Abstract
Purpose of Review
Understanding dynamic relationships between negative affect and substance use disorder (SUD) outcomes, including craving, may help inform adaptive and personalized interventions. Recent studies using intensive longitudinal methods were reviewed to examine relationships between negative affect and the outcomes of either craving or substance use during and following SUD treatment.
Recent Findings
Results on associations between negative affect and craving/substance use were mixed and difficult to synthesize, given methodological differences across studies. The strength and direction of these relationships varied across outcomes, subgroups, contexts, and time course.
Summary
The current literature is mixed concerning negative affect and craving/substance use associations during and following SUD treatment. Researchers should increasingly recruit diverse individuals, for example, samples of varying racial and ethnic backgrounds and those reporting co-occurring disorders and polysubstance use. Experimental, qualitative, and person-specific methods will improve our understanding of relationships between negative affect and substance-related outcomes during SUD treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Theoretical models of addiction imply that using substances to cope with negative affect is associated with poorer long-term substance use outcomes [1,2,3] and that substance use disorders (SUDs) become increasingly driven by negative reinforcement (i.e., using substances to relieve negative affect) over time [4,5,6]. Accordingly, SUDs often co-occur with disorders defined by high negative affect (e.g., depression, anxiety, posttraumatic stress disorder [PTSD]) [7, 8], and affective disorders are a risk factor for SUD [9]. Those with co-occurring disorders are more likely to experience greater SUD severity and impairment [10, 11] and to seek treatment [12]. Given the central role of negative affect in models of addiction, a large body of research has attempted to characterize the role of negative affect in predicting, moderating, and mediating SUD treatment outcomes to inform tailored, adaptive, and precision interventions.
The Role of Negative Affect in Substance Use Disorder Treatment
Generally, people who more frequently experience negative affect and who meet diagnostic criteria for affective disorders before and during treatment have poorer SUD treatment outcomes (e.g., more frequent/heavier substance use, greater craving) [13,14,15]. Those with higher trait negative affect also tend to respond better to specific SUD treatments, such as mindfulness-based relapse prevention (MBRP) [16] and acamprosate treatment for alcohol use disorder (AUD) [17]. However, the extent to which SUD treatment impacts negative affect is poorly understood. There is some evidence that average trait-level negative affect decreases during treatment [13], but negative affect has been understudied as a SUD treatment mechanism [13, 18].
A clearer understanding of negative affect during SUD treatment is needed to improve treatments. For example, it is unclear whether people with higher trait-level negative affect report greater cravings/substance use (a between-person effect) or if moments with higher state-level negative affect are associated with increased craving/substance use (a within-person effect). It could also be that individuals with higher trait-level negative affect experience increased craving and engage in more substance use during times of higher state-level negative affect or some person-specific or time-varying combination of these effects. The timescale connecting negative affect and craving or substance use is also unknown. For example, does the association between negative affect and craving or substance use change over minutes, hours, and/or cumulatively over extended periods? Time series analyses are needed to determine whether there are systematic trends in negative affect during treatment, including precipitous points of change that could inform adaptive interventions.
Using Intensive Longitudinal Methods to Understand the Role of Negative Affect in Substance Use Disorder Treatment
The use of intensive longitudinal methods, such as ecological momentary assessment (EMA) and daily diary methods, can improve our understanding of negative affect in SUD treatment [19]. These methods have several advantages over traditional, retrospective-based methods (e.g., self-report and calendar-based measures). Intensive longitudinal methods collect multiple observations within individuals over time, often multiple times within a day, using brief self-report measures. Measures can be administered randomly within the day (or within time blocks), at fixed times each day, or during user-initiated events in the individual’s daily life [20]. Accordingly, these methods mitigate recall bias, increase ecological validity, and are better able to disentangle the temporality of constructs. Analytic techniques for analyzing intensive longitudinal data include, but are not limited to (1) multilevel modeling (MLM), which can help to understand the level of analysis (i.e., between- or within-person) at which a relationship occurs and the time course of change in an outcome [21], (2) time-varying effects modeling (TVEM), which can help understand how the strength of a relationship between variables differs across time [22], and (3) network-based methods, such as vector autoregression or group iterative multiple model estimation, which models the presence and magnitude of relationships between nodes for groups and specific individuals within groups [23, 24].
Given these methodological features, intensive longitudinal methods can provide information regarding the contexts during which negative affect is most likely to impact substance use outcomes [19, 25], such as when skills to reduce negative affect might be most beneficial during treatment. Measuring the relationships between negative affect and craving or substance use and how these relationships differ between individuals, within individuals, or between and within individuals can help determine who needs treatments that target negative affect explicitly (e.g., MBRP), when to deliver negative affect-specific strategies, and whether certain subgroups could benefit from skills targeting negative affect at critical moments during treatment. Person-specific or idiographic methods that use intensive longitudinal data can also be employed to model dynamics at the individual level, informing the design of tailored and personalized assessment and interventions [24, 26•]. For example, pre-treatment person-specific models could assess the strength of an individual’s relationship between negative affect and substance-related outcomes to determine if they may benefit from treatments that target negative affect and/or guide the delivery of momentary interventions during contexts with stronger negative affect and substance use associations [27•]. Intensive longitudinal data could also be used as measurement-based care to give clients personalized feedback on relationships between negative affect and substance use [28, 29].
Previous Reviews and Meta-analyses and the Current Review
We reviewed intensive longitudinal studies that examined relationships between negative affect and substance-related outcomes among individuals in SUD treatment. Of note, a recent systematic review and meta-analysis [30••, 31•] synthesized findings on associations between negative affect and substance use in intensive longitudinal studies enrolling a broader range of samples. Specifically, findings from a systematic review focusing on the associations between affective states and cannabis use in daily life [31•] indicated that momentary and daily negative affect (particularly anger/hostility) were concurrently associated with cannabis use among samples experiencing significant levels of psychopathology (e.g., SUDs, personality disorders), but support for the negative reinforcement model of cannabis use was equivocal in community and college student samples. In a large-scale meta-analysis of participant-level data from 69 studies [30••], participants were not more likely to drink or drink heavily on days with higher negative affect, including in college (k = 19), community (k = 18), and clinical samples (k = 6; e.g., those in SUD treatment, with personality disorders, chronic pain).
