adherence in LRRT [163•].
Potentially Increased Available Living Kidney Donors Versus Chronic, Persistent, and Ongoing Shortage of Deceased Donor Kidneys
The number of candidates on the donor waiting list has increased from 50,000 in 2002 to 96,000 in 2013, and the median waiting time has increased from 3 years in 2003 to 4.5 years in 2009 [14••]. However, the number of deceased donors has not increased. Utilizing ECD and DCD kidneys expands the donor pool; however, the use of these organs is compromised with high rate of DGF. As a result, around half of ECD/DCD kidneys were discarded especially the kidneys from older, diabetic, AB blood type, and hepatitis C-positive donors [164•].
Living donation has also decreased since 2002 mainly due to decreased living related donation, but there has been an increase in living unrelated donation KPD since 2007 [14••].
Longer waiting time increases the chances of having medically unsuitable candidates for transplant. As almost 50 % of these candidates are willing to accept ECD kidneys, this potentially increases the risk for unfavorable transplant outcomes. An increase in LDRT should improve overall transplant outcomes from high-quality organs.
Although the renal allograft and kidney transplant recipient outcomes of LDRT are generally superior to those of DDRT, we should also consider the post-donation outcomes of the living kidney donors. This aspect of LDRT is beyond the scope of this review.
Table 2 summarizes the poor outcomes in DRRT and potential benefit of LDRT in mitigating the outcomes.
Lastly, we create an algorithm suggesting how to choose donors (LDRT vs. DDRT) in marginal recipients (Fig. 1).
Suggested algorithm for prekidney transplant evaluation process. CKD chronic kidney disease, DCD donation after circulatory death, DDRT deceased donor renal transplantation, DGF delayed graft function, DWFG death with a functioning allograft, ESRD end-stage renal disease, KPD kidney paired donation, LDRT living donor renal transplantation, SCD standard criteria donor
During pretransplant evaluation, the patients who are acceptable candidate could be either an excellent/good or marginal candidate. Non-candidates may continue dialysis and consider reevaluation of transplant candidacy when the barriers of kidney transplantation are overcome. The excellent/good candidate and marginal candidates whose risks of poor transplant outcomes are corrected should undergo either LDRT or DDRT depending on their conditions and available donor kidneys. Meticulously selected donor kidneys should be offered to all marginal candidates especially those with uncorrectable risks to mitigate poor transplant outcomes in such high-risk recipients. LDRT, KPD, and desensitization should be offered for the marginal candidates when possible. DDRT with SCD or non-DCD should be considered for marginal candidates without a living donor. However, marginal candidates may become non-candidates if contraindications later exist. They should continue on dialysis. Reevaluation for candidacy for kidney transplantation should be initiated when contraindications no longer exist.
Conclusions
Several factors contribute to the outcomes of kidney transplantation. Among of these, both quality of donor kidneys and underlying comorbidities of recipients play important roles. By nature of DDRT, the quality of kidneys is always compromised and transplant outcomes are never optimal particularly in marginal recipients. LDRT generally results in better renal allograft and recipient outcomes even in marginal recipients; however, appropriate selection of both living kidney donors and marginal but acceptable kidney transplant recipients is still one of the most crucial steps in maximizing overall transplant outcomes and mitigating poor outcomes.
Abbreviations
- ABMR:
-
Antibody-mediated rejection
- AF:
-
Atrial fibrillation
- ALERT:
-
Assessment of Lescol in renal transplantation
- AMI:
-
Acute myocardial infarction
- BMI:
-
Body mass index
- CABG:
-
Coronary artery bypass grafting
- CAD:
-
Coronary artery disease
- CIT:
-
Cold ischemic time
- CKD:
-
Chronic kidney disease
- CNI:
-
Calcineurin inhibitor
- COPD:
-
Obstructive pulmonary disease
- CVD:
-
Cardiovascular disease
- DBD:
-
Donation after brain death
- DCD:
-
Donation after circulatory death
- DDRT:
-
Deceased donor renal transplantation
- DGF:
-
Delayed graft function
- DM:
-
Diabetes mellitus
- DSA:
-
Donor-specific antibody
- DWFG:
-
Death with a functioning allograft
- ECD:
-
Expanded criteria donor
- ESRD:
-
End-stage renal disease
- FAVORIT:
-
Folic acid for vascular outcome reduction in transplantation
- HKTP:
-
Hispanic kidney transplant program
- HLA:
-
Human leukocyte antigen
- KDPI:
-
Kidney donor profile index
- KPD:
-
Kidney paired donation
- KTA:
-
Kidney transplantation alone
- LDL:
-
Low-density lipoprotein
- LDRT:
-
Living donor renal transplantation
- MoCA:
-
Montreal cognitive assessment
- PAD:
-
Peripheral arterial disease
- PAK:
-
Pancreas after kidney transplantation
- OPO:
-
Organ procurement organization
- SCD:
-
Standard criteria donor
- SPK:
-
Simultaneous pancreas-kidney transplantation
- SRTR:
-
Scientific registry of transplant recipients
- TUG:
-
Timed up and go test
- UNOS:
-
United network for organ sharing
- USRDS:
-
United States renal data system
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Suthanthiran M, Strom TB. Renal transplantation. N Engl J Med. 1994;331(6):365–76.
Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341(23):1725–30.
Abramowicz D, Cochat P, Claas FH, et al. European Renal Best Practice Guideline on kidney donor and recipient evaluation and perioperative care. Nephrol Dial Transplant. 2015;30(11):1790–7. This article provided a comprehensive guidelines and evidence-based clinical practice for caring in pre-donor and recipient evaluation and perioperative recipient care.
Kasiske BL, Ramos EL, Gaston RS, et al. The evaluation of renal transplant candidates: clinical practice guidelines. Patient Care and Education Committee of the American Society of Transplant Physicians. J Am Soc Nephrol. 1995;6(1):1–34.
Steinman TI, Becker BN, Frost AE, et al. Guidelines for the referral and management of patients eligible for solid organ transplantation. Transplantation. 2001;71(9):1189–204.
Kasiske BL, Cangro CB, Hariharan S, et al. The evaluation of renal transplantation candidates: clinical practice guidelines. Am J Transplant. 2001;1 Suppl 2:3–95.
Knoll G, Cockfield S, Blydt-Hansen T, et al. Canadian Society of Transplantation consensus guidelines on eligibility for kidney transplantation. CMAJ. 2005;173(10):1181–4.
Bunnapradist S, Danovitch GM. Evaluation of adult kidney transplant candidates. Am J Kidney Dis. 2007;50(5):890–8.
Batabyal P, Chapman JR, Wong G, et al. Clinical practice guidelines on wait-listing for kidney transplantation: consistent and equitable? Transplantation. 2012;94(7):703–13.
Braun WE. Long-term complications of renal transplantation. Kidney Int. 1990;37(5):1363–78.
Pascual M, Theruvath T, Kawai T, et al. Strategies to improve long-term outcomes after renal transplantation. N Engl J Med. 2002;346(8):580–90.
Petersen E, Baird BC, Shihab F, et al. The impact of recipient history of cardiovascular disease on kidney transplant outcome. ASAIO J. 2007;53(5):601–8.
Col VJ, Jacquet L, Squifflet JP, et al. Combined heart-kidney transplantation: report on six cases. Nephrol Dial Transplant. 1998;13(3):723–7.
Matas AJ, Smith JM, Skeans MA, et al. OPTN/SRTR 2013 annual data report: kidney. Am J Transplant. 2015;15 Suppl 2:1–34. This national data provided a comprehensive informaiton in all aspects of kidney transplantation.
Hawwa N, Shrestha K, Hammadah M, et al. Reverse remodeling and prognosis following kidney transplantation in contemporary patients with cardiac dysfunction. J Am Coll Cardiol. 2015;66(16):1779–87. This study demonstrated the crucial role of kidney transplantation in improving cardiac structure and function. It should assist for decision making on selection suitable cardiac patients to undergo kidney transplantation.
Katz SD, Parikh CR. Reverse left ventricular remodeling after kidney transplantation: unraveling the complex autointoxication of Uremia. J Am Coll Cardiol. 2015;66(16):1788–90. This editorial of the reference #21 and supports successful kidney transplantation with improved renal function could improve cardiac function.
Nesbit RM, Burk LB, Olsen NS. Blood level of phenol in uremia. Arch Surg. 1946;53:483–8.
Vanholder R, Glorieux G, Lameire N, et al. Uraemic toxins and cardiovascular disease. Nephrol Dial Transplant. 2003;18(3):463–6.
Parfrey PS, Harnett JD, Foley RN, et al. Impact of renal transplantation on uremic cardiomyopathy. Transplantation. 1995;60(9):908–14.
Sood MM, Pauly RP, Rigatto C, et al. Left ventricular dysfunction in the haemodialysis population. NDT Plus. 2008;1(4):199–205.
Umana E, Ahmed W, Alpert MA. Valvular and perivalvular abnormalities in end-stage renal disease. Am J Med Sci. 2003;325(4):237–42.
Abbott KC, Hshieh P, Cruess D, et al. Hospitalized valvular heart disease in patients on renal transplant waiting list: incidence, clinical correlates and outcomes. Clin Nephrol. 2003;59(2):79–87.
