Abstract
Purpose of Review
Ultra-processed foods (UPFs) contain little whole foods, and are associated with increased risk for several, adverse cardio-metabolic health outcomes; yet, UPFs are ubiquitous in the food environment and comprise a significant percentage of calories consumed. Cutting down on UPFs may be challenging, with increasing evidence to support that UPFs may exhibit an addictive potential not observed with minimally processed foods. This narrative review aimed to discuss challenges UPFs pose for dietary adherence and examine evidence pertaining to attempts to cut down on UPFs.
Recent Findings
Findings support an overall high prevalence of unsuccessful attempts to cut down; however, challenges exist with quantifying attempts specifically attributable to UPFs. Emerging research supports that for some individuals, UPFs, compared to minimally processed foods generate greater addictive-like responses.
Summary
UPF consumption facilitates addictive-like eating behaviors in some individuals and evidence supports a greater abuse liability than minimally processed foods, which may pose a unique challenge for diet adherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last 40 years, the prevalence of obesity has increased worldwide, concurrent with the prevalence of weight loss attempts [1]. A systematic review and meta-analysis of weight loss attempts including more than 70 studies and more than one million adults revealed that 42% of the population worldwide reported trying to lose weight at some point [2•]. In the USA, data collected in the National Health and Nutrition Examination Survey (NHANES) from 2013 to 2016 indicated that almost half (49.1%) of adults actively tried to lose weight in the last 12 months [3]. Strategies most commonly employed by individuals trying to lose weight are in-line with healthcare professional recommended, evidence-based guidelines for weight management and include an increase in physical activity and eating a healthier diet [2•, 3].
Generally, attempting to eat a healthier diet centers on improving diet quality by increasing consumption of fruits and vegetables, while reducing consumption of “junk foods” [2•]. What falls into the unofficial category of “junk food” is not specifically delineated, but items commonly associated with this term include foods such as pizza, pastries, ice cream, potato chips, cookies, French fries, and carbonated soft drinks. Likewise, many of these also fall into a food classification system known as ultra-processed foods (UPFs) [4]. Although there is some disagreement in the exact categorization of certain foods and beverages as UPFs, the most accepted and applied food classification system in the scientific literature is the NOVA (not an acronym) system [4]. UPFs do not occur naturally (think fish “sticks” vs. whole fish); they are industrial formulations strategically manufactured to create a product that is shelf-stable, inexpensive to make and purchase, and highly palatable. They are often energy-dense, nutrient deficient, and contain a sophisticated mixture of refined carbohydrates (i.e., sugar), salt, and fat (e.g., salty snacks, fast food, sugar-sweetened beverages, ice cream) [4, 5]. Despite containing little to no whole foods, UPFs are ubiquitous in the food environment, and comprise a significant percentage of calories consumed by both adults and children, particularly in high-income countries [6•, 7]. In Canada, the UK, and the USA, approximately 45.0%, 50.4%, and 57.9% of total energy intake, respectively, purportedly comes from UPFs [8,9,10]. A similar trend was observed in US adolescents as a recent study reported that ~ two-thirds of total energy intake was derived from UPFs [7]. While highly palatable and appealing, consumption of UPFs is associated with the development of obesity, and contributes to an increased risk for a number of adverse health conditions including hypertension, metabolic syndrome, cardiovascular disease, type 2 diabetes, and all-cause mortality [6•]. Moreover, compared to naturally occurring and minimally processed foods (e.g., fruits, vegetables, lean meats, brown rice), there is increasing evidence to support that UPFs impact reward-related systems in the brain, and in some individuals may trigger addictive-like behaviors (e.g., intense cravings, impaired control) [11].
