Abstract
Aim
To investigate the prevalence of molar–incisor hypomineralisation (MIH) amongst primary schoolchildren of Shiraz, Iran, taking into account the possible influence of biographic and socio-demographic parameters.
Study design and methods
A randomised cluster sample of 9- to 11-year-old children (N = 810) had their first permanent molars and incisors (index teeth) evaluated using the European Academy of Paediatric Dentistry criteria for MIH. The examinations were conducted at schools by a calibrated examiner. Prevalence of MIH was assessed based on biographic and socio-demographic parameters including area of residency, school type, father’s level of education, weight-for-age and height-for-age.
Results and statistics
Of the children examined, 164/810 (20.2 %) had MIH and 53.7 % of them presented with MIH lesions in all first molars. Mild defects represented by demarcated yellow brown opacities comprised 35.5 % of the total MIH lesions. The prevalence of MIH was significantly greater in girls, children with healthy body weight and height, those whose fathers did not have a tertiary education and from families of low socio-economic status. Regression analyses indicated that none of the biographic and socio-demographic variables represented a significant risk factor in the occurrence of MIH except for body weight. Obesity was negatively correlated to MIH (OR = 0.45; 95 % CI 0.25–0.82).
Conclusions
The prevalence of MIH in a group of Iranian children was 20.2 %. Biographic and socio-demographic parameters appeared to have no significant correlation with MIH except body weight, which warrants further research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-fluoride-associated developmental defects of tooth enamel are recognised as an increasing clinical problem (Crombie et al. 2008; Ghanim et al. 2011a). The term molar–incisor hypomineralisation (MIH) was coined to describe the clinical presence of developmental defects that can be seen as opacities, discolouration or as a mixture of change in appearance and loss of enamel substance (Weerheijm et al. 2003). The first permanent molars and permanent incisors have been reported as the most frequently affected teeth, however, any other tooth, primary or permanent, may be affected at the same time (Weerheijm et al. 2003). Recently, it has been reported that a hypomineralised second primary molar might be a clinically valuable predictor for MIH (Elfrink et al. 2012; Ghanim et al. 2013a). MIH lesions occur due to a pre-eruptive disturbance of enamel mineralisation during late gestation or early infancy (Arrow 2009; Ghanim et al. 2013b). The condition can influence the general health and quality of life of the affected child and its treatment is often challenging to both the patient and clinician (Jälevik and Klingberg 2012). Affected teeth often develop advanced carious lesions, and therefore have a great need for dental treatment (Leppäniemi et al. 2001; Ghanim et al. 2013c). This increased caries risk concomitant with hypomineralisation results in considerable dental morbidity often culminating in extraction with subsequent orthodontic consequences (Ong and Bleakley 2010). Recently, there has been increasing attention regarding the fact that MIH can be a sign of interruption in a child’s growth caused by early childhood illnesses (Alaluusua 2010; Fagrell et al. 2011).
Recent international studies in MIH reported a wide range of prevalence rates ranging from very low (2.8 %) to very high (40.2 %) prevalence values (Jälevik 2010). There is limited information about MIH prevalence in the Middle East Region, although existing studies provide useful background data. In Libya, researchers reported a very low prevalence for MIH (2.9 %) (Fteita et al. 2006), whereas in Jordan and Iraq, the reported prevalence was found to be higher (17.6 and 18.6 %, respectively) (Zawaideh et al. 2011; Ghanim et al. 2011b). A MIH prevalence of 12.7 % in Iranian children (Zahedan City) was reported recently (Ahmadi et al. 2012). Generally speaking, the use of variable examination protocols, sampling and recording methodologies have contributed largely to variation in the reported distributions that drives advocacy for the conduct of further studies with more standardised protocols and study design. On the other hand, this range in prevalence could be an actual difference secondary to socio-behavioural, environmental and genetic factors of the studied populations.
The aim of the present study was to determine the prevalence of MIH in 9- to 11-year-old children from Shiraz, Iran, taking into account the possible role of biographic and socio-demographic parameters in the occurrence of MIH.
