Abstract
Background
The study and application of exercise in multiple sclerosis (MS) often requires cardiopulmonary exercise testing (CPET) to provide a comprehensive assessment of exercise tolerance and responses, including an evaluation of the pulmonary, cardiovascular, and skeletal muscle systems. Research on CPET in persons with MS has considerable limitations, including small sample sizes, often without controls; not reporting outcomes across disability status; and different modalities of exercise testing across studies. Although some key outcome variables of CPET have been studied in persons with MS, additional calculated variables have not been directly studied.
Objective
The objective of this study was to provide a comprehensive examination of outcome variables from CPET among persons with MS and healthy controls.
Methods
We included data from 162 persons with MS and 80 healthy controls who underwent CPET on a leg ergometer and satisfied criteria for valid testing for measuring oxygen uptake (VO2), carbon dioxide production (VCO2), ventilation (VE), respiratory exchange ratio, work rate, and heart rate (HR). Calculated variables [i.e. ventilatory anaerobic threshold (VO2/VCO2), VE/VCO2 slope, VO2/power slope, VO2/HR slope, and oxygen uptake efficiency slope] were processed using standard guidelines. We examined differences in the CPET variables between groups (e.g. MS vs. controls and categories of mild, moderate, and severe disability status) using analysis of covariance (ANCOVA), controlling for age, sex, body mass index, and disease duration.
Results
Overall, persons with MS demonstrate alterations in outcomes from CPET compared with controls, and these are generally exacerbated with increasing disability.
Conclusion
Our results provide novel information for the evaluation of CPET in MS for developing exercise prescriptions and documenting adaptations with exercise training based on the comprehensive variables obtained during CPET.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Persons with multiple sclerosis (MS) demonstrate alterations in outcomes of cardiopulmonary exercise testing (CPET) compared with healthy controls. |
In persons with MS, outcomes of CPET are generally exacerbated with increasing disability. |
The evaluation of CPET outcomes is important for developing exercise prescriptions and evaluating adaptations with exercise training in MS. |
1 Introduction
Multiple sclerosis (MS) is a chronic neurologic disease with a prevalence in the US of 1 per 1000 persons [1]. This neurologic disease involves inflammation, axonal demyelination and transection, as well as neurodegeneration within the central nervous system (CNS). Such CNS damage results in neurological disability, functional impairments, and symptoms such as leg spasticity, muscle weakness, walking and balance dysfunction, and fatigue, pain, and depression [2]. Exercise can be an important tool for safely managing the consequences of MS [3, 4].
The study and application of aerobic exercise in MS requires cardiopulmonary exercise testing (CPET). CPET involves symptom-limited, maximal incremental exercise, often coupled with indirect spirometry for analyzing expired gases (e.g. O2 and CO2). This provides a comprehensive assessment of exercise tolerance and responses, including an evaluation of the pulmonary, cardiovascular, and skeletal muscle systems [5]. CPET outcomes include measures of oxygen uptake (VO2), carbon dioxide production (VCO2), and ventilation (VE) [6]. This paradigm further allows for accurate quantification of cardiorespiratory fitness and is necessary for developing an exercise prescription and documenting adaptations to chronic exercise training. CPET further provides critical information regarding the physiological systems that underlie these exercise responses [7].
CPET typically has been applied for examining cardiorespiratory fitness in persons with MS. For example, peak aerobic capacity (VO2peak) is a commonly reported outcome of CPET in MS [8], and previous studies indicate that persons with MS have a lower exercise tolerance than controls, based on significant differences in VO2peak [9]; however, one limitation of using VO2peak as the ‘gold standard’ CPET measure in persons with MS is that it is dependent on maximal effort of the participant. An alternative measure that overcomes this limitation involves the oxygen uptake efficiency slope (OUES). Although the OUES is not universally accepted, researchers have examined the OUES as an alternative marker of exercise tolerance based on the curvilinear relation between VE and VO2peak [10], and reported high concurrent validity of the OUES based on correlations with peak work rate (WRpeak) and VO2peak. Research on CPET in persons with MS has considerable limitations, including small sample sizes, often without appropriate controls [10, 11], and not reporting outcomes across disability status [12]. CPET further involves different modalities of exercise testing across studies (i.e. arm vs. leg ergometry) [11, 13]. Additionally, outcome variables of CPET (e.g. VE/VCO2 slope) identified in other populations (e.g. pulmonary hypertension) [6, 7] have not been directly studied in persons with MS across the disability spectrum [9]. This collectively underscores the need for a systematic, comprehensive focus on the evaluation of CPET in MS for better developing exercise prescriptions and documenting adaptations with chronic training.
Data derived from CPET in persons with MS are clinically relevant. It is well-established that VO2peak is an excellent prognostic indicator in a variety of patient populations [14]. Submaximal variables such as VE/VCO2 slope and OUES have been used to successfully predict clinical prognosis and risk for cardiovascular diseases in several clinical populations [15–17]. Thus, the clinical utility of CPET is well-established, although specific data on prognosis in MS are lacking. Given the prevalence of comorbidities such as cardiovascular disease in persons with MS [18], CPET could provide useful clinical information regarding what physiological system limits work capacity. For example, the VE/VCO2 slope provides information on ventilator efficiency and limitations [5]; the VO2/Power slope represents the adequacy of oxygen transport to working muscles [14]; and the HRpeak and VO2/HR slope provides information on cardiac function [14]. Consequently, CPET is a very useful tool to identify prognostic implications and limitations in the ability to do physical work, and provides a basis for exercise prescription in persons with MS.