In an effort to capture these addictive-like behaviors, the Yale Food Addiction Scale (YFAS) was developed and validated [12]. The YFAS was based on the Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV [13] substance use disorder diagnostic criteria to evaluate symptoms and behaviors of “addictive-like” eating. The YFAS paralleled substance use disorder symptoms such as too much time spent obtaining food, feelings of withdrawal, important activities given up, unsuccessful attempts to quit, continued use despite consequences, and others. In 2013, the YFAS-Children (YFAS-C) was developed and validated to assess addictive-like eating behaviors in children (mean age = 8.32 years) [14]. Although not recognized as a clinical diagnosis, food addiction (FA) can be determined with the YFAS and YFAS-C with the presence of three or more symptoms and clinically significant impairment or distress. In accordance with updates to substance use disorder criteria in the DSM-5 [15], the YFAS 2.0 was similarly re-developed to include more symptoms (n = 11) and to differentiate FA severity based on symptom counts (mild: 2–3, moderate: 4–5, severe: ≥ 6) [16]. A child scale, the Dimensional Yale Food Addiction Scale for Children 2.0 [17], was also re-developed to reflect the updated DSM-5 criteria; however, the dimensional scoring approach is more sensitive to sub-clinical variations in FA symptoms and a FA diagnostic score is not calculated. Although the YFAS and YFAS 2.0 were developed with the intent to measure addictive-like eating behaviors and FA, UPFs were not directly assessed as the mechanism underlying these behaviors. In 2017, however, a study by Schulte et al. [18] identified that UPFs were significantly and positively associated with FA symptoms and this relationship was even more pronounced in those who met the diagnostic criteria for FA. This study provided the first, preliminary evidence that UPFs, compared to minimally processed foods, were more likely to exhibit an addictive potential [18].
Not all individuals who exhibit symptoms of addictive-like eating will meet the diagnostic criteria for FA; however, the symptoms of FA should not be overlooked, particularly in regard to recent research on UPFs and their addictive potential. Perhaps more importantly, which symptom(s) are commonly endorsed warrant closer examination. Considering the pervasiveness of diet culture and prevalence of people worldwide who have attempted to lose weight [2•], it may come as no surprise that one of the most commonly endorsed FA symptoms is the “persistent desire or repeated unsuccessful attempts to quit.” This aligns with current evidence regarding weight loss attempts—they are largely unsuccessful long-term, lead to more weight gain, and more futile weight loss attempts (i.e., weight cycling) [1]. Yet, where do UPFs fit into this scenario?
With this narrative review, we sought to examine the research, primarily from the last 5 years, to examine how UPFs may present as a challenge for diet adherence, and to take a closer look at the FA symptom, unsuccessful attempts to cut down, and challenges associated with accurately quantifying these attempts. We explored several databases including PubMed, PsycINFO, Ovid, and Google Scholar as well as references from relevant articles to identify peer-reviewed studies pertinent to the topic. Identified articles, published in English and regardless of study design, were considered. The overall aim was to discuss why UPFs may pose a distinct challenge for dietary adherence and examine the existing evidence pertaining to attempts to cut down on UPFs.
Challenges to Healthy Eating in a World of UPFs
Diet adherence is the extent to which an individual follows/complies with dietary recommendations [19]. This can be a diet prescribed by a healthcare professional to help manage a chronic condition (e.g., celiac, diabetes, etc.) or dietary guidelines developed by government entities (i.e., Dietary Guidelines for Americans) to achieve and/or maintain good health. Whatever the recommended diet, in order to achieve the desired/expected outcome, adherence is a critical factor [19]. Furthermore, for short- and long-term weight loss success, a higher level of diet adherence rather than a specific diet type (i.e., low calorie, low carbohydrate) may be more important [19]. Given the marked prevalence of UPFs in both the food environment and dietary intake [6•], it seems prudent to consider how UPFs may pose a unique challenge to diet adherence. There are several, plausible mechanisms by which UPFs physiologically disrupt the human body warrants attention particularly when considering how they may pose challenges to diet adherence.
Energy homeostasis involves a series of complex circuits and feedback loops between the gut and brain. The circuit and feedback loops are regulated by hormonal and neural signaling to control caloric intake, hunger, satiety, and eating behaviors in order to maintain an adequate balance of energy [20]. Although an in-depth examination of satiety and hunger is beyond the scope of this narrative, we present an overview of how UPFs, as sophisticated combinations of macronutrients, food additives (e.g., flavor enhancers, colors) along with complex processing, dysregulate innate neuro-enteric mechanisms. As a result, individuals tend to overconsume such foods and with time, gain weight. For example, mounting evidence in rodent models suggests that high fructose corn syrup, a major ingredient in UPFs, alters the colonization and diversity within the gut (i.e., dysbiotic microbiota) [21, 22]. With chronic ingestion, alterations in glucose tolerance, hepatic metabolism, lipid neogenesis, and oxidative stress occur—all antecedent to the development of metabolic dysregulation. During this process and with increasing levels of adiposity, there is further dysregulation of key satiety hormones (e.g., leptin, ghrelin, and insulin) as well as impaired signaling to the arcuate nucleus, an area of the hypothalamus involved in energy homeostasis that influences food seeking and eating behaviors [23]. Findings from neuroimaging studies support that cues for UPFs (e.g., milkshakes) activate the reward/motivation systems in a similar manner as those observed for drugs of dependence [24, 25]. Moreover, repeated, high levels of UPF consumption may induce a hormonal resistance (e.g., insulin, leptin) and blunt the response from the systems that work to counteract excessive caloric intake [26••, 27]. The speed at which UPFs are absorbed, and the speed and magnitude of a reward signal delivered, encourages repeated consumption of UPFs; ultimately, this self-perpetuating process is a prime facilitator of addictive-like eating behaviors in some individuals and may override normal cognitive control brain mechanisms similar to those found in habit-forming substances [25, 26••, 28]. This scenario may sound analogous to that, which one may expect to hear when discussing a substance use disorder. Notably, there is a growing body of evidence to support that UPFs may have dependence (i.e., abuse) liability similar to those observed with habit-forming drugs (e.g., cigarettes, alcohol, and illicit drugs) [29••].