Materials and methods
Study population
The city of Shiraz is situated in the south of Iran 200 km from the Persian Gulf, with approximately 1,500,000 inhabitants (ISC 1999). The city is divided by the city’s Education Head Office into 4 educational zones: Southwest (Zone 1), Northwest (Zone 2), Southeast (Zone 3), and Northeast (Zone 4). Although the divisions were primarily based on geographic location, zones 1 and 2 are generally considered as more affluent areas than zones 3 and 4. There is no institution water fluoridation in Shiraz; communal water is supplied from variety of sources with fluoride level ranges between 0.5 and 0.7 ppm (Golkari 2009). Early in 2012 there were about 18,500 students in grades 3–5 (ages 9–11 years) enrolled in 372 primary schools (private and public) in Shiraz. Schools are segregated by gender in Iran.
The list of all primary schools and permission to enter schools and conduct the study was obtained from Shiraz Education head office. Ethical approval was also obtained from the Ethics Committee of the Shiraz Dental School. A multi-stage random sampling was carried out by rolling a dice. Firstly, eight schools were randomly selected from each zone (random selection of 9 % of the total schools per zone equally divided as private and public; females and males). Secondly, within each selected school, one class of each target grade was selected randomly. Then half of children of each selected class were chosen randomly for the study.
A package containing an information brochure explaining the aims and a consent form asking guardians to consent to their children participating in the study was given to the selected children to pass on to their guardians. Information regarding father’s level of education was also asked in the consent form.
The following were the inclusion criteria: children aged 9–11 years, life-long residents in Shiraz City, having at least one first permanent molar erupted or partially erupted and presence at school on the day of examination. The exclusion criteria were: amelogenesis imperfecta, tetracycline staining, or subjects who were currently undergoing orthodontic treatment at the time of assessment; children in whom the crowns of the first permanent molars were completely broken down where the potential cause of breakdown was impossible to determine.
Clinical examination
Immediately before examination, each subject was given a soft toothbrush and fluoridated toothpaste. After brushing, the clinical examination was performed in the school dental hygiene room with the aid of an assistant to record the observations on a pre-tested dental chart provided for that purpose. The teeth were dried with sterile cotton rolls and examined with the aid of a head light using a disposable mirror head. Information regarding height-for-age and weight-for-age of the subjects was provided by the hygiene instructor of the relevant school. The obtained data were based on the regularly updated registers of heights to nearest centimetre and weights to nearest kilogram.
For the diagnosis of MIH, the judgement criteria established and modified by the EAPD (Weerheijm et al. 2003; Lygidakis et al. 2010) were used (Table 1). For the purpose of distinguishing MIH from diffuse opacities and enamel hypoplasia, the latter was diagnosed according to the Federation Dentaire International (FDI) (1992) definitions. The buccal/labial, occlusal/incisal, and lingual/palatal surfaces of the index teeth (permanent first molars and incisors) were examined and any visible developmental defects of enamel equal or greater than 1 mm in diameter were recorded (Lygidakis et al. 2010). The term molar hypomineralisation (MH) was used when referring to demarcated hypomineralisation defects affecting first molars only. The term incisor hypomineralisation (IH) was used to refer to demarcated hypomineralisation defects affecting incisors only, whereas the term MIH was used to refer to at least one affected first molar or a combination of affected first molars and incisors. Teeth that were erupted less than one-third of the crown height were recorded as unerupted.
All examinations were carried out by a single investigator (RB) who was calibrated to perform the dental examination using clinical photographs of subjects from a previous study (Ghanim et al. 2011b). Using kappa statistics, the inter- and intra-examiner agreements for MIH were reported as good to very good (0.75 and 0.80, respectively) (Landis and Koch 1977). Intra-examiner reproducibility was assessed by re-examining 10 % of the subjects; in total, 81 children were re-examined during the study and the intra-examiner reproducibility scoring was excellent (kappa = 0.92) (Landis and Koch 1977).
The severity of the hypomineralised defect was considered in terms of the clinical status and tooth surface area involved. A tooth diagnosed with colour changes only (i.e. creamy white or yellow/brown) was considered as mildly affected, moderate lesions had loss in enamel substance, whereas loss of enamel associated with affected dentine and/or atypical restoration was considered as severely affected. The extent of the defect in a tooth was measured by the surface area of the enamel affected as follows: ‘<1/3 of the tooth surface involved’; ‘at least 1/3 but <2/ 3’; and ‘at least 2/3 of a tooth surface involved’ (Federation Dentaire International (FDI) 1992).