Sharma A, Gilbertson DT, Herzog CA. Survival of kidney transplantation patients in the United States after cardiac valve replacement. Circulation. 2010;121(25):2733–9.
Lenihan CR, Montez-Rath ME, Scandling JD, et al. Outcomes after kidney transplantation of patients previously diagnosed with atrial fibrillation. Am J Transplant. 2013;13(6):1566–75. This study emphasize one of the most common cardiac conditions which is overlooked during pretransplant evaluation but it commonly leads to major consequences both cardiovascular complications and poor transplant outcomes.
Perez Fontan M, Rodriguez-Carmona A, Garcia Falcon T, et al. Early immunologic and nonimmunologic predictors of arterial hypertension after renal transplantation. Am J Kidney Dis. 1999;33(1):21–8.
Ebpg, European Renal A, European Society for Organ T. European best practice guidelines for renal transplantation (part 1). Nephrol Dial Transplant. 2000;15 Suppl 7:1–85.
Pilmore H. Cardiac assessment for renal transplantation. Am J Transplant. 2006;6(4):659–65.
Molnar MZ, Foster 3rd CE, Sim JJ, et al. Association of pre-transplant blood pressure with post-transplant outcomes. Clin Transpl. 2014;28(2):166–76. This is a recent published study of the large cohort about pretransplant blood pressure on posttransplant outcomes, which potentially be implemented to new guideline for pretransplant blood pressure level which still lack of recommendaton.
Frei U, Schindler R, Wieters D, et al. Pre-transplant hypertension: a major risk factor for chronic progressive renal allograft dysfunction? Nephrol Dial Transplant. 1995;10(7):1206–11.
Cosio FG, Falkenhain ME, Pesavento TE, et al. Relationships between arterial hypertension and renal allograft survival in African-American patients. Am J Kidney Dis. 1997;29(3):419–27.
Cosio FG, Dillon JJ, Falkenhain ME, et al. Racial differences in renal allograft survival: the role of systemic hypertension. Kidney Int. 1995;47(4):1136–41.
Authors/Task Force m, Windecker S, Kolh P, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35(37):2541–619.
Hassan NA, D’Orsi ET, D’Orsi CJ, et al. The risk for medial arterial calcification in CKD. Clin J Am Soc Nephrol. 2012;7(2):275–9.
Abou-Hassan N, Tantisattamo E, D’Orsi ET, et al. The clinical significance of medial arterial calcification in end-stage renal disease in women. Kidney Int. 2015;87(1):195–9.
Sung RS, Althoen M, Howell TA, et al. Peripheral vascular occlusive disease in renal transplant recipients: risk factors and impact on kidney allograft survival. Transplantation. 2000;70(7):1049–54.
Snyder JJ, Kasiske BL, Maclean R. Peripheral arterial disease and renal transplantation. J Am Soc Nephrol. 2006;17(7):2056–68.
Kasiske BL, Klinger D. Cigarette smoking in renal transplant recipients. J Am Soc Nephrol. 2000;11(4):753–9.
Venstrom JM, McBride MA, Rother KI, et al. Survival after pancreas transplantation in patients with diabetes and preserved kidney function. JAMA. 2003;290(21):2817–23.
Tanaka H, Sukhova GK, Libby P. Interaction of the allogeneic state and hypercholesterolemia in arterial lesion formation in experimental cardiac allografts. Arterioscler Thromb. 1994;14(5):734–45.
Dimeny E, Tufveson G, Lithell H, et al. The influence of pretransplant lipoprotein abnormalities on the early results of renal transplantation. Eur J Clin Investig. 1993;23(9):572–9.
Seron D, Moreso F, Ramon JM, et al. Protocol renal allograft biopsies and the design of clinical trials aimed to prevent or treat chronic allograft nephropathy. Transplantation. 2000;69(9):1849–55.
Dimeny E, Wahlberg J, Lithell H, et al. Hyperlipidaemia in renal transplantation--risk factor for long-term graft outcome. Eur J Clin Investig. 1995;25(8):574–83.
Guijarro C, Massy ZA, Kasiske BL. Clinical correlation between renal allograft failure and hyperlipidemia. Kidney Int Suppl. 1995;52:S56–9.
Fernandez-Miranda C, Morales JM, Porres A, et al. Increased lipoproteins and fibrinogen in chronic renal allograft dysfunction. Am J Nephrol. 1997;17(5):445–9.
Castello IB. Hyperlipidemia: a risk factor for chronic allograft dysfunction. Kidney Int Suppl. 2002;80:73–7.