In 2017, Schulte et al. [30] sought to determine which foods might be most associated with addictive-like eating. Subjective experience indicators of abuse liability (i.e., craving, pleasure liking, intensity, and averseness) for 30 nutritionally diverse foods were obtained from an online sample of 507 adults [30]. Cluster analytic techniques were employed to group foods based on each of the subjective indicators of abuse liability. Results indicated that foods might not be equally reinforcing; rather, they may fall on a risk spectrum in terms of their association with addictive-like eating behaviors. Clustered together, UPFs were associated with endorsements of greater loss of control, liking, pleasure, and craving compared to minimally processed foods. Overall, UPFs appeared to have the greatest habit forming or “addictive” potential [30]. Building upon this preliminary work and utilizing robust, behavioral methodology from substance abuse literature, Schulte et al. [29••] examined further the addictive potential of foods. Findings again supported that UPFs have a greater abuse liability compared to minimally processed foods.
Recent, emerging research supports that for some individuals, highly rewarding UPFs, compared to minimally processed foods, generate greater addictive-like responses including more frequent and stronger cravings, loss of control, and distress when intake is restricted [11, 31]. A neuroimaging study conducted by DiFeliceantonio et al. in 2018 [32] was the first to demonstrate that foods high in both carbohydrates and fat, the combination of which is not readily found in non-processed foods, elicited supra-additive striatal responses. The potentiated reward signal generated by these UPFs may help explain why certain foods are craved more than others and subsequently play an influential role in overeating [28]. In a recent mixed method study, Neff et al. [33] explored the relationship between nutritional characteristics and addictive-like eating in a group of self-identified “food addicts.” A sample of 182 adults responded to open-ended questions as to which foods they believed they were addicted. The vast majority (84%) of the foods identified as addictive were considered UPFs; only six of the 51 unique foods did not meet the criteria for classification into one of the “high” sugar, fat, or salt categories. Furthermore, over half of this community sample met the YFAS FA diagnosis criteria (52.2%) with a reported mean of 5.40 FA symptoms for the group [33]. Collectively, findings support an abuse liability of UPFs, an addictive potential not commonly observed of minimally processed foods.
(Un)successful Attempts to Cut Down on UPFs
Central to evidence-based recommendations for obesity prevention and treatment are dietary approaches that emphasize eating behavior changes including an increased consumption of nutrient-dense foods (i.e., whole grains, vegetables) and cutting down on energy-dense, nutrient deficient foods (i.e., UPFs) [34]. The ability to cut down on UPFs is vital to not only achieving weight loss goals, but also to potentially warding off adverse health conditions. It is also one of the symptoms captured with the YFAS scales, specifically delineated as the “persistent desire or repeated unsuccessful attempts to quit” [16].