We aim to advance beyond these prior studies in three ways, including (1) explicitly study the negative affect and substance use association among those experiencing more severe SUDs who are seeking treatment, (2) examine multiple substances, and (3) examine substance use outcomes in addition to use (e.g., craving). Addressing these gaps will help to understand the role of negative affect in substance use maintenance during treatment to inform intervention targets related to negative affect. Accordingly, based on the current review, we discuss treatment implications and recommend future directions for research on negative affect and substance use outcomes.
Method
Search Strategy and Scope of Review
We searched PubMed and PsycINFO databases for peer-reviewed articles published between January 2017 and April 2022 that used intensive longitudinal methods to examine relationships between negative affect and substance-related outcomes during treatment. Search terms included the following combinations: (“ecological momentary assessment” OR “experience sampling” OR “intensive longitudinal” OR “daily diary”) AND (“affect” OR “mood” OR “stress” OR “anxiety” OR “depression”) AND (“substance use” OR “alcohol use” OR “cannabis use” OR “marijuana use” OR “craving” OR “cocaine use” OR “stimulant use”). We also conducted backward searching of references cited in relevant articles and searches of articles that have subsequently cited relevant articles. Google Scholar alerts using relevant keywords were also established to capture articles published between April 2022 to submission (July 2022).
The studies included in this review used intensive longitudinal methods to examine relationships between negative affect, broadly defined (e.g., multiple negative affect states averaged, specific negative affect states, stress, PTSD symptoms), and substance use outcomes (e.g., craving, substance use frequency or intensity) among individuals in SUD treatment. All studies reviewed used intensive longitudinal methods (i.e., daily diary and/or EMA) to examine negative affect, though some studies used retrospective calendar-based methods to examine substance use outcomes. We also included three studies that did not explicitly recruit treatment-seekers but did use intensive longitudinal methods to examine mechanisms of SUD treatment (i.e., naltrexone for alcohol use [32]; topiramate for cannabis use [33, 34]). We did not review studies that only examined tobacco use outcomes to limit the scope of the review.
Results
Methodological Features of Reviewed Studies
The methodological features of the 32 reviewed studies are presented in Table 1. Overall, ten studies were conducted during alcohol treatment, 13 during opioid treatment, three during cannabis treatment, and six during SUD treatment, in which all substance types were included. Studies included randomized controlled trials of medications for SUDs or psychotherapy and naturalistic studies of individuals in outpatient or residential treatment. Most reviewed studies collected reports multiple times a day, including random or fixed reports (three to six per day) and user-initiated reports at times of drug use and high stress. However, five studies collected reports only once per day.
Negative affect and related symptom constructs were assessed using a variety of measures; 21 studies assessed averaged negative affective states or specific (e.g., anger, anxiety) negative affective states, often measured with adaptations of the Positive and Negative Affect Schedule [35, 36] or the circumplex model [37]. Fourteen studies assessed stress or stressful situations and often used single-item measures, though one study used an adaptation of the Perceived Stress Scale [38] and another used an adaptation of the Daily Inventory of Stressful Events [39]. Three studies examined PTSD symptoms, including adaptations of the PTSD Checklist (PCL)-5 and the PCL-Civilian Version [40,41,42]. Other measures assessed negative affect as a trigger for drug use [43], negative affect as a consequence of cannabis use [34], and negativity of events [44•, 45]. Several studies used measures of negative affect to calculate nuanced metrics, such as emotion differentiation (or the ability to identify one’s specific emotions) across and within individuals [46•] and instability in and persistence of negative affect and stress [43, 47, 48].
Substance-related outcomes were most commonly assessed daily or momentarily via intensive longitudinal data reports. However, some studies examined substance use outcomes measured with more traditional methods, such as calendar-based methods [47, 47] and urine drug screens [38, 43, 49]. Many studies examined craving as a correlate of negative affect, often measured via a single item representing momentary or daily craving. Consumption outcomes included substance use occurrence/frequency, quantity (e.g., number of standard drinks, grams of cannabis consumed), and subtyping of substance-related profiles (e.g., subgroups based on whether abstinence was initiated before or during treatment or never during the treatment period; [50]).
Lastly, most of the reviewed studies leveraged MLM to examine the associations between negative affect and substance-related outcomes between persons (i.e., the association between average negative affect and craving/substance use across the reporting period) or within persons (i.e., the association between daily/momentary negative affect and same-report or next-report craving/substance use). Several reviewed studies utilized multilevel mediation models or multilevel structural equation modeling to examine negative affect as a mediator of the association between a given factor (e.g., sleep quality) and substance-related outcomes [34, 51] or mediators (e.g., parental bonding, craving) of the association between negative affect and substance-related outcomes [39, 40]. Two studies used TVEM to examine the time course of relationships between negative affect and substance use [43, 52••]. Other analytic methods included latent variable modeling to examine the time course of change or subgroups of change in negative affect and substance use during treatment [50, 53•, 54] and chi-square automatic interaction detector decision trees to identify the best predictors, interactions between predictors, and cut points (including negative affect) in predicting substance-related outcomes [55].
Relationships Between Negative Affect and Craving or Substance Use in Alcohol Treatment
Between-Person Relationships
Studies examining average negative affect/stress levels and alcohol use demonstrated primarily null associations. Two naltrexone treatment trials that recruited adolescents and young adults demonstrated non-significant associations between average negative affect and the average likelihood of drinking to intoxication [56], as well as estimated blood alcohol level during drinking episodes [32]. Likewise, average negative affect and stress were not associated with drinking intensity or craving for individuals enrolled in outpatient AUD treatment [57], nor were average PTSD symptoms associated with drinking intensity following a brief intervention for co-occurring AUD and PTSD [42]. Only one study found a significant relationship between stress and substance use outcome, such that among individuals with AUD in two separate trials—one evaluating prazosin vs. placebo and the other delivering a behavioral intervention—average craving mediated the relationship between the proportion of stressful days and probability of drinking the next day [39].