Nicoletto BB, Fonseca NK, Manfro RC, et al. Effects of obesity on kidney transplantation outcomes: a systematic review and meta-analysis. Transplantation. 2014;98(2):167–76. This meta-analysis emphasized the worse renal allograft outcomes in terms of delayed graft function in obease recipients; however, it provideed the new findings of uneffect allograft and patient outcomes with obesity recipients from studies conducted over the past 15 years.
Dudley C, Harden P. Renal Association Clinical Practice Guideline on the assessment of the potential kidney transplant recipient. Nephron Clin Pract. 2011;118 Suppl 1:c209–24.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56.
Garonzik-Wang JM, Govindan P, Grinnan JW, et al. Frailty and delayed graft function in kidney transplant recipients. Arch Surg. 2012;147(2):190–3.
McAdams-DeMarco MA, Law A, Salter ML, et al. Frailty and early hospital readmission after kidney transplantation. Am J Transplant. 2013;13(8):2091–5. This study provides a noval preditor of an important early transplant outcomes in high risk elderly kidney transplant recipients.
McAdams-DeMarco MA, Law A, King E, et al. Frailty and mortality in kidney transplant recipients. Am J Transplant. 2015;15(1):149–54.
Terasaki PI, Ozawa M. Predicting kidney graft failure by HLA antibodies: a prospective trial. Am J Transplant. 2004;4(3):438–43.
Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–94.
Gordon EJ, Ladner DP, Caicedo JC, et al. Disparities in kidney transplant outcomes: a review. Semin Nephrol. 2010;30(1):81–9.
Hariharan S, Johnson CP, Bresnahan BA, et al. Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med. 2000;342(9):605–12.
Opelz G, Pfarr E, Engelmann A, et al. Kidney graft survival rates in black cyclosporine-treated recipients. Collab Transplant Study Transplant Proc. 1989;21(6):3918–20.
Butkus DE, Meydrech EF, Raju SS. Racial differences in the survival of cadaveric renal allografts. Overriding effects of HLA matching and socioeconomic factors. N Engl J Med. 1992;327(12):840–5.
Gjertson DW. Determinants of long-term survival of adult kidney transplants: a 1999 UNOS update. Clin Transpl. 1999;341–52.
Isaacs RB, Nock SL, Spencer CE, et al. Racial disparities in renal transplant outcomes. Am J Kidney Dis. 1999;34(4):706–12.
Meier-Kriesche HU, Ojo A, Magee JC, et al. African-American renal transplant recipients experience decreased risk of death due to infection: possible implications for immunosuppressive strategies. Transplantation. 2000;70(2):375–9.
Hardinger KL, Stratta RJ, Egidi MF, et al. Renal allograft outcomes in African American versus Caucasian transplant recipients in the tacrolimus era. Surgery. 2001;130(4):738–45. discussion 45–7.
Ojo AO, Hanson JA, Wolfe RA, et al. Long-term survival in renal transplant recipients with graft function. Kidney Int. 2000;57(1):307–13.
Eckhoff DE, Young CJ, Gaston RS, et al. Racial disparities in renal allograft survival: a public health issue? J Am Coll Surg. 2007;204(5):894–902. discussion −3.
Smith SR, Butterly DW. Declining influence of race on the outcome of living-donor renal transplantation. Am J Transplant. 2002;2(3):282–6.
Milford EL, Ratner L, Yunis E. Will transplant immunogenetics lead to better graft survival in blacks? Racial variability in the accuracy of tissue typing for organ donation: the fourth American workshop. Transplant Proc. 1987;19(2 Suppl 2):30–2.
Kerman RH, Kimball PM, Van Buren CT, et al. Possible contribution of pretransplant immune responder status to renal allograft survival differences of black versus white recipients. Transplantation. 1991;51(2):338–42.
Gaston RS, Hudson SL, Deierhoi MH, et al. Improved survival of primary cadaveric renal allografts in blacks with quadruple immunosuppression. Transplantation. 1992;53(1):103–9.
Neylan JF. Immunosuppressive therapy in high-risk transplant patients: dose-dependent efficacy of mycophenolate mofetil in African-American renal allograft recipients. U.S. Renal Transplant Mycophenolate Mofetil Study Group. Transplantation. 1997;64(9):1277–82.
Neylan JF. Racial differences in renal transplantation after immunosuppression with tacrolimus versus cyclosporine. FK506 Kidney Transplant Study Group. Transplantation. 1998;65(4):515–23.
Lindholm A, Welsh M, Alton C, et al. Demographic factors influencing cyclosporine pharmacokinetic parameters in patients with uremia: racial differences in bioavailability. Clin Pharmacol Ther. 1992;52(4):359–71.
First MR, Schroeder TJ, Monaco AP, et al. Cyclosporine bioavailability: dosing implications and impact on clinical outcomes in select transplantation subpopulations. Clin Transpl. 1996;10(1 Pt 1):55–9.