Statistical methods
In order to determine variations from the non-MIH-affected population the sample was divided into: those diagnosed with MIH, referred to as ‘MIH-affected group’ (n = 164) and those who were ‘non-MIH-affected group’ (n = 646). Ranking of the population sample from highest to lowest socio-economic status used zone type in a descending order. Information obtained on father’s level of education was classified into three categories “primary school education”; “high school diploma”; and “tertiary education”. Raw data of the height-for-age and weight-for-age measurements of both girls and boys were converted into percentiles based on the percentile curves of the height-for-age and weight-for-age growth charts specifically designed for Iranian children (age 2–18 years) (Hosseini et al. 1998a, b). The data were tabulated as follows: (1) underweight/height; <3rd percentile, (2) healthy weight/height; 3rd percentile to <90th percentile, (3) overweight/height; 90th to <97th percentile, (4) obese/extreme height; ≥97th percentile. Binary logistic regression analysis was performed to determine differences between the study groups by socio-demographic and biographic variables. All explanatory variables were fitted into a single model except for the variables with missing values (represented by father’s level of education data) that were fitted into a separate model. Adjusted Odds Ratios (OR) with 95 % test-based confidence intervals (CI) were calculated. Results at an alpha level less than 0.05 were considered statistically significant. Data were entered into and analysed using SPSS version 18.0 (SPSS Inc, Chicago, IL, USA).
Results
Sample distribution and MIH prevalence
Usable responses were obtained from 810 of 1,056 parents/guardians indicating their permission to have their children undertake the dental examination (response rate 76.7 %). The sample was distributed equally by age group (270; 33.3 %, each) with slightly more girls than boys (450; 55.6 %), as well as more children from public than private schools (360; 44.4 %). The distribution of the study sample by the area of residency was identical in zone one to three (180; 22.2 %) and higher in zone four (270; 33.3 %). Regarding father’s level of education, 265 (32.7 %) of the total sample did not respond to the question. Over half (59 %) of the fathers had an intermediate level of education. No statistical difference in sample distribution was found in terms of socio-demographic and biographic variables. The vast majority (98.5 %) of the children had their 12 index teeth fully erupted.
The majority of the examined subjects were not affected by a developmental defect of enamel (DDE), with 309 (38.1 %) having at least one permanent index tooth with a DDE. Of these subjects, 55 had diffuse opacities (6.8 %), 88 hypoplasia (10.9 %), and 2 (0.2 %) combined lesions including demarcated opacities. Of the remaining 164 subjects, 68 (8.4 %) had MH and 96 (11.8 %) had MIH indicating an overall prevalence of MIH to be 20.2 %. The prevalence of IH was 1.1 %. The mean number of MIH-affected teeth per child was 3.26 ± 0.91.
Prevalence of MIH by socio-demographic and biographic variables
Differences between the study groups analysed by biographic and socio-demographic variables are presented in Table 2. MIH lesions were seen more often in girls (59 %) than boys (χ 2(1) = 4.7, p = 0.029). On comparing MIH prevalence by age groups the differences did not reach statistical significance. The prevalence was higher in children from public schools (57 %) than private schools and reported as highest in children from zone four (38 %) and lowest in children from zone two (19 %). There was no statistically significant association between MIH and school type, but the association was significant by the area of residency (χ 2(3) = 14.9, p = 0.002). Regarding father’s educational level, significantly more MIH cases were detected in the group of father’s with an intermediate level of education (χ 2(2) = 33.4, p = 0.001). MIH lesions were significantly more prevalent in healthy height and weight subjects (64 and 76 %, respectively) (χ 2(2) = 79.4, p = 0.000; χ 2(2) = 132.0, p = 0.001, respectively).
The association between weight-for-age and area of residency for both study groups was found to be low with borderline statistical significance (Spearman Rank Correlation 0.35, p = 0.056).