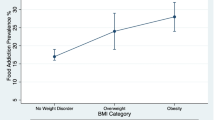
The first systematic review and meta-analysis of studies (n = 25) that examined FA prevalence and symptoms using the YFAS was conducted in 2014 [35]. The weighted mean prevalence of FA diagnosis in the adult population sample was 19.9%; however, the most commonly reported symptom in 70% of studies was “the persistent desire or unsuccessful attempts to cut down food intake.” The majority of studies included in this initial review were comprised of females with overweight/obesity, and recruited from clinical settings, thereby limiting the generalizability of the findings [35]. However, a cross-sectional investigation of FA and dietary profiles conducted shortly thereafter by Pursey et al. [36] observed a similar pattern in healthy, young adults (mean age = 24.1 years). While only 14.7% of the 435 respondents (~ 73% classified as healthy weight) met the YFAS criteria for FA, 94.2% reported at least one FA symptom. The most commonly endorsed symptom was the persistent desire or unsuccessful attempts to cut down at 91.6% followed by the continued use despite adverse consequences at 37.2% [36]. A similar study investigated FA and foods implicated in addictive-like eating in young adults, and again the most commonly endorsed symptom (91.7%) was the persistent desire or repeated unsuccessful attempt to quit [18]. Furthermore, the most commonly endorsed symptoms by individuals with obesity awaiting bariatric surgery were the persistent desire or repeated unsuccessful attempts to quit and continued use despite adverse consequences at 49% and 50%, respectively [37].
Investigations of FA and FA symptoms in adolescents yielded results analogous to those observed in adults, particularly in regard to FA symptom prevalence. Meule et al. [38] conducted one of the first studies to explore FA in adolescents in 2015. The YFAS was administered to 50 adolescents with obesity (mean age = 16.50 years) prior to entering an inpatient, weight management program. Nineteen adolescents (38%) met the criteria for FA; however, almost every participant (94%) endorsed the repeated, unsuccessful attempts to cut down symptom [38]. In two recent examinations of FA in adolescents entering outpatient, weight management programs, this symptom was again the most commonly endorsed [39, 40]. In a sample of Caucasian adolescents with obesity, 30.7% met the criteria for FA, 50% endorsed three or more symptoms of FA, and the inability to cut down was the most commonly reported symptom along with the continued use despite problems (both 53.8%) [39]. Likewise, in a sample of African American adolescents with obesity, 10.1% met the diagnosis criteria for FA, 35% reported three or more symptoms, and the unsuccessful attempt to cut down was again the highest reported symptom with an endorsement prevalence of 56.4% [40]. The second most common endorsed symptom (41.4%) in these adolescents was also the continued use despite adverse consequences [40]. Notably, findings support an overall high endorsement rate of the unsuccessful attempts to cut down symptom across a variety of clinical and non-clinical populations, with- and without a FA diagnosis.
Challenges With Accurately Quantifying Attempts to Cut Down on UPFs
In situations when the YFAS is used, an accurate assessment of an individual’s persistent desire or attempts to cut down on UPFs can be obtained; however, there are a number of factors that may muddy the water when trying to quantify or understand the actual prevalence of these desires or attempts. One of these factors happens to be another FA symptom, withdrawal. According to the DSM-5 substance use disorder criteria [15], withdrawal is defined as the physical and/or psychological symptoms experienced as a result of the discontinuation of an addictive substance or the attempt to cut down on the amount consumed. Weight loss and obesity prevention programs often emphasize overall caloric restriction and/or reduction of UPFs [11, 34, 36]. Evidence for UPF withdrawal is preliminary at this point; however, recent study findings demonstrated that children and adults may experience withdrawal-like symptoms (e.g., affective, cognitive, and physical symptoms) when attempting to cut down on- or eliminating UPFs from their diets [11, 41]. In substance use disorders, withdrawal has been identified as a maintaining factor for current users, as well as a powerful predictor of relapse for those attempting to abstain or cut down [41]. We do not yet know whether this is similarly occurring with UPFs; future research is warranted to understand the interplay between withdrawal symptoms and unsuccessful attempts to cut down on UPFs. Should UPFs elicit withdrawal symptoms akin to drugs of abuse, then how might withdrawal or avoidance of- impact one’s persistence in attempting to cut down on UPFs and the ability to accurately quantify these attempts? A similar question may be posed in regard to attrition and quantifying cut down attempts.
Although weight management programs often have high attrition rates [42, 43], only recently have studies begun exploring the role FA may play in these conditions. Baseline psychosocial and demographic factors associated with treatment failure (study attrition and weight gain) were examined in a large-scale, randomized control weight-loss trial conducted in adults [44]. The strongest psychosocial predictor of treatment failure was FA [44]. Similar findings were observed in a recent investigation of FA behaviors in 9–11 year old children with overweight. In the study conducted by de Almeida et al. [45], FA in children with overweight at baseline of a 16-month, multi-component intervention was identified as the main factor correlated with treatment failure. In another study, adolescents identified as having FA upon entry into an outpatient, weight management program dropped out of the program at a significantly higher rate than those without FA [39]. It is unknown whether and/or how much program attrition may be due to the inability to cut down on UPFs and/or challenges arising from the restriction/reduction of UPFs.