Three studies also examined more complex negative affect–substance use relationships. Mean stress (measured over 6 days) from individuals with AUD engaged in community-based outpatient treatment during the first year of a recovery attempt was not associated with percent days abstinent 90 days later [47]. However, those with high levels of average stress and high levels of stress variability had lower percent days abstinent [47]. Among the same sample, lower average negative affect differentiation was associated with lower percent day abstinent but not drinking intensity [46•]. Finally, a subgroup analysis of individuals receiving prazosin or placebo for AUD revealed three subgroups: those with continuous abstinence during the first 2 weeks of treatment (already abstainers), those who initiated abstinence after the first 2 weeks of treatment (abstinence initiators), and those who drank continuously throughout the trial (continued drinkers) [50]. Already abstainers had the lowest levels of negative affect, and continued drinkers had the highest levels of negative affect, but neither group showed significant negative affect changes during treatment. Abstinence initiators were the only group to demonstrate gradual reductions in negative affect during treatment.
Within-Person Findings
Several studies among adults in various AUD treatments have demonstrated positive associations between negative affect and substance-related outcomes over time. Higher momentary negative affect and stress were associated with concurrent and prospective urges to drink among those in outpatient AUD treatment [58], particularly for those who experienced a lapse during treatment. Likewise, individuals with AUD in a trial examining stepped care demonstrated momentary associations between being in a negative affective context and the presence and intensity of craving [59]. At the daily level of analysis, positive associations between exposure to a stressful event on a given day and same-day craving and next-day likelihood of drinking and drinking intensity have also been identified among those in outpatient behavioral treatment (with or without adjunctive prazosin) [39]. Further, daily PTSD symptoms have been associated with greater than average alcohol consumption following a brief intervention for co-occurring AUD and PTSD [42].
Conversely, among adolescents/young adults receiving naltrexone, higher momentary negative affect was associated with lower daily odds of drinking to intoxication [56] and lower estimated blood alcohol levels during subsequent drinking events [32]. Analyses examining moderators of these negative relationships yielded interesting findings. Specifically, adolescents with higher trait negative urgency, a facet of impulsivity, showed positive associations between momentary negative affect and the daily likelihood of drinking to intoxication [56]. Naltrexone also moderated these associations, such that adolescents who received naltrexone versus placebo had a stronger positive relationship between estimated blood alcohol levels and subsequent negative affect and a stronger negative relationship between negative affect and subsequent estimated blood alcohol levels, particularly at later stages of a drinking event [32]. These findings indicate that naltrexone might increase the aversive effects of alcohol.
Relationships Between Negative Affect and Craving or Substance Use in Opioid Treatment
Between-Person Relationships
Negative affect was often associated with substance use outcomes (particularly craving) for those with opioid use disorder (OUD). Individuals receiving buprenorphine or methadone for OUD and reporting higher stress overall reported greater cravings for heroin and cocaine [60, 61]. Those in a residential program for OUD also demonstrated positive associations between average negative affect and craving [62]. Although some findings indicate those in buprenorphine or methadone treatment (with or without adjunctive clonidine treatment) did not demonstrate significant associations between measures of negative affect (e.g., average levels, variability, stability) and substance use [43, 48, 49], greater variability in stress (but not average stress) was associated with more frequent cocaine- and opioid-positive urine drug screens [43].
Several studies of those in OUD treatment have leveraged latent variable mixture models to examine changes in negative affect and substance-related outcomes. Burgess-Hull and colleagues [53•] identified four stress trajectories over 16 weeks of buprenorphine or methadone treatment: (1) increasing stress, (2) moderate and stable stress, (3) low stress, and (4) declining then increasing stress. Those with increasing stress and moderate and stable stress demonstrated the highest rates of any drug use and greatest levels of opioid craving compared to the low-stress group. These analyses were replicated for craving trajectories. A low craving profile reported the lowest number of stress events, and the increasing then decreasing group reported the highest number of stress events [54].
Within-Person Findings
Within-person positive associations between measures of negative affect (e.g., negative events, stress) and opioid craving were consistently identified among individuals in residential treatment for OUD [51, 62] and those receiving buprenorphine or methadone treatment [60, 61]. Those with primary OUD also evidenced momentary associations between stress and cocaine craving [61, 63]. Moderator analyses suggest that momentary relationships between stress and opioid and cocaine craving are stronger in the presence of cues [61, 63] and that the daily relationships between negative affect and craving might be weaker on days with more frequent positive social events [62].
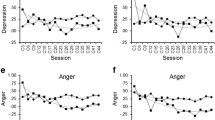
Researchers have also studied the time course of the negative affect-craving relationship. For example, Panlilio and colleagues [43] recruited individuals in buprenorphine or methadone treatment and found strong positive associations between stress and craving for 90 min following a stress event that was ranked moderate-to-extreme in severity; this association (and the presence of the time-sensitive peak) was stronger for those who used opioid and cocaine more frequently. Similarly, opioid and cocaine craving increased linearly in the 5 h before a self-initiated stress event [64]. Among those in residential treatment for OUD, negative affect-craving associations were stronger early in treatment and just before discharge than in the middle of treatment [52••]. Within the day, negative affect-craving associations were strongest during the afternoon [52••].
Only one research group examined within-person relationships between negative affect and consumption outcomes among those with OUD. Among individuals receiving buprenorphine or methadone, daily perceived stress/negative affect and drug use (e.g., opioid-positive urine drug screen, cocaine-positive urine drug screen, self-initiated drug use event) were significantly positively associated [38], and negative affect was higher during the 2–3 day collection period before an opioid-positive urine drug screens [49]. Interestingly, those receiving adjunctive clonidine (vs. placebo) treatment had higher levels of negative affect before submitting an opioid-positive urine drug screen [49]. Investigators concluded that clonidine dampened negative affect-craving associations at moderate, but not high, levels of negative affect [49]. Time course analyses identified linear increases in negative affect over the five hours before drug use was reported [64]; however, the time course of stress and drug use appears more complex. For example, one study found that stress increased linearly in the 8 h before a drug use event, but only for those with moderate and stable levels of stress (versus other stress profiles) [53•]. Alternatively, a second study found that stress was higher before a drug use event [64], but only in the 2 h preceding a drug use event.