To that end, the present study involved a comprehensive examination of outcome variables from CPET (Table 1) among persons with mild, moderate, and severe MS disability, and age-matched controls. Such an examination is advantageous given the breadth and completeness of the variables reported from CPET; inclusion of a large sample of MS and matched controls; comparison across three levels of disability; and adoption of a standardized protocol and modality for conducting CPET. We further provide examples of plots for interpreting CPET outcomes based on Wasserman et al. [14] for illustrations of clinical value in MS (see “Appendix”).
2 Methods
2.1 Participants
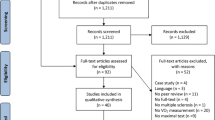
Prospective participants with MS were recruited using multiple sources, including print and e-mail flyers, an online advertisement on the National Multiple Sclerosis Society website, and our database of previous participants with MS. Healthy controls were recruited via public e-mail postings. The inclusion criteria for persons with MS were (1) definite physician diagnosis of MS based on revised McDonald criteria [19]; (2) relapse-free in the previous 30 days; (3) ambulatory with or without assistive devices; (4) aged between 18 and 64 years; (5) willingness and physical ability to undergo maximal CPET; and (6) low risk of contraindications for CPET based on the Physical Activity Readiness Questionnaire [20]. The same inclusion criteria were applied for the healthy controls, with the exception of diagnosis of MS and relapse-free over the past 30 days. Healthy control participants further matched the sample of persons with MS based on age. This study sought a sample of convenience and therefore no power analysis was conducted. Overall, 201 persons with MS and 82 healthy controls satisfied the inclusion criteria and underwent testing. The final sample included 162 persons with MS and 80 healthy controls based on valid CPET data.
2.2 Cardiopulmonary Exercise Test
All participants completed CPET on an electronically-braked, computer-controlled cycle ergometer (Lode BV, Groningen, The Netherlands) and an open-circuit spirometry system (TrueOne, Parvo Medics, Sandy, UT, USA) for analyzing expired gases. The O2 and CO2 analyzers of the spirometry system were calibrated using verified concentrations of gases, and the flow meter was calibrated using a 3 L syringe (Hans Rudolph, Kansas City, MO, USA). Participants were initially fitted to the cycle ergometer and were read standardized instructions for completing CPET, along with instructions for providing ratings of perceived exertion (RPEs). They were then outfitted with a mouthpiece (Hans Rudolph, Kansas City, MO, USA) for collecting expired gases. Participants rested on the cycle ergometer for 1 min and then performed a 4-min warm-up at 0 W. Work rate (WR) continuously increased at a rate of 15 W/min, and participants maintained a cadence of 60 rpm until reaching volitional fatigue or being unable to maintain the 60 rpm cadence. The WR was the same across all disability groups as researchers had no prior knowledge of individual fitness levels, which was necessary for estimation of some CPET outcomes (e.g. VO2/Power slope). Participants were given verbal encouragement over the duration of the test. This test protocol has been validated in persons with MS [21] and has been consistently included in samples of MS and controls [22, 23]. VO2, VCO2, VE, and respiratory exchange ratio (RER) were measured continuously by the open-circuit spirometry system, and heart rate (HR) was continuously measured using a Polar heart rate monitor (Polar Electro Oy, Kempele, Finland); these values are expressed as 20-s averages. VO2peak (L/min; mL/kg/min), VEpeak (L/min), and RERpeak [VCO2 (L/min)/VO2 (L/min)] were defined as the highest recorded 20-s average during the final minutes of the test. WRpeak (W) and HRpeak (bpm) were recorded as peak power output and HR, respectively, during the incremental protocol. RPE was recorded every minute during the test and RPEpeak was recorded as the highest value. The CPET was considered valid if two of the four criteria were satisfied: (1) plateau of VO2 despite a continued increase in WR (i.e. ≤50 ml difference of VO2 per minute between the 30-s average before the last power increment and that after the last power increment) [12, 24]; (2) RERpeak ≥1.10; (3) HRpeak ≥90 % of age-predicted maximum (220-age); and (4) RPEpeak ≥17. Only persons with MS and controls who satisfied two of the four criteria were included in the final sample and data analyses.
2.3 Disability Status
The Patient-Determined Disease Steps (PDDS) scale was included as a self-report measure of MS disability status. This scale was developed as an inexpensive surrogate for the Expanded Disability Status Scale (EDSS) [25] and contains a single-item ordinal scale for measuring self-reported neurological impairment, ranging from 0 (normal) through 8 (bedridden). PDDS scores have been validated in MS [25, 26], and scores of 0–2, 3, and 4–6 have been adopted for classifying participants into categories of mild, moderate, and severe MS disability, respectively [27].