Another impediment in obtaining an accurate depiction of attempts, successes, and failures to cut down on UPFs is that many weight control efforts are pursued on an individual basis. A systematic review and meta-analysis of personal weight loss attempts worldwide including 72 studies (n = 1,184,942) revealed that 42% of adults from general populations attempted to lose weight at some point in time [2•]. Increased/regular physical activity and diet restriction were the most prevalent, personal weight control strategies reported [2•]; however, it is unknown whether- and to what extent UPFs factored into these weight control efforts. Surveillance measures such as the NHANES may provide some insight with dietary intake data as food items collected during dietary recall interviews can be categorized according to the NOVA food classification system [46, 47]. Not all surveillance measures, however, nor research studies capture individuals’ weight control and dietary efforts in the same manner. This presents a barrier as it limits the ability to attribute individuals’ dietary efforts to UPFs [6•, 26••].
The YFAS scales are one method to identify problematic eating behaviors as well as capture attempts to cut down on UPFs, and may serve as a promising tool, that when utilized, may help decrease the rates of attrition, relapse, and weight cycling in through targeted weight loss strategies. Another promising tool is the ProWS [41]. The ProWS scale assesses a range of physical and psychological symptoms that people may experience when they restrict or limit consumption of UPFs. If individuals and/or parents of children attempting to cut down on UPFs are made aware to anticipate withdrawal symptoms, then perhaps we might see improved adherence in weight management programs and less attrition and relapse rates [48•].
While scales such as the YFAS may be helpful in identifying those with addictive-like eating behaviors and symptoms, they are subjective assessments and may present a challenge when attempting to quantify attempts to cut down on UPFs. Subjective experiences of cutting down on UPFs may be influenced by societal messaging that certain foods are “bad” and therefore cut down attempts may be self-reported at a higher rate. Moreover, there may be individual differences in how questions are interpreted based on eating pathology [49]. Although FA may seem counter-intuitive in anorexia nervosa, a restrictive eating disorder, prevalence of FA is surprisingly high in this population. Tran et al. [50] reported that almost half of individuals with a current anorexia nervosa diagnosis met the criteria for FA, with FA endorsed at a higher rate in those with a binge-purge subtype of anorexia compared to those with a restrictive subtype, 47% vs. 74%, respectively. Notably, endorsement rates of the unable to cut down symptom are high in this population as well, with 98% of participants with anorexia nervosa endorsing this symptom in a study by Granero et al. [51]. Parallel to substance use disorders, the YFAS and YFAS 2.0 were intended to measure addictive-like eating behaviors and FA in those who consume frequent, significant quantities of UPFs. Although an individual with a restrictive eating pathology may indicate that they were unsuccessful in cutting down on UPFs, this may represent a subjective, cognitive restraint rather an objectively larger, addictive-like consumption of UPFs. To distinguish between objective versus subjective experiences, a structured or semi-structured clinical interview, rather than self-report, may be warranted to quantify attempts to cut down on UPFs [49].
While one may postulate (likely correctly) that energy restriction/reduction strategies involve attempts to consume less UPFs, the lack of data on UPF consumption specifically, hampers the effort to quantify the scope UPFs may play in these attempts to cut down, successful or not. It is plausible that a proportion of unsuccessful diet attempts, attrition rates, relapses, and weight cycling occurrences may be attributable to unsuccessful attempts to cut down on UPFs; however, more research is needed to understand the potential associations and interactions.
Conclusions
In the context of weight control and diet adherence, willpower, characterized as the ability to exert self-control over our actions or restrain oneself from impulsive behaviors or urges, centers on individual responsibility [52]. This approach is not only ineffective, but also is contradictory to evidence presented earlier—individuals do indeed have the persistent desire to make changes to their diet and attempt to cut down on UPFs. Moreover, the individual, willpower-centric, behavior-based view of addictive-like eating ignores the scientific evidence regarding the biological disruptions and potential activation of addictive-like processes that can occur with the consumption of UPFs (and only UPFs). While there are behavioral aspects involved with the FA construct, the growing body of evidence lends credence to UPFs being uniquely implicated as the primary driver of addictive-like responses and thus, more accurately conceptualized as a substance-based disorder [26••, 53]. Additional research is warranted in order to quantify and discern the extent to which UPFs contribute to unsuccessful weight loss attempts.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gaesser GA, Angadi SS. Obesity treatment: weight loss versus increasing fitness and physical activity for reducing health risks. iScience. 2021;24(10):102995. https://doi.org/10.1016/j.isci.2021.102995.