Logistic regression analyses were performed to compare study groups by socio-demographic and biographic variables (Table 2). The tests of the both models were not statistically significant indicating that none of the above variables could represent a significant risk for MIH occurrence. However, in the model that contains all of the variables, except those for the father’s level of education, after controlling for the other independent variables included in this model, children who displayed healthy weight-for-age were over two times more likely to have MIH lesions (OR = 2.18, 95 % CI 1.20–3.96). In contrast, obesity appeared to have a negative relationship with MIH (OR = 0.45, 95 % CI 0.25–0.82).
Distribution of MIH defect by type of tooth affected, its clinical presentation and severity
Of the total number of permanent index teeth examined (9,720), 778 teeth were affected by demarcated hypomineralisation lesions including 539 (69.3 %) first molars and 239 (30.7 %) incisors. The tooth type most frequently affected was the upper right molar and central incisor (18.1 and 8.2 %, respectively). No significant difference was revealed in the MIH prevalence by dental arch or jaw side.
Over half of the affected children presented with MIH lesions in the four first molars; comprising 53.7 % of the total cases (88/164). The risk of incisor involvement increased with the number of affected molars, where children with all four molars affected were over three times more likely to have four to seven permanent incisors affected than those with one molar affected (OR = 3.2, 95 % CI 1.21–1.96, p = 0.045).
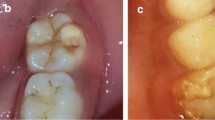
The severity of the defects varied from demarcated enamel opacities to severe structural loss and atypical restorations (Table 3). The mild defects were the most prevalent type of MIH, with the yellow/brown opacities being more frequent in molars than the creamy/white opacities which featured the incisor teeth. However, the number of molars affected with moderate to severe defects was almost equal to those with yellow/brown opacities only (41.3 %). No missing index teeth due to MIH were identified. The severity of MIH lesions increased significantly as age increased (χ 2(5) = 6.3, p = 0.035); however, this association was not significant in terms of gender.
Analysis of the relationship between MIH-clinical severity status and the tooth surface area affected by the hypomineralised defects was statistically significant (χ2(5) = 28.5; p = 0.000) (Fig. 1). Subjects who presented with severe defects had up to 70 % of the tooth surfaces involved compared to less than 15 % in cases with mild defects (creamy white demarcated opacities).
Discussion
Prevalence
Despite cultural and environmental differences, the present findings on MIH in Iran are comparable to those of international studies performed on the same age cohorts supporting the assumption that MIH is a global problem rather than regionally based problem (Kosem et al. 2004; da Costa-Silva et al. 2010; Mahoney and Morrison 2011; Martínez Gómez et al. 2012). The present study indicates that MIH is a widely spread condition amongst Iranian children. Considering common living rituals, the reported prevalence (20.2 %), although higher, it is still comparable to that observed in Jordan and Iraq, but is far greater than that reported for Libya. Notwithstanding similarities in examination protocols and recording methodologies, direct comparisons with the aforementioned Middle East studies should be interpreted with caution. Although the number of potentially affected teeth does not alter with age, the eruption status of the index teeth at the time of examination has not been included within the EAPD evaluation criteria despite it being a critical factor when comparing the prevalence rates from different studies. In the earlier Middle Eastern studies, whilst the optimal age recommended by the EAPD for the clinical examination was included (8 years) (Weerheijm et al. 2003), the problem of not identifying the potentially affected unerupted index teeth could not be addressed. In contrast, following the modified EAPD recommendation (Lygidakis et al. 2010), in the present study an attempt to achieve more complete results was made by examining older age groups where all of the index teeth were fully erupted in almost the entire sample at the time of examination. Tooth eruption status could partly explain the difference in the prevalence rates between the present study and the similar Middle Eastern studies. A specific eruption status scale is required to be added to the clinical index of MIH. However, actual differences between different countries should not be dismissed.
In the present study, girls reported higher defect prevalence than boys, with moderate to severe defects found more often in girls whilst boys were comparatively mildly affected and more likely to have opacities only, in agreement with earlier findings (Jasulaityte et al. 2007; Wogelius et al. 2008). However, generally there is consensus amongst authors that no gender differences exist in demarcated lesion prevalence (Leppäniemi et al. 2001; Fteita et al. 2006; Preusser et al. 2007). Apart from variations in sample size, differences in prevalence estimation by gender may be a result of disparities in chronological tooth development between genders. Differences in defect severity between genders may also be attributed to variation in oral care and behaviour.