2.4 Procedures
The procedures were approved by a university Institutional Review Board, and all participants provided written informed consent before data collection. The procedures were further performed in accordance with the ethical standards of the Helsinki Declaration of 1975, as revised in 2013. Participants provided demographic and clinical information, followed by CPET.
2.5 Cardiopulmonary Exercise Testing (CPET) Variables
Descriptions of the main outcome variables are provided in Table 1. CPET data (VO2, VCO2, VE, RER, WR, and HR; 20-s averages) were exported from the open-circuit spirometry system into Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). Calculated variables [ventilatory anaerobic threshold (VAT; VO2/VCO2), VE/VCO2 slope, VO2/power slope, VO2/HR slope, and OUES] were processed using standard guidelines [6, 28, 29], and two persons (BMS and REK) processed the files together for quality control and consistency in quantifying the main outcome variables. The “Appendix” includes eight-panel graphical displays of the cardiovascular, ventilatory, ventilation-perfusion matching, and metabolic responses during exercise based on Wasserman et al. [14]. We provide the graphic displays of an example case study per group of disability status [mild (a), moderate (b), and severe disability (c)].
2.6 Data Analysis
All analyses were performed using SPSS version 21 (IBM Corporation, Armonk, NY, USA). Differences in age, height, weight, and body mass index (BMI) between the MS and control groups were examined using an independent sample t test, and differences in sex were examined using a Chi-square difference test. Descriptive statistics are presented in the text and tables as mean [standard deviation (SD)] and mean difference (MD) [±standard error (SE)] unless otherwise noted. The primary analytical model involved a between-subjects analysis of covariance (ANCOVA) on the main CPET variables, controlling for age (years), sex (0 = female, 1 = male), and BMI (kg/m2). This proceeded in two separate analyses. We first examined differences in CPET variables between persons with MS and matched controls, and then examined differences in CPET variables among persons with MS based on categories of mild, moderate, and severe disability status [27], controlling for disease duration (years) in addition to age, sex, and BMI. This analysis further involved post hoc Bonferroni corrections for examining specific differences in CPET variables between disability status groupings. Statistical significance was determined as p < 0.05. We expressed the overall effect sizes from the ANCOVAs as partial eta squared (\( \eta_{\text{p}}^{2} \)), and values of 0.01, 0.06, and 0.14 represented small, moderate, and large effects, respectively [30].
3 Results
3.1 Demographic and Clinical Characteristics of the Samples
The demographic characteristics of persons with MS and controls are provided in Table 2. These two groups did not significantly differ in age or height, but did differ in weight, BMI, and sex. The table further contains the clinical characteristics of persons with MS. The majority of cases represented relapsing-remitting MS (RRMS; 96.4 %), and average disease duration was 9.2 (7.1) years. The median (range) PDDS score was 2.0 (0.0–6.0), indicating relatively mild disability (i.e. no restrictions in walking but significant limitations in daily activities). Using the PDDS boundary values for mild, moderate, and severe MS disability [20], 82 persons had mild MS disability (PDDS 0–2), 31 had moderate MS disability (PDDS 3), and 26 had severe disability (PDDS 4–6); 23 cases had missing PDDS data.
3.2 Main CPET Variables in Persons with Multiple Sclerosis (MS) versus Controls
The percentages of persons with MS and controls who achieved the four different criteria for a valid CPET [(1) plateau of VO2 despite a continued increase in WR; (2) RERpeak ≥1.10; (3) HRpeak ≥90 % of age-predicted maximum (220-age); (4) RPE ≥17] and the duration of the CPET, or time to exhaustion (TTE) are presented in Table 3. The main outcome variables from CPET of persons with MS and controls, controlling for covariates of age, BMI, and sex, are provided in Table 3. The MD ±SE is presented as the mean of controls – mean of persons with MS. The ANCOVA identified a small but statistically significant difference in VO2/power slope (MD 0.5, SE ±0.2) and VO2/HR slope (MD 1.4, SE ±1.0) between persons with MS and controls, such that persons with MS demonstrated a flatter slope compared with controls. The ANCOVA identified a statistically significant and moderate-sized difference in OUES between persons with MS and controls (MD 271.6, SE ±89.5), such that persons with MS demonstrated a flatter slope compared with controls. The ANCOVA identified a statistically significant and large-sized difference in absolute VAT (MD 3.0, SE ±0.6), such that persons with MS reached anaerobic threshold at a lower VO2 value (mL/kg/min) than controls. The ANCOVA further identified statistically significant and large-sized differences in VO2peak independent of body weight (MD 0.5, SE ±0.1), VO2peak relative to body weight (MD 6.1, SE ±1.1), RERpeak (MD 0.1, SE ±0.01), VEpeak (MD 18.6, SE ±3.2), HRpeak (MD 15.0, SE ±2.2), and WRpeak (MD 39.2, SE ±6.2), such that persons with MS demonstrated lower peak values compared with controls. No significant difference was noted in VE/VCO2 slope (MD 0.2, SE ±1.0) or relative VAT (%VO2peak; MD −1.1, SE ±1.5) between persons with MS and controls.