• Santos I, Sniehotta FF, Marques MM, Carraca EV, Teixeira PJ. Prevalence of personal weight control attempts in adults: a systematic review and meta-analysis. Obes Rev. 2017;18(1):32–50. https://doi.org/10.1111/obr.12466. First systematic review to investigate weight control attempts worldwide. Meta-analysis was also conducted to identify correlates of weight loss attempts and weight control strategies employed.
Martin CB, Herrick KA, Sarafrazi N, Ogden CL. Attempts to lose weight among adults in the United States, 2013–2016. NCHS Data Brief. 2018;313:1–8.
Monteiro CA, Cannon G, Lawrence M, Costa Louzada Md, Pereira Machado P. Ultra-processed foods, diet quality, and health using the NOVA classification system. Rome: FAO. 2019;48.
Monteiro CA, Cannon G, Moubarac JC, Levy RB, Louzada MLC, Jaime PC. The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21(1):5–17. https://doi.org/10.1017/S1368980017000234.
• Crimarco A, Landry MJ, Gardner CD. Ultra-processed foods, weight gain, and co-morbidity risk. Curr Obes Rep. 2021. https://doi.org/10.1007/s13679-021-00460-y. Narrative review of UPF consumption and association with weight gain, co-morbidity risk, as well as the potential mechanisms underlying these associated risks.
Neri D, Martinez-Steele E, Khandpur N, Levy R. Associations between ultra-processed foods consumption and indicators of adiposity in US adolescents: cross-sectional analysis of the 2011–2016 National Health and Nutrition Examination Survey. J Acad Nutr Diet. 2022. https://doi.org/10.1016/j.jand.2022.01.005.
Nardocci M, Leclerc BS, Louzada ML, Monteiro CA, Batal M, Moubarac JC. Consumption of ultra-processed foods and obesity in Canada. Can J Public Health. 2019;110(1):4–14. https://doi.org/10.17269/s41997-018-0130-x.
Monteiro CA, Moubarac JC, Levy RB, Canella DS, Louzada M, Cannon G. Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr. 2018;21(1):18–26. https://doi.org/10.1017/S1368980017001379.
Martinez Steele E, Baraldi LG, Louzada ML, Moubarac JC, Mozaffarian D, Monteiro CA. Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study. BMJ Open. 2016;6(3):e009892. https://doi.org/10.1136/bmjopen-2015-009892.
Parnarouskis L, Schulte EM, Lumeng JC, Gearhardt AN. Development of the highly processed food withdrawal scale for children. Appetite. 2020;147:104553. https://doi.org/10.1016/j.appet.2019.104553.
Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale food addiction scale. Appetite. 2009;52(2):430–6. https://doi.org/10.1016/j.appet.2008.12.003.
American Psychiatric Association. American Psychiatric Association. Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000.
Gearhardt AN, Roberto CA, Seamans MJ, Corbin WR, Brownell KD. Preliminary validation of the Yale food addiction scale for children. Eat Behav. 2013;14(4):508–12. https://doi.org/10.1016/j.eatbeh.2013.07.002.
American Psychiatric Association. American Psychiatric Association. DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, D.C.: American Psychiatric Association; 2013.
Gearhardt AN, Corbin WR, Brownell KD. Development of the Yale food addiction scale version 2.0. Psychol Addict Behav. 2016;30(1):113–21. https://doi.org/10.1037/adb0000136.
Schiestl ET, Gearhardt AN. Preliminary validation of the Yale food addiction scale for children 2.0: a dimensional approach to scoring. Eur Eat Disord Rev. 2018;26(6):605–17. https://doi.org/10.1002/erv.2648.
Schulte EM, Avena NM, Gearhardt AN. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS One. 2015;10(2):e0117959. https://doi.org/10.1371/journal.pone.0117959.
Gibson AA, Sainsbury A. Strategies to improve adherence to dietary weight loss interventions in research and real-world settings. Behav Sci (Basel). 2017;7(3). https://doi.org/10.3390/bs7030044.