Curtis JJ. Kidney transplantation: racial or socioeconomic disparities? Am J Kidney Dis. 1999;34(4):756–8.
Oriol R, Le Pendu J, Chun C. Influence of the original disease, race, and center on the outcome of kidney transplantation. Transplantation. 1982;33(1):22–6.
Koyama H, Cecka JM, Terasaki PI. Kidney transplants in black recipients. HLA matching and other factors affecting long-term graft survival. Transplantation. 1994;57(7):1064–8.
Gordon EJ, Caicedo JC. Ethnic advantages in kidney transplant outcomes: the Hispanic Paradox at work? Nephrol Dial Transplant. 2009;24(4):1103–9.
Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation--clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343(21):1537–44. 2 p preceding.
Kasiske BL, Snyder JJ, Matas AJ, et al. Preemptive kidney transplantation: the advantage and the advantaged. J Am Soc Nephrol. 2002;13(5):1358–64.
Ilori TO, Adedinsewo DA, Odewole O, et al. Racial and ethnic disparities in graft and recipient survival in elderly kidney transplant recipients. J Am Geriatr Soc. 2015;63(12):2485–93. A large epidemiologic study demontrating transplant disparities in transplant outcomes among major ethnicities in the United States.
Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253–65.
Siris ES, Selby PL, Saag KG, et al. Impact of osteoporosis treatment adherence on fracture rates in North America and Europe. Am J Med. 2009;122(2 Suppl):S3–13.
Gold DT, Alexander IM, Ettinger MP. How can osteoporosis patients benefit more from their therapy? Adherence issues with bisphosphonate therapy. Ann Pharmacother. 2006;40(6):1143–50.
Butler JA, Roderick P, Mullee M, et al. Frequency and impact of nonadherence to immunosuppressants after renal transplantation: a systematic review. Transplantation. 2004;77(5):769–76.
Denhaerynck K, Dobbels F, Cleemput I, et al. Prevalence, consequences, and determinants of nonadherence in adult renal transplant patients: a literature review. Transpl Int. 2005;18(10):1121–33.
Brown KL, El-Amm JM, Doshi MD, et al. Outcome predictors in African-American deceased-donor renal allograft recipients. Clin Transpl. 2009;23(4):454–61.
Prendergast MB, Gaston RS. Optimizing medication adherence: an ongoing opportunity to improve outcomes after kidney transplantation. Clin J Am Soc Nephrol. 2010;5(7):1305–11.
Guerra G, Ciancio G, Gaynor JJ, et al. Randomized trial of immunosuppressive regimens in renal transplantation. J Am Soc Nephrol. 2011;22(9):1758–68.
Chisholm-Burns MA, Spivey CA, Graff Zivin J, et al. Improving outcomes of renal transplant recipients with behavioral adherence contracts: a randomized controlled trial. Am J Transplant. 2013;13(9):2364–73. This study demonstrated the interesting behavorial intervention involving in pharmacy to increase transplant outcomes.
Dew MA, DiMartini AF, De Vito Dabbs A, et al. Rates and risk factors for nonadherence to the medical regimen after adult solid organ transplantation. Transplantation. 2007;83(7):858–73.
Sellares J, de Freitas DG, Mengel M, et al. Understanding the causes of kidney transplant failure: the dominant role of antibody-mediated rejection and nonadherence. Am J Transplant. 2012;12(2):388–99.
Wiebe C, Gibson IW, Blydt-Hansen TD, et al. Evolution and clinical pathologic correlations of de novo donor-specific HLA antibody post kidney transplant. Am J Transplant. 2012;12(5):1157–67.
In: Adams K, Greiner AC, Corrigan JM, editors. The 1st annual crossing the quality chasm summit: a focus on communities. Washington (DC); 2004.
Jamieson NJ, Hanson CS, Josephson MA, et al. Motivations, challenges, and attitudes to self-management in kidney transplant recipients: a systematic review of qualitative studies. Am J Kidney Dis. 2015. This is one of the large meta-analysis of an important topic concerning on adherence and self-management of kidney transplant recipient. It provides samples and practical points commonly encountered in practice and guides the way to improve the outcomes.
Nemati E, Einollahi B, Lesan Pezeshki M, et al. Does kidney transplantation with deceased or living donor affect graft survival? Nephrourol Mon. 2014;6(4), e12182. This study confirms the short- and long-trem outcomes of living donor renal transplantation above deceased donor renal transplantation.
Terasaki PI, Cecka JM, Gjertson DW, et al. High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med. 1995;333(6):333–6.