Socio-demographic and biographic parameters, possible association
Despite the increasing trends in dental research towards exploring the link between oral health and systemic health, the study of MIH remains a daunting task for health care providers due to its unclear aetiological factors; therefore, looking at MIH from different aspects facilitates the identification of aetiological agents which, in turn, might allow the development of preventive strategies (Alaluusua 2010). In the present study, odds ratios were calculated for all of the socio-demographic and biographic variables with no statistically significant association to the outcome variable except for the body weight that may just be random findings. No previous data on this aspect of predilection are available for comparison. Hence, a prospective cohort study including growth, physical development and health factors from early childhood is required with special attention to nutritional deficiencies as precipitating factors.
In the present study, socio-economic status was represented by area of residency; therefore, children from all socio-economic strata were examined. Father’s educational level and school type were used as additional measures of socio-economic grading. Significantly more MIH cases were diagnosed in lower socio-economic areas and associated with an intermediate level of father’s education. In contrast to the present findings, in a recent UK study, higher prevalence levels of MIH were found in children from high socio-economic levels than from deprived areas (Balmer et al. 2012). However, in the present study, regression analysis has not identified any significant risk of the socio-economic status on MIH occurrence. If the prevalence of MIH is actually influenced by individual socio-economic disparities, then factors such as early childhood diet, access to health care and an infant’s household environment could all be involved in the pathogenesis of the defect. Nonetheless, as little is known about the association of socio-economic status with MIH, this is an area for further research.
Clinical characteristics
The present finding that over half of the affected children had, on average, nearly four first molars affected by MIH confirmed the finding of others (Wogelius et al. 2008; Lygidakis et al. 2008; Soviero et al. 2009). It demonstrated the potential impact of MIH on the oral health of children. In addition to the well-known complications of sensitivity, and tooth structure loss, MIH is increasingly recognised as a significant risk factor for increased severity of caries (Mahoney and Morrison 2009; Ghanim et al. 2013c).
Although no significant difference was determined in the distribution of the demarcated defect between the maxilla and the mandible, hypomineralised defects were more prevalent and severe in the maxilla than the mandible in accordance with previous studies (Leppäniemi et al. 2001; Arrow 2008).
In the present study, creamy white opacities were the most prevalent type of MIH lesions, in agreement with previous findings (Suckling et al. 1985; Wogelius et al. 2008). Nonetheless, yellow/brown opacities represent over 35 % of the total defect type. Clearly, teeth diagnosed with the moderate and severe lesions required more treatment than those in the mild categories. It should be remembered that defect progression in teeth diagnosed with opacities is likely to become more severe after a period of oral function (da Costa-Silva et al. 2011).
To appreciate the results some limitations need to be discussed. The present findings were drawn from samples of older children when the true prevalence could have been obscured by restorative treatments or high levels of dental caries. However, in a recent study amongst 6- to 12-year-old Iranian subjects the mean caries index corresponded to the age groups approached in the present study was found to be lower than the global standards (1.18 ± 0.97) (Motlagh et al. 2007).
Conclusions
MIH has a prevalence rate of 20.2 % in this Iranian cohort. Mild lesions comprised the majority of cases with yellow/brown opacities representing over 35 % of the total MIH defects. The severity of defects increased with age, directly correlated to the number of teeth affected as well as to the surface area affected. The prevalence of MIH was significantly greater in girls, children with healthy body weight and height, whose fathers did not have a tertiary education and from families of low socio-economic status. Logistic regression models indicated unexpectedly that normal body weight might represent a significant associated factor for MIH, which requires further research.
References
Ahmadi R, Ramazani N, Nourinasab R. Molar incisor hypomineralization: a study of prevalence and etiology in a group of Iranian children. Iran J Pediatr. 2012;22:245–51.
Alaluusua S. Aetiology of molar–incisor hypomineralisation: a systematic review. Eur Arch Paediatr Dent. 2010;11:53–8.