Bliss ES, Whiteside E. The gut-brain axis, the human gut microbiota and their integration in the development of obesity. Front Physiol. 2018;9:900. https://doi.org/10.3389/fphys.2018.00900.
Wang X, Zhu L, Li X, Wang X, Hao R, Li J. Effects of high fructose corn syrup on intestinal microbiota structure and obesity in mice. NPJ Sci Food. 2022;6(1):17. https://doi.org/10.1038/s41538-022-00133-7.
Zhao S, Jang C, Liu J, Uehara K, Gilbert M, Izzo L, et al. Dietary fructose feeds hepatic lipogenesis via microbiota-derived acetate. Nature. 2020;579(7800):586–91. https://doi.org/10.1038/s41586-020-2101-7.
Farooqi IS, Bullmore E, Keogh J, Gillard J, O’Rahilly S, Fletcher PC. Leptin regulates striatal regions and human eating behavior. Science. 2007;317(5843):1355. https://doi.org/10.1126/science.1144599.
Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68(8):808–16. https://doi.org/10.1001/archgenpsychiatry.2011.32.
Stice E, Spoor S, Bohon C, Veldhuizen MG, Small DM. Relation of reward from food intake and anticipated food intake to obesity: a functional magnetic resonance imaging study. J Abnorm Psychol. 2008;117(4):924–35. https://doi.org/10.1037/a0013600.
•• Gearhardt AN, Schulte EM. Is food addictive? A review of the science. Annu Rev Nutr. 2021;41:387–410. https://doi.org/10.1146/annurev-nutr-110420-111710. Presents a conceptual model of the evolutionary mismatch with the modern food environment, the parallels between food addiction and substance-based disorders, and the clinical and policy implications of UPF food addiction.
Myers MG, Cowley MA, Munzberg H. Mechanisms of leptin action and leptin resistance. Annu Rev Physiol. 2008;70:537–56. https://doi.org/10.1146/annurev.physiol.70.113006.100707.
Small DM, DiFeliceantonio AG. Processed foods and food reward. Science. 2019;363(6425):346–7. https://doi.org/10.1126/science.aav0556.
•• Schulte EM, Sonneville KR, Gearhardt AN. Subjective experiences of highly processed food consumption in individuals with food addiction. Psychol Addict Behav. 2019;33(2):144–53. https://doi.org/10.1037/adb0000441. Utilized behavioral methodology from substance abuse literature to evaluate abuse liability of foods, subjective experiences, and in-laboratory eating behaviors.
Schulte EM, Smeal JK, Gearhardt AN. Foods are differentially associated with subjective effect report questions of abuse liability. PLoS ONE. 2017;12(8):e0184220. https://doi.org/10.1371/journal.pone.0184220.
Cummings JR, Joyner MA, Gearhardt AN. Development and preliminary validation of the anticipated effects of food scale. Psychol Addict Behav. 2020;34(2):403–13. https://doi.org/10.1037/adb0000544.
DiFeliceantonio AG, Coppin G, Rigoux L, Edwin Thanarajah S, Dagher A, Tittgemeyer M, et al. Supra-additive effects of combining fat and carbohydrate on food reward. Cell Metab. 2018;28(1):33-44.e3. https://doi.org/10.1016/j.cmet.2018.05.018.
Neff KMH, Fay A, Saules KK. Foods and nutritional characteristics associated with addictive-like eating. Psychol Rep. 2021; 332941211014156. https://doi.org/10.1177/00332941211014156.
American College of Cardiology/American Heart Association Task Force on Practice Guidelines OEP. Expert panel report: guidelines (2013) for the management of overweight and obesity in adults. Obesity (Silver Spring). 2014;22(Suppl 2):S41-410. https://doi.org/10.1002/oby.20660.
Pursey KM, Stanwell P, Gearhardt AN, Collins CE, Burrows TL. The prevalence of food addiction as assessed by the Yale food addiction scale: a systematic review. Nutrients. 2014;6(10):4552–90. https://doi.org/10.3390/nu6104552.
Pursey KM, Collins CE, Stanwell P, Burrows TL. Foods and dietary profiles associated with ‘food addiction’ in young adults. Addict Behav Rep. 2015;2:41–8. https://doi.org/10.1016/j.abrep.2015.05.007.
Ouellette AS, Rodrigue C, Lemieux S, Tchernof A, Biertho L, Begin C. Establishing a food addiction diagnosis using the Yale food addiction scale: a closer look at the clinically significant distress/functional impairment criterion. Appetite. 2018;129:55–61. https://doi.org/10.1016/j.appet.2018.06.031.