Jones Jr JW, Gillingham KJ, Sutherland DE, et al. Successful long-term outcome with 0-haplotype-matched living-related kidney donors. Transplantation. 1994;57(4):512–5.
Lowell JA, Brennan DC, Shenoy S, et al. Living-unrelated renal transplantation provides comparable results to living-related renal transplantation: a 12-year single-center experience. Surgery. 1996;119(5):538–43.
Suzuki MM, Cecka JM, Terasaki PI. Unrelated living donor kidney transplants. Br Med Bull. 1997;53(4):854–9.
Opelz G. Impact of HLA compatibility on survival of kidney transplants from unrelated live donors. Transplantation. 1997;64(10):1473–5.
Koo DD, Welsh KI, Roake JA, et al. Ischemia/reperfusion injury in human kidney transplantation: an immunohistochemical analysis of changes after reperfusion. Am J Pathol. 1998;153(2):557–66.
de Sandes-Freitas TV, Felipe CR, Aguiar WF, et al. Prolonged delayed graft function is associated with inferior patient and kidney allograft survivals. PLoS One. 2015;10(12), e0144188. The study showing the poorer renal allograft and patient outcomes with the prolonged dealyed graft function stratified by the duration of dealyed graft function.
Ojo AO. Cardiovascular complications after renal transplantation and their prevention. Transplantation. 2006;82(5):603–11.
Kasiske BL, Guijarro C, Massy ZA, et al. Cardiovascular disease after renal transplantation. J Am Soc Nephrol. 1996;7(1):158–65.
Kasiske BL. Risk factors for accelerated atherosclerosis in renal transplant recipients. Am J Med. 1988;84(6):985–92.
Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–305.
Fellstrom B, Jardine AG, Soveri I, et al. Renal dysfunction as a risk factor for mortality and cardiovascular disease in renal transplantation: experience from the Assessment of Lescol in Renal Transplantation trial. Transplantation. 2005;79(9):1160–3.
Weiner DE, Carpenter MA, Levey AS, et al. Kidney function and risk of cardiovascular disease and mortality in kidney transplant recipients: the FAVORIT trial. Am J Transplant. 2012;12(9):2437–45.
Arnadottir M, Hultberg B, Vladov V, et al. Hyperhomocysteinemia in cyclosporine-treated renal transplant recipients. Transplantation. 1996;61(3):509–12.
Ducloux D, Motte G, Challier B, et al. Serum total homocysteine and cardiovascular disease occurrence in chronic, stable renal transplant recipients: a prospective study. J Am Soc Nephrol. 2000;11(1):134–7.
Roodnat JI, Mulder PG, Rischen-Vos J, et al. Proteinuria after renal transplantation affects not only graft survival but also patient survival. Transplantation. 2001;72(3):438–44.
Raggi P, Boulay A, Chasan-Taber S, et al. Cardiac calcification in adult hemodialysis patients. A link between end-stage renal disease and cardiovascular disease? J Am Coll Cardiol. 2002;39(4):695–701.
Fernandez-Fresnedo G, Plaza JJ, Sanchez-Plumed J, et al. Proteinuria: a new marker of long-term graft and patient survival in kidney transplantation. Nephrol Dial Transplant. 2004;19 Suppl 3:iii47–51.
Giachelli CM. Vascular calcification mechanisms. J Am Soc Nephrol. 2004;15(12):2959–64.
Gill JS, Rose C, Pereira BJ, et al. The importance of transitions between dialysis and transplantation in the care of end-stage renal disease patients. Kidney Int. 2007;71(5):442–7.
Matas AJ, Payne WD, Sutherland DE, et al. 2,500 living donor kidney transplants: a single-center experience. Ann Surg. 2001;234(2):149–64.
Lentine KL, Costa SP, Weir MR, et al. Cardiac disease evaluation and management among kidney and liver transplantation candidates: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 2012;60(5):434–80.
Hart A, Weir MR, Kasiske BL. Cardiovascular risk assessment in kidney transplantation. Kidney Int. 2015;87(3):527–34. This articles provided a rational for cardiac work-up in kidney transplantation which is still controversial.
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139–228.
Lee CW. Dual antiplatelet therapy for coronary artery disease. Circ J. 2015;79(2):255–62.
Berger PB, Bell MR, Hasdai D, et al. Safety and efficacy of ticlopidine for only 2 weeks after successful intracoronary stent placement. Circulation. 1999;99(2):248–53.
Wilson SH, Rihal CS, Bell MR, et al. Timing of coronary stent thrombosis in patients treated with ticlopidine and aspirin. Am J Cardiol. 1999;83(7):1006–11.