3.3 Main CPET Variables in Persons with MS per Disability Status
The percentages of persons with MS per disability status who achieved the four different criteria for a valid CPET [(1) plateau of VO2 despite a continued increase in WR; (2) RERpeak ≥1.10; (3) HRpeak ≥90 % of age-predicted maximum (220-age); (4) RPE ≥17], and the duration of the CPET based on TTE, are presented in Table 4. The main outcome variables in persons with MS per disability status, controlling for age, BMI, sex, and disease duration are further provided in Table 4. MDs ± SEs are presented as the mean of mild—moderate; mean of mild—severe; and mean of moderate—severe. The ANCOVA identified statistically significant and large-sized differences in VO2peak independent of body weight (MD 0.2, SE ±0.1; MD 0.4, SE ±0.1; MD 0.2, SE ±0.1) and RERpeak (MD 0.1, SE ±0.02; MD 0.1, SE ±0.02; MD 0.1, SE ±0.03). Post hoc analysis indicated that persons with severe disability demonstrated lower VO2peak independent of body weight and RERpeak compared with persons with mild disability. The ANCOVA identified statistically significant and large-sized differences in VO2peak relative to body weight (MD 2.5, SE ±1.2; MD 7.7, SE ±1.0; MD 5.2, SE ±1.1) and WRpeak (MD 16.1, SE ±6.3; MD 41.9, SE ±7.2; MD 25.8, SE ±7.8). Post hoc analysis indicated that persons with severe disability demonstrated lower VO2peak relative to body weight and WRpeak compared with persons with moderate and mild disability, and persons with moderate disability demonstrated lower VO2peak relative to body weight and WRpeak compared with persons with mild disability. The ANCOVA identified statistically significant and large-sized differences in VEpeak (MD 10.2, SE ±3.9; MD 21.5, SE ±3.2; MD 10.9, SE ±3.9) and HRpeak (MD 2.1, SE ±3.2; MD 20.4, SE ±5.2; MD 18.3, SE ±5.4). Post hoc analysis indicated persons with severe and moderate disability demonstrated lower VEpeak compared with persons with mild disability, and persons with severe disability demonstrated lower HRpeak compared with persons with mild and moderate disability. No significant differences were observed in VO2/power slope (MD −0.4, SE ±0.3; MD 1.0, SD ±0.6; MD 1.4, SE ±0.6), OUES (MD 17.9, SE ±87.9; MD 299.2, SE ±132.6; MD 281.3, SE ±137.9), VE/VCO2 slope (MD 2.3, SE ±1.2; MD 0.0, SE ±1.9; MD −2.3; SE ±1.9), VO2/HR slope (MD 0.7, SE ±1.0; MD −0.2, SE ±1.4; MD −0.9, SE ±1.5), absolute VO2/VCO2 VAT (MD 0.6, SE ±1.0; MD 4.0, SE ±1.0; MD 3.4, SE ±1.0) and relative (%VO2peak) VAT (MD −4.6, SE ±2.2; MD −4.7, SE ±2.2; MD −0.1, SE ±2.5) among the groups.
4 Discussion
The overall results of the current study indicate that persons with MS differ in the majority of CPET outcome variables compared with matched controls, and further differences are observed in those variables among persons with mild, moderate, and severe MS disability. We discuss these differences and the indications for possible clinical indications, as well as importance for exercise training and prescription.
4.1 Peak Aerobic Capacity (VO2peak)
VO2peak independent of body weight (L/min) and VO2peak relative to body weight (mL/kg/min) were significantly lower in persons with MS compared with controls. The average values are lower than that of a previous meta-analysis [9] but are similar in that they reflect lower exercise tolerance in persons with MS compared with controls [6]. This reduced exercise tolerance may be associated with lower daily physical activity levels [31] or a lower HRpeak in persons with MS as VO2peak is closely associated with HRpeak [32]. VO2peak was significantly different in the subsamples of persons with MS, such that persons with severe disability demonstrated lower VO2peak independent of body weight compared with persons with mild disability, as illustrated in panel 1 of the “Appendix”. Persons with severe disability further demonstrated lower VO2peak relative to body weight compared with persons who had moderate and mild disability, and persons with moderate disability demonstrated lower VO2peak relative to body weight compared with persons who had mild disability. This pattern of results is consistent with previous research [8, 10] and seemingly reflects reduced exercise tolerance as a function of increasing disability levels. Figure 1 illustrates the negative association between PDDS scores and VO2peak relative to body weight (F = 39.2, p < 0.05). The association between VO2peak and PDDS indicates that a 1-point increase in PDDS yielded a 1.9 mL/kg/min reduction in VO2peak. This pattern is comparable with a previous study that demonstrated an increase of 1 point on the EDSS would lower VO2peak by 2.6 mL/kg/min in persons with MS [9]. Perhaps VO2peak in persons with moderate (PDSS 3.0) and severe (PDSS 4.0–6.0) disability may be more symptom-limited, such that VO2peak values reflect functional limitations that manifest as reduced exercise capacity [12]. The overall implication is that persons with MS have reduced exercise tolerance, particularly as a function of increasing disability, and this has implications for exercise testing and exercise training prescriptions. Accordingly, exercise tolerance should become a primary target of well-designed exercise training programs in MS, particularly those with severe disability, as reduced exercise tolerance is associated with walking impairment, limitations in performing activities of daily living and reduced quality of life [33].