Arrow P. Prevalence of developmental enamel defects of the first permanent molars among school children in Western Australia. Aust Dent J. 2008;53:250–9.
Arrow P. Risk factors in the occurrence of enamel defects of the first permanent molars among schoolchildren in Western Australia. Community Dent Oral Epidemiol. 2009;37:405–15.
Balmer R, Toumba J, Godson J, Duggal M. The prevalence of molar incisor hypomineralisation in Northern England and its relationship to socioeconomic status and water fluoridation. Int J Paediatr Dent. 2012;22:250–7.
Crombie F, Manton DJ, Kilpatrick N. Molar incisor hypomineralization: a survey of members of the Australian and New Zealand Society of Paediatric Dentistry. Aust Dent J. 2008;53:160–6.
da Costa-Silva CM, Ambrosano GM, Jeremias F, De Souza JF, Mialhe FL. Increase in severity of molar–incisor hypomineralization and its relationship with the colour of enamel opacity: a prospective cohort study. Int J Paediatr Dent. 2011;21:333–41.
da Costa-Silva CM, Jeremias F, de Souza JF et al. Molar incisor hypomineralization: prevalence, severity and clinical consequences in Brazilian children. Int J Paediatr Dent. 2010;20:426–34.
Elfrink ME, Ten Cate JM, Jaddoe VW, Hofman A, Moll HA, Veerkamp JS. Deciduous molar hypomineralization and molar incisor hypomineralization. J Dent Res. 2012;91:551–5.
Fagrell TG, Ludvigsson J, Ullbro C, Lundin SA, Koch G. Aetiology of severe demarcated enamel opacities—an evaluation based on prospective medical and social data from 17,000 children. Swed Dent J. 2011;35:57–67.
Federation Dentaire International (FDI). Commission on Oral Health, Research and Epidemiology. A review of the development defects of enamel index (DDE Index). Int Dent J. 1992;42:411–26.
Fteita D, Ali A, Alaluusua S. Molar–incisor hypomineralization (MIH) in a group of school-aged children in Benghazi, Libya. Eur Arch Paediatr Dent. 2006;7:92–5.
Ghanim A, Morgan M, Mariño R, Manton D, Bailey D. Perception of molar–incisor hypomineralisation (MIH) by Iraqi Dental Academics. Int J Paediatr Dent. 2011a;21:261–70.
Ghanim A, Morgan M, Mariño R, Bailey D, Mariño R. Molar–incisor hypomineralisation: prevalence and defect characteristics in Iraqi children. Int J Paediatr Dent. 2011b;21:413–21.
Ghanim A, Manton D, Mariño R, Morgan M, Bailey D. Prevalence of demarcated hypomineralisation defects in second primary molars in Iraqi Children. Int J Paediatr Dent. 2013a;23:48–55.
Ghanim A, Manton D, Bailey D, Mariño R, Morgan M. Risk factors in the occurrence of molar–incisor hypomineralization among a group of Iraqi children. Int J Paediatr Dent. 2013b;23:197–206.
Ghanim A, Morgan M, Mariño R, Bailey D, Manton D. An in vivo investigation of salivary properties, enamel hypomineralisation and carious lesion severity in a group of Iraqi schoolchildren. Int J Paediatr Dent. 2013c;23:2–12.
Golkari A. Developmental defects of enamel as biomarkers of early childhood life events: Developing methods for their use in life course epidemiology. Thesis Submitted for PhD Degree, University College London, 2009
Hosseini M, Carpenter RG, Mohammad K. Growth charts for Iran. Ann Hum Biol. 1998a;25:237–47.
Hosseini M, Carpenter RG, Mohammad K. Growth charts for Iran. Ann Hum Biol. 1998b;25:249–61.
ISC. Iran Statistical Yearbook of the Year 1377. Tehran: Statistical Centre of Iran; 1999.
Jälevik B, Klingberg G. Treatment outcomes and dental anxiety in 18-year-olds with MIH, comparisons with healthy controls-a longitudinal study. Int J Paediatr Dent. 2012;22:85–91.
Jälevik B. Prevalence and diagnosis of molar–incisor-hypomineralisation (MIH): a systematic review. Eur Arch Paediatr Dent. 2010;11:59–64.