Ma MK, Lim WH, Craig JC, et al. Mortality among younger and older recipients of kidney transplants from expanded criteria donors compared with standard criteria donors. Clin J Am Soc Nephrol. 2015. This study demonstrated to poor outcomes of expanded criteria donor deceased donor renal transplantation through the spectra of all age groups. It emphasized the careful utilizing the expanded criteria kidneys in young recipients.
Kasiske BL, Anjum S, Shah R, et al. Hypertension after kidney transplantation. Am J Kidney Dis. 2004;43(6):1071–81.
Cowley Jr AW, Roman RJ. The role of the kidney in hypertension. JAMA. 1996;275(20):1581–9.
Curtis JJ, Luke RG, Dustan HP, et al. Remission of essential hypertension after renal transplantation. N Engl J Med. 1983;309(17):1009–15.
Guidi E, Bianchi G, Rivolta E, et al. Hypertension in man with a kidney transplant: role of familial versus other factors. Nephron. 1985;41(1):14–21.
Guidi E, Cozzi MG, Minetti E, et al. Donor and recipient family histories of hypertension influence renal impairment and blood pressure during acute rejections. J Am Soc Nephrol. 1998;9(11):2102–7.
Guidi E, Menghetti D, Milani S, et al. Hypertension may be transplanted with the kidney in humans: a long-term historical prospective follow-up of recipients grafted with kidneys coming from donors with or without hypertension in their families. J Am Soc Nephrol. 1996;7(8):1131–8.
Ozdemir FN, Ibis A, Altunoglu A, et al. Pretransplantation systolic blood pressure and the risk of delayed graft function in young living-related renal allograft recipients. Transplant Proc. 2007;39(4):842–5.
Tyden G, Bolinder J, Solders G, et al. Improved survival in patients with insulin-dependent diabetes mellitus and end-stage diabetic nephropathy 10 years after combined pancreas and kidney transplantation. Transplantation. 1999;67(5):645–8.
Rayhill SC, D’Alessandro AM, Odorico JS, et al. Simultaneous pancreas-kidney transplantation and living related donor renal transplantation in patients with diabetes: is there a difference in survival? Ann Surg. 2000;231(3):417–23.
Reddy KS, Stablein D, Taranto S, et al. Long-term survival following simultaneous kidney-pancreas transplantation versus kidney transplantation alone in patients with type 1 diabetes mellitus and renal failure. Am J Kidney Dis. 2003;41(2):464–70.
Weiss AS, Smits G, Wiseman AC. Twelve-month pancreas graft function significantly influences survival following simultaneous pancreas-kidney transplantation. Clin J Am Soc Nephrol. 2009;4(5):988–95.
Sampaio MS, Poommipanit N, Cho YW, et al. Transplantation with pancreas after living donor kidney vs. living donor kidney alone in type 1 diabetes mellitus recipients. Clin Transpl. 2010;24(6):812–20.
Gaston RS, Basadonna G, Cosio FG, et al. Transplantation in the diabetic patient with advanced chronic kidney disease: a task force report. Am J Kidney Dis. 2004;44(3):529–42.
Morath C, Zeier M, Dohler B, et al. Transplantation of the type 1 diabetic patient: the long-term benefit of a functioning pancreas allograft. Clin J Am Soc Nephrol. 2010;5(3):549–52.
Israni AK, Feldman HI, Propert KJ, et al. Impact of simultaneous kidney-pancreas transplant and timing of transplant on kidney allograft survival. Am J Transplant. 2005;5(2):374–82.
Pruijm MT, de Fijter HJ, Doxiadis II, et al. Preemptive versus non-preemptive simultaneous pancreas-kidney transplantation: a single-center, long-term, follow-up study. Transplantation. 2006;81(8):1119–24.
Merion RM, Ashby VB, Wolfe RA, et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA. 2005;294(21):2726–33.
Schold JD, Meier-Kriesche HU. Which renal transplant candidates should accept marginal kidneys in exchange for a shorter waiting time on dialysis? Clin J Am Soc Nephrol. 2006;1(3):532–8.
Gill JS, Schaeffner E, Chadban S, et al. Quantification of the early risk of death in elderly kidney transplant recipients. Am J Transplant. 2013;13(2):427–32. This study demonstrated the survival advantage of living donor renal transplantation compared with wait-listing in early transplant period even such a high risk elderly recipients.
United States Renal Data System. This study demonstrated the survival advantage of living donor renal transplantation compared with wait-listing in early transplant period even such a high risk elderly recipients. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2015.
Kasiske BL, Maclean JR, Snyder JJ. Acute myocardial infarction and kidney transplantation. J Am Soc Nephrol. 2006;17(3):900–7.
Yazbek DC, de Carvalho AB, Barros CS, et al. Cardiovascular disease in early kidney transplantation: comparison between living and deceased donor recipients. Transplant Proc. 2012;44(10):3001–6.