Relationships Between Negative Affect and Craving or Substance Use in Cannabis Treatment
Between-Person Relationships
Two studies examined negative affect and substance-related outcomes in cannabis treatment [33, 34] among adolescents and young adults receiving psychosocial treatment and topiramate or placebo. Emery and colleagues [33] found that average negative affect was not associated with cannabis use frequency or quantity, and Treloar and colleagues [34] found average levels of feeling stressed/tense during a cannabis use episode were not associated with the amount of cannabis consumed. Topiramate did not moderate associations in either study.
Within-Person Findings
Associations between negative affect and cannabis use outcomes within individuals over time were largely null or negative. Studies among adults receiving psychosocial interventions [65] and adolescents/young adults receiving psychosocial treatment and topiramate or placebo [33] showed that momentary negative affect did not predict subsequent cannabis use. Further, momentary negative affect was associated with a lower likelihood of concurrently using cannabis among adolescents/young adults receiving psychosocial treatment and topiramate or placebo but did not impact the amount of cannabis consumed [33]. Additionally, there were negative, bidirectional relationships between stress during cannabis use episodes and the amount of cannabis used later that day [34].
Relationships Between Negative Affect and Craving or Substance Use in SUD Treatment
Between-Person Relationships
Two studies examined between-person relationships among PTSD symptoms and substance use outcomes in SUD treatment, where all types of SUD were included in the samples. Both studies examined these relationships among pregnant persons with a trauma history in outpatient SUD treatment and demonstrated that average PTSD symptoms were not associated with levels of craving [40] or the likelihood of drug use or drinking quantity [41].
Within-Person Findings
Several studies examined within-person relationships between negative affect and craving across different substances and co-occurring disorders. Among adults in outpatient SUD treatment, higher momentary negative affect (e.g., sad mood, anxious mood, event negativity) was concurrently associated with higher momentary opioid craving, but not alcohol or cannabis craving [45]. Likewise, increases in daily stressors were associated with greater daily cravings for illegal drugs, but not alcohol, among legal system-involved men receiving SUD pharmacotherapy [66]. Similarly, among pregnant persons with trauma histories in SUD treatment, higher daily peak PTSD symptoms were associated with a greater likelihood of any drug use but were not associated with greater daily drinking intensity [41]. Momentary negative affect was concurrently and prospectively positively associated with greater craving for adults engaged in outpatient SUD treatment, but only among those without a co-occurring mood or anxiety disorder [44•]. Lastly, an analysis among those receiving outpatient SUD treatment using decision trees to predict future reports of substance use found that negative affect significantly predicted subsequent substance use, but only for those with no recent substance use reported [55]. One study examined a mediator of the relationship between PTSD symptoms and craving among pregnant persons with a trauma history in SUD treatment, and found a positive relationship between momentary PTSD symptoms and craving that was partially mediated by lower quality of momentary parental bonding [40].
Discussion
Understanding the relationships between negative affect and substance-related outcomes may help identify mechanisms of treatment change and inform personalized interventions. We reviewed the recent literature on intensive longitudinal studies to examine associations between negative affect and substance-related outcomes among SUD treatment. Results were generally mixed and difficult to compare, given differences in methods and measurement. Nevertheless, we found more consistent relationships between negative affect measures and substance-related outcomes among those using a range of substances and in SUD treatment than a previous systematic review on cannabis use [31•] and a recent meta-analysis among primarily non-treatment-seekers drinking alcohol [30••]. These relationships tended to be stronger and more consistent at the within-person level of analysis than the between-person level, although findings were mixed at both levels of analysis.
The strength of these relationships varied across outcomes, subgroups, contexts, and time course. For example, positive associations between negative affect and substance-related outcomes appeared more consistent when measuring craving versus substance use, for those with OUD versus those with AUD or cannabis use disorder, during contexts when substance cues were present, and during specific periods (e.g., shortly following a stressor) or during specific phases of treatment (e.g., beginning or end vs. middle of treatment). Associations between negative affect and substance-related outcomes also varied based on individual-level differences (e.g., negative urgency, presence of a co-occurring psychiatric disorder).
Treatment Implications
The identified relationships between measures of negative affect and craving across substances suggest that these experiences often occur concurrently. In addition, some analyses found that substance craving prospectively influenced negative affect [44•, 64], while others found that negative affect prospectively influenced craving [58], which has significant treatment implications. As previously mentioned, those with higher negative affect tend to respond well to MBRP [16]. MBRP and other acceptance-focused mindfulness-based interventions for craving might be particularly effective in decoupling the negative affect–craving association [67]. Another study identified that below-average ability in emotion differentiation was associated with fewer percent days abstinent [46•]. Together, results suggest that skills to identify and manage negative affect might be an effective technique for reducing substance use.
Our results also have implications for intervention timing development. Increasingly sophisticated technology-delivered interventions (e.g., just-in-time adaptive interventions; [68]) can be paired with intensive longitudinal methods to maximize treatment effectiveness. For example, one study demonstrated that positive relationships between negative affect and craving were strongest at the beginning and end of residential treatment [52••]. This suggests that interventions to manage negative affect may be most beneficial when an individual is starting a treatment program or nearing discharge. The afternoon appears to be a maximally impactful time to deliver intervention content [52••]. Providers and clients may wish to discuss with clients how levels of negative affect gradually reduce over time following initiation of abstinence [50], given that increased negative affect in the context of reduced substance use might be a concern for clients.