4.2 Ventilatory Anaerobic Threshold (VAT)
Absolute VAT was significantly lower for persons with MS compared with controls, indicating that persons with MS will likely experience earlier onset of fatigue and will be unable to sustain an exercise workload for a prolonged period of time [7]. However, when expressed as a relative value (%VO2peak), VAT was not significantly different between persons with MS and controls, indicating that persons with MS and controls reach VAT at a similar percentage of VO2peak that are within the approximate range (45–65 %) commonly demonstrated in healthy untrained subjects [34]. Another previous study in persons with MS demonstrated similar differences in both absolute and relative VAT between MS and controls, albeit the differences were non-significant; however, that study had a small sample size with unmatched controls [11]. Therefore, whereas persons with MS may demonstrate an overall lower VAT compared with controls, perhaps associated with symptom limitations that reduce VO2peak, the relative percentage at which VAT occurs is the same. Regarding the disability groupings of persons with MS, no significant differences were observed among groups for absolute VAT. In regard to relative VAT, there was a rightward shift with increasing disability and, although the differences among groups were non-significant, these results may reflect the lower VO2peak in persons with MS who have severe disability that could subsequently increase the relative percentage at which the VAT occurs. Consequently, the level of MS disability impacts maximal functional capacity, as well as submaximal exercise ability, similar to the differences between persons with and without MS in general. Therefore, the current results support VAT as an appropriate CPET variable to consider for quantifying adaptations (i.e. increase in VO2peak) to exercise training as previous evidence has demonstrated VAT to occur later (i.e. higher percentage of VO2peak) after exercise training [6]. The reduction in VAT (and associated VO2peak) is often reflective of comorbidities such as heart disease and peripheral arterial disease [14]. As comorbidities are common in persons with MS [18], this underscores the use and analysis of CPET in a clinical setting for further understanding latent processes of cardiovascular comorbidity.
4.3 Peak Respiratory Exchange Ratio (RERpeak)
RERpeak was significantly lower for persons with MS compared with controls. These values are comparable with a previous study [21] and demonstrate that persons with MS are, on average, capable of achieving criteria necessary for a valid CPET (RER ≥1.10); however, the lower peak values in MS may be related to low skeletal muscle oxidative capacity or respiratory muscle weakness [12]. RERpeak was significantly different in the subsamples of persons with MS, such that persons with severe disability demonstrated a lower peak value compared with those who had mild disability. This finding is not consistent with that from a previous study that reported no significant difference in RERpeak by disability in persons with MS [10]; however, that study involved a small sample of persons with MS, with the majority of participants having low (EDSS ≤2.0) and mild (EDSS 2.5–4.0) levels of disability. Overall, our results indicate that persons with MS who have severe disability may not be as capable of higher intensity exercise effort. Although RERpeak is significantly affected by level of disability, participants reached a peak RER ≥1.10, indicating excellent effort in the CPET [6]; however, it may be valuable for researchers and clinicians to use various outcomes during CPET (HRpeak or RPE), in addition to RERpeak, to evaluate effort.
4.4 Ventilation (VE)/Carbon Dioxide Production (VCO2) Slope
VE/VCO2 slope was not significantly different between persons with MS and controls, nor in the subsamples of persons with MS with mild, moderate, and severe disability. Three examples of the VE/VCO2 slope, per level of disability, are illustrated in panel 4 of the “Appendix”. Persons with MS and controls demonstrated a VE/VCO2 relationship that is nearly equivalent to what is considered normal (VE/VCO2 <30) [35], indicating that persons with MS, regardless of disability, adequately match increasing VE with perfusion and demonstrate ventilatory efficiency comparable with that of controls.
4.5 Oxygen Uptake (VO2)/Power Slope
VO2/power slope was significantly lower for persons with MS compared with controls, indicating that persons with MS were less efficient in converting metabolic energy into potential chemical energy [7]. This is dissimilar from a previous study on CPET in persons with MS that reported the VO2/power slope was not significantly different in persons with MS compared with controls [11]; however, that study included only persons with very mild disability (EDSS ≤3), whereas the current study included persons across the disability spectrum, including persons with severe disability (PDDS ≥4.0). Overall, this indicates that persons with MS might not be as capable of attaining higher levels of VO2 associated with higher WRs compared with controls, perhaps due to reduced mechanical efficiency (potentially resulting from increased spasticity) or a higher overall contribution of anaerobic metabolism. The reduction of VO2/power slope may further indicate alterations in the metabolism of skeletal muscles or inadequacies of O2 transport [36]. This underscores the potential value of both resistance and aerobic exercise training in persons with MS to increase muscle strength, and the oxidative capacity of the working muscle, which may lead to improved functioning [37]. Furthermore, the VO2/power slope is commonly abnormal in individuals with cardiovascular diseases [14] and therefore this measurement is clinically meaningful for persons with MS as cardiovascular diseases are common [18]. However, VO2/power slope was not significantly different among the disability groups of persons with MS, suggesting minimal variability in the association between VO2 and WR across persons with MS [21].