Meule A, Hermann T, Kubler A. Food addiction in overweight and obese adolescents seeking weight-loss treatment. Eur Eat Disord Rev. 2015;23(3):193–8. https://doi.org/10.1002/erv.2355.
Tompkins CL, Laurent J, Brock DW. Food addiction: a barrier for effective weight management for obese adolescents. Child Obes. 2017;13(6):462–9. https://doi.org/10.1089/chi.2017.0003.
Schulte EM, Jacques-Tiura AJ, Gearhardt AN, Naar S. Food addiction prevalence and concurrent validity in African American adolescents with obesity. Psychol Addict Behav. 2018;32(2):187–96. https://doi.org/10.1037/adb0000325.
Schulte EM, Smeal JK, Lewis J, Gearhardt AN. Development of the highly processed food withdrawal scale. Appetite. 2018;131:148–54. https://doi.org/10.1016/j.appet.2018.09.013.
Moroshko I, Brennan L, O’Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obes Rev. 2011;12(11):912–34. https://doi.org/10.1111/j.1467-789X.2011.00915.x.
Skelton JA, Beech BM. Attrition in paediatric weight management: a review of the literature and new directions. Obes Rev. 2011;12(5):e273–81. https://doi.org/10.1111/j.1467-789X.2010.00803.x.
Fielding-Singh P, Patel ML, King AC, Gardner CD. Baseline psychosocial and demographic factors associated with study attrition and 12-month weight gain in the DIETFITS trial. Obesity (Silver Spring). 2019;27(12):1997–2004. https://doi.org/10.1002/oby.22650.
de Almeida VBP, Filgueiras AR, Nogueira PCK, Sesso R, Sawaya AL, Domene SMA. The impact of food addiction behaviours on the treatment of overweight students. Br J Nutr. 2021; 1–23. https://doi.org/10.1017/S0007114521004189.
Monteiro CA, Cannon G, Levy RB, Moubarac JC, Louzada ML, Rauber F, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019;22(5):936–41. https://doi.org/10.1017/S1368980018003762.
Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr. 2016;7(1):121–34. https://doi.org/10.3945/an.115.009258.
• Schiestl ET, Rios JM, Parnarouskis L, Cummings JR, Gearhardt AN. A narrative review of highly processed food addiction across the lifespan. Prog Neuropsychopharmacol Biol Psychiatry. 2021;106:110152. https://doi.org/10.1016/j.pnpbp.2020.110152. Examined exposure to highly processed foods across the lifespan, how these foods may be implicated in eliciting changes in reward functioning, and mechanisms contributing to the development of food addiction across the lifespan.
Schulte EM, Wadden TA, Allison KC. An evaluation of food addiction as a distinct psychiatric disorder. Int J Eat Disord. 2020;53(10):1610–22. https://doi.org/10.1002/eat.23350.
Tran H, Poinsot P, Guillaume S, Delaunay D, Bernetiere M, Begin C, et al. Food addiction as a proxy for anorexia nervosa severity: new data based on the Yale food addiction scale 20. Psychiatry Res. 2020;293:113472. https://doi.org/10.1016/j.psychres.2020.113472.
Granero R, Hilker I, Aguera Z, Jimenez-Murcia S, Sauchelli S, Islam MA, et al. Food addiction in a Spanish sample of eating disorders: DSM-5 diagnostic subtype differentiation and validation data. Eur Eat Disord Rev. 2014;22(6):389–96. https://doi.org/10.1002/erv.2311.
Lean MEJ, Astrup A, Roberts SB. Making progress on the global crisis of obesity and weight management. BMJ. 2018;361:k2538. https://doi.org/10.1136/bmj.k2538.
Schulte EM, Potenza MN, Gearhardt AN. A commentary on the “eating addiction” versus “food addiction” perspectives on addictive-like food consumption. Appetite. 2017;115:9–15. https://doi.org/10.1016/j.appet.2016.10.033.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Food Addiction
Rights and permissions
About this article
Cite this article
Laurent, J., Martin, A.R. & Tompkins, C.L. Persistent and Unsuccessful Attempts to Cut Down on Ultra-Processed Foods and the Associated Challenges for Dietary Adherence. Curr Addict Rep 9, 275–281 (2022). https://doi.org/10.1007/s40429-022-00418-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-022-00418-7