Future Research Directions
Greater attention to individual differences within study recruitment and reporting is needed. Across the studies described in this review, there was minimal consideration of differences in relationships between negative affect and substance-related outcomes across age, gender or sexual orientation status, and racial or ethnic characteristics. Additionally, there was minimal examination of medical comorbidities, such as chronic pain, despite chronic pain contributing to the initiation and maintenance of SUD (e.g., OUD; [69]), and demonstrated relationships between pain and negative affect [70]. As we move towards personalization and precision of assessment and interventions, we must first understand how the associations between negative affect and substance-related outcomes vary as a function of individual-level differences.
Additionally, few studies reported on co-occurring mood, anxiety, and trauma-related symptoms (outside of studies explicitly focused on co-occurrence; [42, 44•]), although co-occurrence is frequently reported among treatment-seeking populations (as discussed in Schulden & Blanco, 2021; [71]). Our review demonstrated mixed evidence regarding the magnitude, valence, and direction of relationships between negative affect and substance-related outcomes as a function of co-occurring disorders. Given the increasing implementation of integrated treatments for those with SUD and co-occurring psychiatric disorders, it is important to understand transdiagnostic factors that impact the association between negative affect and substance-related outcomes and focus on recruitment of individuals with SUD and co-occurring psychiatric disorders. Additionally, we call for explicit measurement of multiple substances and simultaneous use, as polysubstance use is often reported among those seeking treatments [72]. Intensive longitudinal methods can examine negative affective factors that drive poly- or simultaneous-use episodes.
Across reviewed studies, there was clear variability in negative affect measures (see Table 1), making it challenging to synthesize findings across studies. However, a notable strength of this review was the inclusion of more nuanced measures of negative affect, such as emotion differentiation, variability, and persistence. Additional research is needed to develop and strengthen our repertoire of negative affect measures and to improve our psychometric understanding of these more nuanced measures. Future work should leverage observational, experimental, qualitative, and person-specific methods to better understand the relationships between multiple measures of negative affect and substance-related outcomes. For example, reviewed research suggests that the associations between negative affect and substance-related outcomes varied significantly within individuals, across the day, and at different phases during treatment [53•]. As such, intensive longitudinal methods could use user-initiated prompts to assess substance-related outcomes at times with above-average negative affect (e.g., [60]) and with follow-up prompts to assess the time course of negative affect and substance-related outcomes. Likewise, experimental methods could randomize the intensity and/or schedule of assessments to better characterize the time course of the associations between negative affect and substance-related outcomes as they fluctuate over time and across treatment. Moreover, qualitative interviews with individuals with SUDs could help determine which negative affect measures use terminology most applicable and accessible to treatment-seeking populations and which indicators of negative affect (e.g., average vs. peak levels, specific constructs, or differentiation) are perceived to be the most tied to substance use [73•]. Finally, pairing qualitative interviews with person-specific methods and statistical models [26•] could increase our understanding of heterogeneity in the association between negative affect and substance-related outcomes (see [29] for an illustrative example). We recommend that future studies characterize the relationships between negative affect and substance-related outcomes using methods sensitive to variance over time (e.g., time-varying effects model; [22]) and person-specific differences [23]).
Limitations of the Present Review
The present review was not systematic and limited to recent intensive longitudinal studies published in the last 5 years. Additionally, many reviewed findings came from the same parent studies, including all between-person studies on negative affect and cannabis use and all within-person studies on negative affect and opioid use. We chose to focus on individuals in SUD treatment as these individuals may most likely demonstrate relationships between negative affect and substance use [5, 12] and is an important population to study for the purposes of developing novel treatments. However, many studies focused on pharmacotherapies for SUD, which might attenuate negative affect and craving, thus impacting outcomes. Lastly, we focused on negative affect-related variables but did not examine other similar constructs that have received less attention in the field (e.g., low positive affect, anhedonia) and may also be associated with outcomes in SUD treatment. Some findings indicate that positive affect may play a more important role in substance use than negative affect [30••].
Conclusions
Understanding relationships between negative affect and substance-related outcomes during treatment may help inform personalized interventions. Results on the associations between negative affect and craving or substance use were generally mixed, and the strength and direction of these relationships varied across outcomes, subgroups, contexts, and time course. Our review indicated the need for interventions that target the negative affect-craving association (e.g., MBRP) and times when such interventions might be most effective (e.g., immediately before treatment discharge). Future research should increase attention to individual differences (e.g., race and ethnicity) and recruitment of individuals with co-occurring disorders and polysubstance use. Experimental, qualitative, and person-specific methods are needed to help understand the relationships between negative affect and substance-related outcomes during treatment.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cox WM, Klinger E. A motivational model of alcohol use. J Abnorm Psychol. 1988;97:168–80.
Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. J Pers Soc Psychol. 1995;69:990–1005.
Cooper M, Kuntsche E, Levitt A, Barber LL, Wolf S. Motivational models of substance use a review of theory and research on motives for using alcohol marijuana and tobacco. In Sher KJ editor The Oxford Handbook Subs Use Disorders. 2015;1:375–421.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacol. 2010;35(1):217–38.
Koob GF, Buck CL, Cohen A, Edwards S, Park PE, Schlosburg JE, et al. Addiction as a stress surfeit disorder. Neuropharmacol. 2014;76:370–82.
Solomon RL, Corbit JD. An opponent-process theory of motivation: I. Temporal dynamics affect Psychol Rev. 1974;2:119–45.
Lai HMX, Cleary M, Sitharthan T, Hunt GE. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: a systematic review and meta-analysis. Drug Alcohol Depend. 2015;154:1–13.
Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from wave 2 of the national epidemiologic survey on alcohol and related conditions. J Anxiety Disord. 2011;25:456–65.
Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas KR, et al. Mental disorders as risk factors for substance use, abuse and dependence: results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 2010;105:1117–28.
Helle AC, Trull TJ, Watts AL, McDowell Y, Sher KJ. Psychiatric comorbidity as a function of severity: DSM-5 alcohol use disorder and HiTOP classification of mental disorders. Alcohol Clin Exp Res. 2020;44:632–44.