4.6 VO2/Heart Rate (HR) Slope
VO2/HR slope was significantly lower for persons with MS compared with controls. These values are higher than those in a previous study that reported VO2/HR slopes of 10.8 (2.3) and 13.7 (4.3) in persons with MS and controls, respectively [38]. However, that study included a very small sample size and a submaximal exercise test on a cycle ergometer rather than CPET. No significant difference was observed in the subsamples of persons with MS who had mild, moderate, and severe disability in the present study. Three examples of VO2/HR slope, per level of disability, are illustrated in panel 2 of the “Appendix”. The overall implication is that persons with MS extract less O2 per heartbeat throughout exercise, and this may reflect an attenuated stroke volume response to exercise [6]. The VO2/HR slope is less steep in individuals with heart failure, or less linear in patients with myocardial ischemia [14], and therefore this is an important outcome for clinical evaluation of CPET in MS.
4.7 Oxygen Uptake Efficiency Slope (OUES)
OUES was lower for persons with MS compared with controls, such that persons with MS demonstrated a flatter slope, indicating that persons with MS demonstrated lower efficiency of O2 uptake with increasing VE. Our results are similar to those from a previous study [10] that identified OUES to be lower in persons with MS when compared with typically observed OUES values in the general population; that study did not include control participants [10]. However, OUES was not significantly different in the subsamples of persons with MS. The non-significant trend for a decrease in OUES with increasing disability is consistent with a previous study that identified OUES to be lower in persons with moderate disability (EDSS ≥4.5) compared with persons with mild disability (EDSS ≤2.0) [10]. As OUES relies on cardiovascular, musculoskeletal, and respiratory functions, the present results may indicate that each of these components is reduced in persons with MS [28]. Therefore, addressing the improvement of those functions should be included as important factors of exercise training programs in MS.
4.8 Peak Ventilation (VEpeak)
VEpeak was significantly lower for persons with MS compared with controls. These results are similar to those from a previous study, indicating reduced ventilatory capacity in persons with MS compared with controls [13]. This may reflect decreased ability to ventilate (i.e. reduced tidal volume or respiratory frequency) or a decrease in ventilatory drive (i.e. maintenance of gas exchange) [39]. Furthermore, VEpeak was significantly different in the subsample of persons with MS, such that persons with severe and moderate disability demonstrated a lower peak compared with persons with mild disability. Panel 5 of the “Appendix” illustrates three examples, per level of disability, of the overall trajectory and peak values of VE. Therefore, our results are in agreement with a previous study [13] that demonstrated a significant relationship between VE and level of neurological impairment and fatigue severity, such that severe disease may lead to respiratory muscle weakness, which in turn may lead to reduced ventilatory capacity in persons with MS.
4.9 Peak HR (HRpeak)
HRpeak was significantly lower for persons with MS compared with controls. These results are similar to a previous study [13] that identified the lower HRpeak in persons with MS compared with controls, as well as reduced stroke volume, abnormal HR, and blood pressure responses to exercise in persons with MS. Therefore, lower HRpeak in persons with MS may be explained by cardiovascular autonomic dysfunction [40, 41] or decreased capacity to exercise (e.g. lower VO2peak). The current study further demonstrated HRpeak to be significantly different in the subsample of persons with MS, such that persons with severe disability had lower HRpeak compared with persons who had moderate and mild disability, indicating that HR responses to exercise may be related to neurological impairment [13]. Panel 2 of the “Appendix” illustrates three examples, per level of disability, of the overall trajectory and peak values of HR.
4.10 Peak Work Rate (WRpeak)
WRpeak (W) was significantly lower for persons with MS compared with controls, indicating that persons with MS were not able to obtain as high a workload during CPET. This is similar to previous studies [11, 21] and may be due to muscle weakness commonly seen in persons with MS [42], or associated with reduced VO2peak, as previous evidence in the general population has demonstrated that VO2peak and WRpeak are strongly correlated [43]. Furthermore, WRpeak was significantly lower in persons with severe disability compared with persons with moderate and mild disability, as illustrated in panel 1 of the “Appendix”, suggesting reduced WRpeak as a function of increasing impairment. These results highlight the need for the inclusion of both cardiorespiratory and musculoskeletal components in exercise training interventions for persons with MS [4].
4.11 Limitations
This study has several limitations. First, the sample was predominantly female and consisted of persons with RRMS; hence, our results may not be generalizable for the entire population of persons with MS. Second, we used the PDDS as a self-reported measure of disability with a few cases with missing PDDS data; this is expected as participants can opt to not report an outcome per human subject regulations. Importantly, in MS the PDDS has been validated as a surrogate for the EDSS [25]. Third, we did not measure current physical activity or exercise behavior in the MS and control samples, which may have influenced CPET outcomes. In addition, we did not screen participants for the use of β-blockers and these may significantly affect CPET outcomes, such as lowering HRpeak [44]. The time of day that CPET was performed varied among participants and could impact outcomes. Finally, we did not measure post-test blood lactate levels, which could be an additional, secondary criterion for a valid CPET.