Manson JE, Willett WC, Stampfer MJ, et al. Body weight and mortality among women. N Engl J Med. 1995;333(11):677–85.
Stevens J, Plankey MW, Williamson DF, et al. The body mass index-mortality relationship in white and African American women. Obes Res. 1998;6(4):268–77.
Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–105.
Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable to obesity in the United States. JAMA. 1999;282(16):1530–8.
Kalantar-Zadeh K, Block G, Humphreys MH, et al. Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int. 2003;63(3):793–808.
Meier-Kriesche HU, Arndorfer JA, Kaplan B. The impact of body mass index on renal transplant outcomes: a significant independent risk factor for graft failure and patient death. Transplantation. 2002;73(1):70–4.
Gore JL, Pham PT, Danovitch GM, et al. Obesity and outcome following renal transplantation. Am J Transplant. 2006;6(2):357–63.
Hoogeveen EK, Aalten J, Rothman KJ, et al. Effect of obesity on the outcome of kidney transplantation: a 20-year follow-up. Transplantation. 2011;91(8):869–74.
Gill JS, Lan J, Dong J, et al. The survival benefit of kidney transplantation in obese patients. Am J Transplant. 2013;13(8):2083–90. This is another study that demonstrated the survival advantage of renal transplantation in a high risk obese recipients with the persistent outcomes in living donor renal transplantation.
Marfo K, Lu A, Ling M, et al. Desensitization protocols and their outcome. Clin J Am Soc Nephrol. 2011;6(4):922–36.
Haririan A, Nogueira J, Kukuruga D, et al. Positive cross-match living donor kidney transplantation: longer-term outcomes. Am J Transplant. 2009;9(3):536–42.
Montgomery RA, Lonze BE, King KE, et al. Desensitization in HLA-incompatible kidney recipients and survival. N Engl J Med. 2011;365(4):318–26.
Bentall A, Cornell LD, Gloor JM, et al. Five-year outcomes in living donor kidney transplants with a positive crossmatch. Am J Transplant. 2013;13(1):76–85. This study demonstrated the inferior outcomes of positive crossmatch living-donor renal transplantation; however, selection of patients with class I donor specific antibody should lower the poor outcome.
Stegall MD, Diwan T, Raghavaiah S, et al. Terminal complement inhibition decreases antibody-mediated rejection in sensitized renal transplant recipients. Am J Transplant. 2011;11(11):2405–13.
Jordan SC, Tyan D, Stablein D, et al. Evaluation of intravenous immunoglobulin as an agent to lower allosensitization and improve transplantation in highly sensitized adult patients with end-stage renal disease: report of the NIH IG02 trial. J Am Soc Nephrol. 2004;15(12):3256–62.
Kamar N, Milioto O, Puissant-Lubrano B, et al. Incidence and predictive factors for infectious disease after rituximab therapy in kidney-transplant patients. Am J Transplant. 2010;10(1):89–98.
Montgomery RA, Zachary AA, Ratner LE, et al. Clinical results from transplanting incompatible live kidney donor/recipient pairs using kidney paired donation. JAMA. 2005;294(13):1655–63.
Gordon EJ, Lee J, Kang R, et al. Hispanic/Latino disparities in living donor kidney transplantation: role of a culturally competent transplant program. Transplant Direct. 2015;1(8), e29. This study provides the insite and emphasize of understanding ethnic disparity in minority and how to overcome this barrier to enhance kidney transplantation in this population.
Orr A, Orr D, Willis S, et al. Patient perceptions of factors influencing adherence to medication following kidney transplant. Psychol Health Med. 2007;12(4):509–17.
Denhaerynck K, Schmid-Mohler G, Kiss A, et al. Differences in medication adherence between living and deceased donor kidney transplant patients. Int J Organ Transplant Med. 2014;5(1):7–14. This study revealed the interesting data about non-medication adherance in living-related renal transplantation and lead to awareness of the importance how to approach the patients differently as per type of kidney transplantation.
Singh SK, Kim SJ. Epidemiology of kidney discard from expanded criteria donors undergoing donation after circulatory death. Clin J Am Soc Nephrol. 2015. This study emphasizes the chonic ongoing issues of organ discard in low quality donor kidney.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ekamol Tantisattamo, James Bailey, and Lorenzo Gallon declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Kidney Transplantation
Rights and permissions
About this article
Cite this article
Tantisattamo, E., Bailey, J.L. & Gallon, L. Living Donation Mitigates Poorer Outcomes in Marginal Recipients. Curr Transpl Rep 3, 121–138 (2016). https://doi.org/10.1007/s40472-016-0097-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-016-0097-6