Moss HB, Chen CM, Yi HY. Measures of substance consumption among substance users, DSM-IV abusers, and those with DSM-IV dependence disorders in a nationally representative sample. J Stud Alcohol Drugs Alcohol Res Doc, Inc. 2012;73:820–8.
Blanco C, Iza M, Rodríguez-Fernández JM, Baca-García E, Wang S, Olfson M. Probability and predictors of treatment-seeking for substance use disorders in the U.S. Drug Alcohol Depend. 2015;149:136–44.
Swan JE, Votaw VR, Stein ER, Witkiewitz K. The role of affect in psychosocial treatments for substance use disorders. Curr Addict Rep Springer. 2020;1(2):108–16.
Votaw VR, Stein ER, Witkiewitz K. A Longitudinal mediation model of negative emotionality, coping motives and drinking intensity among individuals receiving community treatment for alcohol use disorder. Alcohol Alcohol. 2021.
Witkiewitz K, Bowen S. Depression craving and substance use following a randomized trial of mindfulness-based relapse prevention. J Consult Clin Psychol US Am Psychol Assoc. 2010;78:362–74.
Roos CR, Bowen S, Witkiewitz K. Baseline patterns of substance use disorder severity and depression and anxiety symptoms moderate the efficacy of mindfulness-based relapse prevention. J Consult Clin Psychol. 2017;85:1041–51.
Roos CR, Mann K, Witkiewitz K. Reward and relief dimensions of temptation to drink: construct validity and role in predicting differential benefit from acamprosate and naltrexone. Addict Biol. 2017;22:1528–39.
Magill M, Tonigan JS, Kiluk B, Ray L, Walthers J, Carroll K. The search for mechanisms of cognitive behavioral therapy for alcohol or other drug use disorders: a systematic review. Behav Res Ther. 2020;131:103648.
Tomko RL, McClure EA. Introduction to the special issue: utilizing ambulatory assessment to better understand the etiology, maintenance, treatment, and remission of addictive disorders. Addict Behav Netherlands: Elsevier Sci. 2018;83:1–4.
Shiffman S. Conceptualizing analyses of ecological momentary assessment data. Nicotine Tob Res. 2014;16:S76-87.
Bolger N, Laurenceau J-P. Intensive longitudinal methods: an introduction to diary and experience sampling research. New York, NY: The Guilford Press; 2013.
Tan X, Shiyko MP, Li R, Li Y, Dierker L. A time-varying effect model for intensive longitudinal data. Psychol Methods US: Am Psychol Assoc. 2012;17:61–77.
Foster KT, Beltz AM. Advancing statistical analysis of ambulatory assessment data in the study of addictive behavior: a primer on three person-oriented techniques. Addict Behav. 2018;83:25–34.
Piccirillo ML, Rodebaugh TL. Foundations of idiographic methods in psychology and applications for psychotherapy. Clin Psychol Rev. 2019;71:90–100.
Moskowitz DS, Young SN. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J Psychiatry Neurosci. 2006;31:13–20.
Piccirillo ML, Beck ED, Rodebaugh TL. A clinician’s primer for idiographic research: considerations and recommendations. Behavior Therapy. 2019;50:938–51. Provides an overview of idiographic (i.e., individual-level) designs within clinical psychology, including a reader-friendly summary of design and data collection considerations, data analytic techniques, and a hypothetical example.
Carpenter SM, Menictas M, Nahum-Shani I, Wetter DW, Murphy SA. Developments in mobile health just-in-time adaptive interventions for addiction science. Curr Addict Rep. 2020;7:280–90. Provides an overview of just-in-time adaptive interventions in addiction science, including existing interventions, design of just-in-time adaptive interventions, and future directions in this area of research.
Frumkin MR, Piccirillo ML, Beck ED, Grossman JT, Rodebaugh TL. Feasibility and utility of idiographic models in the clinic: a pilot study. Psychother Res Routledge. 2021;31:520–34.
Piccirillo ML, Enkema M, Foster KT. Using ambulatory assessment to support clinical practice: an illustration with problematic cannabis use. [Internet]. 2022. Available from: https://doi.org/10.31234/osf.io/jxmk7.
Dora J, Piccirillo M, Foster KT, Arbeau K, Armeli S, Auriacombe M, et al. The daily association between affect and alcohol use: a meta-analysis of individual participant data [Internet]. PsyArXiv; 2022 Feb. Available from:https://osf.io/xevct. A meta-analysis of participant-level data from 69 studies (N=12,394), which showed that daily negative affect was not associated with daily drinking likelihood or quantity. However, higher daily positive affect was associated with an increased likelihood of drinking and greater drinking intensity.
Wycoff AM, Metrik J, Trull TJ. Affect and cannabis use in daily life: a review and recommendations for future research. Drug alcohol dependence. 2018;191:223–33. A systematic review of ecological momentary assessment and daily diary studies that examined associations between affect and cannabis use. Concerning negative affect, the authors of the systematic review concluded that momentary and daily negative affect (particularly anger/hostility) were concurrently associated with cannabis use among samples experiencing significant levels of psychopathology (e.g., SUDs, personality disorders). However, results were equivocal and mixed for community and college student samples.
Carpenter RW, Emery NN, Meisel SN, Miranda R. Naltrexone moderates the association of alcohol use and affect among adolescent drinkers in daily life. Alcohol Clin Exp Res. 2022;46:326–37.
Emery NN, Carpenter RW, Meisel SN, Miranda R. Effects of topiramate on the association between affect, cannabis craving, and cannabis use in the daily life of youth during a randomized clinical trial. Psychopharmacol. 2021;238:3095–106.
Treloar Padovano H, Miranda R. Using ecological momentary assessment to identify mechanisms of change: an application from a pharmacotherapy trial with adolescent cannabis users. J Stud Alcohol Drugs. 2018;79:190–8.
Watson D, Clark LA. The PANAS-X: Manual for the positive and negative affect schedule-expanded form. University of Iowa. 1999. https://doi.org/10.17077/48vt-m4t2.