5 Conclusions
This study provides a comprehensive profile of CPET outcomes for persons with MS. Overall, persons with MS demonstrated alterations in outcomes from CPET and these are generally exacerbated with increasing disability. We believe this study provides novel information for the evaluation of CPET in MS for developing exercise prescriptions and documenting adaptations with exercise training based on the comprehensive variables obtained during CPET. Furthermore, the values could provide comparative metrics for further research using CPET in MS.
References
Mayr WT, Pittock SJ, McClelland RL, Jorgensen NW, Noseworthy JH, Rodriguez M. Incidence and prevalence of multiple sclerosis in Olmsted County, Minnesota, 1985–2000. Neurology. 2003;61(10):1373–7.
Lublin FD. Clinical features and diagnosis of multiple sclerosis. Neurol Clin. 2005;23(1):1–15.
Pilutti LA, Platta ME, Motl RW, Latimer-Cheung AE. The safety of exercise training in multiple sclerosis: a systematic review. J Neurol Sci. 2014;343(1–2):3–7.
Motl RW, Pilutti LA. The benefits of exercise training in multiple sclerosis. Nat Rev Neurol. 2012;8(9):487–97.
Ferrazza AM, Martolini D, Palange P. Cardiopulmonary exercise testing in the functional and prognostic evaluation of patients with pulmonary diseases. Respiration. 2009;77:3–17.
Balady GJ, et al. Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(2):191–225.
Guazzi M, et al. EACPR/AHA Joint Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Eur Heart J. 2012;33(23):2917–27.
Langeskov-Christensen M, Langeskov-Christensen D, Overgaard K, Moller AB, Dalgas U. Validity and reliability of VO2-max measurements in persons with MS. J Neurol Sci. 2014;342(1–2):79–87.
Langeskov-Christensen M, Heine M, Kwakkel G, Dalgas U. Aerobic capacity in persons with multiple sclerosis: a systematic review and meta-analysis. Sports Med. 2015;56(6):905–23.
Heine M, Verschuren O, Kwakkel G. Validity of the oxygen uptake efficiency slope in patients with multiple sclerosis. J Rehabil Med. 2014;46(7):656–61.
Morrison EH, et al. Ratings of perceived exertion during aerobic exercise in multiple sclerosis. Arch Phys Med Rehabil. 2008;89(8):170–4.
Heine M, Hoogervorst EL, Hacking HG, Verschuren O, Kwakkel G. Validity of maximal exercise testing in people with multiple sclerosis and low to moderate levels of disability. Phys Ther. 2014;94(8):1168–75.
Koseoglu BF, Gokkaya NK, Ergun U, Inan L, Yesiltepe E. Cardiopulmonary and metabolic functions, aerobic capacity, fatigue and quality of life in patients with multiple sclerosis. Acta Neurol Scand. 2006;114(4):261–7.
Wasserman K, Hansen JE, Sue DY, Stringer WW, Sietsema KE, Sun X, et al. Principles of exercise testing and interpretation. Philadelphia: Lippincott Williams & Wilkins; 2012.
Coeckelberghs E, Buys R, Goetschalckx K, Cornelissen VA, Vanhees L. Prognostic value of the oxygen uptake efficiency slope and other exercise variables in patients with coronary artery disease. Eur J Prev Cardiol. Epub 29 Jan 2015.
Cahalin LP, Chase P, Arena R, Myers J, Bensimhon D, Peberdy MA, et al. A meta-analysis of the prognostic significance of cardiopulmonary exercise testing in patients with heart failure. Heart Fail Rev. 2013;18(1):79–94.
Magri D, Agostoni P, Corra U, Passino C, Scrutinio D, Perrone-Filardi P, et al. Deceptive meaning of oxygen uptake measured at the anaerobic threshold in patients with systolic heart failure and atrial fibrillation. Eur J Prev Cardiol. 2015;22(8):1046–55.
Marrie RA, Reider N, Cohen J, Stuve O, Trojano M, Cutter G, et al. A systematic review of the incidence and prevalence of cardiac, cerebrovascular, and peripheral vascular disease in multiple sclerosis. Mult Scler. 2015;21(3):318–31.
Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69(2):292–302.
Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Can J Sport Sci. 1992;17(4):338–45.
Motl RW, Fernhall B. Accurate prediction of cardiorespiratory fitness using cycle ergometry in minimally disabled persons with relapsing-remitting multiple sclerosis. Arch Phys Med Rehabil. 2012;93:490–5.
Beier M, Bombardier CH, Hartoonian N, Motl RW, Kraft GH. Improved physical fitness correlates with improved cognition in multiple sclerosis. Arch Phys Med Rehabil. 2014;95(7):1328–34.
Prakash RS, Snook EM, Erickson KI, Colcombe SJ, Voss MW, Motl RW, et al. Cardiorespiratory fitness: a predictor of cortical plasticity in multiple sclerosis. Neuroimage. 2007;34(3):1238–44.
Gordon D, Mehter M, Gernigon M, Caddy O, Keiller D, Barnes R. The effects of exercise modality on the incidence of plateau at VO2max. Clin Physiol Funct Imaging. 2012;32(5):394–9.
Learmonth YC, Motl RW, Sandroff BM, Pula JH, Cadavid D. Validation of patient determined disease steps (PDDS) scale scores in persons with multiple sclerosis. BMC Neurol. 2013;13:37.