Jasulaityte L, Veerkamp KL, Weerheijm KL. Molar incisor hypomineralization: review and prevalence data from a study of primary school children in Kaunas (Lithuania). Eur Arch Paediatr Dent. 2007;8:87–94.
Kosem R, Senk-Erpic A, Kosir N, Kastelec D. Prevalence of enamel defects with emphasis on MIH in Slovenian children and adolescents. Eur J Paediatr Dent. 2004;3(Suppl):17.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Leppäniemi A, Lukinmaa PL, Alaluusua S. Non-fluoride hypomineralizations in the first molars and their impact on the treatment need. Caries Res. 2001;35:36–40.
Lygidakis NA, Dimou G, Briseniou E. Molar–incisor-hypomineralisation (MIH). Retrospective clinical study in Greek children. I. Prevalence and defect characteristics. Eur Arch Paediatr Dent. 2008;9:200–6.
Lygidakis NA, Wong F, Jälevik B et al. Best clinical practice guidance for clinicians dealing with children presenting with molar–incisor-hypomineralisation (MIH): an EAPD Policy Document. Eur Arch Paediatr Dent. 2010;11:75–81.
Mahoney EK, Morrison DG. The prevalence of molar–incisor hypomineralisation (MIH) in Wainuiomata children. N Z Dent J. 2009;105:121–7.
Mahoney EK, Morrison DG. Further examination of the prevalence of MIH in the Wellington region. N Z Dent J. 2011;107:79–84.
Martínez Gómez TP, Guinot Jimeno F, Bellet Dalmau LJ, Giner Tarrida L. Prevalence of molar–incisor hypomineralisation observed using transillumination in a group of children from Barcelona (Spain). Int J Paediatr Dent. 2012;22:100–9.
Motlagh MG, Khaniki GRJ, Adiban H. Investigation of dental caries prevalence among 6–12 year old elementary school children in Andimeshk, Iran. J Med Sci. 2007;7:116–20.
Ong DC, Bleakley JE. Compromised first permanent molars: an orthodontic perspective. Aust Dent J. 2010;55:2–14.
Preusser SE, Ferring V, Wleklinski WE. Prevalence and severity of molar incisor hypomineralization in a region of Germany—a brief communication. J Public Health Dent. 2007;67:148–50.
Soviero V, Haubek D, Trindade C, Matta TD, Poulsen S. Prevalence and distribution of demarcated opacities and their sequelae in permanent 1st molars and incisors in 7 to 13-year-old Brazilian children. Acta Odontol Scand. 2009;67:170–5.
Suckling GW, Brown RH, Herbison GP. The prevalence of developmental defects of enamel in 696 nine-year-old New Zealand children participating in a health and development study. Community Dent Health. 1985;2:303–13.
Weerheijm K, Duggal M, Mejàre I et al. Judgement criteria for molar–incisor hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent. 2003;4:110–3.
Wogelius P, Haubek D, Poulsen S. Prevalence and distribution of demarcated opacities in permanent 1st molars and incisors in 6 to 8-years-old Danish children. Acta Odontol Scand. 2008;66:58–64.
Zawaideh FI, Al-Jundi SH, Al-Jaljoli MH. Molar incisor hypomineralisation: prevalence in Jordanian children and clinical characteristics. Eur Arch Paediatr Dent. 2011;12:31–6.
Acknowledgments
This research was partly supported by Shiraz University of Medical Sciences. The authors thank all students who participated in this study and also appreciate the Schools’ staffs for their assistant to facilitate collecting the data. We also acknowledge Dr M.R. Azar (The Head of Shiraz Dental School) for his support in carrying out this study. Special thanks to Dr D. Bailey, Dr H. Haydari, Mr F. Banizaman Lari (Lecturer in Farhangian University) and Mrs R. Keshavarzi for their valuable assistance throughout the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghanim, A., Bagheri, R., Golkari, A. et al. Molar–incisor hypomineralisation: a prevalence study amongst primary schoolchildren of Shiraz, Iran. Eur Arch Paediatr Dent 15, 75–82 (2014). https://doi.org/10.1007/s40368-013-0067-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-013-0067-y