Thompson ER. Development and validation of an internationally reliable short-form of the positive and negative affect schedule (PANAS). J Cross-Cult Psychol SAGE Publications Inc. 2007;38:227–42.
Larsen RJ, Diener E. Promises and problems with the circumplex model of emotion. Emotion. Thousand Oaks, CA, US: Sage Publications, Inc; 1992;25–59.
Preston KL, Schroeder JR, Kowalczyk WJ, Phillips KA, Jobes ML, Dwyer M, et al. End-of-day reports of daily hassles and stress in men and women with opioid-use disorder: relationship to momentary reports of opioid and cocaine use and stress. Drug Alcohol Depend. 2018;193:21–8.
Wemm SE, Larkin C, Hermes G, Tennen H, Sinha R. A day-by-day prospective analysis of stress, craving and risk of next day alcohol intake during alcohol use disorder treatment. Drug Alcohol Depend. 2019;204:107569.
Sanjuan PM, Pearson MR, Fokas K, Leeman LM. A mother’s bond: an ecological momentary assessment study of posttraumatic stress disorder symptoms and substance craving during pregnancy. Psychol Addict Behav. 2020;34:269–80.
Sanjuan PM, Pearson MR, Poremba C, de LA Amaro H, Leeman L. An ecological momentary assessment study examining posttraumatic stress disorder symptoms, prenatal bonding, and substance use among pregnant women. Drug Alcohol Depend. 2019;195:33–9.
Campbell SB, Krenek M, Simpson TL. The role of patient characteristics in the concordance of daily and retrospective reports of PTSD. Behav Ther. 2017;48:448–61.
Panlilio LV, Stull SW, Bertz JW, Burgess-Hull AJ, Lanza ST, Curtis BL, et al. Beyond abstinence and relapse II: momentary relationships between stress, craving, and lapse within clusters of patients with similar patterns of drug use. Psychopharmacol. 2021;238:1513–29.
Fatseas M, Serre F, Swendsen J, Auriacombe M. Effects of anxiety and mood disorders on craving and substance use among patients with substance use disorder: an ecological momentary assessment study. Drug Alcohol Depend. 2018;187:242–8. One reviewed study focused on differences in the association between negative affect and substance-related outcomes by the presence or absence of a co-occurring psychological disorder. Interestingly, in this sample, momentary negative affect was concurrently and prospectively positively associated with greater craving for adults engaged in outpatient SUD treatment, but only among those without a co-occurring mood or anxiety disorder.
Serre F, Fatseas M, Denis C, Swendsen J, Auriacombe M. Predictors of craving and substance use among patients with alcohol, tobacco, cannabis or opiate addictions: Commonalities and specificities across substances. Addict Behav. 2018;83:123–9.
Emery NN, Walters KJ, Njeim L, Barr M, Gelman D, Eddie D. Emotion differentiation in early recovery from alcohol use disorder: associations with in-4 the-moment affect and 3-month drinking outcomes. Alcohol Clin Exp Res; in press. Available from: https://osf.io/zv5mt/. Calculated person-level and momentary-level emotion differentiation and showed that below-average ability in negative emotion differentiation was associated with fewer percent days abstinence. In addition, moments with higher than average negative affect were associated with worse than average negative emotion differentiation, which underscores the need for Just-In-Time Adaptive Interventions to identify and cope with negative affect.
Eddie D, Barr M, Njeim L, Emery N. Mean versus variability: disentangling stress effects on alcohol lapses among individuals in the first year of alcohol use disorder recovery. J Stud Alcohol Drugs. 2021;82:623–8.
Ellis JD, Mun CJ, Epstein DH, Phillips KA, Finan PH, Preston KL. Intra-individual variability and stability of affect and craving among individuals receiving medication treatment for opioid use disorder. Neuropsychopharmacol. 2022;47:1836–43.
Kowalczyk WJ, Moran LM, Bertz JW, Phillips KA, Ghitza UE, Vahabzadeh M, et al. Using ecological momentary assessment to examine the relationship between craving and affect with opioid use in a clinical trial of clonidine as an adjunct medication to buprenorphine treatment. Am J Drug Alcohol Abuse. 2018;44:502–11.
Hallgren KA, Delker BC, Simpson TL. Effects of initiating abstinence from alcohol on daily craving and negative affect results from a pharmacotherapy clinical trial. Alcohol Clin Exp Res. 2018;42:634–45.
Lydon-Staley DM, Cleveland HH, Huhn AS, Cleveland MJ, Harris J, Stankoski D, et al. Daily sleep quality affects drug craving, partially through indirect associations with positive affect, in patients in treatment for nonmedical use of prescription drugs. Addict Behav. 2017;65:275–82.
Jenkins GJ, Cleveland MJ, Knapp KS, Bunce SC, Cleveland HH. Examining the time-varying association of negative affect and covariates with craving during treatment for prescription opioid dependence with two types of mixed models. Addict Behav. 2021;113:106674. Used time-varying effects models to examine the time course of associations between negative affect and craving during residential opioid use disorder treatment and showed that positive associations were strongest at the beginning and end of residential treatment and in the afternoon. This study has implications for times to deliver interventions that target negative affect-craving relationships.
Burgess-Hull AJ, Smith KE, Schriefer D, Panlilio LV, Epstein DH, Preston KL. Longitudinal patterns of momentary stress during outpatient opioid agonist treatment: a growth-mixture-model approach to classifying patients. Drug Alcohol Depend. 2021;226:108884. Used momentary stress ratings from ecological momentary assessment reports to identify stress trajectories during agonist treatment for opioid use disorder. The researchers identified four stress trajectories (i.e., increasing, moderate and stable, declining and increasing, low) and showed differences in craving, drug use, and associations between stress and drug use across the four trajectory groups.
Burgess-Hull AJ, Panlilio LV, Preston KL, Epstein DH. Trajectories of craving during medication-assisted treatment for opioid-use disorder: subtyping for early identification of higher risk. Drug Alcohol Depend. 2022;233:109362.