Marrie RA, Goldman M. Validity of performance scales for disability assessment in multiple sclerosis. Mult Scler. 2007;13(9):1176–82.
Marrie RA, Cutter G, Tyry T, Vollmer T, Campagnolo D. Does multiple sclerosis-associated disability differ between races? Neurology. 2006;66(8):1235–40.
Mezzani A, et al. Standards for the use of cardiopulmonary exercise testing for the functional evaluation of cardiac patients: a report from the Exercise Physiology Section of the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Cardiovas Prev Rehabil. 2009;16(3):249–67.
Hollenberg M, Tager IB. Oxygen uptake efficiency slope: an index of exercise performance and cardiopulmonary reserve requiring only submaximal exercise. J Am Coll Cardiol. 2000;36(1):194–201.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum; 1988.
Klaren RE, Motl RW, Dlugonski D, Sandroff BM, Pilutti LA. Objectively quantified physical activity in persons with multiple sclerosis. Arch Phys Med Rehabil. 2013;94(12):2342–8.
Christou DD, Seals DR. Decreased maximal heart rate with aging is related to reduced β-adrenergic responsiveness but is largely explained by a reduction in intrinsic heart rate. J Appl Physiol. 2008;105:24–9.
Sandroff BM, Klaren RE, Motl RW. Relationships among physical inactivity, deconditioning, and walking impairment in persons with multiple sclerosis. J Neurol Phys Ther. 2015;39(2):103–10.
Davis JA, Vodak P, Wilmore JH, Vodak J, Kurtz P. Anaerobic threshold and maximal aerobic power for three modes of exercise. J Appl Physiol. 1976;41(4):544–50.
Sun XG, Hansen JE, Garatachea N, Storer TW, Wasserman K. Ventilatory efficiency during exercise in healthy subjects. Am J Respir Crit Care Med. 2002;166:1443–8.
Task Force of the Italian Working Group on Cardiac Rehabilitation Prevention, Working Group on Cardiac Rehabilitation and Exercise Physiology of the European Society of Cardiology, Piepoli MF, et al. Statement on cardiopulmonary exercise testing in chronic heart failure due to left ventricular dysfunction: recommendations for performance and interpretation. Part I: definition of cardiopulmonary exercise testing parameters for appropriate use in chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2006;13(2):150–64.
Kjølhede T, Vissing K, Dalgas U. Multiple sclerosis and progressive resistance training: a systematic review. Mult Scler. 2012;18:1215–28.
Tantucci C, Massucci M, Piperno R, Grassi V, Sorbini CA. Energy cost of exercise in multiple sclerosis patients with low degree of disability. Mult Scler. 1996;2:161–7.
Piepoli MF. Exercise tolerance measurements in pulmonary vascular diseases and chronic heart failure. Respiration. 2009;77:241–51.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33(11):1444–52.
Sutherland G, Andersen MB. Exercise and multiple sclerosis: physiological, psychological, and quality of life issues. J Sports Med Phys Fitness. 2001;41(4):421–32.
Frohman EM, Racke MK, Raine CS. Multiple sclerosis: the plaque and its pathogenesis. N Engl J Med. 2006;354:942–55.
Ashtrand RO, Rodahl K. Textbook of work physiology. New York: McGraw-Hill; 1977.
Tesch PA. Exercise performance and beta-blockade. Sports Med. 1985;2(6):389–412.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Rachel Klaren, Brian Sandroff, Bo Fernhall, and Robert Motl declare that they have no conflicts of interest.
Funding
No financial support was received for the conduct of this study or preparation of this manuscript.
Appendix
Appendix
This appendix provides an eight-panel graphical display of the cardiovascular, ventilatory, ventilation-perfusion matching, and metabolic responses during exercise based on Wasserman et al. [14]. We were unable to provide the ninth panel as we did not measure alveolar or end-expiratory O2 and CO2. We provide the graphic displays of an example case study per group of disability status [mild (a), moderate (b), and severe disability (c)]. Panel 1 illustrates that the person with MS who has severe disability (c) demonstrates lower VO2peak compared with persons who had mild (a) or moderate (b) disability, as well as lower VAT (i.e. submaximal VO2 where there is a dislinear rise in VCO2). Based on Wasserman, this exercise limitation could be associated with certain cardiovascular diseases such as heart disease or peripheral arterial disease. Further interpretation of other panels can be seen in Wasserman et al. [14].
Panel 1: VO2 and VCO2 vs. time and WR
Panel 2: HR and VO2/HR vs. time and WR
Panel 3: HR vs. VO2 and VCO2 vs. VO2
Panel 4: VE for O2 and CO2 vs. time and WR
Panel 5: VE vs. time and WR
Panel 6: VE vs. VCO2
Panel 7: RER vs. time and WR
Panel 8: Tidal volume (VT) vs. VE



Rights and permissions
About this article
Cite this article
Klaren, R.E., Sandroff, B.M., Fernhall, B. et al. Comprehensive Profile of Cardiopulmonary Exercise Testing in Ambulatory Persons with Multiple Sclerosis. Sports Med 46, 1365–1379 (2016). https://doi.org/10.1007/s40279-016-0472-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-016-0472-6