Scott CK, Dennis ML, Gustafson DH. Using ecological momentary assessments to predict relapse after adult substance use treatment. Addict Behav. 2018;82:72–8.
Bold KW, Fucito LM, DeMartini KS, Leeman RF, Kranzler HR, Corbin WR, et al. Urgency traits moderate daily relations between affect and drinking to intoxication among young adults. Drug Alcohol Depend. 2017;170:59–65.
Szeto EH, Schoenmakers TM, van de Mheen D, Snelleman M, Waters AJ. Associations between dispositional mindfulness, craving, and drinking in alcohol-dependent patients: an ecological momentary assessment study. Psychol Addict Behav. 2019;33:431–41.
Waters AJ, Schoenmakers TM, Snelleman M, Szeto EH, Franken IHA, Hendriks VM, et al. Affect, motivation, temptation, and drinking among alcohol-dependent outpatients trying to maintain abstinence: an ecological momentary assessment study. Drug Alcohol Depend. 2020;206:107626.
Kuerbis AN, Shao S, Treloar Padovano H, Jadanova A, Selva Kumar D, Vitale R, et al. Context and craving among individuals with alcohol use disorder attempting to moderate their drinking. Exp Clin Psychopharmacol. 2020;28:677–87.
Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin J-L, et al. Context and craving during stressful events in the daily lives of drug-dependent patients. Psychopharmacol. 2017;234:2631–42.
Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin J-L, et al. Exacerbated craving in the presence of stress and drug cues in drug-dependent patients. Neuropsychopharmacol. 2018;43:859–67.
Knapp KS, Bunce SC, Brick TR, Deneke E, Cleveland HH. Daily associations among craving, affect, and social interactions in the lives of patients during residential opioid use disorder treatment. Psychol Addict Behav US Am Psychol Assoc. 2021;35:609–20.
Moran LM, Kowalczyk WJ, Phillips KA, Vahabzadeh M, Lin J-L, Mezghanni M, et al. Sex differences in daily life stress and craving in opioid-dependent patients. Am J Drug Alcohol Abuse. 2018;44:512–23.
Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin J-L, et al. Before and after: craving, mood, and background stress in the hours surrounding drug use and stressful events in patients with opioid-use disorder. Psychopharmacol. 2018;235:2713–23.
Litt MD, Kadden RM, Tennen H, Dunn HK. Momentary coping and marijuana use in treated adults: exploring mechanisms of treatment. J Consult Clin Psychol. 2021;89:264–76.
Neupert SD, Desmarais SL, Gray JS, Cohn AM, Doherty S, Knight K. Daily stressors as antecedents, correlates, and consequences of alcohol and drug use and cravings in community-based offenders. Psychol Addict Behav. 2017;31:315–25.
Korecki JR, Schwebel FJ, Votaw VR, Witkiewitz K. Mindfulness-based programs for substance use disorders: a systematic review of manualized treatments. Substance Abuse Treatment, Prevention, and Policy. 2020;15:1–37.
Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, et al. Just-in-time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann Behav Med. 2017;52:446–62.
Speed TJ, Parekh V, Coe W, Antoine D. Comorbid chronic pain and opioid use disorder literature review and potential treatment innovations. Int Rev Psychiatry Taylor Francis. 2018;30:136–46.
Ferguson E, Zale E, Ditre J, Wesolowicz D, Stennett B, Robinson M, et al. CANUE: a theoretical model of pain as an antecedent for substance use. Ann Behav Med. 2021;55:489–502.
Schulden JD, Blanco C. Epidemiology of co-occurring psychiatric and substance use disorders. In: Brady KT, Levin FR, Galanter M, Kleber HD, editors. The American Psychiatric Association publishing textbook of substance use disorder treatment, sixth edition. American Psychiatric Publishing, Inc; 2021.
Bhalla IP, Stefanovics EA, Rosenheck RA. Clinical epidemiology of single versus multiple substance use disorders: polysubstance use disorder. Med Care. 2017;55:S24.
Soyster PD, Fisher AJ. Involving stakeholders in the design of ecological momentary assessment research: an example from smoking cessation. PLOS ONE Public Libr Sci. 2019;14:e0217150. Discusses the importance of involving stakeholders in developing intensive longitudinal methods, particularly choosing survey questions that balance the most relevant constructs with minimal participant burden. This manuscript also describes the methods and results of a focus group discussion with current tobacco users to inform the design of a person-centered ecological momentary assessment study aimed at identifying factors increasing or decreasing the likelihood of tobacco use.
Weathers FW, Ford J. Psychometric properties of the PTSD Checklist (PCL-C, PCL-S, PCL-M, PCL-PR). In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press; 1996.
Erbas Y, Kalokerinos EK, Kuppens P, van Halem S, Ceulemans E. Momentary emotion differentiation the derivation and validation of an index to study within-person fluctuations in emotion differentiation. A SAGE Publ Inc. 2022;29:700–16.
Almeida DM, Wethington E, Kessler RC. The daily inventory of stressful events an interview-based approach for measuring daily stressors. A SAGE Publ Inc. 2002;9:41–55.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96.
Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) [Internet]. National Center for PTSD; 2013. Available from: http://www.ptsd.va.gov.
Funding
The preparation of this article was supported in part by grants from the National Institute on Alcohol Abuse and Alcoholism (F31AA029266, T32AA018108, R01AA022328, K99AA029459).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
Table 1 is an original table created by the authors of the manuscript and has not previously been published.
Conflict of Interest
Dr. Katie Witkiewitz is a member of the Alcohol Clinical Trials Initiative Workgroup; its activities were supported by Alkermes, Dicerna, Ethypharm, Lundbeck, Mitsubishi, and Otsuka in the past 36 months. The other authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Emotion and Addiction.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Votaw, V.R., Tuchman, F.R., Piccirillo, M.L. et al. Examining Associations Between Negative Affect and Substance Use in Treatment-Seeking Samples: a Review of Studies Using Intensive Longitudinal Methods. Curr Addict Rep 9, 445–472 (2022). https://doi.org/10.1007/s40429-022-00441-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-022-00441-8